Abstract
INTRODUCTION
Current guidelines on blood ordering in our hospital require all patients undergoing elective breast cancer surgery to have blood grouped, screened and saved as an part of a pre-operative assessment. The aim of this audit was to assess the need for, and cost effectiveness of, this approach in elective breast cancer surgery.
PATIENTS AND METHODS
Retrospective data collection was undertaken for a 2-year period using the theatre booking system. As a result, 497 consecutive elective breast surgery operations including mastectomies, wide local excisions and breast reconstruction procedures were identified for analysis. Using the hospital blood bank computer system, we established the blood group and save or cross-match status as well as the pre- and postoperative haemoglobin results and blood transfusion related data for each of the patients identified.
RESULTS
Of the 497 patients, 438 (88.1%) had blood sent for group-and-save. Of the total 497 patients identified, only 19 (3.82%) patients received a blood transfusion. From the 447 patients undergoing simple mastectomy or wide local excisions alone, 9 patients (1.81%) required transfusion. Fifty patients underwent an immediate reconstruction procedure of whom 10 (20%) required a transfusion.
CONCLUSIONS
This study demonstrates that reconstruction is more likely to be associated with the need for a postoperative transfusion. However, in the context of all breast surgery, blood transfusion is rarely requested. Given this, the time and cost involved in processing a group-and-save pre-operatively is not justified.
Keywords: Breast surgery, Transfusion, Mastectomy, Wide local excision
Our hospital guidelines state that every patient undergoing elective breast surgery should routinely have a blood sample sent for grouping and saving prior to operation. This is usually organised at the time of clerking.
Currently, it takes about 35–45 min for a requested group-and-save blood sample to be processed and costs £4.58. Each unit of blood subsequently requested costs £135.
As the hospital carries out approximately 300 operations each year, a total of £1374 is spent on this aspect of pre-operative preparation. We have analysed whether this expense, disturbance to the patient and use of laboratory time are justified in relation to the number of times subsequent transfusion is carried out.
Patients and Materials
The names and demographic data for each of the patients undergoing elective breast surgery (mastectomy, wide local excision or reconstruction) at Royal Bolton Hospital over a 2-year period (January 2004 to December 2005) were obtained from theatre records. A total of 497 cases were identified.
These data were cross referenced with the hospital's pathology database to assess an individual patient's profile. We determined if a group-and-save was performed and also if there was any subsequent cross-match requested and blood products used.
Results
Of the 497 patients undergoing surgery, 59 patients (11.8%) did not have a pre-operative group-and-save processed.
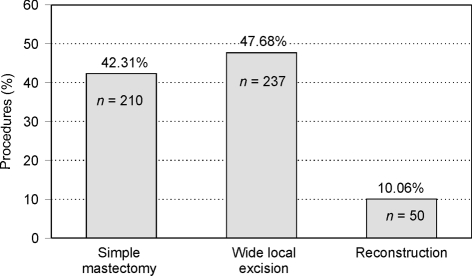
Of those operated on, 260 underwent mastectomy alone of whom 50 had an immediate reconstruction and 237 underwent wide local excision (Fig. 1).
Figure 1.
Percentages of procedures involved.
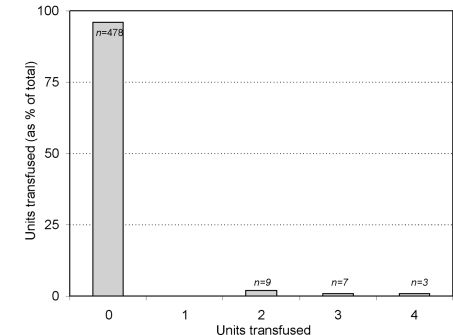
Blood transfusion was only required in 19 patients (3.8%). Of these, two underwent wide local excision, 17 mastectomy, and the remaining 10 patients had mastectomy and immediate reconstruction procedures carried out. An analysis of the number of units used in individual patients is shown in Figure 2. In total, 51 units of blood were transfused.
Figure 2.
Units transfused in individual patients.
Table 1 summarises the reconstruction procedures adopted and transfusion requirements.
Table 1.
Types of reconstruction procedures and the number of blood units required postoperatively
| Reconstruction procedure | Number of cases (50) | Units of blood transfused |
|---|---|---|
| Latissimus dorsi | 30 | 2 U, 5 patients |
| 3 U, 1 patient | ||
| 4 U, 2 patients | ||
| Sub-pectoral | 17 | 3 U, 1 patient |
| TRAM | 1 | 2 U, 1 patient |
| Mini flap | 1 | No units |
| Other | 1 | No units |
In addition, 7 elective breast surgery cases over the 2-year period had 21 blood units ordered which were subsequently not used. Based on current hospital costing, the total haematology cost for group-and-save and subsequent transfusion requests was £8891.04 of which £2006.04 (23%) was spent on processing group-and-save requests. No patient required an emergency peri- or postoperative transfusion.
Discussion
Only 3.8% of patients undergoing elective breast cancer surgery over a 2-year period received blood transfusion (19 out of 497 cases).
Although reconstruction patients accounted for only 10% of the total patients, they accounted for 50% of the transfusion requirement. However, as reconstruction surgery tends to have longer operating times and increased blood loss during the procedure, this is not an unexpected finding. Ten of the reconstruction patients received autologous blood transfusions (20%).
Conclusions
Based on our data, the pre-operative group-and-save policy appears to be an unnecessary procedure which only adds to the burden placed on patients and the haematology laboratories. Had we only carried this out in patients needing transfusion, we would have saved £1913.89 which, although not a large sum, is nevertheless both a cost and time saving.