Abstract
Background/Objective:
To describe characteristics of recurrent pressure ulcers (PrUs) in veterans with spinal cord injury (SCI).
Design:
Descriptive, cohort study.
Settings and Participants:
Twenty-four veterans with SCI from 6 SCI centers in the Department of Veterans Affairs.
Methods:
Data from a prospective study evaluating PrUs were analyzed for 24 veterans with 29 recurrent PrUs during 9 months. Additional retrospective medical record data were analyzed for 15 veterans who received inpatient treatment.
Results:
Participants were male, 50% non-Hispanic white, with paraplegia (63%), complete SCI (83%), a mean age of 56 years, and mean time since SCI of 21 years. Most PrUs recurred (63%, n = 15 patients) in the same location as the most recent ulcer and at the ischial tuberosities (63%). Mean time to recurrence was 16.6 weeks. PrUs were stage III (28%, n = 8) or IV (45%, n = 13) with undermining (48%), necrotic slough (50%), and minimal exudate. One third were (n = 9) larger than 16 cm2. Mean Bates-Jensen Wound Assessment Tool Score was 33.63. Inpatient medical record data (n = 15) showed 73% with documentation indicating infection treated with antibiotics (53%, n = 8 patients), osteomyelitis (47%, n = 7), and/or cellulitis (13%, n = 2) noted. Plastic surgery consultation was obtained for 67% with surgery as an option for 73% (1 without consultation). Scheduled repositioning was documented for 21%.
Conclusions:
Most PrUs were severe, located at the same anatomic site, and recurred within 4 months, suggesting that the recurrent ulcers were more likely incomplete healing of the initial PrUs. This sample of veterans with SCI provides early data on recurrent PrU characteristics.
Keywords: Pressure ulcers, recurrent; Spinal cord injuries; Paraplegia; Closure, mucocutaneous flap; Wound healing; Veterans; Bates-Jensen Wound Assessment Tool; Salzburg Pressure Ulcer Risk Score
INTRODUCTION
Persons with spinal cord injury (SCI) are at high risk for pressure ulcers (PrUs) throughout their lifetime because of decreased mobility and lack of sensation coupled with other physiologic changes. PrUs impact the quality of life and interfere with initial rehabilitation, educational, and vocational pursuits and community reintegration after SCI. The rate of PrUs in people with SCI is high, with reports of 33% to 40% incidence during acute rehabilitation and a similar prevalence for those living in the community (1–5). High rates of recurrence also have been reported, ranging from 31% to 79% (6,7). Studies of risk factors for PrU recurrence have included (a) patient (eg, demographic, SCI, and clinical characteristics) (5,7–10), (b) disease (comorbid conditions) (8,11), and (c) treatment factors (eg, medical vs surgical healing) (12–15). Recurrence has been associated with sex (male) (10), age (younger) (8,10), ethnicity (African American race) (10), unemployment (13,14), nursing home residence (7,10), and previous PrU surgery (15). Recurrence after previous surgical flap closure for PrUs is important because surgical closure using flaps and reconstructive surgery is often the recommended approach for full-thickness PrUs that develop in persons with SCI. Recurrence after surgical flap closure can describe new ulceration that occurs over the surgical site or new ulceration that occurs at a different location. Recurrence rates of individuals whose ulcers were surgically treated have ranged from 11% to 29% in cases with postoperative complications and 6% to 61% in cases without postoperative complications (13,15–21). Krause and Broderick (15) reported that 13% of their sample of 633 subjects with SCI had 1 or more recurrent PrUs per year. Their study suggested that lifestyle, exercise, and diet were protective mechanisms against PrU recurrence. Chen et al (10) studied the effects of age, period (1994–2002 vs 1984–1993), and SCI duration on PrUs. These investigators found that, although during the first 10 years after SCI, PrU risk was relatively stable, there was a significant trend toward increasing PrU prevalence from 10 to 15 years after injury, possibly because of the effects of the aging process.
Although recurrence rates are significant and data exist on possible risk factors for recurrent PrUs, there is limited information on characteristics of recurrent PrUs in this or other populations such as frail nursing home residents. Furthermore, there is lack of clear terminology and procedures for evaluating and classifying “recurrent” ulcers, especially those that develop in the same anatomic region as a prior PrU. When such an ulcer develops, it could be a manifestation of incomplete healing and remodeling stages of the original ulcer, breakdown within previously healed scar tissue where the prior ulcer was located, or breakdown within adjacent tissue that was unaffected by the initial ulcer. Recurrence can also refer to a patient with a history of ulcers. The term “recurrence” could potentially be applied to all of these possibilities, as well as the development of an ulcer in an anatomic region different from the original ulcer. Additionally, we have no answers to these related questions: How long must a PrU remain healed before breakdown at the same site is termed a new PrU? How should we determine severity of recurrent PrUs? Is superficial partial-thickness skin damage over a previous Stage IV PrU site classified as a Stage II PrU, or because it occurred over a site with previous Stage IV PrU damage is it assessed as a Stage IV PrU? Is any PrU that occurs at the same anatomic site as a previous ulcer a recurrent ulcer? How long is long enough for a PrU to have successfully completed the final stage of healing, wound remodeling? The lack of evidence related to recurrent PrUs coupled with inadequate terminology for health care providers to accurately describe these phenomena has hindered research in this area and clinical care for persons with SCI. Thus, the purpose of this study was to describe characteristics of recurrent PrUs in a small sample of veterans with SCI.
METHODS
Subjects and Setting
We analyzed data from a larger prospective randomized, controlled trial (RCT) of an intervention to prevent PrU recurrence in veterans with SCI (7). The RCT intervention consisted of individualized education and monthly telephone follow-up vs usual care. Subjects were recruited for the larger study from 6 VA SCI centers. Subjects were eligible for the larger study if they met the following inclusion criteria: were more than 1 year posttraumatic SCI, age >18 years, admitted to the hospital with a Stage III/IV pelvic ulcer (hereafter referred to as the initial ulcer), access to a phone, and their initial ulcer was healed at the time of discharge from the hospital. Of the 148 veterans who agreed to participate in the larger study at the time of admission to the hospital for treatment of their PrU, 64 met the inclusion criteria, were randomized, and participated in the larger study. Further information on the methods of the RCT has been reported previously (7). Twenty-four veterans of the 64 (38%) who participated in the larger PrU study developed a recurrent PrU defined as 1 or more Stage II or greater skin breakdown at any pelvic anatomic site during the study 9-month follow-up period. Data are reported here for all patients who reported PrU recurrence as defined above (n = 24) and for a subsample who returned to the enrollment site for treatment of the new skin breakdown (n = 15). The study received approval from all the participating institutional review boards at each VA Medical Center and affiliated universities.
Medical Record Data.
Demographic, clinical, and medical factors as well as SCI characteristics and ulcer history were obtained as part of the larger study through patient interview at baseline. Information on comorbid conditions and initial ulcer characteristics was obtained from electronic medical records and verified by the primary care provider. To examine the recurrent ulcer, 2 sources of data were included: (a) patient self-report to study personnel (eg, date, location, and any treatment received for the recurrence) and clinician evaluation of the recurrent ulcer and (b) for those patients who came back to the original enrollment site for in-patient or home care treatment related to the recurrence, we reviewed their VA electronic medical records using a standardized instrument. Of the 24 patients with recurrences, 12 were rehospitalized at the original SCI Center, 6 were treated at home, 1 was treated at a private sector hospital, 1 died, 1 was unavailable for follow-up, 2 went to other VA hospitals (non-SCI Centers), and 1 patient had multiple sclerosis (not SCI) and was excluded from the trial (mistakenly randomized). Of these, we were able to gather additional medical record data for 15 patients, 12 of whom were rehospitalized at the original SCI center and 3 who were treated at home.
Medical record data were abstracted by a physician and an investigator with a doctorate-level nursing degree. Interrater reliability of the medical record abstraction for each item on the abstraction tool was evaluated with 4 medical records reviewed by both the physician and nurse and resulted in κ statistics ranging from κ = 0.50 (for item “was surgery offered” for which there is no single place in the medical record to find this documented) to κ = 1.00.
Bates-Jensen Wound Assessment Tool Data.
The recurrent PrUs were assessed by trained clinicians using the Bates-Jensen Wound Assessment Tool (BWAT). The BWAT, formerly the Pressure Sore Status Tool (22), assesses 13 wound characteristics, rates each on a scale from 1 (best) to 5 (worst), and can be summed for a total score ranging from 13 to 65, with higher scores indicating more severe tissue damage. Interrater reliability of the BWAT has been reported as r = 0.92 for 2 observers in hospitalized patients (22). Wound characteristics evaluated on the BWAT include size, depth, edges, undermining and tunneling, exudate type and amount, necrotic tissue type and amount, surrounding skin color, peripheral tissue edema and induration, and granulation and epithelial tissue.
Salzburg Pressure Ulcer Risk Assessment Score.
Additional medical record data were available from the larger interventional study and included the Salzburg Pressure Ulcer Risk Score, which was obtained from patient self-report and confirmed by review of the patient's electronic medical record (23). The Salzburg PrU Risk Assessment, an instrument developed for SCI, contains 15 items, with higher scores indicating higher risk (range, 0–15) (24).
We also present data on the characteristics of the initial PrU that healed before entry into the larger study, in addition to the characteristics of the recurrent PrUs. Because the biggest predictor of PrU recurrence in the larger study was African-American race (23), we evaluated data on the recurrent PrUs separately for African-Americans (n = 12) and non-Hispanic whites (n = 12).
Statistical Analysis
Descriptive statistics of central tendency and dispersion were used to describe characteristics of the PrUs. t tests and χ2 statistics were used to compare means and proportions between African-American and non-Hispanic white veterans.
RESULTS
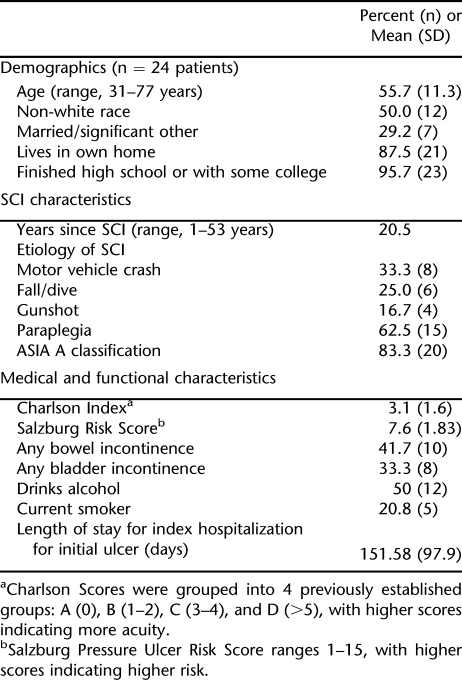
Data for this article were derived from 24 participants with 29 ulcers along with data on hospitalization and treatment from 15 of those participants. Table 1 presents demographic and medical characteristics of the 24 participants on the variables most relevant to this study. The participants were all men, one half were non-Hispanic white, had a mean age of 56 years, had some college education, had a mean of 20 years post-SCI, and were at risk for PrU development as indicated by their Salzburg Pressure Ulcer Risk Score (mean 7.6 ± 2.8 [SD]). Of the 15 participants with hospitalization or treatment medical record data available for review, 12 were African-American, 47% (n = 7) had a diagnosis of diabetes mellitus, 47% (n = 7) had a diagnosis of hypertension, and for all 12 who were hospitalized, management of the PrU was the admitting primary diagnosis.
Table 1.
Characteristics of Participants
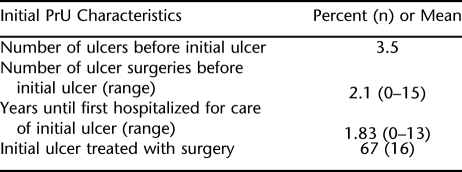
PrU characteristics from the initial hospitalization (before being randomized into the intervention phase of the larger study) are presented in Table 2. The mean number of prior surgeries for any previous ulcers was 2. The recurrence rate among patients with previously healed ulcers who developed new skin breakdown was 38% in the larger study (24 of 64 patients).
Table 2.
Initial Pressure Ulcer Characteristics
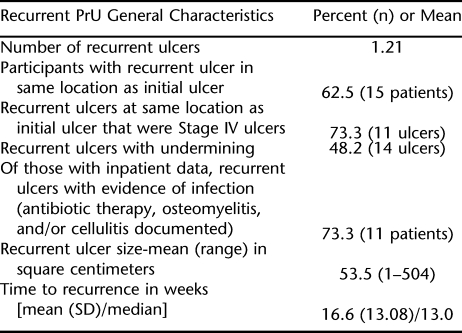
The 24 patients with recurrent ulcers actually presented with 29 PrUs, including participants with 1 PrU (n = 19) and with 2 PrUs (n = 5). Of patients with recurrent PrUs, 63% (n = 15), presented with PrUs that developed over the same anatomic location as the initial ulcer. Of the 5 participants with more than 1 PrU, all had 1 recurrent PrU at the same anatomic location as the initial ulcer and another PrU at a different anatomic location. The majority of all recurrent PrUs developed over the ischium (59%, n = 17 ulcers), with only 24% (n = 7 ulcers) recurring at the sacrum. Of those ulcers that recurred at the same anatomic site, 73% (n = 11 ulcers) were located at the ischium. Two thirds (67%, n = 16 patients) of those with recurrent PrUs had their initial PrU treated with flap surgery for closure, of which 63% (n = 10 patients) experienced recurrent PrUs at the same anatomic site as the surgery was performed. These ulcers recurred quickly, with a median time to recurrence of 13 weeks (Table 3).
Table 3.
Recurrent Pressure Ulcer General Characteristics
The recurrent PrUs of those in our sample were large, full-thickness Stage III (28%, n = 8 ulcers) or Stage IV (45%, n = 13 ulcers) PrUs (Table 3). For those ulcers recurring at the same anatomic site as the prior ulcer, 73% (n = 11) presented as Stage IV ulcers. For the 15 participants with medical record data on inpatient or home care treatment, 73% (n = 11 patients) had documentation indicating PrU infection treated with antibiotic therapy (53%, n = 8 patients), osteomyelitis (47%, n = 7 patients), and/or cellulitis (13%, n = 2 patients).
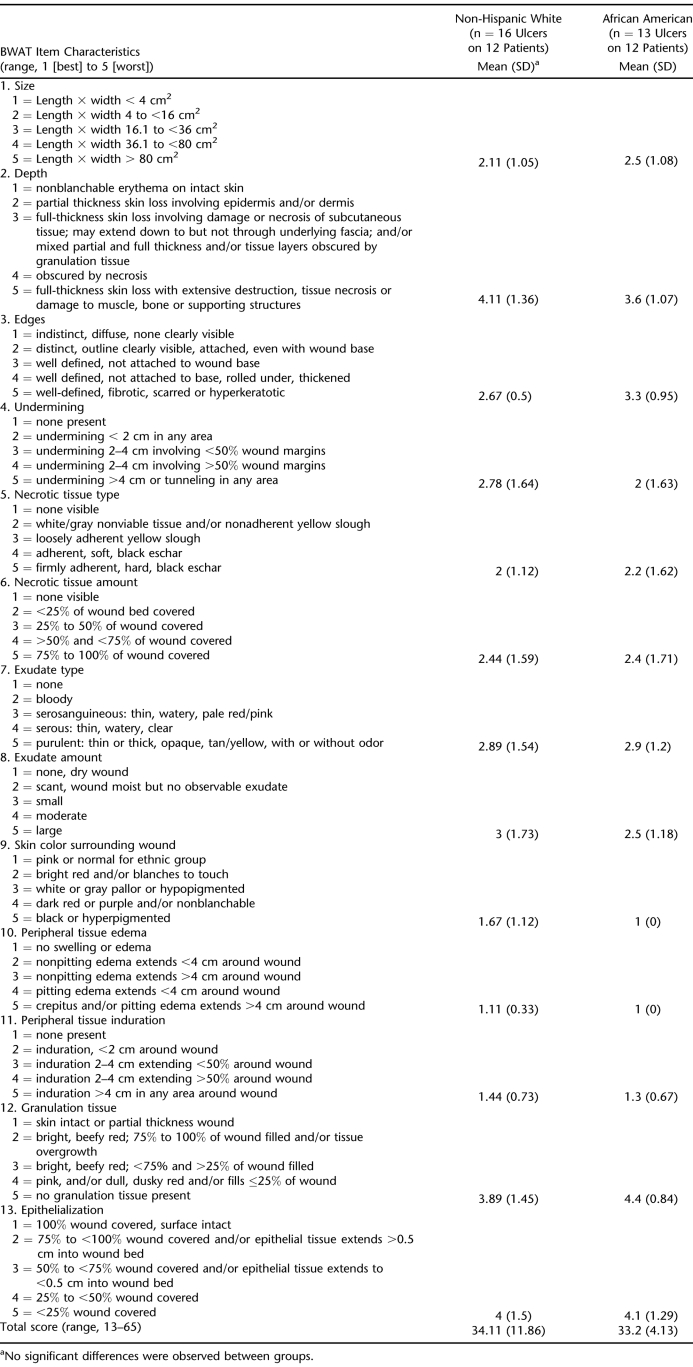
As shown in Table 4, there were no differences in the wound characteristics of recurrent PrUs in African Americans and non-Hispanic whites. The mean BWAT Score was 33.63 (SD = 8.44) for all ulcers, indicating moderately severe ulcers. In general, the recurrent PrUs had minimal to no induration or edema, normal skin color surrounding the wound, and minimal to no epithelialization or granulation tissue. These recurrent PrUs were full-thickness ulcers with scant to small amounts of serosanguineous or serous exudate, 25% to 50% of the wound covered with yellow necrotic slough tissue, and 1 to 4 cm of undermining.
Table 4.
Wound Characteristics of Recurrent Pressure Ulcers
Medical records for the 15 participants who were hospitalized at the original facilities showed that care for the recurrent PrUs was similar to care provided during hospitalization for the initial ulcer (eg, care included plastic surgery consultation, nutrition assessment, and physical therapy involvement). Sixty percent (n = 9 patients) had a plastic surgery consultation noted in the medical record and 67% (n = 10 patients), had medical record documentation of surgery being offered as a treatment option (1 patient had surgery noted as an option with no plastic surgery consultation noted in the medical record). The majority (73%, n = 11 patients) had documentation of nutrition consultation and nutritional laboratory values. Albumin level (n = 9) ranged from 1.4 to 4.0 g/dL, with a mean of 3.07 (SD = 0.88), and of those who had prealbumin values obtained (n = 5), the mean was 16.26 mg/dL (SD = 5.48). Surprisingly, only 20% (n = 3 patients) had medical record documentation of a scheduled repositioning program for bed and chair. Only 2 patients had medical record documentation of frequency of repositioning for pressure relief. Five patients (33%) had documentation of pressure reduction plans for discharge to home. Seventy-three percent (n = 11 patients) had medical record documentation of physical therapy involvement, of which 45% (n = 5 patients) received pressure mapping and 20% (n = 3 patients) received new wheelchair pressure reduction devices during their hospitalization.
DISCUSSION
This article describes the characteristics of recurrent PrUs among veterans with SCI. Recurrent PrUs were severe, with the majority presenting as Stage III or Stage IV PrUs. The duration of the original ulcer for which the patients with recurrences were treated was nearly twice as long as veterans who did not have recurrence (23). In our sample, most of the initial PrUs were treated surgically, and of those, two thirds developed recurrent PrUs at the same site. Most recurrent PrUs occurred at the same site as the initial ulcer and the most common site of recurrence was the ischial tuberosities. That the PrUs recurred at the same anatomic site, were moderate to large full-thickness Stage III or Stage IV PrUs, recurred at the same site in those who underwent surgical repair of the initial ulcer, and recurred quickly (eg, median = 4 months) suggests the recurrent PrUs in this small sample may represent incomplete healing of the initial ulcers that were very deep and often treated with surgery. This is similar to other investigator's findings related to frequency of recurrence at the ischial site and PrU recurrence after surgical repair (16–21).
Information about the development and the recurrence of PrUs comes from both geriatrics and SCI medicine. Kuwahara et al (25) evaluated recurrent PrUs after surgical repair of Stage III or IV sacral PrUs among 16 elderly bedridden patients followed from 1 to 4 years in Japan and showed a 37.5% recurrence rate and an overall mortality rate of 69%. Gusenof et al (26) reviewed the outcome for 22 predominately nonambulatory, nonparaplegic, elderly patients who underwent operative repair of 27 PrUs and were followed for 3 to 24 months. They report a 6-month recurrence rate of 10.5%; however, 50% of the patients experienced surgical complications ranging from wound dehiscence to seroma. These 2 small studies from geriatrics provide minimal evidence regarding PrU recurrence in the frail elderly. The data on PrU recurrence in elders are limited to small evaluations of surgical repair, which leaves a gap in knowledge regarding the rate of PrU recurrence among elders whose PrU is treated conservatively (nonsurgically). There are at least 3 relatively recent studies that to some degree are larger than ours that describe long-term recurrence rates in persons with SCI. Our findings are most similar to the study of Disa et al (19) of PrU recurrence after surgery for PrU closure. Disa et al (19) followed 40 consecutive patients with 68 PrUs after operative repair for a mean of 21 months. They reported a 61% PrU recurrence rate and a 69% patient recurrence rate, with mean time to recurrence of 9.3 months. We report similar PrU recurrence rates but with recurrence occurring much faster (median, 4 months), which may reflect surgical failure; however, our sample also included persons whose ulcers were healed using conservative (nonsurgical) treatment as well. Kierney et al (20), in a retrospective study of 158 persons with SCI, reported much lower PrU recurrence rates (19%) after surgery, with a mean time for follow-up of 3.7 years. The disparity in findings may relate to type of surgical repair or the criteria used for determining whether surgical treatment is indicated. The basic principles of surgical treatment of PrUs have remained unchanged since the 1960s (27), with more recent research that supports the use of myocutaneous flaps in the presence of chronically infected ulcers (28). Factors that have been cited in the plastic surgery literature as key to successful initial flap closure of PrUs include nutrition, treatment of infection, pressure relief, and management of spasticity and contractures (29). Attention has been given to postsurgical bedrest and remobilization protocols to minimize recurrence in the first few weeks after surgery (20,30). However, as discussed by Yamamoto et al (31), muscle used for flaps undergoes significant atrophy and necrosis in response to pressure, and pressure points over bony prominences are normally covered with fasciocutaneous tissue rather than muscle. Thus, a key factor in recurrence rates may be type of surgical repair. Our study was limited in that we did not have information on the type of surgical repair used to treat the initial ulcers; thus, it is difficult to make direct comparisons of recurrence rates related to type of surgical repair.
Late recurrence of ulcers has been attributed to patient factors such as spasticity, pressure relief behavior, or psychosocial factors rather than the design of the surgical flap (19,20,27). Furthermore, some have suggested individual patient differences in daily lifestyle (32) or personal ambivalence about competing priorities or the efficacy of prevention (33) may influence PrU development in community-dwelling persons with SCI. Although our primary premise is that the recurrent PrUs represent incomplete healing of the initial ulcers because of the rapid time to recurrence, these studies provide alternative explanations and suggest that PrU recurrence could be caused by skeletal deformities or postural alignment issues, inappropriate or malfunctioning equipment, or issues related to daily lifestyle. We did not gather data on skeletal deformities, postural alignment issues, or daily lifestyle of participants. All participants received physical therapy consultation, and physical therapy was actively involved in care during hospitalization for the initial ulcer (during the large intervention RCT). We assume that physical therapy involvement would lessen, although not eliminate, the chance that PrU recurrence was caused by inappropriate or malfunctioning equipment. Although inappropriate or malfunctioning equipment is not a likely factor for the PrU recurrences in this study, we cannot rule it out.
Yamamoto et al (31) also found higher recurrence rates for the ischial site (49%) compared with the sacral site (21%), which is similar to our findings of 59% of the recurrent ulcers occurring at the ischium compared with only 24% recurring at the sacral site. This finding is intuitive in this population because the ischial sites are subjected to the greatest pressure when in the seated position (34), and persons with SCI spend significant amounts of time in a wheelchair. Not all persons with SCI perform pressure-relief weight shifts in a timely, consistent manner (35). Attention to posture, seating, and equipment are key elements to PrU prevention among persons with SCI because of the significant amount of time persons with SCI spend in a wheelchair, yet there are limited data on prevention of recurrent PrUs with interventions in these areas. Future work evaluating PrU recurrence should include attention to body alignment, equipment, skeletal deformities, daily lifestyle, and personal health beliefs about PrU prevention. This type of global view may be useful in identifying effective interventions in these areas.
Care provided in the hospital for the recurrent ulcers was similar to care received for the initial ulcers, with no evidence of new interventions (eg, interventions not offered for the initial PrU). The majority received a plastic surgery consultation, were offered surgery as a treatment option, had physical therapy involvement, and received dietary consultation/treatment. Surprisingly, less than one third had medical record documentation of a scheduled repositioning program for bed and wheelchair, and only 2 patients had medical record documentation of frequency of repositioning while in the hospital. It is possible the medical record did not reflect actual care delivery, making our data an underrepresentation of implementation of repositioning programs. However, others have shown that medical record documentation related to repositioning actions in nursing home settings is inaccurate and overestimates actual care delivery for persons (36), raising questions about medical record accuracy for this type of treatment.
Limitations of this study include the small sample size, the inability to follow the recurrent ulcers until they healed, and the use of potentially incomplete retrospective medical record data. Even with these limitations, this study provides important initial data on characteristics of recurrent PrUs, providing a preliminary base for communicating more effectively about recurrent PrUs.
CONCLUSION
We make the following suggestions for future research and clinical practice. First, there is a need for additional clarity in terminology and definitions. The National Pressure Ulcer Advisory Panel (NPUAP) (37) recommends specific PrU staging definitions and against back-staging or reverse staging; however, it has not addressed how to assess the severity of recurrences. Currently, small breaks in the skin along the scar line of a surgically healed Stage IV ulcer would be classified the same way as an ulcer that is several centimeters in diameter or that goes down deep to the bone. This study showed that reliable terminology for classifying recurrent ulcers is lacking, as is a reliable way to describe and assess severity of recurrences.
We further suggest that the term “recurrent PrU” be defined as ulceration at any stage that occurs at the same anatomic site as the initial ulcer within 12 months from time of complete closure of the initial ulcer. Within this period during which wound remodeling occurs, these recurrent PrUs should be considered failure of the initial ulcer to progress through the wound remodeling stage of healing regardless of whether the initial ulcer was surgically repaired or allowed to heal by secondary intention. In our study, using this definition of recurrent PrU, we had a 63% recurrence rate. Although this approach does not allow determination of the etiology of the failure (ie, surgical failure, poor patient management, inappropriate sitting time), it will provide initial guidance on how to approach new skin breakdown in persons with prior PrUs.
We further suggest researchers and clinicians conduct root cause analyses to gather and document more specific information related to the cause of the breakdown and characteristics of the recurrent PrU including: whether or not the recurrent ulcer location is at the initial ulcer's surgical incision site for those undergoing surgical repair, whether or not the recurrent PrU location is adjacent to the initial PrU site in tissues that were near/next to but not involved with the initial ulcer, and/or whether or not the recurrent PrU is located within the initial PrU scar tissue. Assessment of recurrences should include specific wound characteristics (eg, location, located at the same anatomic site, presence of deep tissue injury, type and amount of necrotic tissue and exudate, surrounding tissue characteristics, and presence or absence of undermining, epithelialization, and granulation tissue). Only by consistently and accurately defining, documenting, and describing recurrent PrUs can we better understand how best to intervene to prevent PrU recurrence and work to improve PrU outcomes.
Acknowledgments
We acknowledge the contributions of Barry Goldstein, MD, PhD, and Susan Garber, MA, OT, in the development of this project.
Footnotes
Funding for this project was provided by the Department of Veterans Affairs, Investigator Initiated Research program (IIR 01-151).
This paper presents the findings and conclusions of the authors; it does not necessarily represent the Department of Veterans Affairs or the Health Services Research and Development Service.
REFERENCES
- Mawson AR, Biundo JJ, Neville P, et al. Risk factors for early occurring pressure ulcers following spinal cord injury Am J Phys Med Rehabil. 198867 (3) 123–127. [DOI] [PubMed] [Google Scholar]
- Young JS, Burns PE. Pressure sores and the spinal cord injured. SCI Digest. 1981;3:9–25. [Google Scholar]
- Young JS, Burns PE. Pressure sores and the spinal cord injured, Part II. SCI Digest. 1981;3:1–48. [Google Scholar]
- Chen D, Apple DF, Hudson MF, Bode R.Medical complications during acute rehabilitation following spinal cord injury Arch Phys Med Rehabil. 199980 (11) 1397–1401. [DOI] [PubMed] [Google Scholar]
- Fuhrer MJ, Garber SL, Rintala DH, et al. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors Arch Phys Med Rehabil. 199374 (11) 1172–1177. [PubMed] [Google Scholar]
- Niazi ZB, Salzberg CA, Byrne DW, Viehbeck M.Recurrence of initial pressure ulcer in persons with spinal cord injuries Adv Wound Care. 199710 (3) 38–42. [PubMed] [Google Scholar]
- Guihan ML, Garber SL, Bombardier CH, Durazo-Arvizu R, Goldstein B, Holmes SA.Lessons learned in conducting a trial to prevent pressure ulcers in veterans with spinal cord injury Arch Phys Med Rehabil. 200788 (7) 858–861. [DOI] [PubMed] [Google Scholar]
- Niazi ZB, Salzberg CA, Byrne DW, Viehbeck M.Recurrence of initial pressure ulcer in persons with spinal cord injuries Adv Wound Care. 199710 (3) 38–42. [PubMed] [Google Scholar]
- Vidal J, Sarrias M.An analysis of the diverse factors concerned with the development of pressure sores in spinal cord injured patients Paraplegia. 199129 (4) 261–267. [DOI] [PubMed] [Google Scholar]
- Chen Y, DeVivo MJ, Jackson AB.Pressure ulcer prevalence in people with spinal cord injury: period-duration effects Arch Phys Med Rehabil. 200586 (6) 1208–1213. [DOI] [PubMed] [Google Scholar]
- Salzberg CA, Byrne DW, Cayten CG, et al. Predicting and preventing pressure ulcers in adults with paralysis Adv Wound Care. 199811 (5) 237–246. [PubMed] [Google Scholar]
- Raghavan P, Raza WA, Ahmed YS. Prevalence of pressure sores in a community sample of spinal injury patients. Clin Rehabil. 2003;17:879–884. doi: 10.1191/0269215503cr692oa. [DOI] [PubMed] [Google Scholar]
- Krause JS, Vines CL, Farley TL, et al. An exploratory study of pressure ulcers after spinal cord injury: relationship to protective behaviors and risk factors Arch Phys Med Rehabil. 200182 (1) 107–113. [DOI] [PubMed] [Google Scholar]
- Schryvers OI, Stranc MF, Nance PW.Surgical treatment of pressure ulcers: 20-year experience Arch Phys Med Rehabil. 200081 (12) 1556–1562. [DOI] [PubMed] [Google Scholar]
- Krause JS, Broderick L.Patterns of recurrent pressure ulcers after spinal cord injury: identification of risk and protective factors 5 or more years after onset Arch Phys Med Rehabil. 200485 (8) 1257–1264. [DOI] [PubMed] [Google Scholar]
- Holmes SA, Rintala D, Garber SL, Friedman JD.Prevention of recurrent pressure ulcers after myocutaneous flap J Spinal Cord Med. 200225 (suppl 1) S23 [Google Scholar]
- Goodman CM, Cohen V, Armenta A, Thornby J, Netscher DT.Evaluation of results and treatment variables for pressure ulcers in 48 veteran spinal cord-injured patients Ann Plast Surg. 199943 (5) 572–574. [DOI] [PubMed] [Google Scholar]
- Yasenchak PA, Lynch KB, Bridle MJ, Wegener ST. Annual Meeting of the American Spinal Injury Association. Orlando, FL: May, 1990. Variables related to severe pressure sore recurrence. [Abstract] [Google Scholar]
- Disa JJ, Carlton JM, Goldberg NH.Efficacy of operative cure in pressure sore patients Plast Reconstr Surg. 199289 (2) 272–278. [DOI] [PubMed] [Google Scholar]
- Kierney PC, Engrav LH, Isik FF, et al. Results of 268 pressure sores in 158 patients managed jointly by plastic surgery and rehabilitation medicine Plast Reconstr Surg. 1998102 (3) 765–772. [DOI] [PubMed] [Google Scholar]
- Sorensen JL, Jorgensen B, Gottrup F.Surgical treatment of pressure ulcers Am J Surg. 2004188 (suppl) 42S–51S. [DOI] [PubMed] [Google Scholar]
- Bates-Jensen BM, Vredevoe DL, Brecht ML.Measurement of pressure sore status Decubitus. 19925 (6) 20–28. [PubMed] [Google Scholar]
- Guihan ML, Garber SL, Bombardier CH, et al. Predictors of pressure ulcer recurrence in veterans with spinal cord injury J Spinal Cord Med. 200831 (5) 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzberg CA, Byrne DW, Cayten CG, van Niewerburgh P, Murphy JG, Viehbeck M.A new pressure ulcer risk assessment scale for individuals with spinal cord injury Am J Phys Med Rehabil. 199675 (2) 96–104. [DOI] [PubMed] [Google Scholar]
- Kuwahara M, Tada H, Mashiba K, et al. Mortality and recurrence rate after pressure ulcer operation for elderly long-term bedridden patients Ann Plast Surg. 200554 (6) 629–632. [DOI] [PubMed] [Google Scholar]
- Gusenoff JA, Redett RJ, Nahabedian MY.Outcomes for surgical coverage of pressure sores in nonambulatory, nonparaplegic, elderly patients Ann Plast Surg. 200248 (6) 633–640. [DOI] [PubMed] [Google Scholar]
- Griffith BH, Schultz RC. The prevention and surgical treatment of recurrent decubitus ulcers in patients with paraplegia. Plast Reconstr Surg. 1961;27:248–260. doi: 10.1097/00006534-196103000-00002. [DOI] [PubMed] [Google Scholar]
- Mathes SJ, Feng LJ, Hunt TK.Coverage of the infected wound Ann Surg. 1981198 (4) 420–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer J, Phillips LG.MOC-PS CME article: pressure sores Plast Reconstr Surg. 2008121 (Suppl 1) 1–10. [DOI] [PubMed] [Google Scholar]
- Rogers J, Wilson LF.Preventing recurrent tissue breakdown after pressure sore closure Plast Reconstr Surg. 197556 (4) 419–422. [DOI] [PubMed] [Google Scholar]
- Yamamoto Y, Tsutsumida A, Murazumi M, Sugihara T.Long-term outcome of pressure sores treated with flap coverage Plast Reconstr Surg. 1997100 (5) 1212–1217. [DOI] [PubMed] [Google Scholar]
- Clark FA, Jackson JM, Scott MD, et al. Data-based models of how pressure ulcers develop in daily-living contexts of adults with spinal cord injury Arch Phys Med Rehabil. 200687 (11) 1516–1525. [DOI] [PubMed] [Google Scholar]
- King RB, Porter SL, Vertiz KB.Preventive skin care beliefs of people with spinal cord injury Rehabil Nurs. 200833 (4) 154–162. [DOI] [PubMed] [Google Scholar]
- Consortium for Spinal Cord Medicine. Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals J Spinal Cord Med. 200124 (suppl) S40–S101. [DOI] [PubMed] [Google Scholar]
- Olshansky K.Re: Evaluation of results and treatment variables for pressure ulcers in 48 veteran spinal cord-injured patients Ann Plast Surg. 199943 (5) 572–574. [DOI] [PubMed] [Google Scholar]
- Bates-Jensen BM, Cadogan M, Osterweil D, et al. The Minimum Data Set pressure ulcer indicator: does it reflect differences in care processes related to pressure ulcer prevention and treatment in nursing homes J Am Geriatr Soc. 200351 (9) 1203–1212. [DOI] [PubMed] [Google Scholar]
- National Pressure Ulcer Advisory Panel (NPUAP). NPUAP staging report. Available at: http://www.npuap.org/positn6.html. Accessed May 29, 2008.