Abstract
INTRODUCTION
The introduction of Modernising Medical Careers (MMC) is likely to reduce specialist registrar (SpR) operative experience during higher surgical training (HST). A further negative impact on training by local Independent Sector Treatment Centres (ISTCs) could reduce experience, and thus competence, in primary joint arthroplasty at completion of higher surgical training.
PATIENTS AND METHODS
Retrospective case note and radiograph analysis of patients receiving primary hip and knee arthroplasty in a teaching hospital, before and after the establishment of a local ISTC. Patients and operative details were recorded from the selected case notes. Corresponding radiographs were assessed and the severity of the disease process assessed.
RESULTS
Fewer primary hip and knee replacements were performed by SpRs in the time period after the establishment of an ISTC.
Conclusions
ISTCs may adversely affect SpR training in primary joint arthroplasty.
Keywords: Independent Sector Treatment Centres, Specialist registrar training, Primary hip and knee arthroplasty
There has been a significant evolution in higher surgical training (HST) beginning with the introduction of Calman Training in 1995. The introduction of the specialist registrar (SpR) grade and fixed length of HST reduced the operative experience of trainees at the time of consultant appointment. The training impact of this change provoked relatively little concern as registrar and senior registrar appointments were often considered to be longer than necessary.
The first phase of introduction of the European Working Time Directive (EWTD), made compulsory in postgraduate medical education in August 2004, has had a significant impact on surgical training. Forced change to shift working and reduction in worked hours is likely to reduce SpR experience in elective orthopaedic surgery further.
The development of Modernising Medical Careers (MMC) with new Specialist Training programmes (ST 1–7) following on from the Foundation Programme and replacing SpR training programmes from August 2007 has provoked wide-spread discussion and concern regarding training. The introduction of the Electronic Logbook (a joint venture between the Northern Deanery, British Orthopaedic Association [BOA], Specialist Advisory Committee [SAC], British Orthopaedic Training Association [BOTA] and the Royal College of Surgeons of Edinburgh [RCSEd]) will facilitate accurate monitoring of trainee surgical experience. Analysis of data from 2004 suggests introduction of MMC will reduce the number of primary total hip and knee replacements performed by trainees from 37 and 44 to 22 and 24, respectively.1
There is little consensus on how many times a particular procedure needs to be performed to constitute adequate training for independent practice. There is, however, a general concern that structural changes may compromise the adequacy of this training. In addition to the impact of the change in structure of postgraduate medical education on training there is a potential further impact from Independent Sector Treatment Centres (ISTCs). ISTCs are thought to perform a large number of relatively simple primary joint replacements on relatively fit patients. This is potentially leaving adjacent teaching institutions with a higher proportion of complex cases and a greater number of unfit patients. The purpose of this study was to evaluate the effect of ISTCs on SpR experience in primary joint arthroplasty.
Patients and Methods
A cohort of 100 patients before February 2004 and after May 2004 who underwent primary hip and knee arthroplasty at the Derbyshire Royal Infirmary (DRI) were selected. In February 2004, an ISTC became operational in the locality taking patients already on waiting lists at the DRI for primary hip and knee arthroplasty. These were the longest waiting patients thus at the top of the list. Patients were generally accepted if they were ASA grade 1–3, with body mass index less than 40 kg/m2 and were relatively fit with no significant cardiac history.
Consecutive names from theatre records of two consultants (JWH and JMR) were taken working backwards from February 2004 and forwards from May 2004. From these lists, notes and radiographs were obtained. Overall, 95 sets were obtained for the period August 2002 to January 2004 and 86 sets for the period May 2004 to August 2005. Only patients for whom both notes and radiographs were available were used hence the exclusions. The various parameters extracted from the patient records are summarised in Table 1.
Table 1.
Details extracted from patient records
| Case notes |
|
| Operating records |
|
| Immediate pre-operative radiograph |
|
No radiological scoring system which could easily be used to grade the difficulty of the operation could be identified and so the total number of factors was used to grade difficulty. The information could be used to identify any difference in operating experience afforded to SpRs at a teaching hospital (DRI) following the establishment of an ISTC and attempt to rationalise any difference.
Results
Before February 2004, 32.7% of total hip replacements (THRs) and 54.3% of total knee replacements (TKRs) were performed by SpRs. Overall, 43.2% of primary THRs and TKRs were performed by SpRs. After May 2004 28.0% of THRs and 19.4% of TKRs were performed by SpRs. Overall, 24.0% of primary THRs and TKRs were performed by SpRs. There was a statistically significant reduction in total number of procedures performed by SpRs in the before and after time periods (P = 0.023). When analysed separately, the number of TKRs performed in the time period after May 2004 was statistically significantly reduced (P = 0.010) but the difference for THRs did not achieve statistical significance (P = 0.307).
Only 10.5% of procedures before February 2004 and 1.2% of procedures after May 2004 were not directly supervised by a consultant.
There was little difference in the mean number of recorded co-morbidities per patient with 1.1 and 1.0 per patient receiving THR and TKR, respectively, prior to February 2004 and 0.9 and 1.1 per patient receiving THR and TKR, respectively, after May 2004.
The mean ASA grade was 2.1 and 2.2 for patients receiving THR and TKR, respectively, before February 2004 and 2.2 for patients receiving THR and TKR after May 2004. Table 2 shows the distribution.
Table 2.
ASA grade
| Time period | Joint replaced | ASA grade mean | ASA grade mode | ASA 1 | ASA 2 | ASA 3 | ASA 4 | ASA 5 |
|---|---|---|---|---|---|---|---|---|
| Before February 2004 | Hip | 2.1 | 2 | 16.3% | 53.1% | 28.6% | 2.0% | 0% |
| Before February 2004 | Knee | 2.2 | 2 | 6.5% | 65.2% | 28.3% | 0% | 0% |
| After May 2004 | Hip | 2.2 | 2 | 12.2% | 57.1% | 28.6% | 2.0% | 0% |
| After May 2004 | Knee | 2.2 | 2 | 16.7% | 50.0% | 33.3% | 0% | 0% |
Complications did not appear to have been well recorded and were 6.1% and 13% for THR and TKR, respectively, before February 2004 and 4.1% and 11.1% for THR and TKR, respectively, after May 2005. Of 13 recorded complications there was 1 wound infection and 2 further patients required washouts. The remainder were medical complications.
The average duration of stay is recorded in Table 3. There were 3 patients having TKR before February 2004 with stays longer than 23 days. If these patients are excluded from analysis, the average stay is 7.2 days.
Table 3.
Duration of stay
| Average duration (days) | Range (days) | ||
|---|---|---|---|
| Before February 2004 | Hip | 6.1 | 4–18 |
| Before February 2004 | Knee | 13 | 5–35 |
| After May 2004 | Hip | 6.3 | 4–14 |
| After May 2004 | Knee | 6.8 | 4–12 |
An average score of difficulty of operation was calculated. Each joint has 1–5 possible features. A value of 100% represents a radiograph with all 5 features whilst 20% represents a radiograph with only 1 feature. Average scores for THR and TKR before February 2004 was 68.6% and 50.9%, respectively. After May 2004, average scores for THR and TKR were 66.1% and 57.2%, respectively. Varus and valgus deformity was considered separately for TKR; before February 2004, 21.7% and 6.0% of TKRs had these deformities, respectively. Corresponding figures for after May 2004 were 47.2% and 14.0% varus and valgus deformity. respectively.
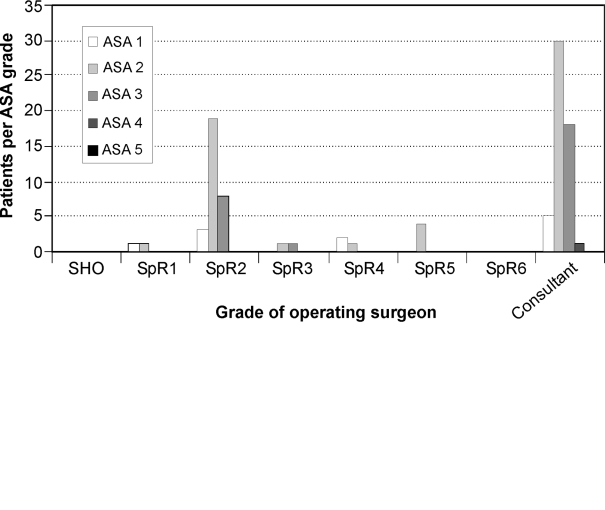
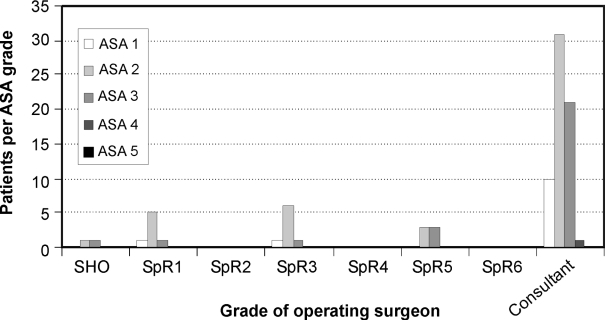
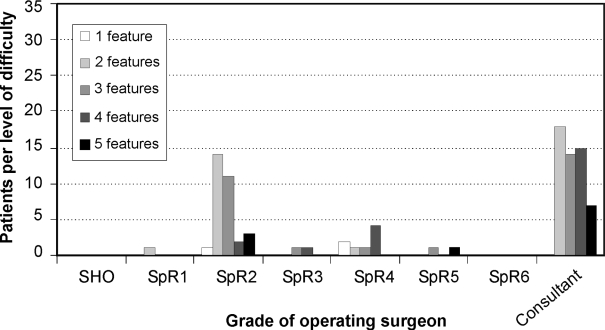
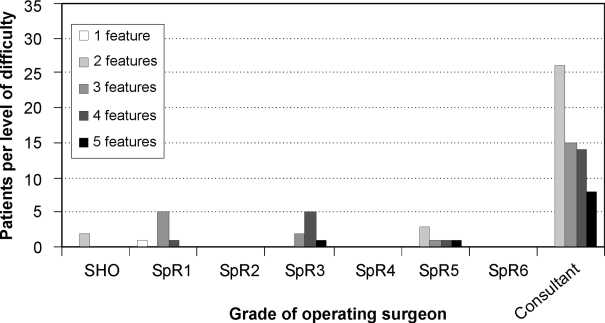
Figures 1 and 2 demonstrate the relationship between ASA grade and operating surgeon grade for arthroplasties performed in each time period. These figures show little relationship between ASA grade and grade of the operating surgeon. Figures 3 and 4 show the relationship between difficulty of operation (considered to be proportional to number of radiological features) and operating surgeon grade. There is no clear relationship between these two factors.
Figure 1.
Relationship between ASA grade and operating surgeon grade for THRs and TKRs before February 2004.
Figure 2.
Relationship between ASA grade and operating surgeon grade for THRs and TKRs after May 2004.
Figure 3.
Relationship between difficulty and operating surgeon grade for THRs and TKRs before February 2004.
Figure 4.
Relationship between difficulty and operating surgeon grade for THRs and TKRs after May 2004.
Discussion
There was a large, and statistically significant, difference in number of procedures performed by SpRs in the two time periods. Overall, 19% less procedures were carried out by SpRs after the ISTC started. More strikingly, SpRs performed almost 35% less TKRs after the ISTC was operational.
There is very little difference between patient co-morbidities and ASA grade in the two time periods and this does not explain the reduction in SpR operative experience. There was little difference between postoperative duration of stay and complications and little difference would be expected considering similarities in patient factors between the two time periods.
A crude assessment of operation difficulty has been used as no simple robust system for such assessment could be identified. There is no clear difference in level of difficulty between the two time periods. However, there were more than twice as many knees with varus or valgus deformity and this may indicate increased level of difficulty. The degree of passive correctabilty was not available and thus these deformities could be easily correctable with bone cuts alone.
There was no clear relationship between grade of operating surgeon and difficulty of operation or ASA grade of patient. A larger number of subjects would be required to demonstrate this relationship.
There was no difference in trainee seniority in each time period which could explain the reduced experience. Three of seven trainees in the first period were year 4 or above and two of four SpRs in the second period were year 5 and above.
Conclusions
There was a large reduction in SpR experience in primary joint arthroplasty following the establishment of a local ISTC. We could not identify any factors concerning operation complexity or patient co-morbidity which could explain this trend. ISTCs may, therefore, adversely affect training and larger studies are required to confirm or refute this and assess any impact on training.
Acknowledgments
We are grateful to Apostolos Fakis, medical statistician at the University of Nottingham, for his input with statistical analysis.
Reference
- 1.Sher JL, Reed MR, Calvert P, Wallace WA, Lamb A. Influencing the National Training Agenda: the UK and Ireland Orthopaedic E-logbook. J Bone Joint Surg Br. 2005;87:1182–6. doi: 10.1302/0301-620X.87B9.16433. [DOI] [PubMed] [Google Scholar]