Abstract
INTRODUCTION
All NHS-suspected cancers should be seen within 2 weeks of referral and are referred under government guidelines (Health Service Circular 205; HSC 205). This policy will be subject to review in 2009. Review is vital to allow the appropriate detection of malignancy without overburdening the premium clinic slots with the healthy.
PATIENTS AND METHODS
A total of 170 consecutive patients were referred from January–June 2005. Referral details, patient information, events and time to diagnosis were recorded.
RESULTS
Of these 170 patients, 143 were suitable for analysis. Forty-three patients (30%) were referred with frank haematuria, of whom 30% had bladder cancer. Nine percent of patients (n = 13) had microscopic haematuria none of whom had cancer. A quarter of the patients (n = 35) were referred with suspected testis cancer but none had cancer. Forty-one patients were referred with serum prostate-specific antigen (PSA) elevation; 18 cancers were detected in this group. Ten men had PSA values greater than 50 ng/ml. Only two cancers were suitable for radical prostatectomy. No cancer was found in patients less than 50 years of age.
CONCLUSIONS
A high cancer incidence was found (27.9%), the majority of which was bladder cancer or advanced prostate cancer. Out of the 143 patients, no malignancy was diagnosed in any patient less than 50 years of age, no malignancy was diagnosed in any of the microscopic haematuria group and there was no cancer diagnosed in the group of patients referred with scrotal swellings. We suggest that some guidelines are leading to referral of patients with low cancer risk. When the HSC 205 is revised in 2009, we hope studies such as ours are taken into consideration in order to improve resource utilisation.
Keywords: ‘2-week wait’ rule, Cancer targets, PSA, Macroscopic haematuria, Testicular mass, Cancer incidence
In contemporary NHS practice, all urology departments are under considerable pressure to comply with the UK Government's implementation of the ‘2-week wait’ rule for suspected cancer referrals. All patients with symptoms or signs of suspected cancer are guaranteed to see a hospital doctor within 2 weeks of their general practitioner (GP) requesting an urgent appointment.1
The guidelines for urgent cancer referrals were implemented to facilitate the appropriate referral from primary to secondary care for patients whom the GP suspected may have cancer.2 Patients whose symptoms fulfil the UK Department of Health criteria should be referred using dedicated forms faxed for urgent assessment.
At the time of introducing the guidelines, there was no clear evidence concerning their effectiveness, in particular their diagnostic yield.3 The original guidance has recently been up-dated and further refinement is due next year. The up-dated Referral Guidelines for Suspected Cancer were published by the Department of Health in 2005. The new guidelines resulted from research and audit undertaken since the publication of the previous guidelines.4
In 2005, new targets were inaugurated, initially outlined in the NHS Cancer Plan 2000. A 31-day maximum wait from decision to treat to the start of treatment along side a 62 day maximum wait from urgent referral by GP to start of treatment of all cancers was imposed.
Most studies, to date, of Health Service Circular 205 (HSC 205) have focused on the appropriateness of the guidelines, the compliance of referrals with stated guidelines, and the poor yield of those urgent referrals, but none have suggested specific refinements. The aim of this study was to evaluate the 2-week wait rule for referral of urological cancer, identify methods to improve referral from the hospital perspective, and suggest possible refinements to the guidelines. This was achieved by examining the outcomes of those patients referred under the ‘2-week wait’ rule, identification of the workload burden, highlighting problems meeting targets and suggesting solutions.
Patients and Methods
This was a retrospective study, examining all patient referrals for suspected urological cancers referred by GPs under the ‘2-week wait’ rule received by Stepping Hill Hospital, Stockport in the 6-month period between January 2005 and June 2005. Referrals were identified from both faxed ‘2-week wait’ rule proformas and standard GP referral letters, based on the HSC 205 guidelines (Table 1).
Table 1.
Guidelines for urgent referral for suspected urological cancer
|
Referral details, patient information and events to diagnosis were recorded. Data collected from the referral letters included age, sex, symptoms and signs, and data from case notes included days from referral to review, investigations performed and number of days to diagnosis.
Results
A total of 170 referrals were received from GPs between January 2005 and June 2005. Four referrals were directed to the wrong speciality (two mis-directed from the central hospital booking service, two through the use of wrong HCS 205 proforma) so were unsuitable for analysis. Four patients did not attend their appointments and, therefore, were also excluded. There were 19 sets of case notes unavailable. A total of 143 referrals were, therefore, suitable for analysis; of these, 112 were received on ‘2-week wait’ rule faxed proformas and 31 were typed letters triaged by the GP as the ‘2-week wait’ rule patient. There were 123 males and 20 females with a mean age of 61 years (range, 17–92 years). All patients were reviewed between 1 and 21 days from referral (average, 9.9 days) with four patients breaching the ‘2-week wait’ rule being reviewed on days 15, 16, 20 and 21 (2.8%).
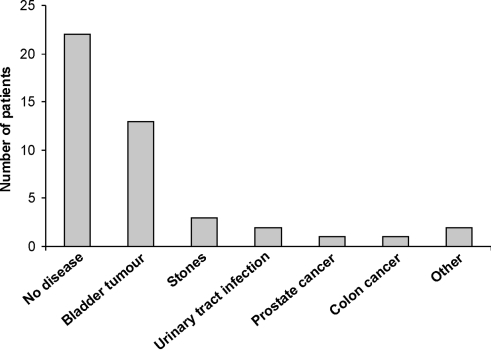
Frank haematuria
Of the referrals, 30% (n = 43) presented with frank haematuria. The average number of days from referral to review was 9.6 days (range, 3–21 days) and the average number of days to diagnosis was 49 days (range, 6–350 days). Of these 43 patients, 39 were reviewed in the haematuria clinic, which, as in most urology departments, has been normal practice and pre-dates the UK Government's cancer plan. At the one-stop haematuria clinic, patients undergo a full history and examination, routine bloods test (FBC, urea and electrolytes), urine dipstick, MSSU and cytology, renal ultrasonography, KUB X-ray and a flexible cystoscopy. Frank haematuria patients with normal investigation or the diagnosis of TCC also subsequently undergo IVU. Four patients were reviewed in consultant out-patient clinics, as no haematuria appointment slot was available within 2 weeks, thus preventing the target from being breached. These four patients were all later assessed in the haematuria clinic within 21 days of referral; none of these four patients were subsequently found to have cancer. Figure 1 shows the distribution of pathologies associated with frank haematuria.
Figure 1.
Diagnostic outcome for patients presenting with frank haematuria. ‘Other’ includes complex renal cyst and hydrocoele.
Microscopic haematuria
Thirteen patients (9% of all referrals) were referred with microscopic haematuria alone; the average number of days to review was 10.8 days (range, 5–14 days), average time to diagnosis was 42 days (range, 8–101 days) and mean age of patients was 56.8 years (range, 40–82 years), compared with 68.4 years for those with frank haematuria. Only one patient was under 50 years of age; she was noted to be a smoker and, therefore, fulfilled the ‘2-week wait’ rule criteria by virtue of being a high-risk patient. Therefore, all 13 patients referred with microscopic haematuria were referred appropriately. Six patients were seen in consultant-led out-patient clinics, six in the haematuria clinic and one was seen as an in-patient. These patients underwent full history and clinical examination, routine blood and urine testing (FBC, urea and electrolytes), KUB X-ray, renal tract ultrasonography and flexible cystoscopy. No cancer was identified in the microscopic haematuria group and one patient was diagnosed with detrusor overactivity syndrome and referred for further management.
Suspected testicular cancer
A quarter of all referrals (n = 35) were referred as suspected testicular cancer. All these patients were seen in the consultant-led clinic in an average of 9.8 days; one patient was seen on day 16 and, therefore, breached the 2-week target. No testicular cancers were detected in these patients. A high proportion of those referred as suspected testicular cancer were diagnosed as simple epididymal pathology (n = 16) or normal testicles (n = 10). Around half of referrals with suspected testicular cancer were referred for testicular ultrasonography (42.8%;n = 15) and 57.2% (n = 20) were discharged from the clinic after the first visit following normal thorough clinical examination by a consultant.
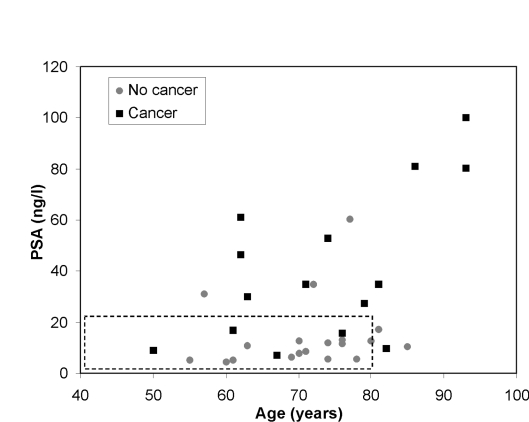
Prostate-specific antigen (PSA)
Of the patients, 28.7% (n = 41) were referred with an elevated age-specific PSA. All were reviewed in a consultant-led out-patient clinic in a mean of 10.1 days (only one patient breached the ‘2-week wait’ rule undergoing review on day 20 from referral). Ten patients were referred with a PSA value greater than 50 ng/ml with four commenced on hormone manipulation without biopsy (patient A – 93 years, PSA 80.4 ng/ml; patient B – 88 years, PSA 208 ng/ml; patient C – 63 years, PSA > 1000 ng/ml; patient D – 93 years, PSA 100.2 ng/ml). Figure 2 shows the relationship between PSA and age in those patients referred. In Figure 2, the hashed box demonstrates that only four of those patients diagnosed with prostate cancer would fall into a category of localised/locally-advanced prostate cancer (with respect to age and PSA only) with possible life expectancy of greater than 10 years and, therefore, would possibly be suitable for potentially curative radical treatment.5–7
Figure 2.
Patients referred under ‘2-week wait’ rule criteria for suspected prostate cancer with a PSA less than 120 ng/l compared to their age. The hashed box illustrates those patients with likely localised/locally advanced disease and a possible life expectancy of greater than 10 years, therefore potential candidates for curative treatment.5–7
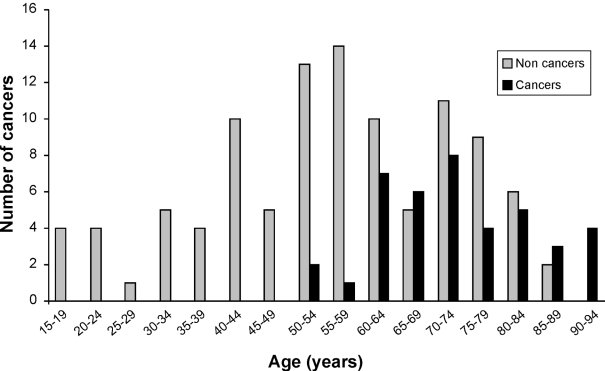
Cancer
Of all patients referred in this 6-month period, 27.9% (40 of 143 referrals) were ultimately diagnosed with cancer (21 prostate cancers, 13 bladder cancers, 1 renal cancer, no testis cancers, 2 penile cancers, 2 bowel cancers and 1 cancer of the clitoris). No cancers were diagnosed in the under 50-year-olds. Three patients (7.5% of patients diagnosed with cancer) were in the age group of 50–59 years, while 22 patients (55%) were in the age group of 60–74 and 15 patients (37.5%) in the age group of 75–92 years (Fig. 3).
Figure 3.
Distribution of number of patients with respect to age and diagnosis of cancer or no cancer in all patients referred under the ‘2-week wait’ rule at Stepping Hill Hospital January 2005 to June 2005 (n = 143).
Discussion
The ‘2-week wait’ rule was initially implemented to guarantee that a suspected cancer patient is seen and fully diagnosed within the shortest possible time, as it is assumed that early diagnosis must offer a better chance of cure. The rule also allows early re-assurance and reduction of distress for many patients evaluated in this ‘fast-track’ manner. Patients prefer to leave the surgery knowing that they have a hospital appointment within 2 weeks.8
We have identified patients who are undergoing unnecessary clinic visits in order only to comply with the ‘2-week wait’ rule. These patients need to be spread over clinics which are often fully booked for a number of weeks into the future. BAUS guidelines suggest that a trainee and consultant should see 10 new and 15 follow-up patients per clinic. Are we as British urologists able to follow such guidance in the light of ever increasing set targets (notably the review of all new patients within 4 weeks) without a significant change in working patterns or increase in manpower? This burden may be reduced with the introduction of a core urology consultant who, as opposed to the specialist urological surgeon, will spend a greater proportion of time with diagnostics; whether this alone will ease the burden is yet to be demonstrated.
Out of all the 143 patients referred over the study period only 40 patients (27.9%) were diagnosed with cancer. A quarter of all referrals were found to have cancer, which if quoted gives the impression that the ‘2-week wait’ rule allows the fast detection of cancer. However, patients with metastatic prostate cancer, bladder cancer, penile cancer and incidentally detected renal cancer were probably not subject to long delays prior to the Government's targets.
In our study, of the 35 patients referred with suspected testicular cancer, none were identified, although our department diagnosed and treated men with testicular cancer in the same time period. This negative yield may reflect our failure, as secondary care, to educate our GP colleagues in the diagnosis of testicular cancer. As a result, we have identified this as a topic for regular GP meetings arranged by our consultants in primary care. However, the confident negative diagnosis of testicular cancer requires a high level of experience in testicular examination or ultrasound diagnosis. Local agreements between radiology, primary care and urology departments are required to agree whether the GP or the urologist are the principal referrer for testicular ultrasonography. It is our practice for a urologist to see these patients as they are equipped to manage other pathologies in a way which ultrasonography does not address. There is currently no ultrasound-based screening programme for testicular cancer; therefore, the authors believe an ultrasound rate of 42.8% is appropriate.
Microscopic haematuria accounted for around 9% of our patients and none had malignant conditions. This raises a question of the clinical significance of such a sign in urgent referral. This concurs with Allen et al.,9 who evaluated the urgent ‘2-week wait’ rule referrals in their department over 12 months with 20 patients referred with microscopic haematuria; again, none had cancer. Therefore, it may be reasonable to suggest removal of microscopic haematuria from the urgent referral guidelines but continue to review those patients in a routine manner. In our study, we have no evidence that microscopic haematuria included as part of a collection of symptoms changes its diagnostic yield; for example, five patients were referred with both lower uri-nary tract symptoms (LUTS) and microscopic haematuria, none of which had cancer (although the number is small).
No cancer was discovered in patients under 50 years of age, which coincides with the fact that cancer is predominantly a disease of ageing with over 50% of common solid tumours being diagnosed in patients over 70 years.10 Figure 3 demonstrates the distribution of urological cancers detected under the ‘2-week wait’ rule. This finding questions whether the criteria should be age-related and not generalised to all age groups, although suspected testicular cancer and frank haematuria would need to be excluded if suggesting a cut-off of 50 years for referral, as our data would advocate.
Urgent assessment and treatment of metastatic prostate cancer does reduce morbidity.11 Evidence exists that active surveillance is appropriate and safe for many patients.6,7 The presence of probable metastatic prostate cancer does require urgent treatment (or diagnosis) as the aim in these men is the timely prevention of complications of the disease. Hormonal manipulation decreases complications but not overall survival in patients with advanced prostate cancer.11 Prostate cancer is unique in that only 17% of men diagnosed with it will die from the disease. Other than in the case of symptomatic disease (i.e. men at risk of cord compression, ureteric obstruction or acute urinary retention), it can be argued that a short delay in diagnosis and treatment has no effect on outcome.12 With proper counselling and education (which may simply just involve written information with regard to the significance of an elevated PSA) there is no reason that anxiety over suspected diagnosis could not be alleviated. This would, of course, require validation.
The HSC 205 guidelines are designed to identify those patients who may have urological malignancy and were originally set at such a level to identify those patients with treatable malignancies but not to overwhelm the system with inappropriate cases. Reviewing our results, we think that the current guidelines do not achieve this. This conclusion was also reached by Khawaja et al.13 and Williams et al.14 demonstrating that a significant number of referrals are inappropriate or non-urgent with resultant overburdening of the service. With the current UK Government targets of the 31 and 62 days a reality, with no extra resources can we operate with the current set of criteria that we suggest are leading the referral of some patients with low risk of significant urological cancers?
Conclusions
The ‘2-week wait’ rule for suspected cancer has its drawbacks and the criteria need refinement (which hopefully will be achieved with the review of criteria in 2009). Never-the-less, the ‘2-week wait’ rule remains a valuable service to the urologist, GPs and their patients. Microscopic haematuria could be removed, and with the exclusion of suspected testicular cancers and frank haematuria, 2-week referrals should be only for the over 50-year-olds. We do not recommend ultrasound screening for testicular cancer but have highlighted the responsibility of secondary care in the education of primary care physicians in clinical examination. The introduction of the new style core urologist may help alleviate the burden of diagnosis, but is yet to be established. Alternatively, a dedicated ‘2-week wait’ rule clinic that could be rotated between consultants on a weekly basis may prevent over booking of regular out-patient clinics thus removing burden.
The greatest strength of the ‘2-week wait’ rule for suspected cancer is probably in allaying the fears of those presenting with frank haematuria, a scrotal lump or an elevated PSA level who do not, in fact, have cancer. Better education of patients and GPs and other strategies may be able to add re-assurance. With the current demands on the NHS, treatment of disease must surely take priority over that of re-assuring the worried (and, in some cases, iatrogenically worried) well.
Acknowledgments
Amr M Hawary and Hazel E Warburton contributed equally to this work.
References
- 1.NHS Executive. The New NHS modern and dependable; a national framework for assessing performance. London: Department of Health; 1998. [Google Scholar]
- 2.Department of Health. The NHS cancer plan. London: Department of Health; 2000. [Google Scholar]
- 3.Jones R, Rubin G, Hungin P. Is the two week rule for cancer referrals working? BMJ. 2001;322:1555–6. doi: 10.1136/bmj.322.7302.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute for Health and Clinical Excellence. Referral Guidelines for Suspected Cancer. London: NICE; 2005. Clinical Guideline 27. [Google Scholar]
- 5.European Association of Urology. Guidelines on prostate cancer. Update March 2007.
- 6.Klotz LH. Active surveillance with selective delayed intervention using PSA doubling time for good risk prostate cancer. Eur Urol. 2005;47:16–21. doi: 10.1016/j.eururo.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Hardie C, Parker C, Norman A, Eeles R, Horwich A, Huddart R, et al. Early outcomes of active surveillance for localized prostate cancer. BJU Int. 2005;95:956–60. doi: 10.1111/j.1464-410X.2005.05446.x. [DOI] [PubMed] [Google Scholar]
- 8.Avon Health Authority. 2001. Dec,
- 9.Allen D, Popert R, O'Brien T. The two-week-wait cancer initiative in urology: useful modernization? J R Soc Med. 2004;97:279–81. doi: 10.1258/jrsm.97.6.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fentiman IS, Tirelli U, Monfardini S, Schneider M, Festen J, Cognetti F, et al. Cancer in the elderly; why so badly treated? Lancet. 1990;335:1020–2. doi: 10.1016/0140-6736(90)91075-l. [DOI] [PubMed] [Google Scholar]
- 11.The Medical Research Council Prostate Cancer Working Party Investigators Group. Immediate versus deferred treatment for advanced prostatic cancer: initial results of the Medical Research Council Trial. BJU Int. 1997;79:235–46. doi: 10.1046/j.1464-410x.1997.d01-6840.x. [DOI] [PubMed] [Google Scholar]
- 12.Albertson PC, Hanley JA, Fine J. 20-Year outcomes following conservative management of clinically localized prostate cancer. JAMA. 2005;293:2095–101. doi: 10.1001/jama.293.17.2095. [DOI] [PubMed] [Google Scholar]
- 13.Khawaja AR, Allan SM. Audit of referral practice to fast-access breast clinic before the guaranteed two-week wait. Ann R Coll Surg Engl. 2001;83:58–60. [PMC free article] [PubMed] [Google Scholar]
- 14.Williams RW, Hughes W, Felmingham S, Irvine GH. An audit of two week wait referrals for head and neck cancer. Ann R Coll Surg Engl. 2002;84:304–6. [Google Scholar]