Abstract
Elucidation of mechanisms underlying the high rates of alcohol use disorder (AUD) remains a pressing clinical and research concern. Despite data indicating that social anxiety disorder (SAD) may be a psychological vulnerability that increases AUD risk, no known prospective research has examined underlying mechanisms. Given the nature of SAD, social support and peer alcohol use may be implicated. The present study set out to clarify the SAD-AUD link in several ways using a prospective dataset comprised of 1803 (47% female) young adults at T1, 1431 of whom were assessed again approximately three years later. First, stringent criteria were used to directly test whether SAD was a risk for AUD. Second, we examined whether social support and peer alcohol use moderated the prospective SAD-AUD link. Structured diagnostic interviews were conducted to assess DSM-IV Axis I disorders, negative life events, social support, and peer alcohol use. Among men, Time 1 (T1) SAD was not significantly related to Time 2 (T2) AUD. Yet, among women, T1 SAD was related to T2 AUD. Further, T1 SAD was the only internalizing disorder to significantly predict T2 AUD after controlling for relevant variables (e.g., T1 depression, other anxiety, alcohol and marijuana use disorders). The SAD-AUD relation demonstrated directional specificity. Family cohesion and adverse family relations significantly moderated this relation. Findings highlight the important role of SAD and familial support in the onset of AUD among women.
Keywords: Alcohol use disorder, Social anxiety disorder, Social Phobia, Social Support, Risk Factor, Gender
1. Introduction
Alcohol use disorders (AUD) are frequently comorbid with social anxiety disorder (SAD) (Buckner et al., 2008; Davidson et al., 1993; Grant et al., 2005; Kessler et al., 1997). For instance, in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), 48% of individuals with a lifetime diagnosis of SAD also met criteria for a lifetime diagnosis of an AUD (Grant et al., 2005). The 12-month prevalence of AUD among individuals with SAD was 13.1% (Grant et al., 2005) compared to 8.5% among the general population (Grant et al., 2004). Women with SAD appear to demonstrate higher rates of AUD than men with SAD (Kessler et al., 1997). Yet, little is known about the specificity or temporal sequencing of the relationships between SAD and AUD. In particular, little empirical work has examined factors that increase AUD risk in this vulnerable population (i.e., individuals with SAD). Similarly we know of no work that has examined factors that may be protective. Elucidation of AUD risk and protective factors among people with SAD would have important implications for the treatment and even the prevention of AUD among this high-risk group.
The high rates of comorbidity between AUD and SAD are a substantial clinical and research concern given that this comorbidity tends to be associated with greater impairment than either condition alone. For instance, among treatment-seeking participants in Project MATCH (Project MATCH Research Group, 1993), patients with AUD and a lifetime history of SAD experienced more severe alcohol dependence and reported more major depressive episodes, less peer social support, and lower occupational status than patients with AUD without SAD (Thevos et al., 1999; Thomas et al., 1999). Similarly, relative to patients with SAD and no AUD history, patients with SAD and a history of AUD exhibit more severe symptoms of SAD, greater psychiatric comorbidity, more health problems, and greater deficits in interpersonal functioning (e.g., even less likely to be married) than individuals with SAD alone (Buckner et al., in press; Schneier et al., 1989). Thus, although both SAD and AUD are individually impairing, their combination is particularly harmful and represents an important public health concern.
1.1 Social anxiety disorder as a risk factor for alcohol use disorders
The prominent theoretical model of the SAD-AUD link suggests that social anxiety is a risk factor for the development of AUD, as it is believed that individuals with social anxiety use alcohol to manage distress associated with their concerns regarding negative evaluation and scrutiny by others, increasing their AUD vulnerability (e.g., Buckner et al., 2006a; Buckner et al., 2008; Carrigan and Randall, 2003; Morris et al., 2005). However, most empirical work examining the relations between SAD and AUD has been cross-sectional in nature and very little research has directly tested the contention that SAD is a risk for AUD. Garber and Hollon (1991) outlined three criteria for causal attribution that have traditionally been recognized in psychopathology risk research. First, the proposed risk factor must be correlated with the outcome. Second, the risk factor must demonstrate temporal precedence. Third, the relation between the risk factor and outcome variable must be non-spurious (i.e., not due to a third variable or set of variables).
With respect to the first criterion, social anxiety is consistently correlated with alcohol problems and AUD (Buckner et al., in press;Buckner et al., 2006a; Buckner et al., 2008; Ham et al., 2005; Morris et al., 2005). In regard to the second criterion, the onset of SAD appears to generally precede the onset of AUD. To illustrate, patients with comorbid AUD and SAD typically report that SAD onset predated AUD onset (Buckner et al., in press; Randall et al., 2001). Prospectively, adolescent SAD was found to predict alcohol dependence by age 30 (Buckner et al., 2008) and elevated fear of scrutiny predicted later AUD onset in U.S. samples (Buckner and Schmidt, in press). Among German adolescents, however, SAD was longitudinally related to greater rates of hazardous drinking but not AUD (Zimmermann et al., 2003) and among adults in the U.S., subclinical (but not clinical) SAD has been linked to AUD 13 years later (Crum and Pratt, 2001). Thus, although the onset of SAD seems to generally precede the onset of AUD, additional work is necessary to demarcate whether this pattern applies to clinical levels of SAD and AUD.
The least amount of empirical work has examined the third risk factor criterion, non-spuriousness. Our recent finding that the prospective link between SAD and alcohol dependence remained observable even with other psychiatric disorders (e.g., internalizing and externalizing disorders) controlled provides initial evidence for non-spuriousness in that it suggests the SAD-AUD link is not due to co-occurring internalizing and externalizing disorders (Buckner et al., 2008). Also, in the National Comorbidity Survey (NCS), SAD was associated with higher rates of AUD relative to most other anxiety disorders (Kessler et al., 1997) and remained related to AUD after controlling for other Axis I disorders (Buckner et al., in press). Although this initial evidence is promising, additional work is necessary to rule out other possible shared vulnerabilities between SAD and AUD. For instance, one of our prospective studies did not include post-traumatic stress disorder (PTSD) as a potential “third variable” (Buckner et al., 2008). Given that PTSD tends to be associated with both SAD and AUD (Kessler et al., 2005), it is important to determine whether the link between SAD and AUD remains after controlling for this anxiety disorder. Similarly, no known studies have examined whether negative life events, a factor that appears causally implicated in the occurrence of both substance use disorders (SUD) and anxiety disorders (Lloyd and Turner, 2008; Turner and Lloyd, 2003, 2004), accounts for the apparent link between SAD and AUD.
1.2 Psychosocial mechanisms underlying the SAD-AUD link
Although theoretical models and emerging data indicate that SAD seems to be a risk factor for alcohol-related problems, very little is known about what contributes to the development of AUD among people with SAD as the research on underlying mechanisms has relied on cross-sectional data. No known prospective work has examined factors that may increase AUD risk among individuals with SAD. Given the nature of SAD (the hallmark feature of which is fear of negative evaluation in social situations), it follows that social influences may play a large role in the development of problematic alcohol use in this population. For instance, peer substance use is one of the most consistent predictors of substance use (e.g.,Beal et al., 2006). Socially anxious individuals may be particularly vulnerable to the influence of peers given their heightened concerns of negative evaluation. In fact, young adults with higher social anxiety are more likely to report using alcohol in response to perceived peer pressure (Buckner et al., 2006a) and to avoid social censure (Stewart et al., 2006). Although promising, this literature is limited by cross-sectional designs, making it impossible to draw firm conclusions about the causal role of peer alcohol use.
Similarly, social support may be particularly relevant to the development of AUD among those with SAD. Low levels of peer and parental support are consistently related to AUD (Barnow et al., 2002; Groh et al., 2007; Patock-Peckham and Morgan-Lopez, 2007). Social anxiety is associated with less social support from peers (La Greca and Lopez, 1998; Torgrud et al., 2004) as well as less parental support and having parents with more negative parenting styles (Boegels et al., 2001; Bruch and Heimberg, 1994; Lieb et al., 2000; Rapee, 1997). Although this indirect evidence suggests that parental and peer support variables may influence AUD risk among those with SAD, we know of no direct tests of this hypothesis.
Another limitation of our current understanding of the relations between AUD and SAD is the role of sex. Very little attention has been paid to whether SAD is a risk for AUD among both men and women. The NCS data suggest that women with SAD exhibit significantly higher rates of both alcohol abuse and dependence than men with SAD (Kessler et al., 1997). Further, empirical evidence suggests that men and women exhibit differential anxiety responses to alcohol, with women exhibiting decreased anxiety following alcohol consumption during a social anxiety-provoking task whereas men demonstrated greater anxiety (Sinha et al., 1998). These data suggest that the relations between AUD and SAD should be examined separately by sex as the practice of combining both men and women in data analytic models may obfuscate the relations between AUD and SAD if one sex is positively associated with alcohol use behaviors whereas the other sex is unrelated or negatively associated.
1.3 Present study aims
1.3.1 Test of SAD as a risk for AUD
The aim of the present study was to extend understanding of the relations between AUD and SAD in several ways. First, we utilized the criteria outlined by Garber and Hollon (1991) to directly test whether SAD is in fact a risk factor for AUD. In other words, we examined whether Time 1 (T1) SAD was related to Time 2 (T2) AUD after controlling for T1 AUD. Consistent with prior work (Buckner et al., 2008), we hypothesized that a history of T1 SAD would be related to the onset of AUD at T2 even after controlling for other types of psychopathology common to both AUD and SAD (e.g., T1 mood, other anxiety disorders, illicit SUD, conduct disorder). We strove to extend prior work by including PTSD as a covariate and by examining these associations by sex. Given NCS data suggesting a stronger relation to AUD among women with SAD relative to men (Kessler et al., 1997), it was predicted that T1 SAD would be related to T2 AUD among women. Prior findings were also extended by examining whether observed relations between SAD and AUD were better accounted for by negative life events. Consistent with the notion that SAD is a risk for AUD (Buckner et al., 2008), it was hypothesized that negative life events would not mediate observed relations between SAD and AUD.
1.3.2 Test of underlying mechanisms
Second, the present study is the first known prospective study of possible moderators of the SAD-AUD relationship. Specifically, we tested whether T1 social support (from parents and peers) and peer alcohol use would be either protective or risk factors in the association of T1 SAD with T2 AUD. It was hypothesized that participants with T1 SAD and low levels of parental and peer support would demonstrate the greatest risk for AUD onset by T2. It was also expected that adolescents with T1 SAD and a greater number of friends who use alcohol would be at greatest risk for AUD onset by T2.
2. Method
2.1 Sample
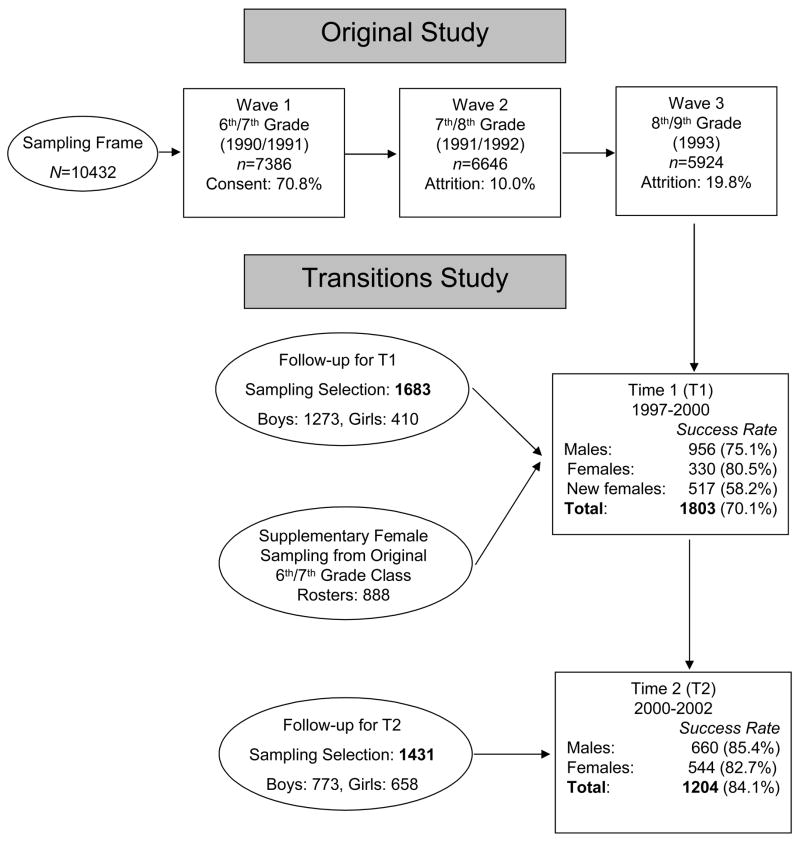
Data for the present study are from the Transitions Study, a project designed to study the substance use trajectories of two cohorts of Hispanic, African American, and non-Hispanic Caucasian young adults. The Transitions Study builds on a previously completed study of the same cohorts on whom substance use and related data were obtained at three points in time: 1990, 1991, 1993 (Vega and Gil, 1998). Two additional waves of data collection were conducted for the Transition Study. Data for Time one (T1) of the Transitions Study were gathered between 1998–2000, when the majority (93%) of respondents were between 19 and 21 years old. Transitions Time two (T2) data were collected between 2000 and 2002. The mean number of years between T1 and T2 interviews was 2.8 (SD = .6). Figure 1 summarizes the various waves of data collection.
Figure 1.
Sampling framework.
For the original study, all 48 of the Miami-Dade county’s public middle schools and all 25 public high schools (including alternative schools) participated and questionnaires were administered annually between 1990 and 1993 (beginning in grades 6 and 7 and ending when participating students were in grades 8 and 9). Detailed analyses provided assurance that the original study’s participants were highly representative of the population from which they were drawn, despite a nearly 20% attrition across the three data points (Vega and Gil, 1998).
This sample constitutes a unique contribution in several respects (Turner and Gil, 2002). First, we believe these data are from one of the largest samples of this age range thus far studied in the United States. Second, these data are among the first large-scale community studies to estimate psychiatric prevalence rates based on DSM-IV criteria. Third, half of the sample is comprised of the understudied Hispanic population of South Florida. Specifically, the original sample was drawn such that 25% were African American, 25% were of Cuban ancestry, 25% represented “other Hispanic“ backgrounds, and 25% were non-Hispanic White.
The Transitions Study consists of data collected at two follow-up assessments. For the first follow-up assessment (T1), all female participants (n = 410) and a random sample of 1,273 male participants from the original study was selected (within the confines of the race and ethnicity criteria aimed at recruiting equal numbers of white non-Hispanic, Cuban, other Hispanic, and African American participants). Because only a small number of females were included in the original study, a supplementary sample was randomly drawn from the Miami-Dade county 1990 sixth- and seventh-grade class roster. Thus, the total number of young women successfully interviewed at T1 was 847. The total T1 sample was comprised of 1803 individuals. No statistically significant differences were observed between participants in the original study and participants at T1 (see Turner and Lloyd, 2003).
A random subsample of 1431 T1 participants was invited to participate in the T2 assessment. Some were ultimately removed from the target sample due to ineligibility (reasons for ineligibility included serving in the military without leave, no longer residing in U.S., etc.); 1205 (84%) of those attempted for T2 were found and completed the T2 interview. Among the subsample of 1431 contacted for T2, there were also no statistically significant differences between those who were interviewed and those who were not (Table 1). Participants were compensated $25 for the completion of each T1 and T2 interview.
Table 1.
Demographic and psychiatric variables for participants contacted to participate in the Time 2 (T2) interview.
| Dependent Variable | T2 Participants n = 1204 | T2 Refusers n = 227 | χ2 |
|---|---|---|---|
| Gender | |||
| Male | 660 (54.8%) | 113 (49.8%) | 1.95 |
| Female | 544 (45.2%) | 114 (50.2%) | |
| Race/ethnicity | |||
| African American | 295 (24.5%) | 55 (24.3%) | .00 |
| Hispanic | 561 (46.6%) | 117 (51.8%) | 2.01 |
| Non-Hispanic White | 323 (26.8%) | 50 (22.1%) | 2.20 |
| Time 1 Lifetime Psychiatric History | |||
| Major depression | 213 (18.0%) | 39 (17.4%) | .05 |
| Dysthymia | 5 (0.4%) | 2 (0.9%) | .84 |
| Social anxiety disorder | 30 (2.5%) | 4 (1.8%) | .45 |
| Panic disorder | 24 (2.0%) | 5 (2.2%) | .04 |
| Generalized anxiety disorder | 15 (1.3%) | 3 (1.3%) | .01 |
| Post-traumatic stress disorder | 139 (11.6%) | 26 (11.6%) | .00 |
| Antisocial personality disorder | 183 (15.3%) | 29 (12.8%) | .94 |
| Attention deficit hyperactivity | 34 (2.8%) | 3 (1.3%) | 1.74 |
| Alcohol abuse | 201 (17.5%) | 29 (12.9%) | 2.87 |
| Alcohol dependence | 117 (9.7%) | 21 (15.2%) | .05 |
| Illicit substance use disorder | 335 (28.3%) | 57 (14.5%) | .71 |
Note. There were no significant differences between the groups on any demographic or psychiatric variable (all p’s > .05).
2.2 Interviewers
All interviewers held bachelor’s degrees and most had some graduate education. They were given a total of seven days of training, two days on general interviewing techniques and procedures and five days on the diagnostic interview. Except for the initial cohort of field staff, this training was followed by the observation of two interviews conducted by experienced interviewers, and being observed while conducting two. The use of portable computer-assisted personal interviews (CAPI) assured appropriate skip patterns and greatly facilitated reliable administration. Standard practice was face-to-face interviewing in the respondent’s home or in our research offices as the respondent chose. However, telephone interviews utilizing previously mailed support materials were employed for those who were away at university or who had moved elsewhere in the contiguous United States. Approximately 30% of the interviews were conducted by telephone. Although most evidence suggests that in-person and telephone interviews yield comparable data (Aktan et al., 1997; Midanick et al., 1999; Rohde et al., 1997), contrary findings have also been reported (Aquilino, 1994). The effect of interviewing mode was assessed using logistic regression. The presence versus absence of a drug-dependence diagnosis was regressed on interviewing mode with and without controls on sex and ethnicity. No evidence was found of any interviewing mode effect either within or across status categories.
2.3 Measures
2.3.1 Diagnostic Assessment
Current and lifetime occurrence of psychiatric and substance use disorders were obtained through interview modules using the Michigan Composite International Diagnostic Interview (CIDI) that was employed in the NCS (Kessler, 1994). The CIDI is a fully-structured interview, based substantially on the Diagnostic Interview Schedule (DIS) (Robins et al., 1981) and designed to be administered by non-clinicians trained in its use. Using the Michigan CIDI, as updated by NCS researchers to cover DSM-IV criteria (Kessler, personal communication), the Axis I disorders assessed were: major depression (MDD), generalized anxiety disorder (GAD), SAD, panic disorder (PD), AUD, marijuana use disorders (MUD), and PTSD. Evidence for the validity of Michigan CIDI diagnostic estimates, evaluated against structured clinical re-interviews (Spitzer et al., 1990), has been reported for most NCS disorders, including affective disorders (Blazer et al., 1994), anxiety disorders (Wittchen et al., 1995; Wittchen et al., 1996), addictive disorders (Nelson et al., 1996; Warner et al., 1995), and PTSD (Kessler et al., 1995). In addition, our assessment instrument included a reliable module (Horton et al., 1998) taken from the revised DIS with items to allow assessment of childhood conduct disorder (CD). The NCS strategy of a preliminary screening process was extended to also include the lifetime use of individual licit and illicit drugs. The goal of this extension was to reduce any fall-off in reporting that might be occasioned by learning during the course of the interview. Test-retest reliability of lifetime diagnoses was low for SAD (κ =.11) and AUD (κ =.30). For each Axis I disorder of interest, a dichotomous variable was created representing the absence (“0”) or presence (“1”) of the disorder. Forty women demonstrated a T2 AUD (28 alcohol abuse, 13 alcohol dependence) and 180 men demonstrated a T2 AUD (88 alcohol abuse, 20 alcohol dependence).
2.3.2 Negative life events
A Life History Calendar (LHC) based on that developed by Freedman et al. (1988) was used as an aid in achieving the most accurate recall of significant life course experiences (Turner and Lloyd, 2003). Forty-one items were employed to assess cumulative exposure to negative life events. Events assessed included experiences with major but not violent stressors (e.g., parental divorce, failing a grade in school), life traumas (e.g., rape, physical and emotional abuse, being injured with a weapon), witnessing violence, receiving information about bad events, and the death of relatives or close friends. A count of how many different negative life events had occurred was determined, serving as our measure of negative life events, with T1 scores ranging from 0–28 (M = 8.21, SD = 4.88).
2.3.3 Parental Support
Consistent with prior work (Barrett and Turner, 2005), parental support was assessed using three measures: Family Cohesion was assessed using a five-item scale that assessed participants’ view of the degree to which their family members share values, loyalty, and pride. In the present study, T1 scores ranged from 6–24 (M = 10.69, SD = 3.52) and demonstrated excellent reliability (α = .88). Positive Family Support was assessed using an eight-item scale that assessed the degree to which participants feels loved and cared for by their family. Present study T1 scores ranged from 8–40 (M = 13.19, SD = 5.42) with excellent reliability (α = .90). Adverse Family Relations were measured using a five-item scale that assessed the extent to which participants feel their family engages in negative interactions (e.g., criticizes, places excessive demands). T1 scores ranged from 6–30 (M = 19.14, SD = 5.32) with excellent reliability (α = .82). Higher scores on family cohesion and positive family support indicate greater levels of positive support whereas higher scores on adverse family relations measure indicate worse relationships.
2.3.4 Peer Support
Social support received from friends was assessed using an eight-item measure that utilized a Likert-type scale to assess the extent to which participants feel their friends demonstrate support. Items were rated from 1 (“strongly agree”) to 5 (“strongly disagree”). In addition, we examined perceived social support from romantic partners using a six-item measure that utilized a Likert-type scale to assess the extent to which participants feel their partners shows support. Items were rated from 1 (“strongly agree”) to 5 (“strongly disagree”). Higher scores reflect lower support. In the present sample, T1 friend support scores ranged from 8–32 (M = 12.49, SD = 4.58) and demonstrated excellent reliability (α = .85). T1 partner support scores ranged from 6–30 (M = 9.00, SD = 3.58) and also demonstrated excellent reliability (α = .85).
2.3.5 Peer alcohol use
T1 peer alcohol use was assessed using a six-point Likert-type scale that asked participants to rate from 1 (none) to 3 (a few) to 6 (all) the number of their friends “drink alcohol heavily”. For female participants in the present sample, the numbers of friends who drank alcohol heavily were as follows: none (50.7%), very few (15.7%), a few (10.2%), some (13.0%), many (7.5%), and all (2.9%). Among males, the numbers were: none (29.0%), very few (19.6%), a few (13.2%), some (19.2%), many (13.7%), and all (5.4%).
2.4 Data analytic strategy
2.4.1 Sample characteristics
First, endorsement rates of T1 variables of interest were examined by SAD status separately for men and women to determine whether differences existed between participants with T1 SAD (SAD+) and participants without T1 SAD (SAD−). Hierarchical logistic regression analyses were conducted assessing main effects and interactions using sex and SAD status (0= SAD−, 1= SAD+) as independent variables. To control for Type I error, an adjusted significance level (p < .01) was used and 99% confidence intervals reported.
2.4.2 Prospective relations
To test the hypothesis that a history of SAD would be significantly related to subsequent development of AUD, logistic regression analyses were conducted using T1 lifetime diagnoses of SAD to predict T2 past-year diagnoses, controlling for T1 lifetime AUD to ensure observed relations were not due to pre-existing AUD. Past-year diagnoses were used to assess onset of new diagnoses at T2. SAD and AUD diagnoses were the primary diagnoses of interest. However, to determine the specificity of observed relations between SAD and AUD, relevant T1 variables were also evaluated: race/ethnicity and T1 lifetime diagnoses of DSM-IV SAD, PD, GAD, PTSD, MDD, MUD, and CD.
2.4.3 Specificity of the Temporal Relations
The non-spuriousness of the relation between AUD and SAD was tested in three ways. First, a multivariate logistic regression analysis was performed in which T2 past-year AUD was regressed simultaneously on all T1 diagnoses of interest. Second, the specificity of the directionality between SAD and AUD was tested. Specifically, an additional hierarchical logistic regression analysis was conducted to assess whether T1 AUD predicted T2 past-year SAD after controlling for T1 SAD.
Third, non-spuriousness was tested by examining whether negative life event variable mediated the relationship between T1 SAD and T2 AUD (Kenny et al., 1998). The first requirement outlined by Kenny and colleagues is that the predictor variable (T1 SAD) must be correlated with the criterion (T2 AUD). The second and third requirements for testing mediation with this strategy require establishing a relation between the predictor variable and the proposed mediating variable (i.e., negative life events), and the proposed mediating variable and the criterion, respectively. To satisfy the third requirement, the proposed mediator must be associated with the criterion after controlling for the effects of the predictor. The final requirement involves evaluating the relation between the predictor and the criterion when the variance accounted for by the proposed mediator has been removed. Traditionally, when this equation yields a non-significant effect for the predictor, the controlling variable is said to mediate the relation.
2.4.4 Social Support and Peer Alcohol Use Moderator Analyses
An additional series of hierarchical logistic regressions were conducted to test the hypothesis that social support and peer use variables would interact with T1 SAD to predict T2 AUD. Separate regressions were conducted for each social support/peer use variable. In each model, T2 AUD was regressed on T1 SAD status, social support/peer use variable, and their centered interaction (Aiken and West, 1991). Covariates were entered at step 1 and included T1 AUDs, MDD, PD, PTSD, GAD, MUD, and CD. The main effects of T1 lifetime SAD status and each social support/peer use variable were entered at step 2 and the centered interaction term was entered at step 3 (Baron and Kenny, 1986). This approach ensured that observed effects for the interactions at step 3 cannot be attributed to shared variance with the variables at steps 1 and 2 (Cohen and Cohen, 1983). Significant interactions were probed using the strategies outlined by Aiken and West (1991) and Holmbeck (2002).
3. Results
3.1 Sample Characteristics
Racial/ethnic characteristics of the sample as well as the rates of the T1 Axis I diagnoses of interest are summarized on Table 2. There was a significant sex X SAD status interaction for T1 PD. There were also significant main effects of sex on several variables. Women were more likely than men to endorse Hispanic ethnicity and they demonstrated greater rates of T1 MDD, GAD, and PTSD. Men demonstrated greater rates of T1 AUD, MUD, and CD.
Table 2.
Race/ethnicity and Time 1 Axis I diagnoses by social anxiety disorder status for each sex
| Dependent | Variable | Sex | T1 SAD – (%) (n = 1748) | T1 SAD + (%) (n = 44) | OR (95% CI) | p |
|---|---|---|---|---|---|---|
| Race/ethnicity | African American | Women | 22.5 | 20.8 | Sex X SAD: OR = .17 (.02–1.58) | .12 |
| Men | 25.9 | 5.0 | ||||
| Hispanic | Women | 50.6 | 54.2 | Sex : OR = .76 (.63–.92) | .004 | |
| Men | 43.8 | 65.0 | ||||
| Non-Hispanic White | Women | 23.5 | 16.7 | Sex X SAD: OR = 1.76 (.41–7.51) | .45 | |
| Men | 27.3 | 30.0 | ||||
| Alcohol use disorder | Women | 4.3 | 20.8 | Sex : OR = 1.87 (1.50–2.34) | <.001 | |
| Men | 31.3 | 35.0 | ||||
| Panic disorder | Women | 3.5 | 4.2 | Sex X SAD: OR = 17.38 (1.22–247.35) | .04 | |
| Men | .5 | 10.0 | ||||
| Generalized anxiety disorder | Women | 2.6 | 8.3 | Sex : OR = .08 (.02–.35) | .001 | |
| Men | .2 | .0 | ||||
| Post-traumatic stress disorder | Women | 14.9 | 37.5 | Sex : OR = .47 (.34–.64) | <.001 | |
| Men | 7.6 | 25.0 | ||||
| Marijuana use disorder | Women | 17.2 | 33.3 | Sex: OR = 2.09 (1.66–2.63) | <.001 | |
| Men | 30.3 | 30.0 | ||||
| Conduct disorder | Women | 18.0 | 33.3 | Sex: OR = 2.02 (1.61–2.53) | <.001 | |
| Men | 30.6 | 30.0 | ||||
| Major depressive disorder | Women | 22.7 | 47.8 | Sex: OR = .44 (.34–.58) | <.001 | |
| Men | 11.5 | 47.4 | ||||
Note. Gender was dummy coded (female=0, male=1). SAD = social anxiety disorder. Disorder rates are lifetime diagnoses at Time 1 (T1). Hierarchical logistic regression analyses were conducted assessing main effects and interactions using gender and SAD status (0=no SAD diagnosis, 1=diagnosis) as independent variables.
The relations between T1 SAD and other T1 disorders among women were examined. T1 SAD was significantly correlated with T1 MDD (OR = 3.12, 99% CI = 1.04–9.35, p = .007) and PTSD (OR = 3.42, 99% CI = 1.12–10.44, p = .005). T1 SAD was not related to T1 MUD (OR = 2.40, 99% CI = .77–7.52, p = .048), PD (OR = 1.18, 99% CI = .08–17.186, p = .87), GAD (OR = 3.45, 99% CI = .47–25.10, p = .11), CD (OR = 2.28, 99% CI = .73–7.14, p = .06), or race/ethnicity, F(1, 838) = 1.38, p = .24.
The relations between T1 SAD and other T1 disorders were next examined among men. T1 SAD was significantly correlated with T1 MDD (OR = 6.93, 95% CI = 2.75–17.43, p < .001), PD (OR = 20.56, 95% CI = 3.74–113.07, p = .001), and PTSD (OR = 4.07, 95% CI = 1.44–11.52, p = .008). T1 SAD was not related to race/ethnicity (F(1, 948) = 4.28, p = 04), T1 GAD (OR = 0.00, p = 1.00), CD (OR = .97, 95% CI = .37–2.55, p = .97), or MUD (OR = .99, 95% CI = .38–2.59, p = .98).
3.2 Prospective Relations among Axis I Disorders
The relations between T2 AUD and T1 Axis I disorders and race/ethnicity after controlling for T1 AUD appear in Table 3. Among female participants, after controlling for T1 AUD, T2 AUD was significantly associated only with T1 SAD. Yet among male participants, T1 SAD was not significantly related to T2 AUD after controlling for T1 AUD. Thus, all subsequent analyses concerning the relations between SAD and AUD were conducted using female participants only.
Table 3.
Odds ratios and confidence intervals for relations between Time 1 predictor variables and Time 2 alcohol use disorder variables by sex
| Alcohol use disorder | ||
|---|---|---|
| Predictor Variable | Women | Men |
| Race/ethnicity | ||
| African American | .13 (.01–.95) | .61 (.32–1.14) |
| Hispanic | 1.50 (.63–3.58) | 1.27 (.83–1.94) |
| Non-Hispanic White | 1.24 (.49–3.13) | .92 (.58–1.46) |
| Marijuana use disorder | 1.78 (.66–4.75) | 2.23 (1.41–3.51)* |
| Major depressive disorder | 1.37 (.54–3.47) | 1.65 (.96–2.85) |
| Conduct disorder | 1.63 (.64–4.17) | 1.28 (.83–1.99) |
| Panic disorder | 1.01 (.14–7.37) | 2.18 (.37–12.89) |
| Generalized anxiety disorder | .86 (.06–13.12) | .00 (.00–.00) |
| Post-traumatic stress disorder | .74 (.22–2.45) | 1.48 (.76–2.85) |
|
| ||
| Social anxiety disorder | 5.48 (1.27–23.64)* | .79 (.17–3.69) |
Note. Values are expressed in odds ratios with 99% confidence intervals. Predictor variables involve Time 1 lifetime diagnoses predicting Time 2 past-year alcohol use disorder after controlling for Time 1 lifetime diagnosis of alcohol use disorder.
p < 01.
3.3 Specificity of the Temporal Relations between Social Anxiety and Alcohol Use Disorders
Multivariate logistic regression analyses suggest that T1 SAD remained the only internalizing disorder to significantly predict T2 AUD when T2 AUD was simultaneously regressed on all T1 diagnoses and race/ethnicity among women, OR = 5.44, 95% CI = 1.58–18.73, p = .007. Regarding the specificity of this pattern of temporal relations, T2 SAD was not significantly related to T1 AUD, OR = .88, 95% CI= .18–4.23, p = .88.
Because negative life events were related to both T1 SAD and T2 AUD (Table 4) thereby satisfying the first and second criteria for mediation, we examined whether the relation between T1 SAD and T2 AUD remained after controlling for the effects of negative life events. Other T1 Axis I disorders were included in the model to provide a very stringent test. T1 negative life events did not mediate the relation between T1 SAD and T2 AUD, as T1 SAD remained significantly related to T2 AUD, OR = 4.43, 95% CI = 1.29–15.22, p = .02.
Table 4.
Correlations between Time 2 alcohol use disorder and Time 1 social anxiety disorder, negative life events, social support and peer alcohol use variables (women)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Social anxiety disorder | - | |||||||||
| 2. Alcohol use disorder | .13** | - | ||||||||
| 3. Total negative life events | .10** | .08* | - | |||||||
| 4. Family cohesion | .04 | .04 | .37** | - | ||||||
| 5. Family support | .05 | .00 | .34** | .76** | - | |||||
| 6. Adverse family relations | −.05 | .00 | −.27** | −.43** | −.46** | - | ||||
| 7. Low friend support | .07* | −.02 | .09* | .25** | .27** | −.11** | - | |||
| 8. Low partner support | .12** | −.02 | .26** | .26** | .24** | −.21** | .26** | - | ||
| 9. Friends alcohol use | .02 | .17** | .08* | .09* | .04 | −.02 | .08* | .04 | - | |
| 10. Friends substance use | .04 | .20** | .15** | .14** | .11** | −.08* | .04 | .07 | .79** | - |
Note. Negative life events, social support, and peer use variables were assessed at Time 1. Time 1 diagnoses are lifetime diagnoses. Time 2 diagnoses are for the past year.
p < 0.01,
p < 0.05.
3.4 Social Support and Peer Substance Use Moderator Analyses
SAD was significantly correlated with greater number of negative life events and lower levels of partner support at T1 (Table 4). SAD was only marginally related to lower peer social support and was not significantly related to family cohesion, family support, and adverse family relations.
The following social support variables significantly moderated the link between T1 SAD and T2 AUD among women: family cohesion (OR = .65, 95% CI= .44–.96, p = .03) and adverse family relations (OR = .68, 95% CI= .46–1.00, p = .05). The following variables were not significant moderators: partner support (OR = 1.24, 95% CI= .97–1.59, p = .08), peer social support (OR = .82, 95% CI= .59–1.13, p = .22), positive parent support (OR = .83, 95% CI= .64–1.09, p = .18), and friends’ alcohol use (OR = .56, 95% CI= .28–1.14, p = .57).
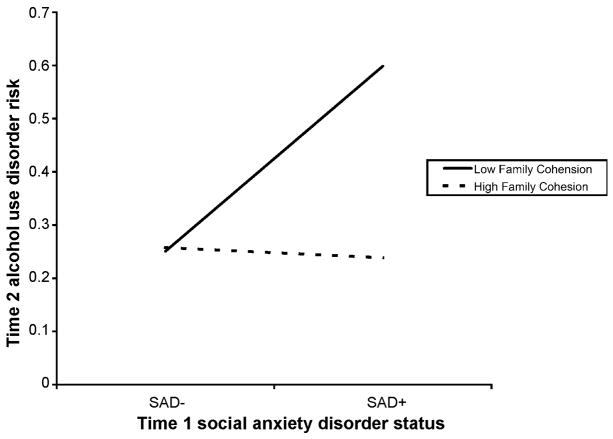
Significant interactions were probed. First, we examined whether T1 SAD+ and T1 SAD− women differed on their rate of T2 AUD as a function of family cohesion. T1 SAD+ women with low family cohesion exhibited the highest rates of T2 AUD (Figure 2). Among those with low family cohesion, the difference between T1 SAD+ and T1 SAD− women was significant, t(1, 830) = 4.63, p < .001. However, the slope was not significant for women with high family cohesion (t(1, 830) = 1.31, p = .19), suggesting that among those with high family cohesion, T1 SAD no longer predicted T2 AUD. Further, among T1 SAD+ women, those with low family cohesion had significantly higher rates of T2 AUD than T1 SAD+ women with high family cohesion, t(1, 830) = −2.64, p = .008. This difference was not significant among T1 SAD−women, t(1, 830) = 1.57, p = .12.
Figure 2.
Rates of time 2 alcohol use disorder among SAD+ and SAD− young women as a function of family cohesion and pride.
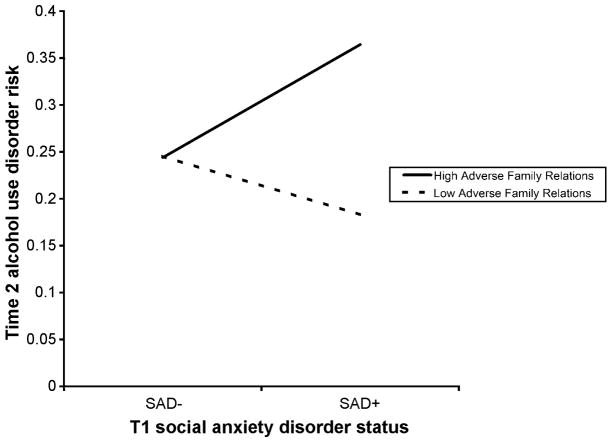
Second, we tested whether T1 SAD+ and T1 SAD− women differed on their rate of T2 AUD as a function of adverse family relations. T1 SAD+ women with high adverse family relations exhibited the highest rates of T2 AUD (Figure 3). Among those with high adverse family relations, the difference between T1 SAD+ and T1 SAD− women was significant, t(1, 836) = 5.15, p < .001. The slope was also significant for women with low adverse family relations (t(1, 836) = 2.11, p = .04), indicating that T1 SAD+ and T1 SAD− women differed in their rate of T2 AUD as a function of adverse family relations. Further, among T1 SAD+ women, those with high adverse family relations had significantly higher rates of T2 AUD than T1 SAD+ women with low adverse family relations, t(1, 836) = 3.49, p = .001. This difference was not significant among T1 SAD− women, t(1, 836) = −.25, p = .80.
Figure 3.
Rates of time 2 alcohol use disorder among SAD+ and SAD− young women as a function of adverse family relations.
4. Discussion
The present investigation is the first known study to examine the relationships between SAD and AUD using the gold standard criteria for assessing causality in psychosocial research (see Garber and Hollon, 1991). Results support prior work (Buckner et al., 2008) suggesting that SAD appears to be a risk for the subsequent onset of AUD. The present study furthers knowledge regarding the relations between AUD and SAD in several key ways. First, we examined the temporal relations between AUD and SAD separately by sex and determined that AUD risk is particularly increased in SAD+ young women, but not their male counterparts. Second, this investigation is the first known prospective examination of possible explanatory pathways by which SAD+ young women go on to develop AUD. Specifically, results indicate that familial interactions appears to play an important role in the development of AUD among SAD+ young women.
4.1 SAD as a risk for AUD
Data from the present study are consistent with theoretical and empirical work indicating that SAD is a risk factor for AUD (e.g., Buckner et al., 2008; Morris et al., 2005). The causal significance of SAD is suggested by findings that satisfy the criteria considered to be the gold standard in testing whether one variable is a risk factor for another in psychosocial research (Garber and Hollon, 1991). The present investigation is one of the very few to examine the non-spuriousness criterion for causality. Findings suggest that the link between T1 SAD and T2 AUD among young women was not better accounted for by a variety of third variables common to both SAD and AUD. In fact, we used a very stringent strategy that controlled for numerous DSM-IV Axis I disorders (i.e., PD, PTSD, GAD, MDD, MUD, CD). The finding that T1 SAD remained significantly related to T2 AUD after controlling for these disorders is particularly noteworthy given that both SAD and AUD demonstrate high rates of these disorders (Buckner et al., 2008; Grant et al., 2005; Kessler et al., 1997).
The present study also built upon prior work by testing the specificity of the directionality of the relation between SAD and AUD. Results indicate that the causal directionality is fairly specific, with SAD increasing risk of subsequent AUD but AUD does not appear to increase SAD vulnerability. However, this finding does not preclude the possibility that, over time, the experience of AUD and its associated impairment could increase the risk of SAD among some vulnerable individuals (e.g., those with elevated trait shyness; see Buckner et al., in press) and future work over longer timeframes is necessary to further delineate the directionality of these relationships.
We further tested the non-spuriousness of the prospective SAD-AUD relation by examining whether negative life events were “third variables” that accounted for the apparently specific temporal relation between these two disorders. Although number of negative life events was positively correlated with both SAD and AUD, they did not appear to account for the prospective relationship between SAD and AUD among young women (Kenny et al., 1998). Data from the present study combined with past work (Buckner et al., 2008) provide preliminary support for the non-spuriousness of the prospective relation between SAD and AUD among women.
4.2 Specificity of SAD
It is particularly noteworthy that no other mood or anxiety disorder appeared to increase AUD vulnerability. This finding is consistent with other work finding that after controlling for relevant demographic and psychiatric variables, other internalizing states (e.g., MDD) did not prospectively predict AUD in a combined-sex sample and among women in particular (Gilman and Abraham, 2001). Our data are also in line with prior research finding that, after controlling for relevant Axis I pathology, the prospective relations between conditions such as depression and AUD are reduced to non-significance (Buckner et al., 2008). In addition, our data are consistent with other work finding that problematic substance use typically precedes the onset of other anxiety conditions (Kessler et al., 2002; Zvolensky et al., 2006).
The identification of SAD as a potentially specific risk factor for the development of AUD is not trivial, as it may have important implications for current theoretical models of AUD. For instance, classic models of substance use including the tension-reduction model (Conger, 1956), motivational models (Cooper et al., 1995), and stress-dampening models (Levenson and et al., 1980) all posit that the use of alcohol to manage negative affect increases AUD risk. In other words, these models propose that negative affect is a risk for problematic alcohol use. However, our data, in conjunction with prior work (Buckner et al., 2008), suggest that it is not negative affect generally that increases AUD risk (at least among females), given the weak association between T1 mood and other anxiety disorders and T2 AUD. Rather, it appears that specific types of negative affect are associated with AUD risk, among which SAD appears to be one. Specifically, it appears that SAD+ women may be vulnerable to using alcohol to manage negative affect thereby increasing AUD risk, whereas individuals with other anxiety conditions may experience anxiety as a consequence of problematic alcohol use.
4.3 Sex specificity of prospective link between SAD and AUD
The present study is the first know examination of the prospective relations between SAD and AUD separately by sex. Results suggest that it is SAD among young women (but not young men) that is related to the onset of subsequent AUD. These data are in line with preliminary evidence that substance-related impairment appears to co-occur with SAD among women in particular (Buckner et al., 2006b; Kessler et al., 1997) and raises the question as to what about SAD in women increases their AUD risk. Family studies may shed some light on these relations. Although studies examining the relations between SAD and AUD by sex are scant, there are some data suggesting there may be a genetic underpinning to the high rates of co-occurring SAD-AUD among women (Merikangas et al., 1996; Nelson et al., 2000). However, understanding the particular risk of AUD among women with SAD is in its infancy and future work examining mechanisms underlying these associated is warranted.
4.3 Psychosocial mechanisms underlying the link between SAD and AUD
Our data indicate that interactions with parents appear to play a critical role in the development of AUD among SAD+ young women. Specifically, SAD+ females appear particularly vulnerable to the effects of adverse family interactions. Theories of social anxiety posit that negative parental interactions (e.g., rejection) are implicated in the genesis and/or maintenance of social anxiety (Bruch et al., 1989) and empirical evidence supports the contention that parents of socially anxious individuals exhibit negative interactions with their children (Boegels et al., 2001; Hummel and Gross, 2001; Lieb et al., 2000; Rapee, 1997). Although we know of no study that has examined the relations between adverse family interactions and SAD by sex, there are data indicating that in families in which parents are highly critical of their children, females tend more submissive to their parents and less likely to make attempts to gain control in interactions relative to males (Wuerker et al., 1999). It may be that in families with high levels of adverse interactions, males are more likely to engage in active strategies to overcome familial adversity whereas females are more likely to engage in strategies to avoid further adversity. These young women may at some point learn to use alcohol as an avoidance strategy. Future work examining the role of avoidance coping strategies in AUD vulnerability among SAD+ women is warranted to directly test this hypothesis.
In addition to the identification of factors that increase the risk of AUD among SAD+ young women, our data suggest that at least some familial factors may protect SAD+ women from elevated AUD risk. Specifically, results indicate that the experience of high family cohesion and pride appears to protect these high-risk women (i.e., SAD+ women) from developing AUD at greater rates than SAD− women. This finding is consistent with prior work suggesting that family cohesion tends to protect at-risk individuals from alcohol and other substance use (Kliewer et al., 2006). The novel finding that family cohesion may protect SAD+ women from greater AUD vulnerability suggests it may be important for future work to examine the utility of prevention efforts that target parenting skills among parents of high-risk SAD+ females.
Notably, social support from peers and peer alcohol use behaviors did not increase AUD risk among SAD+ young women. This finding appears counter to prior work evidence indicating that social anxiety among young adults was related to drinking in situations involving perceived peer pressure (Buckner et al., 2006a) and to avoid social censure (Stewart et al., 2006). However, those studies relied on cross-sectional reports. It may be that previously observed links between social anxiety and peer use variables were a sequelae of alcohol use and not causal. Our pattern of findings suggests that SAD+ young women are not necessarily vulnerable to using alcohol as a result of peer alcohol use. Rather, initiation of problematic alcohol use appears to be more heavily influenced by family interactions. Once SAD+ females begin using alcohol, however, they may be more likely to seek out alcohol-using friends, perhaps as a means to avoid negative evaluation by non-alcohol-using peers. This pattern may create a vicious cycle of alcohol use whereby SAD+ women then use alcohol to avoid negative evaluation by drinking peers (Buckner et al., 2006a; Stewart et al., 2006) as well as for social facilitation (O’Hare, 1990) and to manage negative affect (Buckner et al., 2006a; Stewart et al., 2006).
4.3 Limitations and future directions
The present findings should be considered in light of limitations that indicate further work is needed in this area. First, there were few subjects in some diagnostic categories, resulting in odds ratios with large confidence intervals and replication with samples comprised of larger numbers of individuals with internalizing disorders will strengthen confidence in the observed pattern of findings. Second, a relatively short timeframe of approximately 3 years was utilized and future work examining the relations between SAD and AUD over longer periods of time will go a long way toward demarcating the complex relations between these two disorders across the lifespan. Third, our assessment of peer alcohol use relied on a single item that assessed participants’ perception of peer alcohol use versus actual peer alcohol use. Although our findings are an important first step in the assessment of the influence of peer alcohol use on the relations between SAD and AUD, future work could benefit from a multi-method, multi-informant approach. Fourth, test-retest reliability of lifetime diagnoses of SAD and AUD were low. Low reliability rates among adolescent samples (particularly for anxiety disorders) have been reported elsewhere (e.g., Schwab-Stone et al., 1996). Adolescent and young adult samples are vulnerable to lower test-retest reliability for a variety of reasons (see Reich, 2000). The most likely explanation for the low reliability rates in the present study is that participants may have learned they could shorten the T2 interview by answering no, thereby avoiding follow-up questions. Thus, although this practice may have resulted in diagnosis of fewer AUD cases at T2, this drop in T2 AUD cases likely resulted in a lesser rather than stronger association between T1 AUD and T1 SAD. Despite the low test-retest reliability of lifetime diagnoses, results are consistent with a growing body of work in this area that suggests SAD onset tends to occur prior to AUD onset (Buckner et al., in press; Buckner et al., 2008; Randall et al. 2001). A noteworthy strength of this study was its racially diverse sample. Given that prior work utilized samples that were comprised primarily of non-Hispanic Caucasian participants (Buckner et al., 2008) or did not report the racial composition of their sample (Zimmermann et al., 2003), the use of such a racially and ethnically diverse sample increases the generalizability of study findings (Buckner et al., 2007).
4.4 Conclusions
The present study is the most stringent test to date of the contention that SAD may increase AUD vulnerability above and beyond a variety of relevant factors. Moreover, the temporal relationship between SAD and AUD appears relatively specific, as no such effect was evident for other internalizing disorders (i.e., MDD, other anxiety disorders). Further, AUD did not predict the subsequent onset of SAD among women, providing initial support for the specificity of the directionality of these relationships. Importantly, this study is the first known prospective investigation to examine causal mechanisms that may account for the high risk of AUD among SAD+ young women. The identification of the role family interactions appears to play in the development of AUD among SAD+ women is a crucial first step in understanding the nature of AUD risk among this particularly vulnerable group. Future work aimed at uncovering additional risk and protective factors will go a long way toward informing much-needed prevention and treatment efforts for this high-risk population.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- Aktan GB, Calkins RF, Ribisl KM, Kroliczak A, Kasim RM. Test-retest reliability of psychoactive substance abuse and dependence diagnoses in telephone interviews using a modified diagnostic interview schedule-substance abuse module. Am J Drug Alcohol Abuse. 1997;23:229–248. doi: 10.3109/00952999709040944. [DOI] [PubMed] [Google Scholar]
- Aquilino WS. Interview mode effects in surveys of drug and alcohol use: A field experiment. Public Opin Q. 1994;58:210–240. [Google Scholar]
- Barnow S, Schuckit MA, Lucht M, John U, Freyberger H-J. The importance of a positive family history of alcoholism, parental rejection and emotional warmth, behavioral problems and peer substance use for alcohol problems in teenagers: A path analysis. J Stud Alcohol. 2002;63:305–315. doi: 10.15288/jsa.2002.63.305. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrett AE, Turner RJ. Family Structure and Mental Health: The Mediating Effects of Socioeconomic Status, Family Process, and Social Stress. J Health Soc Behav. 2005;46:156–169. doi: 10.1177/002214650504600203. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- Boegels SM, van Oosten A, Muris P, Smulders D. Familial correlates of social anxiety in children and adolescents. Behav Res Ther. 2001;39:273–287. doi: 10.1016/s0005-7967(00)00005-x. [DOI] [PubMed] [Google Scholar]
- Bruch MA, Gorsky JM, Collins TM, Berger PA. Shyness and sociability reexamined: A multicomponent analysis. J Pers Soc Psychol. 1989;57:904–915. [Google Scholar]
- Bruch MA, Heimberg RG. Differences in perceptions of parental and personal characteristics between generalized and nongeneralized social phobics. J Anxiety Disord. 1994;8:155–168. [Google Scholar]
- Buckner JD, Castro Y, Holm-Denoma JM, Joiner TE., Jr . Mental Health Care for People of Diverse Backgrounds. Radcliffe Publishing, Abingdon; United Kingdom: 2007. [Google Scholar]
- Buckner JD, Eggleston AM, Schmidt NB. Social anxiety and problematic alcohol consumption: The mediating role of drinking motives and situations. Behav Ther. 2006a;37:381–391. doi: 10.1016/j.beth.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Mallott MA, Schmidt NB, Taylor J. Peer influence and gender differences in problematic cannabis use among individuals with social anxiety. J Anxiety Disord. 2006b;20:1087–1102. doi: 10.1016/j.janxdis.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. Understanding social anxiety as a risk for alcohol use disorders: Fear of scrutiny, not social interaction fears, prospectively predicts alcohol use disorders. J Psychiatr Res. doi: 10.1016/j.jpsychires.2008.04.012. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small J, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Timpano KR, Zvolensky MJ, Sachs-Ericsson N, Schmidt NB. Implications of comorbid alcohol dependence among individuals with social anxiety disorder. Depress Anxiety. doi: 10.1002/da.20442. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrigan MH, Randall CL. Self-medication in social phobia: A review of the alcohol literature. Addict Behav. 2003;28:269–284. doi: 10.1016/s0306-4603(01)00235-0. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Lawrence Erlbaum Associates; Hillsdale, NJ: 1983. [Google Scholar]
- Conger JJ. Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Q J Stud Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. J Pers Soc Psychol. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Crum RM, Pratt LA. Risk of heavy drinking and alcohol use disorders in social phobia: A prospective analysis. Am J Psychiatry. 2001;158:1693–1700. doi: 10.1176/appi.ajp.158.10.1693. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Hughes DL, George LK, Blazer DG. The epidemiology of social phobia: Findings from the Duke Epidemiological Catchment Area Study. Psychol Med. 1993;23:709–718. doi: 10.1017/s0033291700025484. [DOI] [PubMed] [Google Scholar]
- Freedman D, Thorton A, Camburn D, Alwin D, Young-DeMarco L. The life history calendar: A technique for collecting retrospective data. In: Clogg CC, editor. Socioogical Methodoogy. Institute for Social Research, University of Michigan; Ann Arbor, MI: 1988. [PubMed] [Google Scholar]
- Garber J, Hollon SD. What can specificity designs say about causality in psychopathology research? Psychol Bull. 1991;110:129–136. doi: 10.1037/0033-2909.110.1.129. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Abraham HD. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alcohol Depend. 2001;63:277–286. doi: 10.1016/s0376-8716(00)00216-7. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Blanco C, Stinson FS, Chou SP, Goldstein RB, Dawson DA, Smith S, Saha TD, Huang B. The epidemiology of social anxiety disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- Groh DR, Jason LA, Davis MI, Olson BD, Ferrari JR. Friends, family, and alcohol abuse: An examination of general and alcohol-specific social support. Am J Addict. 2007;16:49–55. doi: 10.1080/10550490601080084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham LS, Carrigan MH, Moak DH, Randall CL. Social anxiety and specificity of positive alcohol expectancies: Preliminary findings. J Psychopathol Behav Assess. 2005;27:115–121. [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. J Pediatr Psychol. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Horton J, Compton WM, Cottler LB. Assessing psychiatric disorders among drug users: Reliability of the revised DSM-IV. In: Harris L, editor. Problems of Drug Dependence NIDA research monograph, NIH publication no 9. National Institute of Drug Addiction; Washington, DC: 1998. pp. 43–95. [Google Scholar]
- Hummel RM, Gross AM. Socially anxious children: An observational study of parent–child I interaction. Child Fam Behav Ther. 2001;23:19–41. [Google Scholar]
- Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. In: Gilbert DT, Fiske ST, Lindzey G, editors. The Handbook of Social Psychology. McGraw-Hill; New York: 1998. pp. 233–265. [Google Scholar]
- Kessler RC. The National Comorbidity Survey of the United States. Int Rev Psychiatry. 1994;6:365–376. [Google Scholar]
- Kessler RC, Andrade LH, Bijl RV, Offord DR, Demler OV, Stein DJ. The effects of co-morbidity on the onset and persistence of generalized anxiety disorder in the ICPE surveys. Psychol Med. 2002;32:1213–1225. doi: 10.1017/s0033291702006104. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kliewer W, Murrelle L, Prom E, Ramirez M, Obando P, Sandi L, del Carmen Karenkeris M. Violence Exposure and Drug Use in Central American Youth: Family Cohesion and Parental Monitoring as Protective Factors. J Res Adolesc. 2006;16:455–478. [Google Scholar]
- La Greca AM, Lopez N. Social anxiety among adolescents: Linkages with peer relations and friendships. J Abnorm Child Psychol. 1998;26:83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]
- Levenson RW, Sher KJ, Grossman LM, Newman J, Newlin DB. Alcohol and stress response dampening: Pharmacological effects, expectancy, and tension reduction. J Abnorm Psychol. 1980;89:528–538. doi: 10.1037//0021-843x.89.4.528. [DOI] [PubMed] [Google Scholar]
- Lieb R, Wittchen H-U, Höfler M, Fuetsch M, Stein MB, Merikangas KR. Parental psychopathology, parenting styles, and the risk of social phobia in offspring: A prospective-longitudinal community study. Arch Gen Psychiatry. 2000;57:859–866. doi: 10.1001/archpsyc.57.9.859. [DOI] [PubMed] [Google Scholar]
- Lloyd DA, Turner RJ. Cumulative lifetime adversity and alcohol dependence in adolescents and young adults. Drug Alcohol Depend. 2008;93:217–222. doi: 10.1016/j.drugalcdep.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Stevens D, Fenton B. Comorbidity of alcoholism and anxiety disorders: The role of family studies. Alcohol Health Res World. 1996;20:100–106. [PMC free article] [PubMed] [Google Scholar]
- Midanick LT, Hines AM, Greenfield TK. Face to face versus telephone interviews: Using cognitive methods to assess alcohol survey questions. Contemp Drug Probl. 1999;26:673–693. [Google Scholar]
- Morris EP, Stewart SH, Ham LS. The relationship between social anxiety disorder and alcohol use disorders: A critical review. Clin Psychol Rev. 2005;25:734–760. doi: 10.1016/j.cpr.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Nelson CB, Little RJA, Heath AC, Kessler RC. Patterns of DSM-III-R alcohol dependence symptom progression in a general population survey. Psychol Med. 1996;26:449–460. doi: 10.1017/s0033291700035534. [DOI] [PubMed] [Google Scholar]
- Nelson EC, Grant JD, Bucholz KK, Glowinski A, Madden PAF, Reich W, Heath AC. Social phobia in a population-based female adolescent twin sample: Co-morbidity and associated suicide-related symptoms. Psychol Med. 2000;30:797–804. doi: 10.1017/s0033291799002275. [DOI] [PubMed] [Google Scholar]
- O’Hare TM. Alcohol expectancies and social anxiety in male and female undergraduates. Addict Behav. 1990;15:561–566. doi: 10.1016/0306-4603(90)90057-5. [DOI] [PubMed] [Google Scholar]
- Patock-Peckham JA, Morgan-Lopez AA. College drinking behaviors: Mediational links between parenting styles, parental bonds, depression, and alcohol problems. Psychol Addict Behav. 2007;21:297–306. doi: 10.1037/0893-164X.21.3.297. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Project MATCH: Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: A first step toward developing effective treatments. Alcohol Clin Exp Res. 2001;25:210–220. [PubMed] [Google Scholar]
- Rapee RM. Potential role of childrearing practices in the development of anxiety and depression. Clin Psychol Rev. 1997;17:47–67. doi: 10.1016/s0272-7358(96)00040-2. [DOI] [PubMed] [Google Scholar]
- Reich W. Diagnostic interview for children and adolescents (DICA) J Am Acad Child Adolesc Psychiatry. 2000;39:59–66. doi: 10.1097/00004583-200001000-00017. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan JL, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Schneier FR, Martin LY, Liebowitz MR, Gorman JM, Fyer AJ. Alcohol abuse in social phobia. J Anxiety Disord. 1989;3:15–23. [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, Goodman SH, Lahey BB, Lichtman JH, Canino G, Rubio-Stipec M, Rae DS. Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3) J Am Acad Child Adolesc Psychiatry. 1996;35:878–88. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Sinha R, Robinson J, O’Malley S. Stress response dampening: Effects of gender and family history of alcoholism and anxiety disorders. Psychopharmacology (Berl) 1998;137:311–320. doi: 10.1007/s002130050624. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R: Patient Edition (SCID-P), Version 1.0. American Psychiatric Association; Washington, DC: 1990. [Google Scholar]
- Stewart SH, Morris E, Mellings T, Komar J. Relations of social anxiety variables to drinking motives, drinking quantity and frequency, and alcohol-related problems in undergraduates. Journal of Mental Health. 2006;15:671–682. [Google Scholar]
- Thevos AK, Thomas SE, Randall CL. Baseline differences in social support among treatment-seeking alcoholics with and without social phobia. Substance Abuse. 1999;20:107–121. doi: 10.1080/08897079909511399. [DOI] [PubMed] [Google Scholar]
- Thomas SE, Thevos AK, Randall CL. Alcoholics with and without social phobia: A comparison of substance use and psychiatric variables. J Stud Alcohol. 1999;60:472–479. doi: 10.15288/jsa.1999.60.472. [DOI] [PubMed] [Google Scholar]
- Torgrud LJ, Walker JR, Murray L, Cox BJ, Chartier M, Kjernisted KD. Deficits in perceived social support associated with generalized social phobia. Cogn Behav Ther. 2004;33:87–96. doi: 10.1080/16506070410029577. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Gil AG. Psychiatric and substance use disorders in South Florida: Racial/ethnic and gender contrasts in a young adult cohort. Arch Gen Psychiatry. 2002;59:43–50. doi: 10.1001/archpsyc.59.1.43. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: Racial/ethnic contrasts. Addiction. 2003;98:305–315. doi: 10.1046/j.1360-0443.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Stress burden and the lifetime incidence of psychiatric disorder in young adults: Racial/ethnic contrasts. Arch Gen Psychiatry. 2004;61:481–488. doi: 10.1001/archpsyc.61.5.481. [DOI] [PubMed] [Google Scholar]
- Vega WA, Gil AG. Drug Use and Ethnicity in Early Adolescence. Plenum Press; New York: 1998. [Google Scholar]
- Warner LA, Kessler RC, Hughes M, Anthony JC, Nelson CB. Prevalence and correlates of drug use and dependence in the United States: Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:219–229. doi: 10.1001/archpsyc.1995.03950150051010. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Kessler RC, Zhao S, Abelson J. Reliability and clinical validity of UM-CIDI DSM-III-R generalized anxiety disorder. J Psychiatr Res. 1995;29:95–110. doi: 10.1016/0022-3956(94)00044-r. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Zhao S, Abelson JM, Abelson JL, Kessler RC. Reliability and procedural validity of UM-CIDI DSM-III--R phobic disorders. Psychol Med. 1996;26:1169–1177. doi: 10.1017/s0033291700035893. [DOI] [PubMed] [Google Scholar]
- Wuerker AK, Haas GL, Bellack AS. Racial and gender differences in expressed emotion and interpersonal control in families of persons with schizophrenia. Fam Process. 1999;38:477–496. doi: 10.1111/j.1545-5300.1999.00477.x. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Wittchen H-U, Höfler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: A 4-year community study of adolescents and young adults. Psychol Med. 2003;33:1211–1222. doi: 10.1017/s0033291703008158. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Sachs-Ericsson N, Schmidt NB, Buckner JD, Bonn-Miller MO. Lifetime associations between cannabis, use, abuse, and dependence and panic attacks in a representative sample. J Psychiatr Res. 2006;40:477–786. doi: 10.1016/j.jpsychires.2005.09.005. [DOI] [PubMed] [Google Scholar]