Abstract
INTRODUCTION
The correction of anaemia prior to total hip arthroplasty reduces surgical risk, hospital stay and cost. This study considers the benefits of implementing a protocol of identifying and treating pre-operative anaemia whilst the patient is on the waiting list for surgery.
PATIENTS AND METHODS
From a prospective series of 322 patients undergoing elective total hip arthroplasty (THA), patients identified as anaemic (haemoglobin (Hb) < 12 g/dl) when initially placed upon the waiting list were appropriately investigated and treated. Pre- and postoperative Hb levels, need for transfusion, and length of hospital stay were collated for the entire patient cohort.
RESULTS
Of the cohort, 8.8% of patients were anaemic when initially placed upon the waiting list for THA and had a higher transfusion rate (23% versus 3%; P < 0.05) and longer hospital stay (7.5 days versus 6.6 days; P < 0.05). Over 40% of these patients responded to investigation and treatment whilst on the waiting list, showing a significant improvement in Hb level (10.1 g/dl to 12.7 g/dl) and improved transfusion rate.
CONCLUSIONS
Quantifying the haemoglobin level of patients when initially placed on the waiting list helps highlight those at risk of requiring a postoperative blood transfusion. Further, the early identification of anaemia allows for the utilisation of the waiting-list time to investigate and treat these patients. For patients who respond to treatment, there is a significant reduction in the need for blood transfusion with its inherent hazards.
Keywords: Total hip arthroplasty, Anaemia
Total hip arthroplasty (THA) is a common orthopaedic procedure and pre-operative anaemia increases the incidence of intra-operative and postoperative morbidity and mortality for this procedure.1–3 The clinical presentation of anaemia is variable and thus the clinician needs to rely upon haematological indices.
UK Government targets dictate a maximum waiting-list time of 18 weeks for THA surgery within the NHS.4 It has previously been proposed that identifying patients at risk of peri-operative anaemia, by carrying out a full blood count upon referral by their general practitioner (GP), allows for appropriate investigation and treatment before surgery.3 However, current practice often involves anaemia being identified as part of the routine assessment shortly before surgery, leading to possible delays and cancellations whilst investigation and treatment is instigated.
The correction of anaemia prior to THA surgery reduces surgical risk, hospital stay and cost.5 The use of oral iron therapy has been extensively reviewed since it is a frequently employed treatment. Although shown to reduce the incidence of anaemia prior to joint replacement surgery,5 the clinical value of its use following surgery has recently been questioned.6 No consensus exists as to the most beneficial way of treating anaemia with oral iron therapy, as there are significant gastrointestinal side effects.7
Homologous blood transfusion has numerous inherent risks and complications including infection, incompatibility, immunosuppression8–11 and, specifically, is associated with a higher rate of infection following THA surgery.12,13 Thus, it is beneficial to reduce the blood transfusion rate and correction of pre-operative anaemia has been demonstrated to be one method of achieving this.3
This study considers the benefits of implementing a protocol of early identification and treatment of pre-operative anaemia whilst the patient is on the waiting list for surgery. Specifically, we aimed to answer the following questions:
What percentage of patients were anaemic when initially placed upon the waiting list?
What percentage of patients responded to investigation and treatment of anaemia whilst on the waiting list?
Did this approach reduce the transfusion rate?
Patients and Methods
We prospectively analysed 322 patients undergoing elective primary THA over a 3-year period; of these, 181 were female and 141 were male with an average age of 67 years (range, 31–90 years). Osteoarthritis (primary or secondary) and osteonecrosis were the principal indications for surgery. No patients had rheumatoid arthritis.
A full blood count (FBC) was performed on each patient when initially placed on the waiting list. Patients anaemic at this point in time (Hb ≤ 12 g/dl) were investigated and treated accordingly. All patients were subsequently assessed within a nurse-lead pre-operative assessment clinic, including a further FBC. The mean waiting list time was 24.5 weeks.
A variety of prostheses were used depending upon the clinical indication. A drain was routinely used for the first 24 h after surgery and the patient mobilised as soon as possible. Pharmacological thrombo-embolic prophylaxis was provided using either daily aspirin (75 mg) or warfarin/low molecular weight heparin for high-risk patients – the dose being titrated to INR and continued for a period of 6 weeks following surgery. No mechanical thrombo-embolic prophylaxis was employed.
The following parameters were measured:
Patient demographics
- Haemoglobin (Hb)
- When initially put on waiting list (W/L Hb)
- Pre-operative assessment clinic
- Following operation (day 1)
Patient requiring blood transfused?
Length of hospital stay
The entire patient cohort was subdivided depending on the haemoglobin levels when initially placed on the waiting list (W/L Hb) and at the pre-assessment clinic. Patients with an Hb ≤ 12 g/dl when placed on the waiting list were further subdivided into: (i) patients in whom anaemia improved prior to surgery, i.e. preoperative Hb > 12 g/dl – ‘responders’; and (ii) patients in whom anaemia failed to improve, i.e. pre-operative Hb < 12 g/dl – ‘non-responders’.
Chi-square (for group comparisons) and unpaired t-test (for continuous variable comparison) analyses was performed with statistical significance considered to be P < 0.05. The statistical package used was SPSS for Windows v.10.1.0.
Results
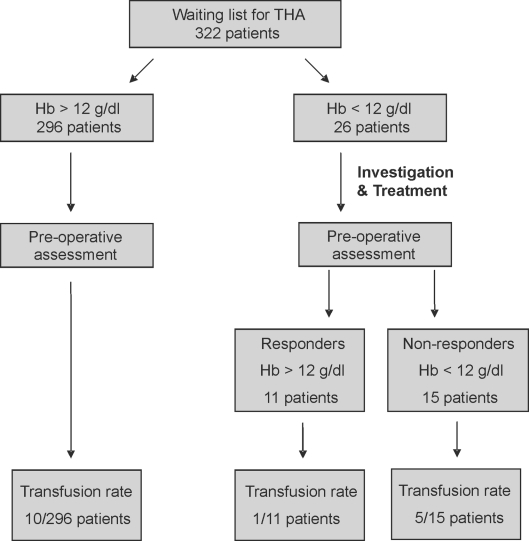
From the initial patient cohort of 322 patients, 26 (8.8%) were found to be anaemic (Hb < 12 g/dl) when initially placed upon the waiting list. Following investigation and treatment, 11 of these patients responded to treatment and were found to have an Hb > 12 g/dl prior to surgery (Fig. 1). A total of 16 patients (4.9%) were anaemic (Hb < 12 g/dl) at the pre-operative assessment, 10 patients fewer than the 26 initially found to be anaemic.
Figure 1.
Entire patient cohort and subsets.
The demographic profile of these separate patient subgroups demonstrate an even gender distribution for patients with a Hb > 12 g/dl when initially placed upon the waiting list, but a statistically significant female predominance (P = 0.02) in patients with an Hb < 12 g/dl (Table 1).
Table 1.
Demographic patient profiles for each of the subgroups in the study, including responders and non-responders
| Male | Female | |
|---|---|---|
| Waiting list (Hb > 12 g/dl) | 139 (47%) | 157 (53%) |
| Waiting list (Hb < 12 g/dl) | 2 (8%) | 24 (92%) |
| Non-responders | 2 | 13 |
| Responders | 0 | 11 |
Of the 26 patients found to be anaemic when initially placed upon the waiting list, four underwent oesophagogastroduodenoscopy (OGD) that was unremarkable and one patient was diagnosed with thyrotoxicosis. Additional treatment entailed cessation of non-steroidal anti-inflammatory drugs (NSAIDs) and concurrent oral iron therapy.
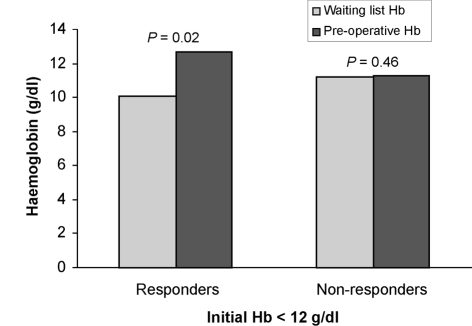
Anaemic patients who responded to investigation and treatment prior to surgery (‘responders’) showed a significant improvement in haemoglobin level (10.1 g/dl to 12.7 g/dl; P = 0.02; Fig. 2).
Figure 2.
Mean change in haemoglobin levels following investigation and treatment.
There was no statistical difference (P = 0.83) in the length of hospital stay between anaemic patients who responded to treatment and non-anaemic patients, but a significant difference between the responding and non-responding groups (P = 0.04). Correspondingly, responders and non-anaemic patients were of similar age whilst the non-responders were significantly older (P = 0.0024; Table 2). The transfusion rate for responders was significantly lower than non-responders (1 out of 11 patients compared to 5 out of 15 patients; P < 0.05).
Table 2.
Length of hospital stay and patient age for nonanaemic patients, responders and non-responders
| Length of stay (days) | Age (years) | |
|---|---|---|
| Non-responders | 8.61 | 82.3 |
| Responders | 6.1 | 67.8 |
| Non-anaemic | 6.6 | 66.4 |
Discussion
The identification and correction of anaemia prior to THA surgery is important and deserves attention.1–3,14,15 Blood transfusion is associated with a prolonged hospital stay2,12 and increased peri-operative risks11 including infection.8,13.
In our series, 26 out of 322 patients (8.8%) were anaemic when initially placed upon the waiting list for THA. This compares favourably to previous studies,3 possibly reflecting the high socio-economic profile of the hospital catchment area. These patients were predominantly female (24 out of 26 patients) and 10 years older than the non-anaemic group, highlighting the need to carefully assess this patient group prior to elective THA surgery.
Over 40% of anaemic patients responded to investigation and treatment whilst on the waiting list. These patients were characteristically younger than the non-responding group and were discharged at a similar time to the nonanaemic group. Whilst one patient in this group was diagnosed with thyrotoxicosis, all other patients were prescribed oral iron therapy with concurrent cessation of NSAIDs.
Anaemic patients who responded to treatment whilst on the waiting list showed a significant improvement (P = 0.02) in haemoglobin level (10.1 g/dl to 12.7 g/dl). They were less likely to require transfusion than patients who failed to respond to treatment. The length of hospital stay and overall transfusion rate (5%) in this study compares favourably with other studies.2,3,13
Our results indicate that the additional cost of performing a full blood count (approximately £1 per test) when the patient is initially placed upon the waiting list is outweighed by the advantages of early identification of anaemia in patients awaiting primary THA surgery. Estimation of haemoglobin level at this stage highlights those at risk of requiring a blood transfusion and allows the waiting-list time to be utilised to instigate appropriate investigate and treatment.
Conclusions
This study demonstrates the benefits of the early identification, investigation and treatment of pre-operative anaemia for patients undergoing elective total hip arthroplasty.
References
- 1.Diamond PT. Severe anaemia: implications for functional recovery during rehabilitation. Disabil Rehabil. 2000;22:574–6. doi: 10.1080/096382800416823. [DOI] [PubMed] [Google Scholar]
- 2.Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano LM. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res. 2002;102:237–44. doi: 10.1006/jsre.2001.6330. [DOI] [PubMed] [Google Scholar]
- 3.Myers E, Grady PO, Dolan AM. The influence of preclinical anaemia on outcome following total hip replacement. Arch Orthop Trauma Surg. 2004;124:699–701. doi: 10.1007/s00402-004-0754-6. [DOI] [PubMed] [Google Scholar]
- 4.Day M. Orthopaedic departments will have more difficulty meeting 18 week waiting target. BMJ. 2007;335:64. doi: 10.1136/bmj.39269.511007.DB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andrews CM, Lane DW, Bradley JG. Iron pre-load for major joint replacement. Transfus Med. 1997;7:281–6. doi: 10.1046/j.1365-3148.1997.d01-42.x. [DOI] [PubMed] [Google Scholar]
- 6.Mundy GM, Birtwistle SJ, Power RA. The effect of iron supplementation on the level of haemoglobin after lower limb arthroplasty. J Bone Joint Surg Br. 2005;87:213–7. doi: 10.1302/0301-620x.87b2.15122. [DOI] [PubMed] [Google Scholar]
- 7.Swerdlow PS. A tradition of testing ironclad practices. JAMA. 1992;267:560–1. [PubMed] [Google Scholar]
- 8.Kendall SJ, Weir J, Aspinall R, Henderson D, Rosson J. Erythrocyte transfusion causes immunosuppression after total hip replacement. Clin Orthop. 2000;381:145–55. doi: 10.1097/00003086-200012000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Sazama K. Reports of 355 transfusion-associated deaths: 1976 through 1985. Transfusion. 1990;30:583–90. doi: 10.1046/j.1537-2995.1990.30790385515.x. [DOI] [PubMed] [Google Scholar]
- 10.Brand A. Immunological aspects of blood transfusions. Transpl Immunol. 2002;10:183–90. doi: 10.1016/s0966-3274(02)00064-3. [DOI] [PubMed] [Google Scholar]
- 11.Williamson LM, Lowe S, Love EM, Cohen H, Soldan K, McClelland DB, et al. Serious Hazards of Transfusion (SHOT) initiative: analysis of the first two annual reports. BMJ. 1999;319:16–9. doi: 10.1136/bmj.319.7201.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81:2–10. doi: 10.2106/00004623-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Triulzi DJ, Vanek K, Ryan DH, Blumberg N. A clinical and immunologic study of blood transfusion and postoperative bacterial infection in spinal surgery. Transfusion. 1992;32:517–24. doi: 10.1046/j.1537-2995.1992.32692367194.x. [DOI] [PubMed] [Google Scholar]
- 14.Callaghan JJ, Spitzer AI. Blood management and patient specific transfusion options in total joint replacement surgery. Iowa Orthop J. 2000;20:36–45. [PMC free article] [PubMed] [Google Scholar]
- 15.Sculco TP. Blood management in orthopedic surgery. Am J Surg. 1995;170:60S–63S. doi: 10.1016/s0002-9610(99)80061-0. [DOI] [PubMed] [Google Scholar]