Abstract
Objective
To explore use-inequity in maternal health-care services in home-based skilled-birth-attendant (SBA) programme areas in Bangladesh.
Methods
Data from a community survey, conducted from February to May 2006, were analysed to examine inequities in use of SBAs, caesarean sections for deliveries and postnatal care services according to key socioeconomic factors.
Findings
Of 2164 deliveries, 35% had an SBA, 22.8% were in health facilities and 10.8% were by caesarean section. Rates of uptake of antenatal and postnatal care were 93% and 28%, respectively. There were substantial use-inequities in maternal health by asset quintiles, distance, and area of residence, and education of both the woman and her husband. However, not all inequities were the same. After adjusting for other determinants, the differences in the use of maternal health-care services for poor and rich people remained substantial [adjusted odds ratio (OR) 2.51 (95% confidence interval, CI: 1.68–3.76) for skilled attendance; OR 2.58 (95% CI: 1.28–5.19) for use of caesarean sections and OR 1.53 (95% CI: 1.05–2.25) for use of postnatal care services]. Complications during pregnancy influenced use of SBAs, caesarean-section delivery and postnatal care services. The number of antenatal care visits was a significant predictor for use of SBAs and postnatal care, but not for caesarean sections.
Conclusion
Use of maternity care services was higher in the study areas than national averages, but a tremendous use-inequity persists. Interventions to overcome financial barriers are recommended to address inequity in maternal health. A greater focus is needed on the implementation and evaluation of maternal-health interventions for poor people.
Résumé
Objectif
Etudier l’inéquité dans le recours aux services de soins maternels dans les zones desservies par des programmes d’assistance à domicile des naissances par du personnel qualifié (SBA) au Bangladesh.
Méthodes
Les données fournies par une enquête en communauté, réalisée de février à mai 2006, ont été analysées pour étudier, en fonction de facteurs socioéconomiques clés, les inéquités dans le recours aux SBA, à une césarienne pour l’accouchement et aux services de soins postnatals.
Résultats
Sur 2164 accouchements, 35% ont bénéficié d’un SBA, 22,8% se sont déroulés dans un établissement de soins et 10,8% se sont effectués par césarienne. Les taux d’utilisation des soins anténatals et postnatals étaient respectivement de 93 et 28%. Il existait des inéquités sanitaires substantielles entre les mères selon le quintile de richesse, l’éloignement et la zone de résidence et le niveau d’éducation maternel et paternel. Cependant, ces inéquités étaient d’une ampleur variable. Après ajustement pour d’autres déterminants, les écarts entres riches et pauvres pour le recours aux services de soins maternels restaient importants : odds ratio ajusté (OR) = 2,51 (intervalle de confiance à 95%, IC = 1,68-3,76) pour l’assistance par du personnel qualifié à la naissance ; OR = 2,58 (IC à 95% = 1,28-5,19)] pour l’accouchement par césarienne et 0R = 1,53 (IC à 95% = 1,05-2,25 pour les services de soins postnatals. La survenue de complications pendant la grossesse influait sur le recours aux SBA, à l’accouchement par césarienne et aux services de soins postnatals. Le nombre de visites anténatales était un paramètre prédictif important pour le recours aux SBA et aux soins postnatals, mais pas pour le recours à une césarienne.
Conclusion
Les services de soins maternels étaient plus utilisés dans les zones étudiées qu’en moyenne dans le pays. Une très forte inéquité persiste cependant dans le recours à ces soins. Des interventions visant à surmonter les obstacles financiers sont recommandées pour faire face à cette inéquité en matière de santé maternelle. Il faut se concentrer davantage sur la mise en œuvre et l’évaluation des interventions en faveur de la santé maternelle visant des personnes défavorisées.
Resumen
Objetivo
Estudiar la inequidad en el uso de los servicios de atención materna en las zonas con programas de parteras calificadas (PC) de atención domiciliaria en Bangladesh.
Métodos
Se analizaron los datos de una encuesta comunitaria llevada a cabo entre febrero y mayo de 2006 para analizar las inequidades en el uso de las PC, la práctica de cesáreas y los servicios de atención posnatal en función de factores socioeconómicos clave.
Resultados
De un total de 2164 partos, el 35% tuvieron lugar con la asistencia de una PC, el 22,8% se produjeron en establecimientos de salud, y un 10,8% se hicieron mediante cesárea. Las tasas de uso de los servicios de atención prenatal y posnatal fueron del 93% y el 28%, respectivamente. Se observaron inequidades sustanciales en el uso de los servicios de salud materna en función de los quintiles de riqueza, la distancia y la zona de residencia y el nivel de instrucción tanto de la mujer como del cónyuge, pero el grado de inequidad difería. Después de ajustar para otros determinantes, las diferencias de uso de los servicios de atención materna entre las personas ricas y las pobres siguieron siendo sustanciales [razón de posibilidades (OR) ajustada de 2,51 (intervalo de confianza del 95%: 1,68-3,76) para la asistencia por personal cualificado; 2,58 (IC95%: 1,28-5,19) para la práctica de cesáreas, y 1,53 (IC95%: 1,05-2,25) para el uso de servicios de atención posnatal]. Las complicaciones durante el embarazo influyeron en el uso de las PC, el parto por cesárea y los servicios de atención posnatal. El número de visitas de atención prenatal fue un factor predictivo importante de la intervención de PC y del recurso a los servicios de atención posnatal, pero no de las cesáreas.
Conclusión
La utilización de los servicios de maternidad en las zonas estudiadas fue mayor que la media nacional, pero sigue habiendo grandes inequidades en lo tocante al uso de esos servicios. Se recomienda emprender intervenciones para superar los obstáculos económicos y corregir las inequidades en salud materna, y hay que hacer más hincapié en la aplicación y evaluación de las intervenciones de salud materna en la población pobre.
ملخص
الەدف
تحرى الجور في استخدام خدمات رعاية صحة الأمومة في المناطق المطَّبق فيەا برامج المولدات المنزليات الحاذقات، في بنغلاديش.
الطريقة
حلل الباحثون المعطيات المستمدة من مسح مجتمعي أجري في المدة من شباط/فبراير إلى أيار/مايو 2006، بغرض دراسة مظاەر الجور في استخدام خدمات المولدات المنزليات الحاذقات، والجراحات القيصرية في الولادات، وخدمات الرعاية التالية للولادة، وفقاً لعدد من العوامل الاجتماعية والاقتصادية الأساسية.
الموجودات
من بين 2164 ولادة، جرت 35% منەا على يد مولدات منزليات حاذقات، و22.8% في مرافق صحية، و10.8% بجراحات قيصرية. وبلغت معدلات الانتفاع بخدمات رعاية ما قبل الولادة 93%، والرعاية التالية للولادة 28%. وكان ەناك جور كبير في الانتفاع بخدمات رعاية صحة الأمومة، وذلك بحسب الشرائح المئوية للانتفاع، والمسافة، ومنطقة الإقامة، ومستوى تعليم المرأة وزوجەا. إلا أن جميع مظاەر الجور لم تكن ەي نفسەا في كل الأحوال. وبعد إجراء التصحيحات الخاصة بالمحدِّدات الأخرى، ظلت الفروق في الانتفاع بخدمات رعاية صحة الأمومة كبيرة بين الفقراء والأغنياء [نسبة الاحتمال المصححة 2.51 (95% فاصلة الثقة 1.68 – 3.76) للمولدات الحاذقات؛ نسبة الاحتمال 2.58 (95% فاصلة الثقة 1.28 – 5.19) لاستخدام الجراحات القيصرية، نسبة الاحتمال 1.53 (95% فاصلة الثقة 1.05 – 2.25) للانتفاع بخدمات الرعاية التالية للولادة]. وكان للمضاعفات أثناء الحمل تأثير على استخدام خدمات المولدات المنزليات الحاذقات، والولادة بالجراحة القيصرية، والانتفاع بخدمات الرعاية التالية للولادة. وكان عدد الزيارات لتلقِّي رعاية ما قبل الولادة عامل تنبؤ يعتد بە إحصائياً بشأن الانتفاع بخدمات المولدات المنزليات الحاذقات، والرعاية التالية للولادة، إلا أنە لم يكن كذلك بالنسبة للجراحات القيصرية.
الاستنتاج
لقد كان الانتفاع بخدمات رعاية صحة الأمومة أعلى في مناطق الدراسة منە في متوسط المعدلات الوطنية، إلا أن جوراً ەائلاً في استخدام ەذە الخدمات ما يزال موجوداً. ويُنصح بإجراء تدخلات للتغلُّب على الحواجز المالية من أجل التصدِّي لمظاەر الجور في مجال صحة الأمومة، كما أن ەنالك حاجة للتـركيز بشكل أكبر على تنفيذ وتقيـيم التدخلات الخاصة بصحة الأمومة بالنسبة للفقراء.
Introduction
Bangladesh is committed to achieving the Millennium Development Goal 5 (MDG5) that specifies a 75% reduction in the maternal mortality ratio between 1990 and 2015.1 The global community has selected the proportion of deliveries with a skilled birth attendant (SBA) as an indicator to monitor progress in the achievement of MDG5.2,3 Programmes implemented in Bangladesh to reduce maternal mortality have followed the evolving strategies of the Safe Motherhood Initiative.4 Since the early 1990s, the emphasis had been on improving the provision of emergency obstetric care.5–7 More recently, the Government determined that efforts to decentralize emergency obstetric care must continue but be complemented by a home-based SBA strategy.8 Private-sector efforts are also increasing. But the key question is whether there has been a corresponding increase in uptake of these services by women across all socioeconomic strata of Bangladeshi society.
Inequity in health refers to inequalities that are unjust according to social-justice theories.9 Inequities in maternal death and access to maternal services exist everywhere, both between and within countries.10,11 Increasing the supply of quality services seems important but not sufficient to improve access.12–14
The objective of this research is to explore inequities in utilization of skilled attendance at birth, delivery by caesarean sections and use of postnatal care services, by key socioeconomic factors in two home-based SBA areas of Bangladesh to provide insights for future programming.
Materials and methods
Study settings
The Bangladesh Association of Voluntary Sterilization (BAVS) implemented a home-based SBA programme between 1992 and 1997 in all rural unions of Chandpur Sadar Upazila about 60 km south and south-east of Dhaka, the capital of Bangladesh. Local community women with 5–10 years of schooling were trained for 6 months in midwifery, including hands-on birthing experience, to do safe home-deliveries and provide antenatal and postnatal care services in their respective communities.
The Nongovernmental Organization (NGO) Service Delivery Project (NSDP), in collaboration with its partner NGOs, initiated a home-based SBA programme in 10 different rural and periurban areas of the country with its existing nurses or midwives (nurses are trained for 4 years and family-welfare visitors for 18 months) in May 2005. During inception, all selected nurses or midwives received 1 week refresher training on evidence-based maternal and newborn health-care techniques.
In February to May 2006, the International Centre for Diarrhoeal Disease, Bangladesh (ICDDR, B) evaluated these two home-based SBA programmes for their functionality, use and sustainability. As part of the evaluation, cross-sectional community surveys were done in both BAVS and NSDP home-based SBA areas among women who had given birth in the previous 12 months (excluding abortions or miscarriages). We present findings from the cross-sectional surveys.
Study sample, data collection and analysis
For field-data collection, self-weighted cluster sampling was used. Selection of clusters was with equal probability and a take-all strategy was followed at the second stage. A list of primary sampling units was generated after reviewing the population distribution of mouzas (a revenue village with a jurisdiction list number) in each study area (BAVS and NSDP). To reduce the workload, mouzas with populations of more than 2000 people were divided into segments with each segment consisting of about 1000 people. Each segment was considered a primary sampling unit. In each study area, an exhaustive list of primary sampling units was generated with the help of local NGO managers. Sixty primary sampling units were then selected randomly from both NSDP and BAVS areas.
For sample-size calculation, we used 9.4% as the prevalence of skilled attendance in rural and periurban areas, and 2% as precision, and a design effect of 1.2 for two stages in the sample selection technique.
Twelve trained interviewers collected data by use of a structured questionnaire. The questionnaire gathered information on background, use of antenatal care, use of SBA, use of postnatal care, perceived quality of care and cost of services. Field supervisors and study investigators closely supervised field activities; 5% of cases were re-interviewed to ensure a high degree of quality of data. In total, 2164 women were interviewed, which was slightly higher than the estimated minimum sample size of 2000. The non-response rate was 0%.
Wealth was measured in terms of asset quintiles with the pooled household-level data following principal components and factor analysis methods.15,16 Other variables used to measure inequity were distance to nearest government hospital (5 km or less or more than 5 km), area of residence (urban or rural), and educational status of both women and their husbands (none, 1–4 years, 5–9 years, and ≥ 10 years of schooling), and religion (Muslim or Hindu and other). Antenatal care was measured in number of visits to any provider whether formal or informal. Outcome measures focused on whether an SBA (doctor, nurse or midwife, excluding trained or untrained traditional birth attendant) was present at delivery, whether caesarean section was used, or whether any postnatal care was received. Home-based attendants with 6 months or 18 months midwifery training in the BAVS study and the NSDP study, respectively, were considered SBAs in this study.
To look for determinants of using these services, multivariate logistic regression models were used to calculate crude and adjusted odds ratios. In multilogistic regression models, the independent variables included asset quintile, education of the woman and her husband, distance to nearest government hospital, religion, number of antenatal care visits, and reported complication status during pregnancy or delivery. Area of residence was excluded from the multivariate model due to the high degree of colinearity with distance to government hospital. The age and parity of women were used as control variables.
Results
Sociodemographic characteristics
Most respondents were Muslims (94.5%) and housewives (95.2%). Average household size was 6.3 people, and monthly household expenditure about US$ 90. More than 80% of households had sanitary latrines, but only 33% had televisions, 26.8% had mobile phones, and 61% had electricity. At least 1 year of schooling had been completed by 80.2% of respondents, while the rate was 72.6% among their husbands. The average distance between home and the nearest government hospital was 6.2 km. Of the respondents, 15% were less than 20 years old while 4.2% were more than 35 years old. About 35% were in their first pregnancy and 10% of women had had five or more pregnancies.
Use patterns of maternal health-care services
In our study areas, 35% of deliveries were attended by SBAs: 22.8% at health facilities and 12.4% at home. Of the 22.8% facility-deliveries, 12.9% took place at private facilities, 9.1% in government facilities, while only 0.8% were in NGO facilities. About two-thirds of all deliveries took place at home with unskilled birth attendants.
Caesarean sections were performed on 10.8% of the study population, while 93% and 28% had at least one antenatal and postnatal care visit respectively. Of all caesarean deliveries, 73% took place at private facilities, 3% in NGO facilities, and the remaining 24% were in government facilities. For those who received antenatal care, the mean number of visits was 4.38, and 50% had four or more visits. Mean gestational age was 16.9 weeks and 30.2 weeks for the first and last antenatal-care visits respectively. Among those who received antenatal care, 32% had their last visit at government facilities, 16% at NGO clinics, 24.5% at private facilities, and the remaining 27.5% were at home. By type of service providers, 32.5% received their last antenatal-care visit from qualified physicians, 36% from NGO paramedics (including home-based SBAs), 25.4% from government paramedics, and 6.1% from informal providers (including TBAs and village doctors). Of those who received postnatal care, their mean number of visits was 1.8. Only 5.5% of mothers received postnatal care within 48 h and 14% within 1 week after giving birth.
Inequities in use of maternal health-care services
There were substantial inequities in the use of SBAs by asset quintile, education, area of residence, and distance to hospital. Use of skilled attendance was 15.6% among mothers from the poorest quintile households and 63.3% for mothers from the richest quintile households. Similarly the skilled attendance rate was 18.2% and 74.3% among mothers with no education and with higher education (≥ 10 years schooling) respectively. Use of SBAs was higher among those living in urban areas than among those in rural areas (42.8% versus 32%). Distance to the nearest government hospital had a negative influence on delivery by an SBA (41% of women living within 5 km of a government hospital gave birth with an SBA compared with 28% of women living more than 5 km from a facility). Use of skilled attendance was higher among other religious groups (mostly Hindus) than among Muslims (61.3% versus 33.6% respectively).
Antenatal care visits increased use of SBAs at birth: only 7.6% of those with no antenatal care visit used SBAs, while nearly 50% of mothers with four or more visits did so. Skilled attendance at birth was 48% among mothers who reported at least one complication during pregnancy or the delivery period compared with 23% among those who did not.
Among women from the poorest quintile households, 3.3% had caesarean sections, whereas 28.4% of mothers from the richest quintile did so. Similarly, use of caesarean section was significantly higher among mothers with higher education, from urban areas, those who lived within 5 km of government hospitals, and who were not Muslim. In the bivariate analysis, the uptake of caesarean section was also significantly higher among those who reported complications and received more antenatal care visits (Table 1).
Table 1. Determinants for use of SBAs, caesarean-section delivery, and use of postnatal care service.
| Predictors | N 2164 | SBA at delivery |
Delivery by caesarean section |
Received postnatal care |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % used | Univariate model OR (95% CI) | Multivariate modela OR (95% CI) | % used | Univariate model OR (95% CI) | Multivariate modela OR (95% CI) | % used | Univariate model OR (95% CI) | Multivariate Modela OR (95% CI) | ||||
| Women’s education | ||||||||||||
| None | 428 | 18.2 | 1.00 | 1.00 | 4.0 | 1.00 | 1.00 | 22.7 | 1.00 | 1.00 | ||
| 1–4 years | 378 | 20.9 | 1.19 (0.84–1.68) | 0.95 (0.65–1.41) | 2.4 | 0.59 (0.26–1.34) | 0.47 (0.20–1.13) | 30.4 | 1.49 (1.09–2.05) | 1.25 (0.89–1.76) | ||
| 5–9 years | 1 066 | 36.2 | 2.55 (1.93–3.35) | 1.35 (0.96–1.92) | 9.8 | 2.64 (1.56–2.47) | 1.24 (0.65–2.37) | 26.0 | 1.19 (0.92–1.55) | 0.90 (0.65–1.24) | ||
| ≥ 10 years | 292 | 74.3 | 12.98 (9.06–18.60) | 2.69 (1.66–4.38) | 34.9 | 12.98 (7.55–22.31) | 1.98 (0.93–4.26) | 43.0 | 2.52 (1.82–3.48) | 1.19 (0.75–1.87) | ||
| Asset quintile | ||||||||||||
| Lowest | 423 | 15.6 | 1.00 | 1.00 | 3.3 | 1.00 | 1.00 | 22.2 | 1.00 | 1.00 | ||
| Second | 442 | 23.1 | 1.62 (1.15–2.29) | 1.47 (1.01–2.13) | 2.9 | 0.86 (0.41–1.91) | 0.63 (0.28–1.41) | 27.1 | 1.30 (0.96–1.78) | 1.24 (0.89–1.72) | ||
| Middle | 433 | 28.6 | 2.17 (1.55–3.03) | 1.51 (1.03–2.19) | 5.3 | 1.64 (0.83–3.23) | 0.88 (0.42–1.86) | 24.2 | 1.12 (0.82–1.54) | 0.97 (0.69–1.37) | ||
| Fourth | 433 | 44.8 | 4.39 (3.18–6.07) | 2.32 (1.60–3.39) | 13.9 | 4.70 (2.58–8.55) | 1.76 (0.89–3.50) | 29.0 | 1.45 (1.04–1.94) | 1.16 (0.81–1.65) | ||
| Highest | 433 | 63.3 | 9.32 (6.71–12.93) | 2.89 (1.91–4.38) | 28.4 | 11.59 (6.54–20.54) | 2.64 (1.30–5.37) | 39.0 | 2.22 (1.64–3.00) | 1.54 (1.05–2.25) | ||
| Husband’s education | ||||||||||||
| None | 592 | 18.9 | 1.00 | 1.00 | 3.5 | 1.00 | 1.00 | 23.0 | 1.00 | 1.00 | ||
| 1–4 years | 311 | 21.5 | 1.18 (0.84–1.65) | 1.01 (0.69–1.47) | 2.6 | 0.72 (0.31–1.64) | 0.71 (0.30–1.70) | 30.0 | 1.42 (1.04–1.94) | 1.38 (0.99–1.92) | ||
| 5–9 years | 782 | 34.5 | 2.26 (1.76–2.91) | 1.22 (0.90–1.66) | 9.1 | 2.72 (1.65–4.47) | 1.31 (0.73–2.37) | 26.0 | 1.18 (0.92–1.51) | 1.06 (0.79–1.42) | ||
| ≥ 10 years | 479 | 64.9 | 7.93 (6.01–10.48) | 2.25 (1.54–3.28) | 27.8 | 10.45 (6.47–16.88) | 2.01 (1.04–3.87) | 38.2 | 2.09 (1.60–2.73) | 1.32 (0.90–1.92) | ||
| Distance to hospital | ||||||||||||
| 0–5 km | 1 104 | 41.8 | 1.00 | 1.00 | 14.3 | 1.00 | 1.00 | 28.5 | 1.00 | 1.00 | ||
| > 5 km | 1 160 | 28.2 | 0.55 (0.46–0.66) | 0.66 (0.53–0.82) | 7.1 | 0.46 (0.34–0.61) | 0.79 (0.56–1.09) | 28.2 | 0.99 (0.81–1.20) | 1.21 (0.98–1.50) | ||
| Reported complication(s) | ||||||||||||
| No | 1 123 | 23.2 | 1.00 | 1.00 | 3.7 | 1.00 | 1.00 | 21.0 | 1.00 | 1.00 | ||
| Yes | 1 041 | 48.0 | 3.07 (2.55–3.69) | 2.40 (1.94–2.97) | 18.3 | 5.78 (4.09–8.17) | 4.12 (2.84–5.98) | 36.1 | 2.13 (1.76–2.57) | 1.75 (1.43–2.15) | ||
| Religion | ||||||||||||
| Muslim | 2045 | 33.6 | 1.00 | 1.00 | 9.8 | 1.00 | 1.00 | 28.1 | 1.00 | 1.00 | ||
| Other | 119 | 61.3 | 3.14 (2.15–4.59) | 2.05 (1.31–3.19) | 27.7 | 3.54 (2.31–5.43) | 2.05 (1.22–3.43) | 31.1 | 1.15 (0.77–1.72) | 0.87 (0.57–1.33) | ||
| Number ANC visit | ||||||||||||
| No visit | 157 | 7.6 | 1.00 | 1.00 | 0.6 | 1.00 | 1.00 | 14.6 | 1.00 | 1.00 | ||
| 1 visit | 231 | 15.6 | 2.23 (1.12–4.44) | 1.70 (0.83–3.48) | 4.8 | 7.78 (1.00–60.71) | 5.00 (0.63–39.98) | 17.7 | 1.26 (0.72–2.19) | 1.26 (0.71–2.23) | ||
| 2 visits | 340 | 24.4 | 3.90 (2.06–7.39) | 2.37 (1.22–4.61) | 4.4 | 7.18 (0.94–54.70) | 2.94 (0.37–23.05) | 20.3 | 1.48 (0.89–2.48) | 1.38 (0.81–2.34) | ||
| 3 visits | 353 | 31.2 | 5.47 (2.91–10.27) | 2.86 (1.48–5.53) | 7.6 | 12.88 (1.74–95.42) | 4.38 (0.57–33.58) | 22.9 | 1.73 (1.04–2.88) | 1.62 (0.96–2.74) | ||
| ≥ 4 visits | 1 083 | 47.9 | 11.12 (6.10–20.27) | 3.82 (2.03–7.19) | 16.5 | 30.80 (4.30–220.88) | 5.30 (0.71–39.47) | 36.7 | 3.38 (2.14–5.36) | 2.74 (1.68–4.47) | ||
ANC, antenatal care; CI, confidence interval; OR, odds ratio; SBA, skilled birth attendant. a Controlled for all covariates in the model and age and parity of mothers.
Use of postnatal care services varied by asset quintiles, education of parents, and number of antenatal care visits, but not by distance to health facility or religion. The uptake of postnatal care services was greater in rural areas (30.1%) than in urban areas (23.2%).
In multilogistic regressions, all seven independent variables were significant predictors for use of SBAs. The best predictor for use of SBAs was the education level of the woman, followed by (strength of association) reported complication status, wealth quintile, number of antenatal care visits, distance to nearest government facility, education of the husband and religion. The significant predictors for use of caesarean section deliveries were (by order of strength of association): education of woman, reported complications during pregnancy and delivery, asset quintile, religion, education of husband and distance to nearest government hospital. The influence of the number of antenatal care visits upon delivery by caesarean sections was attenuated and lost its significant association when effects of all covariates were controlled statistically.
Multilogistic regression shows that significant predictors for use of postnatal care services were asset quintile, reported complication status of mothers, and number of antenatal care visits, but not distance, religion, or education of the women or her husband.
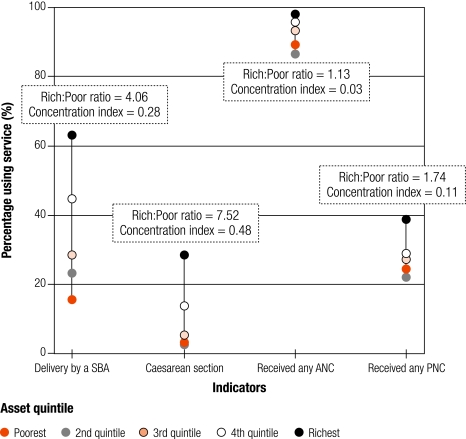
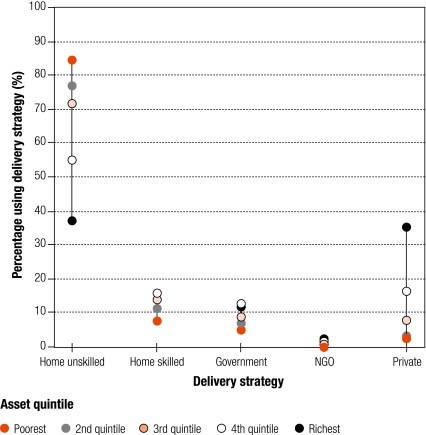
Inequality was highest for delivery by caesarean section (rich:poor ratio = 7.52; concentration index = 0.48; Fig. 1) and lowest for use of any antenatal care services (rich:poor ratio = 1.13; concentration index = 0.03). For delivery by SBA and use of postnatal care services, the rich:poor ratio and concentration index were 4.06 and 0.28, and 1.74 and 0.11, respectively (Fig. 1). Skilled delivery care services from the private sector were used less by poor people than services from government and NGO facilities, or home-based skilled providers. Services from unskilled providers were used most by poor people (Fig. 2).
Fig. 1.
Use-inequity of different maternity care services
ANC, antenatal care; PNC, postnatal care; Rich:Poor ratio, ratio of use by richest to use by poorest; SBA, skilled birth attendant.
Fig. 2.
Use-inequity of skilled attendance from different sectors
Discussion
Achieving the target for MDG5 indicator, in many circumstances, could be accomplished without further improvement in coverage among the poorest people.17 This statement, though not new, is reaffirmed in this study. Even though NGO maternity-care services make up a small proportion of those used by Bangladeshi women, use of maternal health-care services in the home-based NGO areas in Bangladesh is higher than national averages18 (35% versus 13% skilled attendance), and increases with use of antenatal care. However, significant use-inequities persist in these areas and even for the NGO maternity services by asset quintiles, distance to nearest hospital, area of residence, and educational status of both the woman and her husband.
Inequities in the NGO areas were not equal for all indicators: they varied by the type and place of services. Higher-level costlier services were more inequitably distributed (e.g. caesarean sections) than front-line, less-expensive, preventive services (e.g. antenatal care). Facility-based services were less equitably distributed than home-based SBA services. Chowdhury and colleagues reported similar findings in 2006 for ICDDR maternity care services from the Matlab area of Bangladesh where both home and facility-based services were provided free of charge.19
Even after adjusting for other determinants, the poor–rich differentials in the use of all maternal health-care services remained substantial. Poor people used NGO services more than they did government facilities, which in turn they used more than services from private-sector facilities. The private-sector services naturally preclude use by poor people because patients have to pay for them. With the increasing relative contribution to skilled attendance and caesarean-section deliveries of the private sector, use-inequities are likely to be aggravated. Why services from public facilities are used less by poor people than services from NGO facilities, however, is not clear, as government services are provided free of charge. One reason may be that public sector services, though officially free, actually are not. Often people have to pay unofficially for services.20 Other possibilities are that NGO services reach out to poor people, or that poor people view the care more favourably.
Addressing inequities in maternal health should be viewed as a central policy goal together with achievement of MDG5 targets. How can this be done? Free services, whether from government or from NGOs, do not necessarily reach the poorest. There is a need to adopt strategies for poor people to establish equity in terms of access to, and use of, maternal health-care services. To safeguard the interest of poor people, direct interventions are needed. Many demand-side financing schemes have been proposed globally. Interventions recently tried include: improved means of identifying poor individuals (Columbia and Mexico), cash payments for use of services (Mexico), services provided by NGOs working under contracts with carefully specified performance indicators (Cambodia), mass campaigns (Ghana and Zambia), and social marketing (United Republic of Tanzania).21 But the effectiveness of such interventions has not been adequately assessed in different contexts. Recently the Government of Bangladesh in collaboration with the World Bank and WHO has initiated a “demand-side financing maternal health voucher scheme” for poor mothers in 21 subdistricts of Bangladesh. Under this scheme poor mothers are identified by local committees on the basis of certain set criteria and provided with vouchers to buy maternal health-care services (including treatment for obstetric complications) from different preselected providers or facilities in the area.
The challenges in implementing and scaling up such programmes in a resource-poor setting are substantial. We recommend intense monitoring of the process of implementation of the voucher programme during further scaling up to capitalize on lessons learnt for the benefit of the poor. Other financing strategies, such as contracting out services to NGOs that support people, might also make maternal health-care services equitable and efficient. Monitoring and evaluation of ongoing government projects and programmes, such as the community-based SBA programme are also important. We recommend further research to understand what the poorest women see as the main factors that limit access to care, such as cost and quality of care.
Beyond economic equity, our study supports the view that a home-based SBA strategy can increase coverage. Outreach by SBAs is likely to initiate the transition from home births with traditional attendants to use of skilled care at facilities22 especially where women prefer home deliveries23 or where the woman’s mobility is constrained. However, birthing in home conditions can be extremely basic24,25 and issues of adequate coverage by SBAs, safety of the SBAs, privacy and hygiene are paramount. Home birthing without adequate links and transport to emergency obstetric care is also likely to limit the effectiveness of the strategy. There are also doubts about efficiency and sustainability of a home-based SBA strategy in the long-term.26
The strongest predictor for use of both SBAs and caesarean sections was education of the women. Similar findings have been reported from other developing countries.27,28 Non-health interventions to improve the health of women should prioritize female education. In Bangladesh, there were major efforts and significant changes in female education between 1991 and 2004: the proportion of women with no formal education decreased from 56.5% to 35.8%.29
Another factor that increases the likelihood that the women will use skilled attendance at deliveries and postnatal care is increased use of antenatal care. Strengthening demand and quality of antenatal care so that all women get four visits from a competent provider as suggested by WHO would also be useful.
In our study area, population-based caesarean-section rates are within the 5–15% range suggested by WHO and the United Nations Children’s Fund (UNICEF), but the indications for caesarean section seem to be more socioeconomic than medical as most caesarean sections took place in private-sector facilities and were used mainly by well-off families. This finding raises questions about the validity of caesarean section as a proxy for the maternal mortality ratio. There is a need to investigate indications for caesarean sections to understand whether these costly surgeries are done to save lives or make money.
Conclusion
In striving to achieve MDG5, the reduction of socioeconomic inequities in maternal health should be viewed as a central policy and programme goal. Greater focus is now needed on implementation and evaluation of interventions that are efficient and that benefit the poor, such as the ongoing community-based SBA programme and the demand-side voucher scheme for maternal health. There is a need to strengthen antenatal care as recommended by WHO for improving access to skilled attendance at delivery. Other efforts to address costs and financing are an obvious need as is further strengthening of ongoing female education initiatives. ■
Acknowledgements
This research study was funded by USAID, Dhaka (Grant No. GR 00089). ICDDR, B acknowledges with gratitude the commitment of USAID, Dhaka, to the Centre’s research efforts. We acknowledge the contributions from the programme managers and field personnel of BAVS and NSDP and its partner NGOs. We thank Allisyn C Moran (scientist, ICDDR, B) for her valuable comments and Shamim Sufia Islam (data management officer, RHU, PHSD, ICDDR, B) for her assistance in data management and editing.
Footnotes
Competing interests: None declared.
References
- 1.UN millennium development goals. New York: United Nations; 2006. Available from: http://www.un.org/millenniumgoals/ [Accessed on 12 February 2008].
- 2.Ronsmans C, Campbell O, McDermott J, Koblinsky M. Questioning the indicators of need for obstetric care. Bull World Health Organ. 2002;80:317–24. [PMC free article] [PubMed] [Google Scholar]
- 3.Wardlaw T, Maine D. Process indicators for maternal mortality programmes. In: Bercer M, Ravindran TKS, eds. Reproductive health matters Oxford: Blackwell; 1999. pp. 24-30. [Google Scholar]
- 4.Huque ZA, Leppard M, Mavalanker D, Akhter HH, Chowdhury TA. Safe Motherhood Programmes in Bangladesh. In: Berer M, Sundari Ravindran TK, eds. Safe motherhood initiatives: critical issues London: Blackwell Science; 1999. [Google Scholar]
- 5.Gill Z, Ahmed JU. Experience from Bangladesh: implementing emergency obstetric care as part of the reproductive health agenda. Int J Gynaecol Obstet. 2004;85:213–20. doi: 10.1016/j.ijgo.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Islam MT, Hossain MM, Islam MA, Haque YA. Improvement of coverage and utilization of EmOC services in southwestern Bangladesh. Int J Gynaecol Obstet. 2005;91:298–305. doi: 10.1016/j.ijgo.2005.06.029. [discussion 283-4] [DOI] [PubMed] [Google Scholar]
- 7.Islam MT, Haque YA, Waxman R, Bhuiyan AB. Implementation of emergency obstetric care training in Bangladesh: lessons learned. Reprod Health Matters. 2006;14:61–72. doi: 10.1016/S0968-8080(06)27229-X. [DOI] [PubMed] [Google Scholar]
- 8.Murakami I, Egami Y, Jimba M, Wakai S. Training of skilled birth attendants in Bangladesh. Lancet. 2003;362:1940. doi: 10.1016/S0140-6736(03)14983-5. [DOI] [PubMed] [Google Scholar]
- 9.Braveman PA, Gruskin S. Defining equity in health. J Epidemiol Community Health. 2003;57:254–8. doi: 10.1136/jech.57.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kunst AE, Houweling T. A global picture of poor-rich differences in the utilisation of delivery care. Studies in Health Services Organisation and Policy. 2001;17:297–316. [Google Scholar]
- 11.Graham WJ, Fitzmaurice AE, Bell JS, Cairns JA. The familial technique for linking maternal death with poverty. Lancet. 2004;363:23–7. doi: 10.1016/S0140-6736(03)15165-3. [DOI] [PubMed] [Google Scholar]
- 12.Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19:69–79. doi: 10.1093/heapol/czh009. [DOI] [PubMed] [Google Scholar]
- 13.Koblinsky MA, et al. Going to scale with professional skilled care. Lancet. 2006;368:1377–86. doi: 10.1016/S0140-6736(06)69382-3. [DOI] [PubMed] [Google Scholar]
- 14.Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 15.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data — or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 16.Gwatkin DR, Rustein S, Johnson K, Pande RP, Wagstaf A. Measurement of socio-economic status. Socio-economic differences in health, nutrition and population in Bangladesh Washington: HNP/Poverty Thematic Group, World Bank; 2000. [Google Scholar]
- 17.Gwatkin DR. Who would gain most from efforts to reach the Millennium Development Goals for Health? An inquiry into the possibility of progress that fails to reach the poor: HNP discussion paper Washington: World Bank; 2002. [Google Scholar]
- 18.Bangladesh Demographic and Health Survey. 2004. Dhaka and Calverton, MD: National Institute of Population Research and Training, Mitra and Associates, ORC Macro; 2004. Available from: http://www.measuredhs.com/pubs/pub_details.cfm?ID=526&srchTp=type#dfiles [Accessed on 12 February 2008].
- 19.Chowdhury ME, Ronsmans C, Killewo J, Anwar I, Gausia K, Das-Gupta S, et al. Equity in use of home-based or facility-based skilled obstetric care in rural Bangladesh: an observational study. Lancet. 2006;367:327–32. doi: 10.1016/S0140-6736(06)68070-7. [DOI] [PubMed] [Google Scholar]
- 20.Killingsworth JR, Hossain N, Hedrick-Wong Y, Thomas SD, Rahman A, Begum T. Unofficial fees in Bangladesh: price, equity and institutional issues. Health Policy Plan. 1999;14:152–63. doi: 10.1093/heapol/14.2.152. [DOI] [PubMed] [Google Scholar]
- 21.Gwatkin DR, Bhuiya A, Victoria CG. Making health systems more equitable. Lancet. 2004;364:1273–80. doi: 10.1016/S0140-6736(04)17145-6. [DOI] [PubMed] [Google Scholar]
- 22.Koblinsky MA, Campbell O, Heichelheim J. Organizing delivery care: what works for safe motherhood? Bull World Health Organ. 1999;77:399–406. [PMC free article] [PubMed] [Google Scholar]
- 23.Maine D, O’Connor ML. Safe motherhood programmes: Options and issues. New York: Centre for Population and Family Health, Columbia University: 1991. [Google Scholar]
- 24.Walt G, Perera M, Heggenhougen K. Are large-scale volunteer community health worker programmes feasible? The case of Sri Lanka. Soc Sci Med. 1989;29:599–608. doi: 10.1016/0277-9536(89)90179-2. [DOI] [PubMed] [Google Scholar]
- 25.Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–99. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 26.Koblinsky M, Matthews Z, Hussein J, Mavalankar D, Mridha MK, Anwar I, et al. Going to scale with professional skilled care. Lancet. 2006;368:1377–86. doi: 10.1016/S0140-6736(06)69382-3. [DOI] [PubMed] [Google Scholar]
- 27.Ikeako LC, Onah HE, Iloabachie GC. Influence of formal maternal education on the use of formal maternity services in Inagu, Nigeria. J Obstet Gynaecol. 2006;26:30–4. doi: 10.1080/01443610500364004. [DOI] [PubMed] [Google Scholar]
- 28.Mekonnen Y, Mekonnen A. Factors influencing the use of maternal health care services in Ethiopia. J Health Popul Nutr. 2003;21:374–82. [PubMed] [Google Scholar]
- 29.Collin SM, Anwar I, Ronsmans C. A decade of inequality in maternity care: antenatal care, professional attendance at delivery and caesarean section in Bangladesh, 1991-2004. Int J Equity Health. 2007;6:9. doi: 10.1186/1475-9276-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]