Abstract
Background
The requirement that patients give up curative treatment makes hospice enrollment unappealing for some patients, and may particularly limit use among African American patients.
Objectives
To determine whether African-American patients with cancer are more likely than white patients are to have preferences for cancer treatment that exclude them from hospice, and whether they are less likely to want specific hospice services.
Methods
283 patients receiving treatment for cancer at six oncology clinics within the University of Pennsylvania Cancer Network completed conjoint interviews measuring their perceived need for five hospice services and their preferences for continuing cancer treatment. Patients were followed for six months or until death.
Results
African American patients had stronger preferences for continuing their cancer treatments on a 7-point scale even after adjusting for age, sex, finances, education, ECOG performance status, quality of life, and physical and psychological symptom burden (adjusted means 4.75 vs. 3.96; β coefficient 0.82; 95% confidence interval 0.22-1.41; p=0.007). African-American patients also had greater perceived needs for hospice services after adjusting for these characteristics (adjusted means 2.31 vs. 1.83) (β coefficient 0.51; 95% confidence interval 0.11-0.92; p=0.01). However, this effect disappeared after adjusting for household finances.
Conclusions
Hospice eligibility criteria may exclude African-American patients disproportionately despite greater perceived needs for hospice services in this population. The mechanisms driving this health disparity likely include both cultural differences and economic characteristics, and consideration should be given to redesigning hospice eligibility criteria.
Patients with cancer have substantial needs for care throughout the course of illness, from diagnosis through the end of life.1-8 Hospice offers a comprehensive program of services designed to meet these needs, including a visiting nurse, respite care, a chaplain, a home health aide, and a counselor. Approximately 500,000 patients with cancer enroll in hospice every year, and evidence indicates that hospice enrollment is associated with improved patient and family outcomes and higher satisfaction with care.9-14
African-American patients are less likely than white patients to utilize hospice.15-17 Although these disparities are well-described, it is not known why they exist. It is possible that African Americans delay or avoid hospice enrollment because of the requirement that they forgo curative treatment.18 This criterion forces patients to make a “terrible choice” between continued treatment and hospice services,19-21 a choice widely believed to obstruct timely hospice use.22-25 The criterion has been part of the Medicare Hospice Benefit since its creation 25 years ago, and since almost all hospice are Medicare-certified, they follow Medicare eligibility criteria for all patients regardless of age or insurance. This barrier may be particularly significant for African-Americans, who are more likely than whites to want various life-prolonging interventions.26-29 However, it is not known if they also have more aggressive cancer treatment preferences, and if such preferences help explain the disparity in hospice utilization.
An alternative explanation for the under-utilization of hospice among African Americans is that they might be less likely to want the services that hospice provides. No studies have evaluated this possibility either. Although some studies suggest that African Americans have less favorable attitudes towards hospice,30-34 their perceived needs for hospice services have not been described.
It is important to determine why these disparities in hospice enrollment exist.35, 36 If they are the result of aggressive treatment preferences among African Americans, then lower rates of hospice utilization are arguably unfair, and represent a real disparity in care that could be eliminated by redesigning hospice eligibility criteria. On the other hand, if African Americans are less likely to want hospice services, then changes to the benefit are not necessary, and, instead, modifications to the services offered may be warranted. Therefore, the goal of this study was to define and compare preferences for cancer treatment and perceived needs for hospice services among African American and white patients.
Methods
Setting and sample
We conducted this study in a population of patients with cancer because cancer is the most common hospice admitting diagnosis (approximately 50%).37 Patients with cancer were recruited over 18 months from six oncology clinics within the University of Pennsylvania Comprehensive Cancer Center Network. Patients were eligible if they had clinical or radiological evidence of active cancer, were receiving chemotherapy or radiation therapy, and had a life expectancy of six months or less if they were to discontinue cancer-directed treatment, according to their oncologist. These patients met the prognostic eligibility criterion for hospice, which requires that patients have a prognosis of six months or less if their disease runs its usual course (e.g. without treatment).18 Nursing staff at each clinic assisted a rotating team of three interviewers to identify and approach eligible patients. This study was approved by the Institutional Review Boards of participating sites.
Data Collection
After providing informed consent, patients completed separate structured interviews using Tablet PCs. First, they provided demographic data, including self-described race, age, marital status, and household finances (e.g. money available at the end of the month).38 In addition, patients completed the Global Distress Index of the Memorial Symptom Assessment Scale,39 the Functional Assessment of Cancer Therapy-General,40 the Medical Outcomes Survey Social Support Scale,41, a single-item global rating of health,42 the Eastern Cooperative Oncology Group performance status scale (ECOG-PS)43, 44 and an assessment of Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs).45, 46
Patients' perceived needs for hospice services were assessed using a conjoint interview, which refers to a process by which subjects are asked to make choices among goods or services by considering several attributes jointly.47 One advantage of this approach over direct ratings is that the value of each service is determined while considering other services, revealing preferences in a more naturalized setting rather than eliciting them one by one. Second, whereas direct rating tasks often suffer from ceiling effects, in conjoint tasks subjects must choose those services that are most important.
For these interviews, we used Sawtooth Software's Adaptive Conjoint Analysis package (ACA for Windows, version 4.0, Sawtooth Software, Sequim, Washington). Adaptive Conjoint Analysis is a hybrid48-50 method of conjoint analysis that uses an interactive self-administered computer program to decrease respondent burden, while preserving the psychometric advantages of conjoint techniques. Like classic conjoint methods, hybrid conjoint methods like ACA determine the importance that subjects place on various services by examining the choices that they make between pairs of services. In addition, though, hybrid methods also use subjects' direct ratings of the importance of those services, which substantially reduces the number of choices that each person is required to make. Although they were developed for use in marketing,47 conjoint techniques and hybrid modifications have been used increasingly to study health-related preferences.51-58 Their validity, reliability, and predictive power are well-established.59, 60
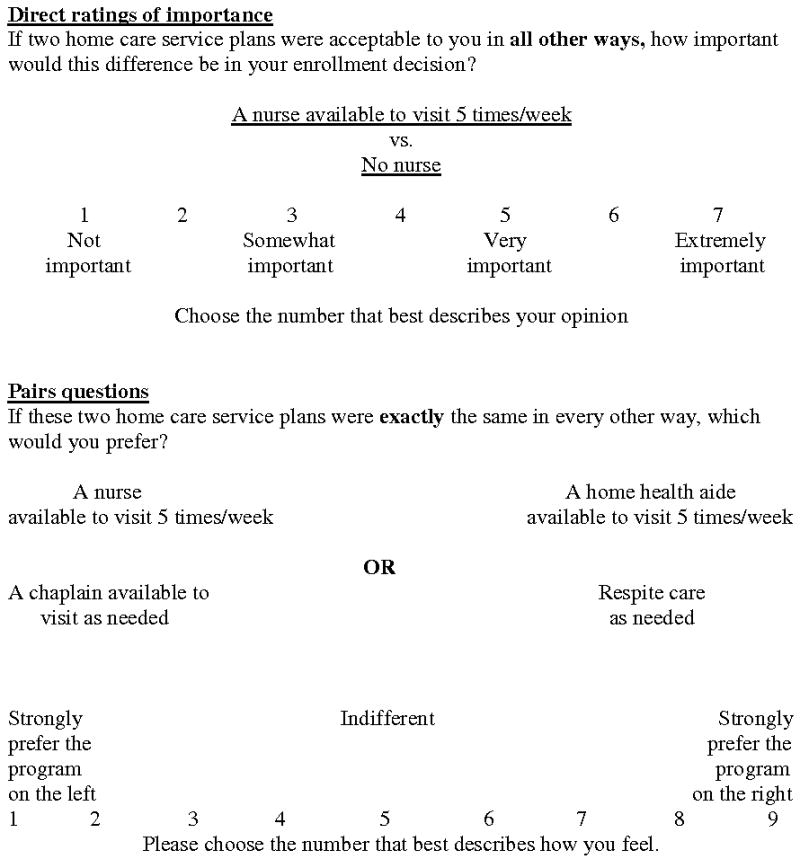
Patients reviewed a brochure describing five of the hospice services that are required by Medicare: a visiting nurse, a chaplain, a home health aide, a counselor, and respite care.18 (Figure 1) These services were selected based on previous studies that found they are among the most valuable to patients.61-63 The subsequent interview used abbreviated (4-6 word) descriptions of each service, and patients kept the brochure open for rapid reference. To assess patients' perceived needs for each service, they were asked to consider how much each service would help them if it were offered at that time. (Figure 2.) First, they rated the importance of each service on a scale from 1 (“Not at all important”) to 7 (“Extremely important”). Second, they evaluated pairs of programs presented side-by-side, each containing two or three services, and rated their preference on a 1-9 scale (“1-Strongly prefer the program on the left”; “5-Indifferent” “9-Strongly prefer the program on the right”).
Figure 1. Descriptions of hospice services.
Figure 2. Examples of questions used in conjoint interviews to measure patient's perceived needs (direct ratings of importance and comparisons of pairs of services).
Patients' preferences for cancer treatment were assessed by asking whether they would want to continue receiving their current cancer treatment in order to achieve various probabilities of surviving for six months (almost 100%, 90-99%, 50-89%, 10-49%, 1-9%, and almost 0%). This question was adapted from previous work in seriously ill populations.64, 65 These probabilities were varied systematically (from lowest to highest and then back to the second-lowest) to balance order effects. The lowest probability of six-month survival was recorded for which a patient would be willing to continue receiving treatment. Responses were used to create a 7-level ordinal variable describing the strength of a patient's treatment preferences (one level for each of the six responses above, plus one for those patients who would not want to continue treatment even for an almost 100% chance of surviving for six months). This last category was used to create a dichotomous variable that identified patients who would not want treatment even for an almost 100% probability of surviving for six months and who thus would have been eligible for hospice.
Data analysis
Using the scale described above, preferences for aggressive cancer treatment were compared using a Wilcoxon-rank sum test in bivariate analysis. Adjusted analysis of preferences was done using an ordinal logistic regression model. Based on respondents' direct ratings and their choices among service options, Adaptive Conjoint Analysis uses least squares regression to calculate the utility, or usefulness, of each service for each patient.66 These utilities reflect the perceived need that a patient has for each service, and higher utilities correspond to a greater perceived need. We analyzed patients' perceived needs for each of the five services individually, as well as patients' perceived needs for all five services combined (their total utilities). Because utilities were not normally distributed we used the Wilcoxon rank sum test to compare perceived needs among patient subgroups, and linear regression models with a log transformation and exponentiated coefficients to identify variables that were independently associated with service needs. Variables with a significance value of less than 0.25 were considered for inclusion in a multivariable linear regression model,67 also with a log transformation and exponentiated coefficients.
A sample of 283 patients would be adequate to detect a small difference in the summed utilities of all five hospice services between African-American and white patients, assuming at least 20% of the sample would be African American (ability to detect 0.33 standardized difference, α=0.05, two-sided). Stata software (Stata for Windows, version 8.0, Stata Co., College Station, TX) was used for all statistical analysis.
Results
Patient characteristics
Patients who agreed to participate (300/352; 85%) were similar to those who refused with respect to age, ECOG performance score, race, and education (data not shown). However, women were significantly more likely to participate compared to men (152/169, 92% vs.148/183, 82%; Fisher's exact test p=0.02). Of the 300 patients who consented, this sample was restricted to those patients (n=283; 94%) who self-identified as either African-American (n=81;29%) or white (n=202;71%). The characteristics of these patients are described in Table 1.
Table 1. Patient characteristics.
| Overall (N=300) | African American (N=81) | White (N=202) | P-values | |
|---|---|---|---|---|
| Sex | N (%) | N (%) | N (%) | P=0.10 |
| Male | 148 (49) | 47 (58) | 95 (47) | |
| Age: Mean (Range) | 58(20-89) | 63 (31-89) | 57 (20-89) | P=0.002 |
| Over 65 | 84 (28) | 33 (41) | 49 (24) | |
| Marital status | P=0.20 | |||
| Single | 45 (15) | 19 (23) | 23 (11) | |
| Married | 174 (58) | 28 (35) | 136 (67) | |
| Divorced/separated | 45 (15) | 19 (23) | 23 (11) | |
| Widowed | 22 (7) | 9 (11) | 13 (6) | |
| Living w/ partner | 14 (5) | 6 (7) | 7 (3) | |
| Household finances (funds available at the end of the month) | P<0.001 | |||
| Has money left over | 142 (47) | 14 (17) | 122 (60) | |
| Has just enough to make ends meet | 80 (27) | 29 (36) | 47 (23) | |
| Does not have enough money to make ends meet | 52 (17) | 27 (33) | 20 (10) | |
| Refused | 26 (9) | 11 (14) | 13 (6) | |
| Educational level | P<0.001 | |||
| Did not graduate from high school | 24 (8) | 14 (17) | 8 (4) | |
| High school | 85 (28) | 32 (40) | 50 (25) | |
| Some college or technical school | 76 (25) | 19 (23) | 53 (26) | |
| College | 55 (18) | 8 (10) | 43 (21) | |
| Graduate school | 60 (20) | 8 (10) | 48 (24) | |
| ECOG performance score | P=0.13 | |||
| 0 | 90 (30) | 23 (28) | 64 (32) | |
| 1 | 32 (11) | 6 (7) | 23 (11) | |
| 2 | 124 (41) | 32 (40) | 85 (42) | |
| 3 | 46 (15) | 17 (21) | 26 (13) | |
| 4 | 8 (3) | 3 (4) | 4 (2) | |
| Cancer type | P=0.91 | |||
| Breast | 84 (28) | 20 (25) | 58 (29) | |
| Gastrointestinal | 53 (18) | 15 (19) | 35 (17) | |
| Hematologic | 37 (12) | 4 (5) | 31 (15) | |
| Lung | 36 (12) | 9 (11) | 26 (13) | |
| Prostate | 35 (12) | 20 (25) | 14 (7) | |
| Oropharynx | 29 (10) | 8 (10) | 19 (9) | |
| Genitourinary | 18 (6) | 1 (1) | 16 (8) | |
| Sarcoma | 5 (2) | 4 (5) | 1 (0.5) | |
| Melanoma | 2 (1) | 0 (0) | 2 (1) | |
| Glioblastoma | 1 (0) | 0 (0) | 0 (0) | |
| Global distress index symptoms | ||||
| Lack of appetite | 111 (37) | 34 (42) | 69 (34) | P=0.22 |
| Lack of energy | 204 (68) | 51 (63) | 150 (69) | P=0.30 |
| Pain | 164 (55) | 50 (62) | 101 (50) | P=0.07 |
| Drowsiness | 171 (57) | 47 (58) | 113 (56) | P=0.75 |
| Constipation | 94 (31) | 30 (37) | 55 (27) | P=0.10 |
| Dry Mouth | 137 (46) | 43 (53) | 83 (42) | P=0.07 |
| Sadness | 116 (39) | 29 (36) | 80 (40) | P=0.55 |
| Worrying | 170 (57) | 47 (58) | 115 (57) | P=0.87 |
| Irritability | 121 (40) | 32 (40) | 80 (40) | P=0.99 |
| Nervousness | 116 (39) | 30 (37) | 78 (39) | P=0.81 |
| Continue cancer treatment w/probability of survival | P=0.002 | |||
| Almost 100% | 140 (47) | 48 (59) | 86 (43) | |
| 90-99% | 22 (7) | 9 (11) | 11 (5) | |
| 50-89% | 34 (11) | 3 (4) | 28 (14) | |
| 10-49% | 50 (17) | 16 (20) | 31 (15) | |
| 1-9% | 9 (3) | 0 (0) | 9 (4) | |
| Almost 0% | 7 (2) | 0 (0) | 5 (2) | |
| No treatments | 38 (13) | 5 (6) | 32 (16) | ` |
Patient race and cancer treatment preferences
African-American patients had stronger preferences for aggressive cancer treatment (using the scale of choices from 1 to 7) compared to white patients (median 6 vs. 4, Wilcoxon rank sum test p=0.006). That is, they were willing to continue their treatment in return for a smaller likelihood of six-month survival. In an ordinal logistic regression model, African American patients had stronger preferences for aggressive cancer treatment (adjusted means 4.75 vs. 3.96; β coefficient 0.82; 95% confidence interval 0.22-1.41; p=0.007) after adjusting for age, sex, household finances, education, ECOG performance status, quality of life (FACT-G), and physical and psychological symptom burden (physical and psychological subscales of the GDI, respectively). Compared to white patients, African American patients were also less likely to say that they would refuse all cancer treatment even if it were associated with an “almost 100%” probability of surviving for six months (5/81, 6% vs. 32/202, 16%; odds ratio 2.86; 95% CI 1.04-9.74; p=0.03).
Patient race and perceived needs for hospice services
Compared to white patients, African American patients reported greater needs for all hospice services combined (median utilities 2.26 vs. 1.79; Rank sum test p=0.005). African-American patients assigned higher utilities to all hospice services except a home health aide (Figure 3).
Figure 3. Patient utilities for hospice services.
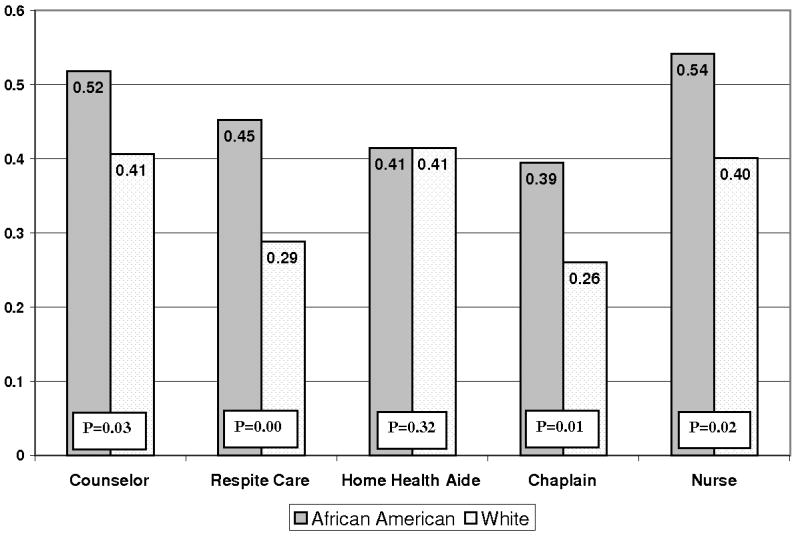
In a multivariable regression model, African-American race remained associated with greater perceived needs for services after adjusting for age, education, ECOG performance status, dependencies in ADLs, and physical and psychological symptom burden (GDI physical and psychological subscales, respectively) (adjusted mean utilities 2.31 vs. 1.83) (β coefficient 0.51; 95% confidence interval 0.11-0.92; p=0.01). This model did not include economic factors, which were considered separately, below.
To describe the relationship between perceived needs for hospice services and economic factors, which are often closely associated with race,68 we used household finances as an indicator of economic status (not enough/enough/more than enough money left at the end of the month). In unadjusted analysis, patients with fewer financial resources had greater perceived needs for hospice services (more than enough money left over: 1.51; enough money left over: 2.34 not enough money left over: 2.53). When the perceived needs of African American and white patients were compared after adjusting for household finances, there was no significant difference (adjusted mean utilities 2.38 vs. 1.75; β =0.24; 95% CI -0.22-0.70; p=31). Similarly, in a combined model that included household finances as well as all of the patient characteristics used in earlier models, African Americans did not have greater perceived needs for hospice services.
In sub-analyses, we compared the perceived needs for hospice services of African American (n=76) and white patients (n=170) whose preferences excluded them from hospice. In these groups, African American patients had significantly greater perceived needs than white patients did (total utilities 2.34 vs. 1.81; rank sum test p=0.006). We also compared the perceived needs of African-American patients whose treatment preferences made them ineligible for hospice (n=76) and white patients whose treatment preferences were consistent with hospice (n=32). After controlling for health status by adjusting for age, ECOG performance status, dependencies in ADLs, and GDI physical and psychological subscale scores, ineligible African-American patients had greater perceived needs for hospice services than eligible whites did (adjusted means 2.31 vs. 1.73; β coefficient 0.70; 95% confidence interval 0.05-1.35; p=0.03). However, after adjusting for household finances these two groups had similar utilities for hospice services (1.91 vs. 1.83; β coefficient -0.34; 95% confidence interval -0.56-0.11 p=0.27). Because of the small number of African American patients whose preferences made them eligible for hospice (n=5) a comparison of these patients' perceived needs with those of ineligible African Americans was not possible.
Discussion
The Medicare hospice benefit and similar benefits of other insurers were designed to ensure that patients in the last six months of life have access to high-quality palliative care. However, African-American patients are less likely to utilize hospice than white patients. This study suggests that disparities in hospice utilization among patients with cancer may be the result of cancer treatment preferences among African American patients that make them ineligible despite greater perceived needs for hospice care. In particular, this study offers three main insights into these disparities in hospice access.
First, we found that African-American patients with cancer are more likely than white patients to want aggressive cancer treatment. This difference in preferences persists after adjusting for clinical and demographic characteristics. This result is important because although other studies have observed racial differences in preferences for life-sustaining technologies,26-29 they have not examined preferences for cancer treatment. Preferences for aggressive cancer care, as well as other aggressive technologies, could be linked to medical distrust, quality of care, or to communication issues between patients and providers.
Second, we found that African-American patients with cancer had greater perceived needs for specific hospice services compared to white patients. This difference appears to be independent of clinical characteristics (e.g. symptom burden, performance status) that are associated with greater needs. Furthermore, African American patients whose treatment preferences would have excluded them from hospice had greater perceived needs than did white patients who would have been eligible.
Third, we found that that the greater perceived need for hospice services among African Americans was attributable largely to differences in self-reported finances. That is, the observed differences in perceived needs between African American and white patients may reflect financial resources since those reporting the fewest financial resources also report the greatest need for services. This finding is consistent with other studies suggesting that the mechanisms driving health disparities include not only cultural differences associated with race but also economic characteristics that may be fundamentally unrelated to race.36, 68, 69 Thus, these economics factors should be further explored to understand why poorer patients want more services. For instance, it is possible that wealthier patients have more resources for care at the end of life, and use these resources to obtain services outside of hospice. If so, then wealthier patients may be better able to avoid the “terrible choice” requiring that they forgo treatment in order to receive hospice benefits. However, this is not known.
Together, these findings suggest that the hospice eligibility criteria of Medicare and other insurers requiring patients to give up cancer treatment contribute to racial disparities in hospice utilization. Moreover, these criteria do not select those patients with the greatest needs for hospice services. To the degree that this eligibility requirement prevents hospice utilization by those patients with the greatest needs, it fails to fulfill its purpose and should be reconsidered. It is also unfair: other Medicare-supported services do not require that patients forgo one treatment in order to get another.70 Instead, this study suggests that hospice access could be made fairer by using eligibility criteria that are more directly need-based. For instance, eligibility might be better determined by assessing needs for specific hospice services such as pain or symptom management. This would make eligibility for hospice similar to eligibility for the Medicare Home Care Benefit, which is perhaps the closest Medicare program.70
This study has several limitations. First, the results reported here are based on patients' self-reported needs for hospice services, but it is possible that these patients could not adequately appreciate how the services described here could benefit them.63 However, patients arguably are the best judges of their own needs, even if those assessments are imperfect.
Second, this study assessed only five hospice services. It is possible that the finding of greater perceived needs reported here by African-American patients would not be found for other services that hospice provides (e.g. delivery of medications or durable medical equipment). Although this is possible, there is no reason to believe that the pattern observed for the five services described here are unique.
Third, this study did not assess actual choices about hospice enrollment, which may be influenced by factors like the availability of family members who can assist with home care. A patient without adequate informal caregiving support and supervision at home may be less likely to enroll. Therefore, further research is needed to define which patient characteristics, such as the availability of family support, influence actual choices about hospice enrollment.
For 25 years, hospice services have been restricted to patients in the last six months of life who are willing to give up curative treatment.18 Although this restriction was intended to control costs, it has substantially reduced access to hospice for many patients who have needs for hospice services, and a disproportionate number of these patients are African American. This eligibility criterion should be reconsidered, and needs-based criteria should be considered in order to make hospice eligibility criteria both fairer and more consistent with eligibility criteria for other health insurance benefits.70
Acknowledgments
Acknowledgements of research support: The authors are in part supported by an MRSGT-08-013-01-CPPB American Cancer Society Mentored Scholar Research Grant (Fishman), University of Pennsylvania's NIH-funded Center of Excellence for Cancer Communication Research Grant (Fishman), an R01CA109540 (Casarett), a VA Advanced Research Career Development Award, a Presidential Early Career Award for Scientists and Engineers (Casarett), and by the Abramson Cancer Center (O'Dwyer), the Center for Clinical Epidemiology and Biostatistics (Fishman) and the Center for Health Equity Research and Promotion (Casarett, Fishman).
References
- 1.Lutz S, Norrell R, Bertucio C, et al. Symptom frequency and severity in patients with metastatic or locally recurrent lung cancer: a prospective study using the Lung Cancer Symptom Scale in a community hospital. Journal of Palliative Medicine. 2001;4(2):157–65. doi: 10.1089/109662101750290191. [DOI] [PubMed] [Google Scholar]
- 2.Coyle N, Adelhardt J, Foley KM, Portenoy RK. Character of terminal illness in the advanced cancer patient: pain and other symptoms in the last four weeks of life. Journal of Pain & Symptom Management. 1990;5:83–93. doi: 10.1016/s0885-3924(05)80021-1. [DOI] [PubMed] [Google Scholar]
- 3.Vaino A, Auvinen A. Prevalence of symptoms among patients with advanced cancer: an international collaborative study. Journal of Pain & Symptom Management. 1996;12:3–10. doi: 10.1016/0885-3924(96)00042-5. [DOI] [PubMed] [Google Scholar]
- 4.Hickok JT, Morrow GR, McDonald S, Bellg AJ. Frequency and correlates of fatigue in lung cancer patients receiving radiation therapy: implications for management. Journal of Pain & Symptom Management. 1996;11(6):370–7. doi: 10.1016/0885-3924(96)00008-5. [DOI] [PubMed] [Google Scholar]
- 5.Twycross R, Harcourt J, Bergl S. A survey of pain in patients with advanced cancer. Journal of Pain & Symptom Management. 1996;12(5):273–82. doi: 10.1016/s0885-3924(96)00149-2. [DOI] [PubMed] [Google Scholar]
- 6.Harrington V, Lackey NR, Gates MF. Needs of caregivers of clinic and hospice cancer patients. Cancer Nursing. 1996;19(2):118–25. doi: 10.1097/00002820-199604000-00006. [DOI] [PubMed] [Google Scholar]
- 7.McMillan SC, Mahon M. The impact of hospice services on the quality of life of primary caregivers. Oncology Nursing Forum. 1994;21(7):1189–95. [PubMed] [Google Scholar]
- 8.Steele RG, Fitch MI. Needs of family caregivers of patients receiving home hospice care for cancer. Oncology Nursing Forum. 1996;23:823–28. [PubMed] [Google Scholar]
- 9.Kane R, Wales J, Bernstein L, Leibowitz A, Kaplan S. A randomized controlled trial of hospice care. The Lancet. 1984 April 21;:890–94. doi: 10.1016/s0140-6736(84)91349-7. [DOI] [PubMed] [Google Scholar]
- 10.Casarett D, Karlawish J, Crowley R, Mirsch T, Morales K, Asch DA. Improving use of hospice care in the nursing home: a randomized controlled trial. JAMA. 2005;294:211–7. doi: 10.1001/jama.294.2.211. [DOI] [PubMed] [Google Scholar]
- 11.Teno J, Clarridge B, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 12.Miller S, Mor V, Wu N, Gozalo P, Lapane K. Does receipt of hospice care in nursing homes improve the management of pain at the end of life? Journal of the American Geriatrics Society. 2002;50(3):507–15. doi: 10.1046/j.1532-5415.2002.50118.x. [DOI] [PubMed] [Google Scholar]
- 13.Miller SC, Mor V, Teno J. Hospice enrollment and pain assessment and management in nursing homes. Journal of Pain & Symptom Management. 2003 Sep;26(3):791–9. doi: 10.1016/s0885-3924(03)00284-7. [DOI] [PubMed] [Google Scholar]
- 14.Seamark DA, Williams S, Hall M, Lawrence CJ, Gilbert J. Dying from cancer in community hospitals vs. hospice: closest lay carers' perceptions. Br J Gen Pract. 1998;48:1317–21. [PMC free article] [PubMed] [Google Scholar]
- 15.Greiner K, Allen SP, Ahluwalia JS. Hospice Usage by Minorities in the Last Year of Life: Results from the National Mortality Followback Survey. Journal of the American Geriatrics Society. 2003;51(7):970–8. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- 16.Han B, Remsburg RE, Iwashyna TJ. Differences in hospice use between black and white patients during the period 1992 through 2000. Medical Care. 2006;44:731–77. doi: 10.1097/01.mlr.0000215858.37118.65. [DOI] [PubMed] [Google Scholar]
- 17.Johnson KS, Kuchibhatla M, Tanis D, Tulsky JA. Racial differences in hospice revocation to pursue aggressive care. Arch Intern Med. 2008;168(2):218–24. doi: 10.1001/archinternmed.2007.36. [DOI] [PubMed] [Google Scholar]
- 18.Medicare Hospice Regulations. 42 Code of Federal Regulations, Part 418.22. 1996. [Google Scholar]
- 19.Gibson R. Palliative care for the poor and disenfranchised: a view from the Robert Wood Johnson Foundation. J R Soc Med. 2001;94:486–9. doi: 10.1177/014107680109400921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Testimony presented before the Congress of the United States House of Representatives Committee on Government Reform; October 19, 1999; 1999. [May 25, 2007]. http://www.dyingwell.org/uschrtest.htm. [Google Scholar]
- 21.Gelband H, Foley K. Improving Palliative Care for Cancer: Summary and Recommendations. Washington DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 22.Byock IR, Forman WB, Appleton M. Academy of hospice physicians' position statement on access to hospice and palliative care. Journal of Pain & Symptom Management. 1996;11(2):69–70. doi: 10.1016/0885-3924(95)00154-9. [DOI] [PubMed] [Google Scholar]
- 23.McGorty EK, Bornstein BH. Barriers to physicians' decisions to discuss hospice: insights gained from the United States hospice model. Journal of Evaluation in Clinical Practice. 2003;9:363–72. doi: 10.1046/j.1365-2753.2003.00406.x. [DOI] [PubMed] [Google Scholar]
- 24.Daugherty CK, Steensma DP. Overcoming obstacles to hospice care: an ethical examination of inertia and inaction. Journal of Clinical Oncology. 2002 Jun 1;20(11):2752–5. doi: 10.1200/JCO.2002.20.11.2752. [DOI] [PubMed] [Google Scholar]
- 25.Miller SC, Weitzen S, Kinzbrunner B. Factors associated with the high prevalence of short hospice stays. Journal of Palliative Medicine. 2003 Oct;6(5):725–36. doi: 10.1089/109662103322515239. [DOI] [PubMed] [Google Scholar]
- 26.Blackhall L, Frank G, Murphy S, Michel V, Palmer J, Azen S. Ethnicity and attitudes towards life sustaining technology. Soc Sci Med. 1999;48:1779–89. doi: 10.1016/s0277-9536(99)00077-5. [DOI] [PubMed] [Google Scholar]
- 27.Caralis P, Davis B, Wright K, Marcial E. The influence of ethnicity and race on attitudes toward advance directives, life-prolonging treatments, and euthanasia. Journal of Clinical Ethics. 1993;4:155–65. [PubMed] [Google Scholar]
- 28.Degenholtz H, Thomas SB, Miller MJ. Race and the intensive care unit: Disparities and preferences for end-of-life care. Critical Care Medicine. 2003;31(5):s373–s8. doi: 10.1097/01.CCM.0000065121.62144.0D. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell SL, Teno JM, Roy J, Kabumoto G, Mor V. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. JAMA. 2003;290(1):73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- 30.Neubauer B, Hamilton C. Racial differences in attitudes toward hospice care. Hosp J. 1990;6(1):37–48. doi: 10.1080/0742-969x.1990.11882664. [DOI] [PubMed] [Google Scholar]
- 31.Hwang S, Chang V, Cogswell J, Srinivas S, Kasimis B. Knowledge and attitudes toward end-of-life care in veterans with symptomatic metastatic cancer. Palliat Support Care. 2003 Sep;1(3):221–30. doi: 10.1017/s1478951503030396. [DOI] [PubMed] [Google Scholar]
- 32.Taxis J. Attitudes, values, and questions of African Americans regarding participation in hospice programs. Journal of Hospice and Palliative Nursing. 2006;8(2):77–85. [Google Scholar]
- 33.Cort M. Cultural mistrust and use of hospice care: challenges and remedies. Journal of Palliative Medicine. 2004;7(1):63–71. doi: 10.1089/109662104322737269. [DOI] [PubMed] [Google Scholar]
- 34.Born W, Greiner K, Sylvia E, Butler J, Ahluwalia J. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. Journal of Palliative Medicine. 2004;7(2):247–56. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 35.Foley K, Gelband H. Improving palliative care for cancer: summary and recommendations Institute of Medicine and National Research Council. Washington, D.C.: National Academy Press; 2001. [PubMed] [Google Scholar]
- 36.Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the African American community. JAMA. 2000;284(19):2518–21. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- 37.National Trend Summary 2005. National Hospice and Palliative Care Organization; Washington DC: 2006. [Google Scholar]
- 38.Cornoni J, Ostfeld A, Taylor J, et al. Establishing populations for epidemiologic studies of the elderly: study design and methodology. Aging. 1993;5:27–37. doi: 10.1007/BF03324123. [DOI] [PubMed] [Google Scholar]
- 39.Portenoy RK, Thaler HT, Kornblith AB, et al. The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. European Journal of Cancer. 1994;30A(9):1326–36. doi: 10.1016/0959-8049(94)90182-1. [DOI] [PubMed] [Google Scholar]
- 40.Cella DF, Tulsky DS, Gray G. The functional assessment of cancer therapy scale: development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–9. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 41.Sherbourne CD, Stewart AL. The MOS Social Support Survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 42.Jenkinson C, Wright L, Coulter A. Criterion validity and reliability of the SF-36 in a population sample. Quality of Life Research. 1994;3:7–12. doi: 10.1007/BF00647843. [DOI] [PubMed] [Google Scholar]
- 43.Conill C, Verger E, Salamero M. Performance status assessment in cancer patients. Cancer. 1990;65(8):1864–6. doi: 10.1002/1097-0142(19900415)65:8<1864::aid-cncr2820650832>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 44.Sloan JA, Loprinzi CL, Laurine JA, et al. A simple stratification factor prognostic for survival in advanced cancer: the good/bad/uncertain index. Journal of Clinical Oncology. 2001;19:3539–46. doi: 10.1200/JCO.2001.19.15.3539. [DOI] [PubMed] [Google Scholar]
- 45.Katz S, Akpom CA. Index of ADL. Medical Care. 1976;14:116–18. doi: 10.1097/00005650-197605001-00018. [DOI] [PubMed] [Google Scholar]
- 46.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Maryland State Medical Journal. 1965;14:62–5. [PubMed] [Google Scholar]
- 47.Green P, Rao V. Conjoint Measurement for Quantifying Judgmental Data. Journal of Marketing Research. 1971;8(August):355–63. [Google Scholar]
- 48.Green P. Hybrid Models for Conjoint Analysis: An Expository Review. Journal of Marketing Research. 1984;21(May):155–9. [Google Scholar]
- 49.Leigh T, MacKay D, Summers J. Reliability and Validity of Conjoint Analysis and Self-Explicated Weights: A Comparison. Journal of Marketing Research. 1984;21(November):456–62. [Google Scholar]
- 50.Moore W, Semenik R. Measuring Preference With Hybrid Conjoint Analysis: The Impact of a Different Number of Attributes in the Master Design. Journal of Business Research. 1988;16:261–74. [Google Scholar]
- 51.Leung G, Chan S, Chau P, Chua S. Using Conjoint Analysis to Assess Patients' Preferences When Visiting Emergency Departments in Hong Kong. Academic Emergency Medicine. 2001;8:894–8. doi: 10.1111/j.1553-2712.2001.tb01151.x. [DOI] [PubMed] [Google Scholar]
- 52.Markham F, Diamond J, Hermansen C. The Use of Conjoint Analysis to Study Patient Satisfaction. Evaluation & the Health Professions. 1999;22(3):371–8. doi: 10.1177/01632789922034365. [DOI] [PubMed] [Google Scholar]
- 53.Ryan M. A Role for Conjoint Analysis in Technology Assessment in Health Care. International Journal of Technology Assessment in Health Care. 1999;15(3):443–57. [PubMed] [Google Scholar]
- 54.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. British Medical Journal. 2000;320:1530–3. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shackley P, Slack R, Michaels J. Vascular patients' preferences for local treatment: an application of conjoint analysis. Journal of Health Services & Research Policy. 2001;6(3):151–7. doi: 10.1258/1355819011927404. [DOI] [PubMed] [Google Scholar]
- 56.Jan S, Mooney G, Ryan M, Bruggemann K, Alexander K. The use of conjoint analysis to elicit community preferences in public health research: a case study of hospital services in South Australia. Australian and New Zealand Journal of Public Health. 2000;24(1):64–70. doi: 10.1111/j.1467-842x.2000.tb00725.x. [DOI] [PubMed] [Google Scholar]
- 57.Shea JA, Asch DA, Johnson RF, et al. What predicts gastroenterologists' and surgeons' diagnosis and management of common bile duct stones? Gastrointestinal Endoscopy. 1997;46:40–7. doi: 10.1016/s0016-5107(97)70208-6. [DOI] [PubMed] [Google Scholar]
- 58.Fraenkel L, Bogardus S, Wittink DR. Understanding patient preferences for the treatment of lupus nephritis with adaptive conjoint analysis. Medical Care. 2001;39(11):1203–16. doi: 10.1097/00005650-200111000-00007. [DOI] [PubMed] [Google Scholar]
- 59.Srinivasan V, Jain A, Malhotra N. Improving Predictive Power of Conjoint Analysis by Constrained Parameter Estimation. Journal of Marketing Research. 1983;20(November):433–8. [Google Scholar]
- 60.Srinivasan V, Flaschsbart P, Dajani J, Hartley R. Forecasting the Effectiveness of Work-Trip Gasoline Conservation Policies Through Conjoint Analysis. Journal of Marketing. 1981;45(Summer):157–72. [Google Scholar]
- 61.Casarett D, Crowley R, Hirschman K. How should clinicians describe hospice to patients and their families? Journal of the American Geriatrics Society. 2004;52:1923–8. doi: 10.1111/j.1532-5415.2004.52520.x. [DOI] [PubMed] [Google Scholar]
- 62.Casarett D, Crowley R, Stevenson C, Xie S, Teno J. Making difficult decisions about hospice enrollment: What do patients and families want to know? Journal of the American Geriatrics Society. 2005;53:249–54. doi: 10.1111/j.1532-5415.2005.53110.x. [DOI] [PubMed] [Google Scholar]
- 63.Rickerson E, Harrold J, Carroll J, Kapo J, Casarett D. Timing of hospice referral and families' perceptions of services: Are earlier hospice referrals better? Journal of the American Geriatrics Society. 2005;53:819–23. doi: 10.1111/j.1532-5415.2005.53259.x. [DOI] [PubMed] [Google Scholar]
- 64.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. New England Journal of Medicine. 2002;346(14):1061–6. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 65.Casarett D, Van Ness P, O'Leary J, Fried T. Are patient preferences for life-sustaining treatment really a barrier to hospice enrollment for older adults with serious illness? Journal of the American Geriatrics Society. 2006;54:472–8. doi: 10.1111/j.1532-5415.2005.00628.x. [DOI] [PubMed] [Google Scholar]
- 66.ACA/Hierarchical Bayes Technical Paper. Sawtooth Software Technical Paper Series. Sawtooth Software, Inc.; Sequim, WA: 2001. [Google Scholar]
- 67.Mickey J, Greenland S. A study of the impact of confounder-selection criteria on effect estimation. American Journal of Epidemiology. 1989;129:125–37. doi: 10.1093/oxfordjournals.aje.a115101. [DOI] [PubMed] [Google Scholar]
- 68.Braveman P, Cubbin C, Egerter S, et al. Socioeconomic Status in Health Research: One Size Does Not Fit All. JAMA. 2005;294:2879–88. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 69.Shavers V, Brown M. Racial and ethnic disparities in the receipt of cancer treatment. Review J Natl Cancer Inst. 2002;94(5):334–57. doi: 10.1093/jnci/94.5.334. [DOI] [PubMed] [Google Scholar]
- 70. [June 4, 2007];Your Medicare Benefits. Centers for Medicare & Medicaid Services. http://www.medicare.gov/Publications/Pubs/pdf/10116.pdf.


