Abstract
INTRODUCTION
Up to 40% of scaphoid fractures are missed at initial presentation as clinical examination and plain radiographs are poor at identifying scaphoid fractures immediately after the injury. Avoiding a delay in diagnosis is essential to prevent the risk of non-union and early wrist arthritis. We demonstrate the use of CT scanning for the early confirmation of a scaphoid fracture.
PATIENTS AND METHODS
We conducted a retrospective, chronological review of patients who attended an upper limb fracture clinic from January 2001 to October 2003 in a small district general hospital. We performed a CT scan on all ‘clinical scaphoid’ patients who had negative plain X-ray films.
RESULTS
Overall, 70% of patients had a CT scan within 1 week of injury and not from date of accident and emergency attendance; 83% of patients had a CT scan within 2 weeks of injury. Of 118 patients identified, 32% had positive findings and 22% of ‘clinical scaphoid’ patients had scaphoid fractures. The proportion of positive findings for an acute scaphoid fracture was 68%. Additional pathologies identified on CT were capitate, triquetral and radial fractures.
CONCLUSIONS
Our audit shows that it is practical to perform CT on suspicious scaphoid fractures in a small district general hospital. We identified an extremely high false-negative rate for plain X-rays and demonstrate that the appropriate use of CT at initial fracture clinic attendance with ‘clinical scaphoid’ leads to an earlier diagnosis and reduces the need for prolonged immobilisation and repeated clinical review.
Keywords: Scaphoid fracture, Computed tomography, Fracture clinic
Carpal injuries are common presentations to emergency departments, general practitioners and orthopaedic clinics. The scaphoid bone is the most commonly injured of the carpal bones accounting for 50–80% of carpal injuries and predominantly occurs in young. healthy individuals.1,2 Scaphoid fractures are the most problematic to diagnose in a clinical setting because it can take up to 6 weeks for scaphoid fractures to become conclusive on plain X-ray films. It is estimated that up to 40% of scaphoid fractures are missed at first presentation.3,4 A recent meta-analysis of scaphoid fractures calculated that the positive predictive value of clinical examination (those who proved to be ‘clinical scaphoid’ warranted X-rays of scaphoid views who subsequently had scaphoid fracture) is in the range 13–69% with an average of 21%.5 This means that four out of five patients without a fracture will be unnecessarily immobilised before radiological diagnosis is confirmed.
Patients and Methods
We conducted a retrospective, chronological review of patients who attended an upper limb fracture clinic from January 2001 to October 2003 in a district general hospital. Patients with negative X-ray findings but positive clinical signs for scaphoid injury satisfied the criteria for CT. We defined clinical signs for a scaphoid injury as tenderness over the anatomical snuffbox, pain on axial loading of first metacarpal and tenderness over scaphoid tubercle in the presence of normal plain films and included patients whose plain X-rays proved inconclusive.
Patients with clinical indications of scaphoid fracture but negative plain films had their wrists immobilised in a scaphoid cast in the accident unit while awaiting a hand clinic appointment.
CT scans, where necessary, were carried out on the same day as review on the first presentation to the fracture clinic with results available immediately. This facility was made available by the radiology department.
Results
A total of 118 patients presented with an acute wrist injury with subsequent signs of scaphoid injury in the absence of a diagnostic fracture on plain X-ray within the time period. Causes of injury are summarised in Table 1.
Table 1.
Types of injury sustained by the study group (n = 118)
| Injury | Number of patients (%) |
|---|---|
| Fall onto outstretched hand (FOOSH) | 94 (80%) |
| Road traffic accident | 11 (9%) |
| Sport related | 9 (8%) |
| Direct trauma | 4 (3%) |
The age range was 10–72 years and the majority of patients were 29–45 years old. Of patients, 52% were female.
Eighty-four (70%) patients had CT imaging of their scaphoid within 1 week of the exact date of injury and 99 (83%) patients had CT imaging within 2 weeks of injury.
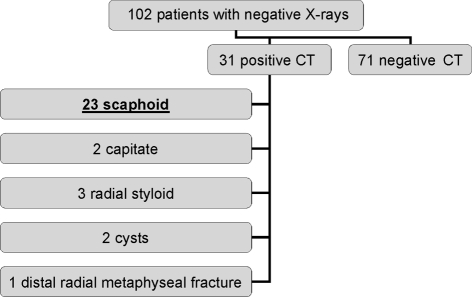
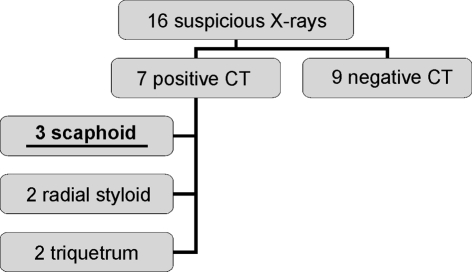
Of the 118 X-ray films, 16 were suspicious of which eight were suspected scaphoid fractures. Fractures of the distal radius and other carpal bones were also identified as shown in Figure 1. Overall, 102 patients had a clinical scaphoid injury but negative X-rays. Of these 102 patients with negative X-rays, 32 had positive CT findings. Of these 32 patients with positive CT scans, 23 revealed acute scaphoid fractures. The other 8 diagnoses included: two capitate, three distal radial fractures, two scaphoid cysts and one distal radial fracture (Fig. 1).
Figure 1.
Outcomes of patients with negative plain films.
Figure 2.
Outcomes of patients with suspicious initial plain films.
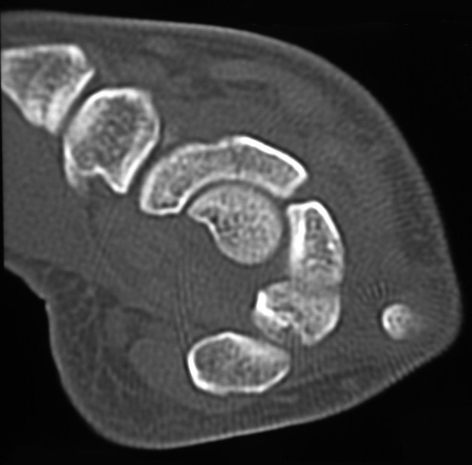
Figure 3.
A scaphoid fracture.
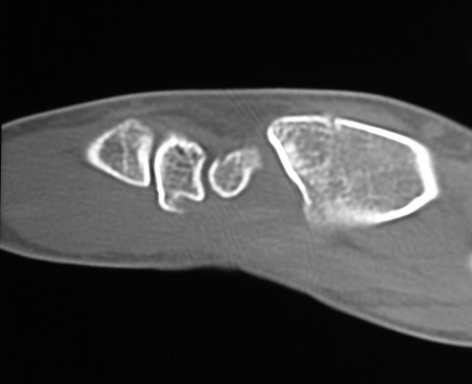
Figure 4.
A distal radial styloid fracture.
Of patients with normal plain radiographs, 31% (32 of 102) had positive findings, of which 22% (23 of 102) were scaphoid fractures. CT imaging confirmed 3 from 8 possible scaphoid fractures on plain X-ray films.
Of the patients with normal X-rays, 31% had positive findings on CT. The proportion of positive findings for an acute scaphoid fractures was 74% (23 of 31).
Eighty patients had normal CT findings. All patients were immobilised in a scaphoid cast until the fracture healed (for a period of 6–9 weeks) and discharged.
Two patients treated with plaster had continuing pain and underwent MRI scanning confirming no positive findings. One patient with a proximal pole fracture treated with plaster for 3 months, successfully underwent open reduction and internal fixation after a subsequent CT scan showed non-union.
Discussion
Failure to diagnose and immobilise scaphoid injuries can lead to osteoarthritis, mal-union, non-union and avascular necrosis; non-union is in the order of 5–12%.6,7 Even asymptomatic non-union has been shown to lead to deterioration, both clinically and radiologically, with time.8 Fracture of the scaphoid bone can be difficult to diagnose because it may take up to several weeks for radiological evidence to be conclusive.9 Initial radiographic sensitivity can be up to 64% and falls on further imaging to only 30%.10 Immobilisation for a clinical scaphoid injury is usually in a scaphoid cast for at least 6 weeks until a conclusion is drawn from imaging in conjunction with repeated clinical examination. In such cases, the options available are a modified carpal view, bone scintigraphy, MRI, and CT. Some use modified views first and then proceed to CT when diagnosis is still in doubt.11
Isotope bone scintigraphy as a second-line investigation has high sensitivity for fractures but poor specificity with a false-positive rate of 25% when compared with delayed radiograph.12,13 Taking into account that bone scintigraphy is more sensitive than plain radiograph, a significant proportion of patients may potentially be over-treated. CT is an accurate and reliable source of imaging to diagnose scaphoid fractures and has been shown to be more sensitive than bone scintigraphy (sensitivity, specificity and positive and negative predicted value of CT is 100% compared to 78%, 90%, 78% and 90%, respectively, for bone scintigraphy).14
It has been suggested that MRI should be used as the gold standard to diagnose scaphoid injuries.15 Some authors advocate that CT could be used as gold standard to record whether union has been achieved.16
MRI has definite advantages in that it provides an accurate diagnosis of scaphoid fractures including information on the vascularity of the fragments involved and elucidates soft tissue injuries that conventional scaphoid views, modified carpal box view and CT are not able to delineate. However, the use of MRI in most UK NHS hospitals to elucidate scaphoid injury in an acute setting is usually not practical.
Our clinic makes use of CT to image the ‘clinical’ scaphoid when initial films of scaphoid views fail to show pathology. Our findings that 31% of normal X-rays were pathological on CT imaging and the overwhelming number of these were scaphoid fractures (74% of pathologies) represent a large number of patients with fractures that were missed by initial plain films. Moreover, they also represent an even larger number of patients (69%) with clinical scaphoid that would have been plastered for at least 6 weeks and asked to re-attend fracture/hand clinic at least three times before discharge, confirming the prophecy ‘we over-treat a lot of patients to avoid under-treating a few’.17
In addition, CT scans can help the surgeon decide whether a structural bone graft is required, the preferred screw fixation and whether a volar or dorsal approach is more appropriate.
The cost of scaphoid films is £16 and a limited CT scaphoid scan is £57 including radiologist fees. But CT scanning has the potential for greater savings in terms of allowing the diagnosis of a fracture to be made earlier and timely appropriate treatment to commence.
Conclusions
Our data demonstrate that it is possible to combine a CT facility with an upper limb clinic in a UK hospital and, thus, advance the diagnostic time period. We have shown an extremely high false-negative rate for plain X-rays and advocate CT at the first attendance to fracture clinic if there is suspicion of scaphoid injury. An earlier diagnosis leads to appropriate management and reduces restrictions to the patient in terms of prolonged immobilisation and repeated clinical reviews. We, therefore, recommend the early use of CT imaging as a second-line investigation for ‘clinical scaphoid’ injury.
References
- 1.Larsen CF, Brodum V, Skov O. Epidemiology of scaphoid fractures in Odense, Denmark. Acta Orthop Scand. 1992;63:216–20. doi: 10.3109/17453679209154827. [DOI] [PubMed] [Google Scholar]
- 2.Mehta M, Brautigan MW. Fracture of carpal navicular. Efficacy of clinical findings and improved diagnosis of six view radiography. Ann Emerg Med. 1990;19:225–31. doi: 10.1016/s0196-0644(05)82039-6. [DOI] [PubMed] [Google Scholar]
- 3.Cooney WP, Linscheid RI, Dobyns JH. Fractures and distortion of the wrist. In: Rockwood CA, editor. Fractures in adult. Philadelphia, PA: Lippincott-Raven; 1996. pp. 755–67. [Google Scholar]
- 4.Waizengger M, Barton NJ, David TR, Waistie ML. Clinical signs in scaphoid fractures. J Hand Surg Br. 1994;19:743–6. doi: 10.1016/0266-7681(94)90249-6. [DOI] [PubMed] [Google Scholar]
- 5.Dorsay TA, Major NM, Helms CA. Cost-effectiveness of immediate MR imaging versus traditional follow-up for revealing radiographically occult scaphoid fracture. Am J Radiol. 2001;177:1257–63. doi: 10.2214/ajr.177.6.1771257. [DOI] [PubMed] [Google Scholar]
- 6.Leslie IJ, Dickson RA. The fractured carpal scaphoid. Natural history and factors influencing outcome. J Bone Joint Surg Br. 1981;63:225–30. doi: 10.1302/0301-620X.63B2.7217146. [DOI] [PubMed] [Google Scholar]
- 7.Dias JJ, Brenkel IJ, Finlay DB. Patterns of non union in fractures in the waist of scaphoid. J Bone Joint Surg Br. 1989;71:307–10. doi: 10.1302/0301-620X.71B2.2925752. [DOI] [PubMed] [Google Scholar]
- 8.Lindstrom G, Nystrom A. Natural history of scaphoid non-union, with special reference to ‘asymptomatic’ cases. J Hand Surg Br. 1993;18:403–6. doi: 10.1016/0266-7681(92)90204-f. [DOI] [PubMed] [Google Scholar]
- 9.Tiel-van Buul MM, van Beek EJ, Broekhuizen AH, Nooit-Gedacht EA, Davids PH, Bakker AJ. Diagnosing scaphoid fractures: radiographs cannot be used as gold standard! Injury. 1992;23:77–9. doi: 10.1016/0020-1383(92)90035-q. [DOI] [PubMed] [Google Scholar]
- 10.Tiel-van Buul MM, van Beek EJ, Borm JJ, Gubler FM, Broekhuizen AH, van Royen EA. The value of radiographs and bone scintigraphy in suspected scaphoid fracture. A statistical analysis. J Hand Surg Br. 1993;18:403–6. doi: 10.1016/0266-7681(93)90074-p. [DOI] [PubMed] [Google Scholar]
- 11.Toth F, Mester S, Cseh G, Bener A, Nyarady J, Lovasz G. Modified carpal box technique in the diagnosis of suspcted scaphoid fractures. Acta Radiol. 2003;44:319–25. doi: 10.1080/j.1600-0455.2003.00064.x. [DOI] [PubMed] [Google Scholar]
- 12.Tiel-van Buul MM, van Beek EJ, Broekhuizen AH, Bakker AJ, Bos KE, van Royen EA. Radiography and scintigraphy of suspected scaphoid fracture. J Bone Joint Surg Br. 1993;75:61–5. doi: 10.1302/0301-620X.75B1.8421037. [DOI] [PubMed] [Google Scholar]
- 13.Brismar J. Skeletal scintigraphy of the wrist in suggested scaphoid fracture. Acta Radiol. 1988;29:101–7. [PubMed] [Google Scholar]
- 14.Breederveld RS, Tuinebreijer WE. Investigation of computed tomographic scan concurrent criterion validity in doubtful scaphoid fracture of the wrist. J Trauma. 2004;57:851–4. doi: 10.1097/01.ta.0000124278.29127.42. [DOI] [PubMed] [Google Scholar]
- 15.Brydie A, Raby N. Early MRI in the management of clinical scaphoid fracture. Br J Radiol. 2003;76:296–300. doi: 10.1259/bjr/19790905. [DOI] [PubMed] [Google Scholar]
- 16.Plancher KD. Methods of imaging the scaphoid. Hand Clin. 2001;17:703–6. [PubMed] [Google Scholar]
- 17.Barton N. Twenty questions about scaphoid fractures. J Hand Surg Br. 1992;17:289–310. doi: 10.1016/0266-7681(92)90118-l. [DOI] [PubMed] [Google Scholar]