Abstract
We propose that excessive fructose intake (>50 g/d) may be one of the underlying etiologies of metabolic syndrome and type 2 diabetes. The primary sources of fructose are sugar (sucrose) and high fructose corn syrup. First, fructose intake correlates closely with the rate of diabetes worldwide. Second, unlike other sugars, the ingestion of excessive fructose induces features of metabolic syndrome in both laboratory animals and humans. Third, fructose appears to mediate the metabolic syndrome in part by raising uric acid, and there are now extensive experimental and clinical data supporting uric acid in the pathogenesis of metabolic syndrome. Fourth, environmental and genetic considerations provide a potential explanation of why certain groups might be more susceptible to developing diabetes. Finally, we discuss the counterarguments associated with the hypothesis and a potential explanation for these findings. If diabetes might result from excessive intake of fructose, then simple public health measures could have a major impact on improving the overall health of our populace.
I. Introduction
II. Unique Characteristics of Fructose Metabolism
III. Fructose Causes Metabolic Syndrome in Animals
IV. Mechanism(s) for Fructose-Induced Insulin Resistance
V. Mechanism(s) by Which Fructose Induces Other Features of the Metabolic Syndrome: Role of Uric Acid
VI. Human Studies with Fructose
VII. Epidemiological Studies: Sugar Intake and Type 2 Diabetes
VIII. Epidemiological Studies: Uric Acid and Type 2 Diabetes
IX. Do Other Conditions That Modify Uric Acid Levels Affect the Development of Metabolic Syndrome or Diabetes?
X. Twelve Countering Arguments and Caveats
XI. The Thrifty Gene Revisited
XII. What Research Should Be Done to Prove Our Hypothesis?
I. Introduction
Although diabetes was described by Aretaeus, Galen, and Paracelsus, by the mid to late 1800s William Prout (1) and others recognized that diabetes could have two presentations: one manifesting as a rapidly progressive and wasting condition in a thin and feeble individual (likely type 1 diabetes), and a slower and more progressive disease in an overweight or obese subject (likely type 2 diabetes) (1,2). Both conditions were rare; indeed, Osler (3) projected a prevalence of approximately two or three cases per 100,000 population in Europe and North America. By the early 1900s, however, a remarkable rise in the prevalence of the second type of diabetes was observed in Europe and the United States (4). Similarly, a dramatic increase in diabetes was observed in a number of tropical countries (5). In these early reports, the type of subject developing diabetes was often wealthy, overweight, and living in an urban environment (4,5). However, over the last 50 yr there has been a transition such that diabetes is now increasing most rapidly among the poor and minorities (6). Although some of the increase in diabetes prevalence may be due to the increasing longevity of the population, an increase in the rate of type 2 diabetes is also being observed among the young, suggesting that an active process is driving the epidemic. Today diabetes is present in over 217 million individuals worldwide. Approximately 7% of the U.S. adult population has type 2 diabetes that carries a yearly financial burden of over $130,000,000,000 (7). Over the next few decades a remarkable increase in diabetes is projected, especially in Asia and India (8). By 2030, over 350 million people are projected to suffer from this condition, making it one of the most serious diseases of humankind (7,8).
Identifying the etiology of type 2 diabetes is key to prevention. The frequent association of diabetes with obesity has led many investigators to propose that obesity may be responsible for up to 90% of type 2 diabetes (9). Obesity, and in particular intraabdominal fat accumulation, has been shown to induce insulin resistance via several mechanisms, and insulin resistance is considered the central pathogenic mechanism underlying type 2 diabetes (10). Nevertheless, studies in certain populations, such as Asians, have documented high rates of type 2 diabetes in the absence of classical obesity (11,12). There are also many obese subjects that do not have diabetes. This suggests that whereas obesity may be a risk factor, other pathogenic factors may exist that could contribute to the epidemic of type 2 diabetes. Furthermore, whereas central obesity is a likely mechanism for the development of diabetes, Kahn and Flier (10) have also stated that “it is possible that an unknown common factor, either genetic or environmental, produces both insulin resistance and the central pattern of regional adiposity.”
Although insulin resistance is characteristic of the subject with type 2 diabetes, insulin resistance also precedes its development. Indeed, a major breakthrough was the observation that diabetes is often presaged by a constellation of signs associated with insulin resistance, which has since been described as the “metabolic syndrome.” Although recognized by several investigators during the last century (13,14,15,16,17,18,19), the presence of this syndrome was best characterized by Reaven (20) in the late 1980s. The metabolic syndrome is currently defined as having at least three of five characteristic signs (abdominal obesity, impaired fasting glucose, hypertriglyceridemia, low high-density lipoprotein (HDL) cholesterol, and elevated blood pressure) (21). However, other conditions are also associated with metabolic syndrome, including fatty liver (nonalcoholic steatohepatitis), mild kidney disease, and the presence of endothelial dysfunction, systemic inflammation, and oxidative stress. Today the metabolic syndrome affects over 55 million (26.7%) individuals in the United States, and rates continue to rise (22).
More recently there has developed a debate over whether the metabolic syndrome is clinically useful above and beyond its individual components and whether it should be considered a disease entity (23,24). Some studies also suggest that the metabolic syndrome represents multiple clusters of signs (25). On the other hand, if the syndrome represented a common pathway for the development of diabetes, as suggested by one study (26), then considering metabolic syndrome a disease entity would be reasonable.
In this paper we present the hypothesis that many cases of metabolic syndrome, as well as type 2 diabetes, may have a single etiology. Specifically, we revisit the old hypothesis that excessive intake of sugar, and in particular fructose, may be an important cause of type 2 diabetes. We define excessive intake of fructose as more than 50 g/d based on population studies suggesting that obesity rates are greater than 10% when mean intake increases beyond this amount (27). The hypothesis that sugar consumption might predispose to diabetes was entertained by the famous diabetologist, Frederick Allen (28), as well as by other investigators of the early 20th century (4,5,29). The hypothesis was resurrected in the 1960s, particularly by Campbell and Yudkin (30,31,32,33,34), but it has largely been eschewed, and restriction of sugar has not been recommended as a means to prevent diabetes by the American Diabetes Association (35).
However, recent studies from our group and others have provided evidence for how sucrose, and in particular its component fructose, may cause diabetes. Fructose intake is associated with the metabolic syndrome, thus supporting this latter condition as a disease entity. Furthermore, fructose appears to cause insulin resistance through classic (adiposity based) mechanisms as well as mechanisms independent of energy intake or weight gain (36,37). To better understand how fructose acts, we will first review certain unique characteristics of its metabolism.
II. Unique Characteristics of Fructose Metabolism
Fructose is a simple sugar that is present in fruits and honey and is responsible for their sweet taste. However, the major source of fructose worldwide is sucrose, or table sugar, which is derived from sugar cane and sugar beets. Sucrose is a disaccharide that consists of 50% fructose and 50% glucose. After ingestion, sucrose is degraded in the gut by sucrase, releasing free fructose and glucose that are then absorbed. In addition to sucrose, the other major source of fructose is high fructose corn syrup (HFCS), which was introduced in the early 1970s as an additional sweetener. HFCS consists of free fructose and glucose mixed in a variety of concentrations, but most commonly as 55% fructose and 45% glucose. In the United States, HFCS and sucrose are the major source of fructose in the diet, and HFCS is often a major ingredient in soft drinks, pastries, desserts, and various processed foods.
Fructose is absorbed in the intestine via specific transporters [glucose transporter 5 (Glut 5), Glut 2, and possibly SLC2A9] and undergoes metabolism largely (50–75%) by the liver, with the rest being primarily metabolized by the kidney and adipocytes (38,39). Although fasting concentrations are low (10–60 μm), postprandial concentrations may reach 2.2 mm in the portal system and 1 mm systemically (40,41,42).
The uptake of fructose by cells is largely mediated by Glut 5 and Glut 2 transporters, followed by metabolism by fructokinase (ketohexokinase, KHK) (Fig. 1). Fructokinase may exist in two isoforms, of which KHK-C appears to be the principal isoform involved in fructose metabolism (43). The dominant sites of KHK-C expression include the liver, the intestinal epithelium, the proximal tubule of the kidney, the adipocyte, and possibly the vascular endothelium (43,44,45). Fructose may also be metabolized by hexokinase (glucokinase); however, the Km for fructose is much higher than glucose, and hence minimal amounts of fructose are metabolized via this pathway (38).
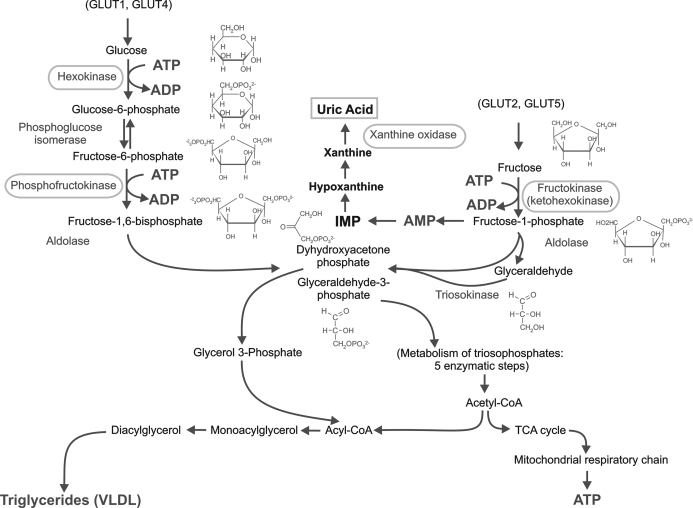
Figure 1.
Fructose metabolism. Fructose enters cells via a transporter (typically Glut 5, Glut 2, or SLC2A9) where it is preferentially metabolized by fructokinase (KHK) to generate fructose-1-phosphate. Unlike phosphofructokinase, which is involved in glucose metabolism, fructokinase has no negative feedback system to prevent it from continuing to phosphorylate substrate, and as a consequence ATP can be depleted, causing intracellular phosphate depletion, activation of AMP deaminase, and uric acid generation. In addition, fructose is lipogenic and can generate both glycerol phosphate and acyl coenzyme A, resulting in triglyceride formation that is both secreted and stored in hepatocytes. IMP, Inosine monophosphate; TCA, trichloroacetic acid.
Fructose differs from glucose primarily due to its different transporters and the first three enzymes involved in its metabolism (Fig. 1). A key enzyme is fructokinase, which uses ATP to phosphorylate fructose to fructose-1-phosphate. Unlike enzymes involved in glucose metabolism (glucokinase and phosphofructokinase), in which downstream metabolites prevent excessive phosphorylation, fructokinase is poorly regulated and will phosphorylate all fructose rapidly with the depletion of ATP (46). The administration of fructose rapidly depletes ATP in human liver (47,48). Similarly, concentrations of fructose as low as 1.0 mm (similar to that observed postprandially in plasma after a fructose-enriched meal) can significantly reduce ATP levels in vascular endothelial cells (45) and human proximal tubular cells (44). The effect of fructose to cause ATP depletion acts like a type of ischemia and can cause transient arrest of protein synthesis (46,47) and the production of inflammatory proteins, endothelial dysfunction, and oxidative stress (44,45).
Fructose is also highly lipogenic, stimulates triglyceride synthesis, and increases fat deposition in the liver, likely mediated in part by increasing fatty acyl coenzyme A and diacylglycerol (49). Splanchnic perfusion studies have shown that hepatic production of triglycerides is much greater with fructose compared with equimolar concentrations of glucose (50). Fructose administration results in greater postprandial hypertriglyceridemia than that observed with isocaloric glucose, and it can also result in higher apolipoprotein B levels (49,51). Fructose feeding is also an effective way to induce fatty liver (52,53) and may be preferentially used by hibernating mammals as a means to increase fat stores (54).
One of the more striking aspects of fructose is its ability to stimulate uric acid production (55). As ATP is consumed, AMP accumulates and stimulates AMP deaminase, resulting in uric acid production (56). Serum uric acid can increase rapidly after ingestion of fructose, resulting in increases as high as 2 mg/dl within 1 h (55,57,58). Although initially the rise in uric acid is transient, studies in which high fructose (or sucrose) diets have been administered have found that even fasting uric acid levels will increase after several weeks (59,60). Choi et al. (61,62) have reported a dose-dependent relationship between fructose ingestion and serum uric acid levels in both men and women, although in another study this relationship could not be confirmed in women (63).
Another distinct characteristic of fructose is that it has a positive feedback system in which fructose up-regulates its transporter (Glut 5) as well as fructokinase. Experimentally, fructose administration has been shown to up-regulate Glut 5 and fructokinase in the rat intestine, liver, and kidney (64,65). Subjects administered a high fructose diet show an enhanced rise in uric acid in response to a standard fructose load (58). We have reported that subjects with metabolic syndrome and fatty liver have a history of significantly greater fructose intake and have higher levels of fructokinase mRNA in their liver biopsies compared with control subjects with other types of liver disease (53). Because fructose intake appears to be higher in obese subjects (53,66), this could account for the greater serum triglyceride response observed in these subjects after a fructose load (51,67,68,69).
Finally, fructose is quite distinct from glucose because it does not signal insulin release. Moreover, fructose can actually lower plasma glucose acutely due to stimulation of hepatic glucose uptake due to a stimulation of hexokinase (70,71,72). This has led to the concept that catalytic amounts of fructose may be beneficial in the diabetic. However, as discussed in Section X, the other short-term and long-term effects of fructose have led societies such as the American Diabetes Association not to recommend fructose supplementation for the diabetic subject (73).
As will be seen in Section III, it is the lipogenic characteristics of fructose, in association with its ability to induce ATP depletion and uric acid generation, that are largely responsible for its ability to induce metabolic syndrome. Furthermore, it is fructose’s unfortunate ability to induce increasing sensitivity with increasing exposure (58) that makes it increasingly relevant in a society that is rapidly increasing its total fructose intake.
III. Fructose Causes Metabolic Syndrome in Animals
Beginning with studies in the 1950s, it was recognized that diets high in sucrose can rapidly induce features of metabolic syndrome in rats, including hyperglycemia, insulin resistance, hyperlipidemia, hypertension, weight gain, and hyperuricemia (74,75,76). Further studies documented that these metabolic changes were due to the fructose content (77). Indeed, if rats are pair-fed equivalent amounts of fructose or glucose so that total energy intake is the same and body weight change is equivalent, only the fructose-fed rats develop features of metabolic syndrome (hypertriglyceridemia, hyperuricemia, and hyperinsulinemia) (37,78).
In addition to the ability of fructose to cause hypertriglyceridemia (37), low HDL cholesterol (79), weight gain (80,81,82), blood pressure elevation (83,84,85), and impaired glucose tolerance (37,78), the administration of fructose to rats can result in other findings associated with the metabolic syndrome, including endothelial dysfunction (78,86), oxidative stress (87), sympathetic nervous system activation (85,88), activation of the renin angiotensin system (89), systemic inflammation (45), fatty liver (52), increased intraabdominal fat accumulation (90), leptin resistance (82,91), proteinuria (78), renal hypertrophy (84), glomerular hypertension (84), and renal microvascular disease (83,84). Metabolic syndrome is also recognized as a risk factor for chronic kidney disease (92); fructose feeding also accelerates chronic kidney disease in rats compared with dextrose-fed rats administered identical caloric intake (93).
Despite the relatively consistent ability of fructose to induce hypertriglyceridemia, weight gain is often variable in studies using rats (83,91). Recent studies from our group may provide insights into this mechanism. In this study, rats were fed fructose or starch-based diets for 6 months. Despite the fact that there was no difference in weight gain between groups, the fructose-fed rats developed leptin resistance that was not observed in starch-fed rats. When the leptin-resistant rats were placed on a classic Western, high-fat, and high-sugar diet, the rats gained weight much more rapidly than their starch-fed littermates (91). This suggests an interaction between fructose and high-fat diet in the ability to induce obesity. A similar interaction has been shown in the ability of a high-salt diet to increase blood pressure in fructose-fed rats (94).
There is also evidence that sucrose, and possibly fructose, may have neuropsychiatric effects. Sugar may be addicting, similar to many commonly addictive drugs (95,96). Rats exposed to sugar demonstrate sugar bingeing and craving, with dopamine and opioid receptor binding, enkephalin mRNA expression, and dopamine and acetylcholine release in the nucleus accumbens (95,96). Similarly, humans exposed to cake or ice cream show enhanced activation of certain areas in the brain by positron emission tomography scanning, possibly due to alteration in dopaminergic activity (97).
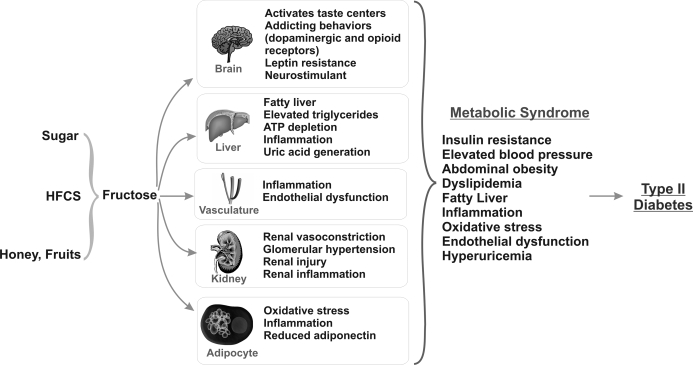
A summary of the effects of fructose on the various organ systems is shown in Fig. 2.
Figure 2.
Effect of fructose on various organ systems. Table sugar, HFCS, and natural sources provide fructose, which in excess has numerous effects on the brain, liver, vasculature, kidney, and adipocyte. The net effects induce all features of the metabolic syndrome and ultimately type 2 diabetes.
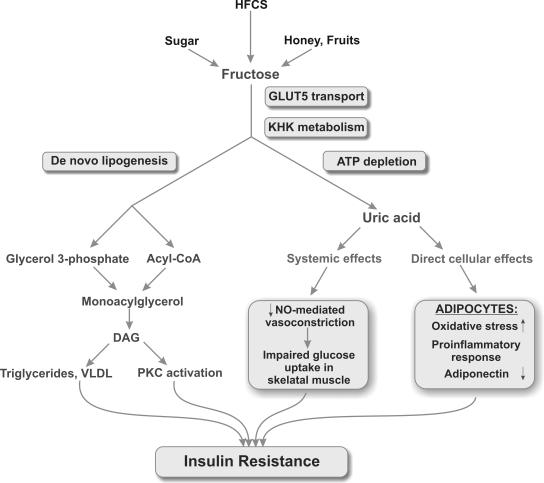
IV. Mechanism(s) for Fructose-Induced Insulin Resistance (Fig. 3)
Figure 3.
Potential mechanisms by which fructose and uric acid may induce insulin resistance. Fructose enters cell via a transporter (primarily Glut 5) where it is acted on by fructokinase (KHK). As part of this metabolism, ATP depletion may occur, generating uric acid with systemic effects that block insulin-dependent NO-mediated vascular dilation as well as direct cellular effects on the adipocyte. Fructose also causes de novo lipogenesis that can lead to intracellular triglycerides that can also induce insulin resistance. DAG, Diacylglycerol; PKC, protein kinase C; VLDL, very low-density lipoprotein.
Fructose may induce insulin resistance in part by classic obesity-associated mechanisms. For example, hepatic triglyceride accumulation may result in protein kinase C activation and hepatic insulin resistance due to increased uptake of free fatty acids (49). Elevation of very low-density lipoprotein and systemic free fatty acids also results in increased lipid uptake in skeletal muscle and other peripheral organs that can mediate systemic insulin resistance (49). Leptin resistance, which is induced by fructose but not starch-based diets (91), has also been shown to mediate insulin resistance in other settings (10).
Moreover, there is evidence that fructose-induced insulin resistance is mediated by fructose-induced hyperuricemia (37,78,83). Lowering uric acid using either xanthine oxidase inhibitors or uricosuric agents can prevent the development of metabolic syndrome induced by fructose (37,78,83). At least two mechanisms may account for these findings. First, it is known that insulin-mediated endothelial nitric oxide (NO) release can account for one third of insulin’s action possibly by increasing blood flow to skeletal muscle and peripheral tissues and enhancing glucose uptake (98). Mice incapable of generating endothelial NO develop full features of metabolic syndrome (99). Uric acid inhibits endothelial NO in cell culture (100,101,102) and in the animal (100), and the mechanisms involve uric acid-induced oxidant production (103,104), C-reactive protein production (101), stimulation of arginase (105), and direct scavenging (106). Asymptomatic hyperuricemia in humans is also associated with endothelial dysfunction (107), and lowering uric acid with allopurinol improves endothelial function in diabetics (108). The second proposed mechanism is by a direct effect of uric acid on the adipocyte. There is evidence that insulin resistance is mediated in part by inflammation and oxidative stress within the adipocyte (109). Sautin et al. (104) have recently shown that uric acid induces this phenotype in cultured adipocytes. In addition, Cheung et al. (110) reported that xanthine oxidoreductase knockout mice fail to become fat due to a defect in adipogenesis. These studies therefore implicate xanthine oxidase and uric acid in metabolic syndrome.
The observation that fructose-induced insulin resistance can occur independent of weight gain or differences in energy intake (37,78) does not negate the possibility that the insulin resistance could still be mediated by the adipocyte. We have found, for example, that fructose-glucose or sucrose combinations result in increased intraabdominal fat accumulation compared with starch-fed rats given equivalent energy intake and with similar weight gain (R.J. Johnson, C. Roncal, Y.Y. Sautin, T. Nakagawa, L.G. Sánchez-Lozada, unpublished observations). Finally, it is likely that insulin resistance will continue to manifest once an animal develops extensive fat stores via classical mechanisms (10), so that continued insulin resistance might be expected even if fructose intake was reduced. Hence, fructose induced insulin resistance might be considered an initiator of the insulin resistance syndrome, with obesity-based mechanisms perpetuating the condition.
V. Mechanism(s) by Which Fructose Induces Other Features of the Metabolic Syndrome: Role of Uric Acid
There is increasing evidence that intracellular ATP depletion and uric acid generation may have important roles in the ability of fructose to induce features of the metabolic syndrome. As mentioned, lowering uric acid was found to ameliorate a number of features of metabolic syndrome in fructose-fed rats, including hypertension, hypertriglyceridemia, hyperinsulinemia, insulin resistance, renal vasoconstriction, glomerular hypertension, and renal microvascular disease (37,78,83). Allopurinol can also reduce fructose-induced monocyte chemoattractant protein-1 (MCP-1) production in human proximal tubular cells (44).
The finding that uric acid might have a role in metabolic syndrome is surprising because uric acid is considered one of the major antioxidants in the circulation (111). Furthermore, whereas uric acid is commonly elevated in subjects with metabolic syndrome (112), it has been thought to be elevated secondary to the hyperinsulinemia (113) that occurs in these subjects.
Nevertheless, the evidence that uric acid may be a true mediator of cardiovascular disease is mounting. Uric acid, whereas an antioxidant in the extracellular environment, can induce oxidative stress in a variety of cells including vascular smooth muscle cells and murine adipocytes (103,104,114). The mechanism appears to involve stimulation of nicotinamide adenine dinucleotide phosphate oxidase (104). Uric acid also reduces NO bioavailability in endothelial cells, adipocytes, and vascular smooth muscle cells (100,102,103,104), and the mechanism is mediated by oxidative stress (103,104,114), the stimulation of arginase (115), and the direct scavenging of NO by uric acid (106). Uric acid also stimulates vascular smooth muscle cells by entering cells via a specific organic anion transport pathway with the stimulation of mitogen-activated kinases (p38 and ERK) and nuclear transcription factors (nuclear factor-κB and activator protein-1), resulting in platelet-derived growth factor-dependent proliferation, cyclooxygenase-2-dependent thromboxane production, MCP-1 and C-reactive protein synthesis, and stimulation of angiotensin II (101,103,116,117,118,119,120). Uric acid also inhibits endothelial cell proliferation and migration (101). Finally, uric acid has potent effects on proximal tubular cells (stimulating MCP-1 production) as well as adipocytes (inducing oxidative stress, stimulating oxidized lipids, and lowering NO levels) (44,104).
More recently, uric acid has been implicated in the pathogenesis of hypertension (reviewed in Ref. 121). An elevated uric acid has been found to be an independent risk factor for hypertension in multiple studies (121). Uric acid is also commonly elevated in subjects with essential hypertension, particularly in newly diagnosed hypertension (122). Furthermore, lowering uric acid has been found to normalize blood pressure in 66% of adolescents with essential hypertension and asymptomatic hyperuricemia compared with 3% in the placebo-treated controls (123).
The mechanism by which uric acid could raise blood pressure has been studied in the rat. Rats normally have a low uric acid due to the presence of uricase, an enzyme in the liver that degrades uric acid to allantoin. In contrast, humans have no functional uricase due to a mutation that occurred in the Miocene epoch (124). To study the effects of hyperuricemia, it was necessary to provide a uricase inhibitor (oxonic acid) in the diet. When uric acid levels were raised, the laboratory animals developed the clinical, histological, and hemodynamic characteristics of essential hypertension (125,126). The hypertension was shown to be initially mediated by oxidative stress, activation of the renin angiotensin system, and endothelial dysfunction, and it could be reversed by treating with antioxidants, l-arginine, or inhibitors of the renin angiotensin system (116,125,127,128). However, as renal microvascular disease develops, the blood pressure switches from being uric acid-dependent to one that is salt-sensitive and kidney dependent (119), similar to many other models of salt-sensitive hypertension (129).
Experimentally raising uric acid in rats has also been shown to induce mild renal injury as well as accelerate established renal disease (118,125,130,131). The mechanism appears to be due to uric acid-dependent renal vasoconstriction and glomerular hypertension (132,133). Consistent with this observation are increasing clinical studies identifying uric acid as a risk factor for renal progression, including in diabetic nephropathy (134,135,136), and intervention trials showing that lowering uric acid may be renoprotective (137,138,139).
Interestingly, the observation that uric acid mediates many of the effects of fructose helps explain why high concentrations of fructose are often required to induce metabolic syndrome in the rat. Because the rat has uricase, fructose does not increase uric acid levels very effectively. Indeed, if uricase is inhibited, a rat will show a greater than 10-fold increase in uric acid in response to a fructose load (140). Although diets of 35 to 60% of fructose are required to induce hyperinsulinemia at 3 months, the administration of 20% fructose will result in hyperinsulinemia and hypertension for the same period if uricase is inhibited (141). Another reason why the rat may be relatively resistant to fructose is because the rat makes ascorbate, and ascorbate can block the effects of fructose both in vitro and in vivo (104,114,142). Another reason for the relative resistance could relate to the fact that fructose is usually administered without glucose. However, glucose can markedly increase fructose absorption (143). We have recently found that lower doses of fructose (30%) readily induce metabolic syndrome if glucose is present in equimolar concentrations (R.J. Johnson, C. Roncal, Y.Y. Sautin, T. Nakagawa, L.G. Sánchez-Lozada, unpublished observations). Finally, duration of fructose exposure may also be important. For example, concentrations of fructose as low as 15% can induce impaired glucose tolerance in rats if administered for longer than 1 yr (144).
VI. Human Studies with Fructose
Numerous studies have also examined the short-term effects of sucrose or fructose in humans (reviewed in Refs. 36,145 and 146). Although marked variability has been reported, in most cases the results are predictable based on the mechanisms we have already elucidated. For example, very high doses of fructose (250 g/d × 7 d) cause insulin resistance in 1 wk (147), whereas slightly lower doses (216 g/d for 4 wk) only induce insulin resistance at sites where fructokinase is highly expressed (liver and adipocyte) (148), and even lower doses (100 g/d × 4 wk) result in no insulin resistance at all (149). In subjects with underlying insulin resistance or obesity, the ability of fructose to induce insulin resistance can be shown with diets as low as 15% fructose (67) or 25% fructose (150). Increased sensitivity to fructose in this latter population would be predicted because underlying endothelial function would be worse compared with healthy subjects and because this group might be expected to have a prior history of fructose exposure and hence higher levels of Glut 5 and fructokinase.
Similarly, most studies show that fructose administered as 17 to 20% of the diet (about 60–70 g of fructose daily) for up to 4 wk raises plasma triglycerides in men (60,151). In one study of young healthy men (with presumed good endothelial function), the increase in triglycerides was only shown postprandially (152). Young healthy women are more resistant to fructose-induced hypertriglyceridemia, whereas obese or hyperinsulinemic women (51,69) or men (68) are much more sensitive. Sucrose can also lower HDL cholesterol in young men (153).
Most short-term studies have failed to show an effect on blood pressure, with the exception of two studies using sucrose (59,154). However, one recent study showed that the effect of acute fructose loading to raise blood pressure is best observed within 1 h of ingestion (155), which is similar to when uric acid increases in the circulation. Interestingly, the administration of an identical dose of glucose had no effect on blood pressure.
The effect of acute fructose administration on weight gain has been more difficult to show. However, three studies have reported that overweight or hyperinsulinemic subjects administered sucrose-based diets have a final weight greater than controls (59,154,156), and the effects on weight gain are greater in subjects who were formally obese compared with those who were always lean (156). Likewise, in a recent preliminary study, Stanhope et al. (150) demonstrated that a diet of 25% fructose resulted in increased intraabdominal fat accumulation (documented by computed tomography scan) in obese women compared with similar women administered a 25% glucose-based diet.
One mechanism by which fructose may cause weight gain could be that fructose does not acutely stimulate insulin. Glucose, for example, acutely stimulates insulin release, which causes a downstream stimulation of leptin and an inhibition of ghrelin, all of which signal the satiety centers in the brain with the sensation of fullness. In contrast, fructose does not acutely stimulate insulin and, as a consequence, does not result in as significant a rise in postprandial leptin levels (157). In one study, subjects fed fructose complained of being more hungry and ate more calories the following day compared with a group fed starch (157).
In addition to the acute effects of fructose, it is possible that there could be chronic effects such as those observed in the rat in which leptin resistance develops (91). Because long-term clinical studies with fructose-based diets have not been performed, it is unknown whether this mechanism is operative in humans. However, serum leptin levels were higher in humans given a high fructose diet for 4 wk compared with those placed on a starch-based diet (149).
Finally, there is evidence that administration of 25% fructose-based, but not glucose-based, diets results in a significant increase in circulating soluble intercellular adhesion molecule-1 levels (150), consistent with findings in rats administered a physiologically relevant (20%) fructose diet (45). Sugar or HFCS-containing soft drinks have also been recently associated with an increased risk for renal disease as manifested by albuminuria (158).
Although the evidence is not as compelling as in the rat, one must remember that these are short-term studies. Nevertheless, it is clear that fructose can induce features of the metabolic syndrome in humans. As will be discussed, epidemiological studies suggest that the effects of sugar or fructose may require up to 10 yr before frank obesity and diabetes develop (31). So how good is the epidemiological evidence linking sugar to the development of diabetes?
VII. Epidemiological Studies: Sugar Intake and Type 2 Diabetes
Sugar intake was minimal in the general population before 1800 (27). However, with the expansion of the sugar plantations in North and South America, and with the rise in the sugar beet industry in Europe, a marked increase in sugar consumption can be observed in Europe and the United States beginning in the early 1800s (27). Between 1700 and 1800, yearly per capita sugar intake in England increased from 4 pounds (1.8 kg) to 18 pounds (8.1 kg); by 1900, this had increased to almost 90 pounds (40 kg). Although sugar was originally afforded only by the wealthy, the marked increase in production, coupled with a reduction in taxes, resulted in sugar becoming available for the general population (27). Furthermore, sugar became one of the best staples of the Westerner for trade when visiting developing countries.
Interestingly, reports of diabetes occurring in the wealthy and obese begin to occur in Europe (primarily from England, France, and Germany) during this time (1,2,159). By the early 1900s, a remarkable increase in diabetes was already being noted in the United States and elsewhere (4,5). An important study was reported by Haven Emerson, director of the Institute of Public Health at Columbia University. Emerson used death rates from diabetes (determined by death certificates) as a surrogate for the prevalence of diabetes in the general population. Emerson noted that death rates from diabetes per 100,000 population had increased markedly between 1880 and 1920 in New York, rising from 2.8 to 18.9 cases (4). The population at greatest risk were those who were Caucasian, wealthy, sedentary, and over the age of 45; men and postmenopausal women were the most susceptible (4). Merchants, particularly in the food industry, were particularly at risk, whereas laborers, miners, and African-Americans had decreased risk (4).
Emerson and Larimore (4) also noted a remarkable association of diabetes with sugar consumption. Although the intake of meat per capita had fallen during the previous 15 yr, the intake of sugar in the population had increased markedly. Indeed, Emerson and Larimore noted that sugar intake corresponded to rates of diabetes in other countries as well; for example, they noted that diabetes rates in Australia were significantly lower, and this population consumed much less sugar and 30% more meat (4).
Other investigators also noted a remarkable association of sugar intake with diabetes rates. For example, Concepcion (29) noted that diabetes was rare in the Philippines, except in Manila where it correlated with sugar consumption. Charles (5) and Chakravarti (160) noted that diabetes was becoming increasingly common among the wealthy Hindu in the Lower Bengal who had an excessive intake of sugar. Similar associations of diabetes with sugar intake among the wealthy were noted in Egypt (161), whereas among the rich Chinese the development of diabetes correlated with the “adaption of European food, especially drinking sweet wines” (162).
As mentioned, sugar also became one of the key staples for trade with indigenous peoples. For example, the Pima Indians were originally described as a healthy and athletic tribe that lived in the Gila River Basin in Arizona. However, in the early 1800s a major wagon route to California was opened directly through Pima lands. With the advent of the California Gold Rush, thousands of settlers traveled to California, often stopping at the Pima wagon post for supplies. According to Hrdlička (163), a favorite trade item for the Pima was sugar. Interestingly, by 1900 both obesity and diabetes were emerging although the population was very poor.
The introduction of a Western diet, including sugar, was also associated with a remarkable transformation of the Maori (164,165,166,167), the Australian aborigine (168), and other Native American Indian tribes (169,170,171,172) from a healthy people devoid of cardiovascular disease to a population with excessive rates of diabetes, obesity, and heart disease. Sugar intake remains high in these populations (173,174). Likewise, diabetes was also once rare among peoples living in China, Japan, India, the Phillipines, Polynesia, Sudan, and West Africa (175); however, with the introduction of Western culture, there has been a remarkable transformation (6).
Similarly, diabetes began to increase in Iceland in association with a rise in carbohydrate intake, especially sugar (176). Today obesity and diabetes are increasing worldwide and are especially common in certain populations such as Pacific Islanders (177). Furthermore, whereas it has been known that vegetarians are often protected from cardiovascular disease and hypertension (178), this does not appear to be true for vegetarians who eat increased amounts of sugar. For example, in one study vegetarian Indians living in South Africa who developed diabetes ate more sugar than nonvegetarian subjects (179). Fernando (180) also reported that diabetes was increasing in Ceylon among the rich and educated, many of whom were eating vegetarian, high carbohydrate-containing foods. Unfortunately, Fernando did not note what percentage of the high-carbohydrate foods were from sugar.
There is also a relationship of sugar intake with the increased risk for diabetes observed in the African-American and Hispanic populations in the United States. As discussed above, diabetes was initially rare among the black African (30,181) and the African-American (4). However, L. I. Dublin, the head statistician of the Metropolitan Life Insurance Company and one of the early leaders in epidemiology, noted that diabetes was already becoming common by the 1920s among African-Americans in some urban cities in the South (4). Similarly, in the early 1900s, hypertension began to manifest among the African-American, especially in the southeastern United States and the Caribbean (182,183). In the early 1960s, diabetes in Jamaica was still less common than that observed in the United States and Europe, but it was already higher than that observed in the black African (184). By the 1970s, the risk for diabetes among African Americans had surpassed that of the Caucasian. One potential explanation could be the fact that African-Americans and Hispanics ingest greater quantities of sugar than Caucasians (185,186).
In South Africa, Campbell (30) noted an emerging epidemic of diabetes among the Natal Indians working in the “Sugar Belt.” Unlike their relatives in India, who were eating only about 12 pounds (5.4 kg) of sugar per capita per year, the average Natal Indian was ingesting 77 pounds (35 kg) (30). The Zulu appeared to be more resistant, but the most wealthy, who ate nearly 10-fold more sugar than the rural Zulu, were also at risk (30).
Studies have also linked increasing diabetes rates with immigration of peoples into countries where sugar intake is high. For example, one study reported that Yemenite Jews that had settled in Israel had remarkably higher rates of diabetes than Yemenites living in Yemen. Interestingly, the only dietary difference was the almost complete absence of sugar in the diet in Yemen, whereas sugar accounted for 20% of the total carbohydrate intake for Yemenites in Israel (187). Furthermore, increased rates of diabetes have been observed in Japanese and Filipinos after immigration to the United States and Canada (188,189).
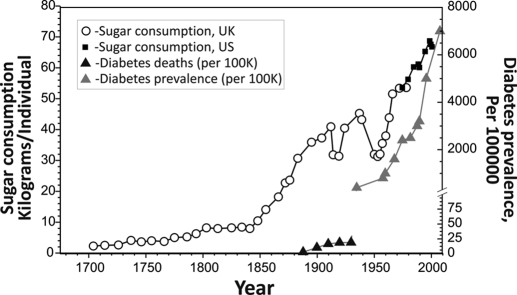
The introduction of HFCS in the 1970s has resulted in a 30% increase in total fructose intake in the last 20 yr, and this is also associated with remarkable increases in the rates of obesity and diabetes (27,36,190). Soft drinks, which contain either HFCS or sugar and represent a major dietary source of fructose, have been associated with the development of obesity (66,190,191) as well as impaired glucose tolerance or diabetes (66,192,193,194,195). Fruit drinks are also associated with the development of diabetes, whereas ingestion of whole fruits is not (195,196). In some studies, the effect of fructose intake to predict diabetes has been shown to be independent of body mass index or energy intake (66,191,195,196). Soft drinks also increase the risk for nonalcoholic fatty liver disease (53). Figure 4 shows the remarkable association of sugar intake with diabetes over the last two centuries.
Figure 4.
Parallel epidemic of diabetes and sugar consumption. Sugar intake has been increasing steadily over the last 200 yr (33,310,318,319). In parallel, there has been a rise in diabetes (first described based on death certificates of diabetes-related deaths per 100,000 population) (4) and later by diabetes prevalence rates (268). [The data showing sugar consumption are adapted with permission from R.J. Johnson, et al.: Am J Clin Nutr 86:899–906, 2007 (27) © The American Society for Nutrition.]
VIII. Epidemiological Studies: Uric Acid and Type 2 Diabetes
Given the evidence that uric acid may be involved in fructose-induced metabolic syndrome, it is important to evaluate the relationship of uric acid to metabolic syndrome and diabetes. Uric acid levels are known to be elevated in subjects with metabolic syndrome (13,112,197), and the reverse is also true—that subjects with hyperuricemia frequently have metabolic syndrome (198,199,200,201,202). Gout, which is a manifestation of hyperuricemia, has also been associated with the development of diabetes. Although the association of gout with diabetes is observed in the general population (200), it is especially common in particular groups, notably the Maori, the Australian aborigine, Polynesians, the Natal Indians of South Africa, and the African-American (30,166,168,203,204,205,206).
Interestingly, once a patient is diabetic, uric acid levels are often normal (207). One reason is due to glycosuria, which inhibits uric acid absorption in the proximal tubule. However, diabetic subjects who continue to be hyperuricemic appear to be at increased risk for developing diabetic complications, especially renal disease (136,208).
Many authorities had described the elevation in uric acid in metabolic syndrome as a secondary phenomenon because insulin increases uric acid absorption in the proximal tubule (113,209). However, two studies have reported that an elevated uric acid level predicts the development of metabolic syndrome per se (210,211), and in the former study this was demonstrated even in subjects who were free of all features of metabolic syndrome at baseline (210). An elevated uric acid level also predicts the development of hyperinsulinemia (212,213,214), obesity (215), fatty liver disease (216), and diabetes in most (214,217,218,219,220,221,222,223,224,225,226,227,228,229,230) but not all (231) studies (Table 1). Furthermore, in many of these studies uric acid remained an independent predictor of diabetes after controlling for baseline body mass index (210,218,219,220,221,222,223). These studies suggest that uric acid cannot simply be viewed as a secondary phenomenon.
Table 1.
Elevated uric acid as a predictor for the development of type 2 diabetes
| Study (Ref.) | Population | Follow-up | Endpoint | Independent | Relative risk (CI) |
|---|---|---|---|---|---|
| Korea (211) | 4,779 men | 3 yr | MS | Yes | 1.41 (1.08–1.84), 5th vs. 1st quintile |
| Dallas (210) | 9,689 adults | 5.7 yr | MS | Yes | 1.6 (1.34–2.91) in men and 2.29 (1.0–5.27) in women, 3rd vs. 1st tercile |
| ARIC (213) | 9,020 adults | 11 yr | ↑Insulin | Yes | 1.3 (1.2–1.4) per 1.4 mg/dl |
| Spokane (212) | 60 adults with MI | 6 months | ↑Insulin | Yes | 5.47 (1.6–17.7) for >5.5 mg/dl |
| Rotterdam (220) | 4,536 adults | 10.1 yr | Diabetes | Yes | 1.68 (1.22–1.30), 3rd vs. 1st tercile |
| Framingham (224) | 5,209 adults | 26 yr | Diabetes | Men | 2.3 (>6.2 mg/dl in men) and 2.1 (>5.1 mg/dl in women) |
| Osaka (219) | 2,310 adult men | 6 yr | IFG/diabetes | Yes | 1.78 (1.11–2.85), 5th vs. 1st quintile |
| Osaka (231) | 6,356 men | 9 yr | Diabetes | No | 1.24 (0.9–1.7), 5th vs. 2nd quintile |
| Mauritius (217) | 2,605 adults | 5 yr | IFG/diabetes | Yes | 1.37 (1.20–1.57) per 1 sd |
| Britain (221) | 7,735 men | 12.8 yr | Diabetes | Yes | 1.5 (0.9–2.5), 5th vs. 1st quintile |
| Sweden (222) | 766 men | 13.5 yr | Diabetes | Yes | 5.8 (2.2–16.0), 5th vs. 1st quintile |
| Kinmen (218) | 641 hyperuricemic adults | 7 yr | Diabetes | Women | 1.44 (1.13–2.25) per mg/dl |
| Finland (214) | 522 adults with IGTT | 4.1 yr | Diabetes | Yes | 1.87 (1.07–3.26), 3rd vs. 1st tertile |
| Mauritius (223) | 4,259 Mauritian and creole | 5 yr | Diabetes | Men | 1.14 (1.01–1.3) and 1.37 (1.11–1.68) in Mauritian and Creole men per sd |
| Nauru (228) | 266 adults | 6 yr | Diabetes | Women | Not given |
| Israel (225,226,227) | 10,000 men | 5 yr | Diabetes | Yes | 1.35 (CI not given) per mg/dl |
| China (229) | 2,609 adults | 9 yr | Diabetes | Yes | 1.4 (1.02–1.92), 5th vs. 1st quintile |
| United States (230) | 11,351 men | 6 yr | Diabetes | Yes | 1.70 (1.38–2.11), 5th vs. 1st quintile |
MS, Metabolic syndrome; IFG, impaired fasting glucose; ↑Insulin, hyperinsulinemia; MI, myocardial infarction; IGTT, impaired glucose tolerance test; CI, confidence interval.
IX. Do Other Conditions That Modify Uric Acid Levels Affect the Development of Metabolic Syndrome or Diabetes?
If uric acid has a role in the development of diabetes, then other mechanisms raising uric acid might also have a role in the etiology of type 2 diabetes. A list of some of the common causes of hyperuricemia is shown in Table 2. For example, red meats are high in purines and can raise uric acid levels and increase the risk for gout (232); some studies also suggest that diets high in meats increase the risk for diabetes (233,234,235,236,237,238). Although all alcohol can raise uric acid levels, beer is the greatest offender due to the presence of brewer’s yeast that contains high levels of guanosine (239,240). Excessive intake of beer can also cause abdominal obesity (“beer belly”) with features similar to metabolic syndrome (241,242,243); excessive alcohol intake also has been reported to increase the risk of diabetes in some studies (244,245,246). Indeed, there are historical reports of an increased risk for diabetes among Trappist Monks who drank Trappist beer, a type of unfiltered beer with high residual sugar and yeast content (28).
Table 2.
Conditions associated with high uric acid levels
| Gender /age | Adult men, postmenopausal women |
| Race | African-American, Polynesian, Maori |
| Cardiovascular condition | Hypertension, metabolic syndrome, cardiovascular disease, obesity, insulin resistance, nonalcoholic fatty liver, obstructive sleep apnea |
| Kidney | Renal failure |
| Pregnancy | Preeclampsia |
| Diet | High purine meats, fructose, high-fat diets, beer |
| Habits | Acute exercise |
| Toxins | Lead (low dose) |
| Drugs | Calcineurin inhibitors, diuretics, pyrazinamide, ethambutol, low-dose aspirin, niacin, some HIV medications |
| Catabolic states | Leukemia, tumor lysis, polycythemia vera, postbariatric surgery, starvation, psoriasis |
| Ketosis | Diabetic ketoacidosis, starvation, high-fat diet |
| Lactate | Congestive heart failure, alcohol, Gaucher’s disease |
| Hereditary | Lesch Nyhan syndrome, increased phosphoribosylpyrophosphate synthetase, familial juvenile hyperuricemic nephropathy |
| Other | Down’s syndrome, hyperparathyroidism, hypothyroidism, sarcoidosis, emotional or physical stress, marathon running, high altitude |
Certain foods are also known to reduce uric acid levels and/or decrease the risk for gout, including dairy products and caffeine (247); both have also been reported to decrease the risk for metabolic syndrome and diabetes (248,249,250). There is also evidence that vitamin C (ascorbate) can counter the effects of fructose to cause metabolic syndrome. Vitamin C blocks the actions of uric acid on various cell types (251), vitamin C levels correlate with lower uric acid levels (252), and vitamin C supplementation also can lower uric acid levels by increasing urate excretion (253). Interestingly, low plasma ascorbate levels may also increase the risk for gestational diabetes (254), low intake of vitamin C was found to increase the risk for type 2 diabetes in one study (255), and vitamin C supplementation can improve features of metabolic syndrome in subjects with type 2 diabetes (256). Thus, the vitamin C content in natural fruits (as well as other antioxidants and flavonoids) may provide a safeguard against the untoward consequences related to excessive fructose ingestion.
Thiazide diuretics are well known to cause both hyperuricemia and features of metabolic syndrome (hyperglycemia, insulin resistance, and hypertriglyceridemia), and patients receiving thiazides are at increased risk for developing diabetes (257,258). We have reported that the thiazides can exacerbate fructose-induced metabolic syndrome in the rat and that these features can be reversed, and blood pressure further improved, by pharmacologically lowering serum uric acid (78).
Chronic lead intoxication is also a well-recognized cause of hyperuricemia, hypertension, and renal disease (259,260). Chronic lead ingestion is also associated with a higher body mass index and elevated fasting blood glucose levels (261). It is interesting that Emerson and Larimore (4) wrote that diabetes was nearly absent in miners with the exception of lead miners. We have found that experimentally induced hypertension in chronic lead-treated rats can be reversed by lowering uric acid levels (C. Roncal, unpublished observations). An elevated uric acid level and features of metabolic syndrome or diabetes often complicate calcineurin use in transplantation and in complicated pregnancy; and uric acid may have a role in calcineurin toxicity (262) and preeclampsia (263,264,265). Excessive intake of fructose during pregnancy is also associated with increased risk for preeclampsia and carries greater risk than obesity itself (266). Finally, high-fat diets can also increase uric acid levels (267), but we believe fructose may be more potent, in part because of its unique effect to up-regulate its own metabolic enzymes that drive the process (53). Indeed, high fat intake has not been associated with increased risk for diabetes when total energy intake was controlled (268). Nevertheless, it raises the interesting possibility that there could be a synergistic effect of sugar with a high-fat diet to cause the metabolic syndrome.
X. Twelve Countering Arguments and Caveats
The hypothesis that fructose (or sugar) may be an etiological agent causing type 2 diabetes has been refuted in the past due to a variety of arguments. We summarize 12 reasons the fructose hypothesis could be challenged and provide potential explanations.
1. How can one separate the role of obesity in causing diabetes from fructose per se? Many authorities consider obesity as the most important risk factor for diabetes, and it is known that insulin resistance can result from intraabdominal fat accumulation (10). As discussed in Section IV, there is evidence that fructose may cause insulin resistance via both obesity-based and nonobesity-based mechanisms. In experimental studies, fructose has been shown to induce insulin resistance by raising uric acid levels independent of energy intake or changes in body weight (37,78). An elevated uric acid can also predict the development of diabetes independent of baseline body mass index (210,218,219,220,221,222,223). Diabetes can also occur in the absence of frank obesity, especially in Asia (11,12). Although these studies suggest that fructose may act independently of obesity, it is clear that the two will be closely intertwined, especially because fructose ingestion may cause leptin resistance (91) and intraabdominal fat accumulation (49,90). Teasing out the differences may require carefully designed clinical trials (see Section XII).
2. If fructose is bad, then why do some investigators recommend it for diabetics? Fructose has been reported to be good for diabetics because fructose does not stimulate insulin secretion from the pancreas and, in fact, may acutely reduce blood sugar by increasing hepatic uptake due to stimulation of hepatic glucokinase (70,71,72). However, this ignores the long-term consequence of fructose to cause insulin resistance (146). In addition, fructose is a greater stimulant of advanced glycation end-products than glucose (269), and these products are not detected by most routine assays (270). Experimental studies document the fact that fructose can cause cataracts in diabetic animals (271). Finally, the fact that fructose increases triglycerides has led the American Diabetic Association not to recommend fructose as a food supplement for diabetic subjects (272).
3. Why are sugar cane workers, who ingest large amounts of sugar, not at risk for diabetes? Observations that sugar cane workers in Panama and South Africa, who were exposed to large amounts of sugar by chewing on sugarcane, did not develop diabetes in contrast to the owners of the plantations who ate refined sugar has been used either to refute sugar as the cause (273) or to suggest that it is only the refined sugar that carries risk (31). A more likely explanation may be that it is not simply the quantity of fructose ingested that matters, but also the rate of ingestion. The effect of fructose to deplete ATP and generate uric acid is contingent on the concentration of fructose to which the cells are exposed (274). Chewing sugar cane may result in prolonged exposure to low concentrations but may not be equivalent to bolus exposure such as provided in soft drinks or rich desserts. In addition, working in the cane fields was likely associated with physical exertion and possibly less food availability that could counter the negative effects of excessive fructose intake; indeed regular exercise is known to lower uric acid levels (275).
4. If sugar causes diabetes, then why is diabetes low in some countries with high sugar intake? Mills (175) reported in 1930 that of the 13 countries with the highest sugar intake, 11 were among the 13 with the highest rate of diabetes. Nonetheless, both Mills (175) and Joslin et al. (276) suggested that sugar was unlikely the cause of diabetes because there were some countries with high sugar intake where diabetes rates were low, most significantly Hawaii, Argentina, and Cuba. According to the U.S. Bureau of Census, the prevalence of diabetes in the United States in 1920 was 18.9 cases per 100,000 population (based on deaths) (4), whereas in Hawaii there were only 8.5 deaths per 100,000 in 1926 despite very high sugar consumption (54 kg per capita per year) (276). However, comparing diabetes death rates of Hawaii with the general U.S. population may not be appropriate given that Hawaii was primarily an agricultural community during the 1920s; indeed, for the same period, the rate of diabetes for U.S. agricultural workers was only 4 cases per 100,000 (4), suggesting that rates in Hawaii were indeed higher than expected.
5. The studies in rats showing that fructose can cause metabolic syndrome are not relevant because they use supraphysiological doses. A discussion of this issue is provided in Section V. Most studies administering fructose to rats have used diets in the 50 to 60% range; in contrast, the mean fructose content of the American diet is 9%, with the upper range approaching 15 to 20% (36,146). There are two reasons for the use of high concentrations of fructose in rats. First, it is common for high doses of agents to be used to induce a syndrome rapidly. As mentioned, a 20-yr lag was noted by Campbell (241) between exposure to excessive sugar intake and manifesting diabetes (note that this may be shorter now that we are having 30 to 40% more exposure). If rats are placed on 15% fructose diets, they also develop insulin resistance, but it takes 15 months (144). Second, fructose-induced metabolic syndrome is mediated by fructose-induced hyperuricemia (37) and can be blocked by vitamin C (142). Because rats express uricase (which degrades uric acid) and also synthesize vitamin C, they are naturally resistant to the effects of fructose. Indeed, if uricase is inhibited, rats develop marked hyperuricemia in response to a fructose load (140) and also rapidly develop hyperinsulinemia in response to a diet containing only 20% fructose (141).
6. Fructose is unlikely a cause of hypertension because fructose does not raise blood pressure in rats by intraaortic telemetry. Studies in rats have shown that fructose does not increase blood pressure in conscious, unrestrained rats using intraaortic telemetry despite raising blood pressure when measured by other means (such as intraarterial measurements made during anesthesia or by extraneous catheter or by tail cuff) (277,278). These studies suggest that the elevation of blood pressure observed with these latter methods may reflect a heightened response to stress (like white coat hypertension) as opposed to true hypertension. Indeed, mice fed fructose display higher blood pressures by telemetry when they are awake and feeding (85). Despite these results, studies in humans have documented that 60 g of fructose will acutely raise blood pressure, whereas this is not observed with glucose (155). Short-term intake of sugar has also been reported to increase blood pressure in some (59,154,279) but not all studies (280).
Fructose may also cause hypertension indirectly as a consequence of causing renal microvascular disease. Indeed, we have found that fructose causes afferent arteriolar disease in rats that is mediated by uric acid (84), and in other models we have shown that the induction of renal microvascular disease will lead to the development of salt-sensitive hypertension even if the initiating stimulus is removed (129). Indeed, hyperuricemic rats also develop a renal arteriolopathy, and after its development the rats display salt-sensitive hypertension even if the uric acid levels return to control levels (119). Consistent with this finding, the administration of fructose and a high-salt diet to rats results in renal microvascular disease and hypertension that persists despite withdrawing the diet (94). Furthermore, high fructose intake is associated with high salt intake (281), raising the likelihood that this mechanism could be engaged in man.
7. What is the direct evidence that fructose causes obesity in people? As discussed in Section VI, epidemiological studies have linked high fructose-containing drinks with weight gain (66,191,282,283), and the general increase in obesity in the United States correlates closely with the rise in overall fructose intake (27,36,190). Raben et al. (154) also reported in a randomized double-blind study that the administration of sucrose-containing soft drinks resulted in significantly greater weight gain than with diet soft drinks. Similarly, Tordoff and Alleva (284) also reported a trial in which increased weight gain was observed after 3 wk in subjects drinking soft drinks containing HFCS compared with soft drinks containing aspartame. Fructose supplementation also increased weight in diabetic subjects (285). Finally, there is strong evidence that fructose intake will increase intraabdominal fat accumulation compared with starch-based diets, especially in overweight women (49). In addition, there is evidence that programs that reduce soft drink consumption can result in weight loss (286) and possibly reduce insulin resistance (287).
These studies suggest that supplemental intake of fructose-containing foods or drinks may not result in a reduction in intake of other energy sources, consistent with the possibility that fructose may alter satiety as suggested by Teff et al. (157). However, Le et al. (149) reported that the supplementation of 1.5 g fructose/kg daily did not result in any weight gain after 1 month in young healthy men. This study and others have led to controversy over whether fructose causes weight gain more than other energy sources (288).
One potential explanation may relate to the rat studies that show that long-term (6 month) administration of a high-fructose diet is required for the development of leptin resistance (91). Leptin levels were high at the end of the study by Le et al. (149), so perhaps differences in weight would have been observed if the diet studies had extended for a longer period.
An additional issue revolves around the interpretation of epidemiological studies examining the relationship of sugar intake to obesity. Subjects who become obese may well reduce their sugar intake because sugar is widely recognized as a food that can cause weight gain. Hence, the relationship of sugar to obesity is best performed with longitudinal studies to determine whether sugar intake predicts obesity, rather than cross-sectional studies in which subjects who have already become obese are examined. Furthermore, some subjects will preferentially drink diet soft drinks as a “compensation” for being able to eat other high-calorie, sugar-sweetened foods. Hence, studies such as the paper by Dhingra et al. (192) that reported that both caloric- and diet soft drinks predict obesity and metabolic syndrome may be deceiving unless total fructose intake is considered.
8. If metabolic syndrome and diabetes are due to fructose-induced hyperuricemia, then urinary uric acid excretion should be high and not low as has been reported in subjects with metabolic syndrome (112). Fructose does acutely increase uric acid excretion, but as animals develop renal vasoconstriction and hypertension, the fractional excretion of uric acid falls (37). This suggests a positive feedback system, similar to that observed with the renin angiotensin system in which renal artery vasoconstriction stimulates angiotensin II, which can feedback to cause more renal vasoconstriction.
9. If an elevated plasma uric acid is the cause of metabolic syndrome, then how do we explain reports that elevated uric acid can occur in the absence of an increase in metabolic syndrome, or that metabolic syndrome can occur in the absence of an elevation in uric acid? In 1966, Prior et al. (289) reported that natives living on the island of Pukapuka had a high frequency of hyperuricemia despite minimal evidence of diabetes, hypertension, or obesity, thereby challenging the concept that uric acid might be a cause of these conditions. However, as the authors noted in their paper, sugar had been recently introduced into this community (290). This raises the possibility that the natives were still in the “incubation period” before diabetes and hypertension would manifest (4,30).
Nevertheless, there remain other examples where an elevated uric acid level has been observed with minimal evidence of hypertension or diabetes (291,292). It remains possible that these individuals have other genetic polymorphisms (e.g., in endothelial NO synthase) or dietary habits [such as flavonoid-rich cocoa (293), phytic acid-rich legumes, or high vitamin C intake (251)] that may provide countering protection. Similarly, it is also highly likely that there are numerous mechanisms that may cause obesity and diabetes such that it would not be necessary to have an elevated uric acid in all settings.
10. It is not plasma uric acid that causes the metabolic syndrome, but rather xanthine oxidase-associated oxidants. Xanthine oxidase acts on xanthine to produce uric acid and oxidants. This raises the question that an elevated uric acid may simply reflect the presence of xanthine oxidase-associated oxidants and that it is the latter that is mediating the effects on target tissues. Indeed, uric acid may function as an antioxidant (111,294). Consistent with this hypothesis are recent reports that reduction of uric acid can improve endothelial function only if xanthine oxidase inhibitors are used and not if uric acid is lowered by other means (295,296); furthermore, the infusion of uric acid into humans has been reported to improve endothelial function (297,298), not the converse as suggested by the animal studies (100).
However, it is possible that most of the effects of uric acid are intracellular and that xanthine oxidase inhibitors are more effective at lowering intracellular uric acid concentrations. Studies in cell culture that have used exogenous uric acid have consistently shown no effect if uric acid entry into the cell is prevented (101,103,114). Although fructose raises systemic levels of uric acid, it is possible that some of its effects are mediated in the cells where uric acid is generated, such as the fructokinase-rich hepatocyte, adipocyte, and proximal tubular cell. Consistent with this possibility is the observation that allopurinol blocks fructose-induced MCP-1 in the human proximal tubular cell (44). However, this cannot account for all of the mechanisms by which fructose-induced hyperuricemia acts for uricosurics improve the metabolic syndrome in fructose-fed rats (37). In addition, two older studies found that increasing uric acid in rats by uricase inhibitors results in hyperglycemia, elevated blood pressure, hypertriglyceridemia, and fatty liver (299,300). However, the author did not show that lowering uric acid was protective, so it is unclear whether these effects were actually due to the uric acid per se.
11. If fructose and uric acid cause the metabolic syndrome and diabetes, then why does lowering uric acid not cure diabetes or metabolic syndrome? It is increasingly recognized that often the mechanisms initiating a process may be distinct from those maintaining the process. For example, hypertension can often be precipitated by injecting a substance that causes renal vasoconstriction, but over time renal microvascular disease develops that perpetuates the hypertension even after the stimulus is removed (129,301). Similarly, once sufficient kidney damage develops, progressive renal disease will occur, driven by the intrarenal hemodynamic changes that have resulted from the initial loss of renal function (302). A wealth of literature also suggests that insulin resistance can be perpetuated once obesity and intracellular lipid accumulation manifest, especially in sites other than adipose tissue (303,304). Thus, reducing fructose or lowering uric acid might be expected to provide some benefits once insulin resistance and diabetes develop but may not be able to fully reverse these conditions.
12. Several genome-wide scans have identified genetic polymorphisms that correlate with increased risk for gout but do not show linkage with diabetes or hypertension, thereby challenging a causal relationship between uric acid and diabetes. Recently SLC2A9 has been identified as a transporter that transports fructose as well as uric acid (305,306). Polymorphisms in SLC2A9 are associated with increased urinary uric acid excretion and lower serum uric acid levels (305,306). Interestingly, whereas these polymorphisms appear to protect the individual from gout, there is no evidence that these polymorphisms are linked with diabetes (305,306). This raises the question of whether the uric acid has a causal role in this disease or whether it may simply represent a secondary marker. However, an alternative explanation is that only 6% of the variation in serum uric acid can be accounted for by these polymorphisms, and hence the currently published studies are underpowered to identify this relationship. Furthermore, because it is the intracellular uric acid that mediates its metabolic effects (101,114,120,307), we also need additional studies to determine how the SLC2A9 modulates intracellular uric acid levels in response to fructose.
XI. The Thrifty Gene Revisited
In 1962, James Neel suggested that humans acquired “thrifty genes” during the feast and famine days of hunting and gathering, which then predisposed them to obesity and diabetes in today’s society of overnutrition and physical inactivity (308). Diets of our early ancestors were extremely low in sodium and fructose content (309). We have proposed that an elevated uric acid and low vitamin C may be critically important in the “stress response” that is associated with starvation and may have a role in the ability of a starving animal to increase its foraging behavior and fat accumulation (54). We have further suggested that the mutational loss of vitamin C synthesis during the Eocene and of uricase during the mid Miocene provided a survival advantage during periods of environmental stress by virtue of their ability to induce insulin resistance, obesity, fatty liver, and elevated blood pressure (119,251). By mildly increasing blood glucose levels, insulin resistance may protect against hypoglycemia and also preserve glucose for the brain, which does not require insulin for glucose uptake (311). Although we suggest that these mutations likely provided a survival advantage at that time, in today’s setting in which dietary purines, fructose, and salt are ingested at high levels, these mutations may predispose us to hypertension, obesity, and diabetes. Hence, we suggest that genes involving vitamin C, fructose, and uric acid metabolism represent the thrifty genes postulated by Neel.
XII. What Additional Studies Should be Done to Test the Hypothesis?
Sugar and high-fat foods currently make up about 40% of the diet in low-income and developing countries (312). Serum uric acid levels have also been rising in the Western world (313,314,315). Currently, recommendations for prevention of diabetes include physical exercise and weight reduction, often with an emphasis on low-fat diets (35). Sugar is often considered as a source of “empty calories” (316,317) but is generally not appreciated for its potential hormonal effects.
It is our hope that future studies will address the fructose and uric acid hypotheses. Specifically, studies are needed to determine the effectiveness of a low-fructose diet vs. other diets such as DASH (Dietary Approaches to Stop Hypertension) or low-carbohydrate diets in the prevention or treatment of obesity and metabolic syndrome. The effectiveness of low-fructose diets in the prevention or treatment of hypertension, chronic kidney disease, and fatty liver should also be entertained. Lowering uric acid, with or without dietary intervention, should also be examined as a means to prevent or treat early hypertension, metabolic syndrome, obesity, and diabetes. Genetic studies are also needed to determine whether specific polymorphisms involved in fructose or uric acid metabolism may account for the increased predisposition of certain populations to develop metabolic syndrome and diabetes. Additional studies are also needed to determine the cellular mechanisms by which fructose and uric acid induce these phenotypes. If fructose and uric acid can be identified as true remediable risk factors, then a new chapter in the prevention of obesity and metabolic syndrome will unfold.
Acknowledgments
We thank Gary Taubes for his personal discussions and for his book, “Good Calories, Bad Calories,” which provided some excellent historical references on sugar and its relationship to diabetes.
Footnotes
Support for this publication was provided by U.S. Public Health Service Grants DK-52121 and HL-68607, by American Heart Association Grant 0755595B (to Y.Y.S.), and by generous monies from Gatorade. L.G.S.-L. is supported by Grant 081054 from CONACyT, Mexico.
Disclaimers: S.E.P., J.M., L.G.S., D.I.F., M.Sha., M.Shi., and C.R. have nothing to disclose. R.J.J., Y.Y.S., M.Se., and T.N. are listed as inventors on patent applications related to blocking the effects of fructose, or lowering serum uric acid, as a means to prevent or treat metabolic syndrome, hypertension, or cardiorenal disease. R.J.J. is also co-author of a lay book, “The Sugar Fix” (Rodale, 2008), a book that discusses the health effects of excessive fructose intake. R.J.G. has a consulting agreement with FibroGen as Chair of the Data Safety and Monitoring Board for clinical trial of a proprietary product in diabetic renal disease.
First Published Online January 16, 2009
Abbreviations: Glut, Glucose transporter; HDL, high-density lipoprotein; HFCS, high fructose corn syrup; KHK, ketohexokinase; MCP-1, monocyte chemoattractant protein-1; NO, nitric oxide.
References
- Prout W 1848 On the nature and treatment of stomach and renal diseases; being an inquiry into the connexion of diabetes, calculus, and other affections of the kidney and bladder, with indigestion,. 5th ed. London: John Churchill [Google Scholar]
- Duckworth D 1889 A treatise on gout. London: C Griffin Co. [Google Scholar]
- Osler W 1893 The principles and practice of medicine. New York: D. Appleton and Co. [Google Scholar]
- Emerson H, Larimore LD 1924 Diabetes mellitus: a contribution to its epidemiology based chiefly on mortality statistics. Arch Intern Med 34:585–630 [Google Scholar]
- Charles R 1907 Diabetes in the tropics. Br Med J 19:1051–1064 [Google Scholar]
- Yusuf S, Reddy S, Ounpuu S, Anand S 2001 Global burden of cardiovascular diseases. Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 104:2746–2753 [DOI] [PubMed] [Google Scholar]
- Smyth S, Heron A 2006 Diabetes and obesity: the twin epidemics. Nat Med 12:75–80 [DOI] [PubMed] [Google Scholar]
- Yach D, Stuckler D, Brownell KD 2006 Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nat Med 12:62–66 [DOI] [PubMed] [Google Scholar]
- Hossain P, Kawar B, El Nahas M 2007 Obesity and diabetes in the developing world—a growing challenge. N Engl J Med 356:213–215 [DOI] [PubMed] [Google Scholar]
- Kahn BB, Flier JS 2000 Obesity and insulin resistance. J Clin Invest 106:473–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan WH, Flegal KM, Chang HY, Yeh WT, Yeh CJ, Lee WC 2004 Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: implications for definitions of overweight and obesity for Asians. Am J Clin Nutr 79:31–39 [DOI] [PubMed] [Google Scholar]
- Sone H, Mizuno S, Ohashi Y, Yamada N 2004 Type 2 diabetes prevalence in Asian subjects. Diabetes Care 27:1251–1252; author reply, 1252 [DOI] [PubMed] [Google Scholar]
- Kylin E 1923 [Studies of the hypertension-hyperglycemia-hyperuricemia syndrome] Studien uber das Hypertonie-Hyperglykamie- hyperurikamiesyndrome. Zentralblatt fur innere Medizin 44:105–127 [Google Scholar]
- Haller H 1977 [Epidemiology and associated risk factors of hyperlipoproteinemia]. Z Gesamte Inn Med 32:124–128 [PubMed] [Google Scholar]
- Singer P 1977 [Diagnosis of primary hyperlipoproteinemias]. Z Gesamte Inn Med 32:128 [PubMed] [Google Scholar]
- Vague J 1947 La differenciation sexuelle; facteur determinant des formes de l’obesite. Presse Med 55:339 [PubMed] [Google Scholar]
- Vague J 1954 [Obesity in the development of arteriosclerosis and diabetes.]. Sem Hop 30:3244–3246 [PubMed] [Google Scholar]
- Avogaro P, Crepaldi G, Enzi G, Tiengo A 1965 [Metabolic aspects of essential obesity]. Epatologia 11:226–238 [PubMed] [Google Scholar]
- Phillips GB 1977 Relationship between serum sex hormones and glucose, insulin and lipid abnormalities in men with myocardial infarction. Proc Natl Acad Sci USA 74:1729–1733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaven GM 1997 Banting lecture 1988. Role of insulin resistance in human disease. Nutrition 13:65 [DOI] [PubMed] [Google Scholar]
- Grundy SM 2007 Metabolic syndrome: a multiplex cardiovascular risk factor. J Clin Endocrinol Metab 92:399–404 [DOI] [PubMed] [Google Scholar]
- Ford ES, Giles WH, Mokdad AH 2004 Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care 27:2444–2449 [DOI] [PubMed] [Google Scholar]
- Grundy SM 2006 Does the metabolic syndrome exist? Diabetes Care 29:1689–1692; discussion, 1693–1696 [DOI] [PubMed] [Google Scholar]
- Kahn R, Buse J, Ferrannini E, Stern M 2005 The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 28:2289–2304 [DOI] [PubMed] [Google Scholar]
- Meigs JB 2000 Invited commentary: insulin resistance syndrome? Syndrome X? Multiple metabolic syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol 152:908–911; discussion, 912 [DOI] [PubMed] [Google Scholar]
- Pladevall M, Singal B, Williams LK, Brotons C, Guyer H, Sadurni J, Falces C, Serrano-Rios M, Gabriel R, Shaw JE, Zimmet PZ, Haffner S 2006 A single factor underlies the metabolic syndrome: a confirmatory factor analysis. Diabetes Care 29:113–122 [DOI] [PubMed] [Google Scholar]
- Johnson RJ, Segal MS, Sautin Y, Nakagawa T, Feig DI, Kang DH, Gersch MS, Benner S, Sanchez-Lozada LG 2007 Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease. Am J Clin Nutr 86:899–906 [DOI] [PubMed] [Google Scholar]
- Allen FM 1913 Studies concerning glycosuria and diabetes. Cambridge, MA: Harvard University Press [Google Scholar]
- Concepcion I 1922 Incidence of diabetes mellitus among Filipinos. J Philippine Islands Med Assoc 2:57–61 [Google Scholar]
- Campbell GD 1963 Diabetes in Asians and Africans in and around Durban. S Afr Med J 37:1195–1208 [PubMed] [Google Scholar]
- Campbell GD, Batchelor EL, Goldberg MD 1967 Sugar intake and diabetes. Diabetes 16:62–63 [DOI] [PubMed] [Google Scholar]
- Cleave TL, Campbell GD 1967 The saccharine disease. Am J Proctol 18:202–210 [PubMed] [Google Scholar]
- Yudkin J 1967 Evolutionary and historical changes in dietary carbohydrates. Am J Clin Nutr 20:108–115 [DOI] [PubMed] [Google Scholar]
- Yudkin J 1972 Sugar and disease. Nature 239:197–199 [DOI] [PubMed] [Google Scholar]
- Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD, Purnell JQ, Wheeler M 2004 Nutrition principles and recommendations in diabetes. Diabetes Care 27(Suppl 1):S36–S46 [DOI] [PubMed] [Google Scholar]
- Havel PJ 2005 Dietary fructose: implications for dysregulation of energy homeostasis and lipid/carbohydrate metabolism. Nutr Rev 63:133–157 [DOI] [PubMed] [Google Scholar]
- Nakagawa T, Hu H, Zharikov S, Tuttle KR, Short RA, Glushakova O, Ouyang X, Feig DI, Block ER, Herrera-Acosta J, Patel JM, Johnson RJ 2006 A causal role for uric acid in fructose-induced metabolic syndrome. Am J Physiol 290:F625–F631 [DOI] [PubMed] [Google Scholar]
- Van den Berghe G 1986 Fructose: metabolism and short-term effects on carbohydrate and purine metabolic pathways. Prog Biochem Pharmacol 21:1–32 [PubMed] [Google Scholar]
- Froesch ER 1972 Fructose metabolism in adipose tissue. Acta Med Scand Suppl 542:37–46 [DOI] [PubMed] [Google Scholar]
- Mayes PA 1993 Intermediary metabolism of fructose. Am J Clin Nutr 58:754S–765S [DOI] [PubMed] [Google Scholar]
- Kawasaki T, Akanuma H, Yamanouchi T 2002 Increased fructose concentrations in blood and urine in patients with diabetes. Diabetes Care 25:353–357 [DOI] [PubMed] [Google Scholar]
- Macdonald I, Keyser A, Pacy D 1978 Some effects, in man, of varying the load of glucose, sucrose, fructose, or sorbitol on various metabolites in blood. Am J Clin Nutr 31:1305–1311 [DOI] [PubMed] [Google Scholar]
- Asipu A, Hayward BE, O'Reilly J, Bonthron DT 2003 Properties of normal and mutant recombinant human ketohexokinases and implications for the pathogenesis of essential fructosuria. Diabetes 52:2426–2432 [DOI] [PubMed] [Google Scholar]
- Cirillo P, Gersch MS, Mu W, Scherer PM, Kim KY, Gesualdo L, Henderson GN, Johnson RJ, Sautin YY, Ketohexokinase-dependent proinflammatory effect of fructose in human proximal tubular cells. J Am Soc Nephrol, in press [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maenpaa PH, Raivio KO, Kekomaki MP 1968 Liver adenine nucleotides: fructose-induced depletion and its effect on protein synthesis. Science 161:1253–1254 [DOI] [PubMed] [Google Scholar]
- Maenpaa PH, Raivio KO, Kekomaki MP 1968 Liver adenine nucleotides: fructose-induced depletion and its effect on protein synthesis. Science 161:1253–1254 [DOI] [PubMed] [Google Scholar]
- Bode JC, Zelder O, Rumpelt HJ, Wittkamp U 1973 Depletion of liver adenosine phosphates and metabolic effects of intravenous infusion of fructose or sorbitol in man and in the rat. Eur J Clin Invest 3:436–441 [DOI] [PubMed] [Google Scholar]
- Nair S, P Chacko V, Arnold C, Diehl AM 2003 Hepatic ATP reserve and efficiency of replenishing: comparison between obese and nonobese normal individuals. Am J Gastroenterol 98:466–470 [DOI] [PubMed] [Google Scholar]
- Stanhope KL, Havel PJ 2008 Fructose consumption: potential mechanisms for its effects to increase visceral adiposity and induce dyslipidemia and insulin resistance. Curr Opin Lipidol 19:16–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe BM, Ahuja SP 1977 Effects of intravenously administered fructose and glucose on splanchnic secretion of plasma triglycerides in hypertriglyceridemic men. Metabolism 26:963–978 [DOI] [PubMed] [Google Scholar]
- Swarbrick MM, Stanhope KL, Elliott SS, Graham JL, Krauss RM, Christiansen MP, Griffen SC, Keim NL, Havel PJ 2008 Consumption of fructose-sweetened beverages for 10 weeks increases postprandial triacylglycerol and apolipoprotein-B concentrations in overweight and obese women. Br J Nutr 100:947–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerman Z, Oron-Herman M, Grozovski M, Rosenthal T, Pappo O, Link G, Sela BA 2005 Fructose-induced fatty liver disease: hepatic effects of blood pressure and plasma triglyceride reduction. Hypertension 45:1012–1018 [DOI] [PubMed] [Google Scholar]
- Ouyang X, Cirillo P, Sautin Y, McCall S, Bruchette JL, Diehl AM, Johnson RJ, Abdelmalek MF 2008 Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J Hepatol 48:993–999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RJ, Sautin YY, Oliver WJ, Roncal C, Mu W, Gabriela Sanchez-Lozada L, Rodriguez-Iturbe B, Nakagawa T, Benner SA 23 July 2008 Lessons from comparative physiology: could uric acid represent a physiologic alarm signal gone awry in western society? J Comp Physiol [B] 10.1007/s00360-008-0291-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perheentupa J, Raivio K 1967 Fructose-induced hyperuricaemia. Lancet 2:528–531 [DOI] [PubMed] [Google Scholar]
- Morris Jr RC, Nigon K, Reed EB 1978 Evidence that the severity of depletion of inorganic phosphate determines the severity of the disturbance of adenine nucleotide metabolism in the liver and renal cortex of the fructose-loaded rat. J Clin Invest 61:209–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiaschi E, Baggio B, Favaro S, Antonello A, Camerin E, Todesco S, Borsatti A 1977 Fructose-induced hyperuricemia in essential hypertension. Metabolism 26:1219–1223 [DOI] [PubMed] [Google Scholar]
- Stirpe F, Della Corte E, Bonetti E, Abbondanza A, Abbati A, De Stefano F 1970 Fructose-induced hyperuricaemia. Lancet 2:1310–1311 [DOI] [PubMed] [Google Scholar]
- Israel KD, Michaelis 4th OE, Reiser S, Keeney M 1983 Serum uric acid, inorganic phosphorus, and glutamic-oxalacetic transaminase and blood pressure in carbohydrate-sensitive adults consuming three different levels of sucrose. Ann Nutr Metab 27:425–435 [DOI] [PubMed] [Google Scholar]
- Reiser S, Powell AS, Scholfield DJ, Panda P, Ellwood KC, Canary JJ 1989 Blood lipids, lipoproteins, apoproteins, and uric acid in men fed diets containing fructose or high-amylose cornstarch. Am J Clin Nutr 49:832–839 [DOI] [PubMed] [Google Scholar]
- Choi HK, Curhan G 2008 Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. BMJ 336:309–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi JW, Ford ES, Gao X, Choi HK 2007 Sugar-sweetened soft drinks, diet soft drinks, and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum 59:109–116 [DOI] [PubMed] [Google Scholar]
- Gao X, Qi L, Qiao N, Choi HK, Curhan G, Tucker KL, Ascherio A 2007 Intake of added sugar and sugar-sweetened drink and serum uric acid concentration in US men and women. Hypertension 50:306–312 [DOI] [PubMed] [Google Scholar]
- Burant CF, Saxena M 1994 Rapid reversible substrate regulation of fructose transporter expression in rat small intestine and kidney. Am J Physiol 267:G71–G79 [DOI] [PubMed] [Google Scholar]
- Korieh A, Crouzoulon G 1991 Dietary regulation of fructose metabolism in the intestine and in the liver of the rat. Duration of the effects of a high fructose diet after the return to the standard diet. Arch Int Physiol Biochim Biophys 99:455–460 [PubMed] [Google Scholar]
- Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, Hu FB 2004 Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 292:927–934 [DOI] [PubMed] [Google Scholar]
- Hallfrisch J, Ellwood KC, Michaelis 4th OE, Reiser S, O'Dorisio TM, Prather ES 1983 Effects of dietary fructose on plasma glucose and hormone responses in normal and hyperinsulinemic men. J Nutr 113:1819–1826 [DOI] [PubMed] [Google Scholar]
- Hallfrisch J, Reiser S, Prather ES 1983 Blood lipid distribution of hyperinsulinemic men consuming three levels of fructose. Am J Clin Nutr 37:740–748 [DOI] [PubMed] [Google Scholar]
- Stanhope KL, Griffen SC, Keim NL, Ai M, Otokozawa S, Nakajima K, Schaefer E, Havel PJ 2007 Consumption of fructose-, but not glucose-sweetened beverages produces an atherogenic lipid profile in overweight/obese men and women. Diabetes 56(Suppl 1):A16 [Google Scholar]
- Moore MC, Cherrington AD, Mann SL, Davis SN 2000 Acute fructose administration decreases the glycemic response to an oral glucose tolerance test in normal adults. J Clin Endocrinol Metab 85:4515–4519 [DOI] [PubMed] [Google Scholar]
- Shiota M, Galassetti P, Monohan M, Neal DW, Cherrington AD 1998 Small amounts of fructose markedly augment net hepatic glucose uptake in the conscious dog. Diabetes 47:867–873 [DOI] [PubMed] [Google Scholar]
- Shiota M, Moore MC, Galassetti P, Monohan M, Neal DW, Shulman GI, Cherrington AD 2002 Inclusion of low amounts of fructose with an intraduodenal glucose load markedly reduces postprandial hyperglycemia and hyperinsulinemia in the conscious dog. Diabetes 51:469–478 [DOI] [PubMed] [Google Scholar]
- 2002 American Diabetes Association position statement: evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. J Am Diet Assoc 102:109–118 [DOI] [PubMed] [Google Scholar]
- Portman OW, Lawry EY, Bruno D 1956 Effect of dietary carbohydrate on experimentally induced hypercholesteremia and hyperbetalipoproteinemia in rats. Proc Soc Exp Biol Med 91:321–323 [DOI] [PubMed] [Google Scholar]
- al-Nagdy S, Miller DS, Yudkin J 1970 Changes in body composition and metabolism induced by sucrose in the rat. Nutr Metab 12:193–219 [DOI] [PubMed] [Google Scholar]
- Sleder J, Chen YD, Cully MD, Reaven GM 1980 Hyperinsulinemia in fructose-induced hypertriglyceridemia in the rat. Metabolism 29:303–305 [DOI] [PubMed] [Google Scholar]
- Bruckdorfer KR, Kang SS, Yudkin J 1973 Plasma concentrations of insulin, corticosterone, lipids and sugars in rats fed on meals with glucose and fructose. Proc Nutr Soc 32:12A–13A [PubMed] [Google Scholar]
- Reungjui S, Roncal CA, Mu W, Srinivas TR, Sirivongs D, Johnson RJ, Nakagawa T 2007 Thiazide diuretics exacerbate fructose-induced metabolic syndrome. J Am Soc Nephrol 18:2724–2731 [DOI] [PubMed] [Google Scholar]
- Yadav H, Jain S, Prasad GB, Yadav M 2007 Preventive effect of diabegon, a polyherbal preparation, during progression of diabetes induced by high-fructose feeding in rats. J Pharmacol Sci 105:12–21 [DOI] [PubMed] [Google Scholar]
- Rajasekar P, Anuradha CV 2007 Fructose-induced hepatic gluconeogenesis: effect of L-carnitine. Life Sci 80:1176–1183 [DOI] [PubMed] [Google Scholar]
- Yadav H, Jain S, Sinha PR 2007 Antidiabetic effect of probiotic dahi containing Lactobacillus acidophilus and Lactobacillus casei in high fructose fed rats. Nutrition 23:62–68 [DOI] [PubMed] [Google Scholar]
- Lee YC, Ko YH, Hsu YP, Ho LT 2006 Plasma leptin response to oral glucose tolerance and fasting/re-feeding tests in rats with fructose-induced metabolic derangements. Life Sci 78:1155–1162 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lozada LG, Tapia E, Bautista-Garcia P, Soto V, Avila-Casado C, Vega-Campos IP, Nakagawa T, Zhao L, Franco M, Johnson RJ 2008 Effects of febuxostat on metabolic and renal alterations in rats with fructose-induced metabolic syndrome. Am J Physiol 294:F710–F718 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lozada LG, Tapia E, Jimenez A, Bautista P, Cristobal M, Nepomuceno T, Soto V, Avila-Casado C, Nakagawa T, Johnson RJ, Herrera-Acosta J, Franco M 2007 Fructose-induced metabolic syndrome is associated with glomerular hypertension and renal microvascular damage in rats. Am J Physiol 292:F423–F429 [DOI] [PubMed] [Google Scholar]
- Farah V, Elased KM, Chen Y, Key MP, Cunha TS, Irigoyen MC, Morris M 2006 Nocturnal hypertension in mice consuming a high fructose diet. Auton Neurosci 130:41–50 [DOI] [PubMed] [Google Scholar]
- Katakam PV, Ujhelyi MR, Hoenig ME, Miller AW 1998 Endothelial dysfunction precedes hypertension in diet-induced insulin resistance. Am J Physiol 275:R788–R792 [DOI] [PubMed] [Google Scholar]
- Song D, Hutchings S, Pang CC 2005 Chronic N-acetylcysteine prevents fructose-induced insulin resistance and hypertension in rats. Eur J Pharmacol 508:205–210 [DOI] [PubMed] [Google Scholar]
- Verma S, Bhanot S, McNeill JH 1999 Sympathectomy prevents fructose-induced hyperinsulinemia and hypertension. Eur J Pharmacol 373:R1–R4 [DOI] [PubMed] [Google Scholar]
- Miatello R, Cruzado M, Risler N 2004 Mechanisms of cardiovascular changes in an experimental model of syndrome X and pharmacological intervention on the renin-angiotensin-system. Curr Vasc Pharmacol 2:371–377 [DOI] [PubMed] [Google Scholar]
- Baret G, Peyronnet J, Grassi-Kassisse D, Dalmaz Y, Wiernsperger N, Geloen A 2002 Increased intraabdominal adipose tissue mass in fructose fed rats: correction by metformin. Exp Clin Endocrinol Diabetes 110:298–303 [DOI] [PubMed] [Google Scholar]
- Shapiro A, Mu W, Roncal CA, Cheng KY, Johnson RJ, Scarpace PJ 2008 Fructose-induced leptin resistance exacerbates weight gain in response to subsequent high fat feeding. Am J Physiol Regul Integr Comp Physiol 295:R1370–R1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Muntner P, Hamm LL, Jones DW, Batuman V, Fonseca V, Whelton PK, He J 2004 The metabolic syndrome and chronic kidney disease in U.S. adults. Ann Intern Med 140:167–174 [DOI] [PubMed] [Google Scholar]
- Gersch MS, Mu W, Cirillo P, Reungjui S, Zhang L, Roncal C, Sautin YY, Johnson RJ, Nakagawa T 2007 Fructose, but not dextrose, accelerates the progression of chronic kidney disease. Am J Physiol 293:F1256–F1261 [DOI] [PubMed] [Google Scholar]
- Vasdev S, Gill V, Parai S, Gadag V 2007 Fructose-induced hypertension in Wistar-Kyoto rats: interaction with moderately high dietary salt. Can J Physiol Pharmacol 85:413–421 [DOI] [PubMed] [Google Scholar]
- Avena NM, Rada P, Hoebel BG 2006 Sugar bingeing in rats. Curr Protoc Neurosci Chapter 9:Unit9.23C [DOI] [PubMed] [Google Scholar]
- Avena NM, Rada P, Hoebel BG 2008 Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev 32:20–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Thanos PK, Fowler JS 2004 Similarity between obesity and drug addiction as assessed by neurofunctional imaging: a concept review. J Addict Dis 23:39–53 [DOI] [PubMed] [Google Scholar]
- Roy D, Perreault M, Marette A 1998 Insulin stimulation of glucose uptake in skeletal muscles and adipose tissues in vivo is NO dependent. Am J Physiol 274:E692–E699 [DOI] [PubMed] [Google Scholar]
- Duplain H, Burcelin R, Sartori C, Cook S, Egli M, Lepori M, Vollenweider P, Pedrazzini T, Nicod P, Thorens B, Scherrer U 2001 Insulin resistance, hyperlipidemia, and hypertension in mice lacking endothelial nitric oxide synthase. Circulation 104:342–345 [DOI] [PubMed] [Google Scholar]
- Khosla UM, Zharikov S, Finch JL, Nakagawa T, Roncal C, Mu W, Krotova K, Block ER, Prabhakar S, Johnson RJ 2005 Hyperuricemia induces endothelial dysfunction. Kidney Int 67:1739–1742 [DOI] [PubMed] [Google Scholar]
- Kang DH, Park SK, Lee IK, Johnson RJ 2005 Uric acid-induced C-reactive protein expression: implication on cell proliferation and nitric oxide production of human vascular cells. J Am Soc Nephrol 16:3553–3562 [DOI] [PubMed] [Google Scholar]
- Feig DI, Nakagawa T, Karumanchi SA, Oliver WJ, Kang DH, Finch J, Johnson RJ 2004 Hypothesis: uric acid, nephron number, and the pathogenesis of essential hypertension. Kidney Int 66:281–287 [DOI] [PubMed] [Google Scholar]
- Corry DB, Eslami P, Yamamoto K, Nyby MD, Makino H, Tuck ML 2008 Uric acid stimulates vascular smooth muscle cell proliferation and oxidative stress via the vascular renin-angiotensin system. J Hypertens 26:269–275 [DOI] [PubMed] [Google Scholar]
- Sautin YY, Nakagawa T, Zharikov S, Johnson RJ 2007 Adverse effects of the classical antioxidant uric acid in adipocytes: NADPH oxidase-mediated oxidative/nitrosative stress. Am J Physiol Cell Physiol 293 C584–C596 [DOI] [PubMed] [Google Scholar]
- Zharikov S, Krotova K, Hu H, Baylis C, Johnson RJ, Block ER, Patel JM 2008 Uric acid decreases NO bioavailablity and increases arginase activity in cultured pulmonary artery endothelial cells. Am J Physiol Cell Physiol 295:C1183–C1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gersch C, Palii SP, Kim KM, Angerhofer A, Johnson RJ, Henderson GN 2008 Inactivation of nitric oxide by uric acid. Nucleosides Nucleotides Nucleic Acids 27:967–978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercuro G, Vitale C, Cerquetani E, Zoncu S, Deidda M, Fini M, Rosano GM 2004 Effect of hyperuricemia upon endothelial function in patients at increased cardiovascular risk. Am J Cardiol 94:932–935 [DOI] [PubMed] [Google Scholar]
- Butler R, Morris AD, Belch JJ, Hill A, Struthers AD 2000 Allopurinol normalizes endothelial dysfunction in type 2 diabetics with mild hypertension. Hypertension 35:746–751 [DOI] [PubMed] [Google Scholar]
- Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, Nakayama O, Makishima M, Matsuda M, Shimomura I 2004 Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 114:1752–1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung KJ, Tzameli I, Pissios P, Rovira I, Gavrilova O, Ohtsubo T, Chen Z, Finkel T, Flier JS, Friedman JM 2007 Xanthine oxidoreductase is a regulator of adipogenesis and PPARγ activity. Cell Metab 5:115–128 [DOI] [PubMed] [Google Scholar]
- Ames BN, Cathcart R, Schwiers E, Hochstein P 1981 Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: a hypothesis. Proc Natl Acad Sci USA 78:6858–6862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facchini F, Chen YD, Hollenbeck CB, Reaven GM 1991 Relationship between resistance to insulin-mediated glucose uptake, urinary uric acid clearance, and plasma uric acid concentration. JAMA 266:3008–3011 [PubMed] [Google Scholar]
- Quinones GA, Natali A, Baldi S, Frascerra S, Sanna G, Ciociaro D, Ferrannini E 1995 Effect of insulin on uric acid excretion in humans. Am J Physiol 268:E1–E5 [DOI] [PubMed] [Google Scholar]
- Kanellis J, Watanabe S, Li JH, Kang DH, Li P, Nakagawa T, Wamsley A, Sheikh-Hamad D, Lan HY, Feng L, Johnson RJ 2003 Uric acid stimulates monocyte chemoattractant protein-1 production in vascular smooth muscle cells via mitogen-activated protein kinase and cyclooxygenase-2. Hypertension 41:1287–1293 [DOI] [PubMed] [Google Scholar]
- Zharikov SI, Krotova K, Hu H, Baylis C, Johnson RJ, Block ER, Patel JM 2008 Uric acid decreases NO production and increases arginase activity in cultured pulmonary artery endothelial cells. Am J Physiol Cell Physiol 295:C1183–C1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzali M, Kanellis J, Han L, Feng L, Xia YY, Chen Q, Kang DH, Gordon KL, Watanabe S, Nakagawa T, Lan HY, Johnson RJ 2002 Hyperuricemia induces a primary renal arteriolopathy in rats by a blood pressure-independent mechanism. Am J Physiol 282:F991–F997 [DOI] [PubMed] [Google Scholar]
- Rao GN, Corson MA, Berk BC 1991 Uric acid stimulates vascular smooth muscle cell proliferation by increasing platelet-derived growth factor A-chain expression. J Biol Chem 266:8604–8608 [PubMed] [Google Scholar]
- Kang DH, Nakagawa T, Feng L, Watanabe S, Han L, Mazzali M, Truong L, Harris R, Johnson RJ 2002 A role for uric acid in the progression of renal disease. J Am Soc Nephrol 13:2888–2897 [DOI] [PubMed] [Google Scholar]
- Watanabe S, Kang DH, Feng L, Nakagawa T, Kanellis J, Lan H, Mazzali M, Johnson RJ 2002 Uric acid, hominoid evolution, and the pathogenesis of salt-sensitivity. Hypertension 40:355–360 [DOI] [PubMed] [Google Scholar]
- Price KL, Sautin YY, Long DA, Zhang L, Miyazaki H, Mu W, Endou H, Johnson RJ 2006 Human vascular smooth muscle cells express a urate transporter. J Am Soc Nephrol 17:1791–1795 [DOI] [PubMed] [Google Scholar]
- Feig DI, Kang DH, Johnson RJ 2008 Uric acid and cardiovascular risk. N Engl J Med 359:1811–1821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feig DI, Johnson RJ 2003 Hyperuricemia in childhood primary hypertension. Hypertension 42:247–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feig DI, Soletsky B, Johnson RJ 2008 Effect of allopurinol on the blood pressure of adolescents with newly diagnosed essential hypertension. JAMA 300:922–930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oda M, Satta Y, Takenaka O, Takahata N 2002 Loss of urate oxidase activity in hominoids and its evolutionary implications. Mol Biol Evol 19:640–653 [DOI] [PubMed] [Google Scholar]
- Mazzali M, Hughes J, Kim YG, Jefferson JA, Kang DH, Gordon KL, Lan HY, Kivlighn S, Johnson RJ 2001 Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension 38:1101–1106 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lozada LG, Tapia E, Avila-Casado C, Soto V, Franco M, Santamaria J, Nakagawa T, Rodriguez-Iturbe B, Johnson RJ, Herrera-Acosta J 2002 Mild hyperuricemia induces glomerular hypertension in normal rats. Am J Physiol 283:F1105–F1110 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lozada LG, Soto V, Tapia E, Avila-Casado C, Sautin YY, Nakagawa T, Franco M, Rodriguez-Iturbe B, Johnson RJ 2008 Role of oxidative stress in the renal abnormalities induced by experimental hyperuricemia. Am J Physiol Renal Physiol 295:F1134–F1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Lozada LG, Tapia E, Lopez-Molina R, Nepomuceno T, Soto V, Avila-Casado C, Nakagawa T, Johnson RJ, Herrera-Acosta J, Franco M 2007 Effects of acute and chronic L-arginine treatment in experimental hyperuricemia. Am J Physiol 292:F1238–F1244 [DOI] [PubMed] [Google Scholar]
- Johnson RJ, Herrera-Acosta J, Schreiner GF, Rodriguez-Iturbe B 2002 Subtle acquired renal injury as a mechanism of salt-sensitive hypertension. N Engl J Med 346:913–923 [DOI] [PubMed] [Google Scholar]
- Nakagawa T, Mazzali M, Kang DH, Kanellis J, Watanabe S, Sanchez-Lozada LG, Rodriguez-Iturbe B, Herrera-Acosta J, Johnson RJ 2003 Hyperuricemia causes glomerular hypertrophy in the rat. Am J Nephrol 23:2–7 [DOI] [PubMed] [Google Scholar]
- Roncal CA, Mu W, Croker B, Reungjui S, Ouyang X, Tabah-Fisch I, Johnson RJ, Ejaz AA 2007 Effect of elevated serum uric acid on cisplatin-induced acute renal failure. Am J Physiol 292:F116–F122 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lozada LG, Tapia E, Santamaria J, Avila-Casado C, Soto V, Nepomuceno T, Rodriguez-Iturbe B, Johnson RJ, Herrera-Acosta J 2005 Mild hyperuricemia induces vasoconstriction and maintains glomerular hypertension in normal and remnant kidney rats. Kidney Int 67:237–247 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lozada LG, Tapia E, Soto V, Avila-Casado C, Franco M, Wessale JL, Zhao L, Johnson RJ 2008 Effect of febuxostat on the progression of renal disease in 5/6 nephrectomy rats with and without hyperuricemia. Nephron Physiol 108:69–78 [DOI] [PubMed] [Google Scholar]
- Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S 2004 Significance of hyperuricemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis 44:642–650 [PubMed] [Google Scholar]
- Iseki K, Oshiro S, Tozawa M, Iseki C, Ikemiya Y, Takishita S 2001 Significance of hyperuricemia on the early detection of renal failure in a cohort of screened subjects. Hypertens Res 24:691–697 [DOI] [PubMed] [Google Scholar]
- Rosolowsky ET, Ficociello LH, Maselli NJ, Niewczas MA, Binns AL, Roshan B, Warram JH, Krolewski AS 2008 High-normal serum uric acid is associated with impaired glomerular filtration rate in nonproteinuric patients with type 1 diabetes. Clin J Am Soc Nephrol 3:706–713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanbay M, Ozkara A, Selcoki Y, Isik B, Turgut F, Bavbek N, Uz E, Akcay A, Yigitoglu R, Covic A 2007 Effect of treatment of hyperuricemia with allopurinol on blood pressure, creatinine clearance, and proteinuria in patients with normal renal functions. Int Urol Nephrol 39:1227–1233 [DOI] [PubMed] [Google Scholar]
- Siu YP, Leung KT, Tong MK, Kwan TH 2006 Use of allopurinol in slowing the progression of renal disease through its ability to lower serum uric acid level. Am J Kidney Dis 47:51–59 [DOI] [PubMed] [Google Scholar]
- Talaat KM, El-Sheikh AR 2007 The effect of mild hyperuricemia on urinary transforming growth factor β and the progression of chronic kidney disease. Am J Nephrol 27:435–440 [DOI] [PubMed] [Google Scholar]
- Stavric B, Johnson WJ, Clayman S, Gadd RE, Chartrand A 1976 Effect of fructose administration on serum urate levels in the uricase inhibited rat. Experientia 32:373–374 [DOI] [PubMed] [Google Scholar]
- Sanchez-Lozada L, Lopez-Molina R, Soto V, Tapia E, Avila-Casado C, Bautista R, Nakagawa T, Franco M, Johnson RJ 2007 Low fructose caloric intake concomitant to hyperuricemia induces hyperinsulinemia and renal structural damage in rats. J Am Soc Nephrol 18:184A [Google Scholar]
- Vasdev S, Gill V, Parai S, Longerich L, Gadag V 2002 Dietary vitamin E and C supplementation prevents fructose induced hypertension in rats. Mol Cell Biochem 241:107–114 [DOI] [PubMed] [Google Scholar]
- Rumessen JJ, Gudmand-Hoyer E 1986 Absorption capacity of fructose in healthy adults. Comparison with sucrose and its constituent monosaccharides. Gut 27:1161–1168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakely SR, Hallfrisch J, Reiser S, Prather ES 1981 Long-term effects of moderate fructose feeding on glucose tolerance parameters in rats. J Nutr 111:307–314 [DOI] [PubMed] [Google Scholar]
- Le KA, Tappy L 2006 Metabolic effects of fructose. Curr Opin Clin Nutr Metab Care 9:469–475 [DOI] [PubMed] [Google Scholar]
- Segal MS, Gollub E, Johnson RJ 2007 Is the fructose index more relevant with regards to cardiovascular disease than the glycemic index? Eur J Nutr 46:406–417 [DOI] [PubMed] [Google Scholar]
- Beck-Nielsen H, Pedersen O, Lindskov HO 1980 Impaired cellular insulin binding and insulin sensitivity induced by high-fructose feeding in normal subjects. Am J Clin Nutr 33:273–278 [DOI] [PubMed] [Google Scholar]
- Faeh D, Minehira K, Schwarz JM, Periasamy R, Park S, Tappy L 2005 Effect of fructose overfeeding and fish oil administration on hepatic de novo lipogenesis and insulin sensitivity in healthy men. Diabetes 54:1907–1913 [DOI] [PubMed] [Google Scholar]
- Le KA, Faeh D, Stettler R, Ith M, Kreis R, Vermathen P, Boesch C, Ravussin E, Tappy L 2006 A 4-wk high-fructose diet alters lipid metabolism without affecting insulin sensitivity or ectopic lipids in healthy humans. Am J Clin Nutr 84:1374–1379 [DOI] [PubMed] [Google Scholar]
- Stanhope KL, Keim NL, Hellerstein MK, Beysen C, McGahan JP, Griffen SC, Havel PJ 2007 Consumption of fructose-, but not glucose-sweetened beverages for 10 weeks induces glucose intolerance and insulin resistance, and increases visceral adiposity in overweight/obese men and women. Diabetes 57(Suppl A):A101 [Google Scholar]
- Bantle JP, Raatz SK, Thomas W, Georgopoulos A 2000 Effects of dietary fructose on plasma lipids in healthy subjects. Am J Clin Nutr 72:1128–1134 [DOI] [PubMed] [Google Scholar]
- Swanson JE, Laine DC, Thomas W, Bantle JP 1992 Metabolic effects of dietary fructose in healthy subjects. Am J Clin Nutr 55:851–856 [DOI] [PubMed] [Google Scholar]
- Yudkin J, Eisa O, Kang SS, Meraji S, Bruckdorfer KR 1986 Dietary sucrose affects plasma HDL cholesterol concentration in young men. Ann Nutr Metab 30:261–266 [DOI] [PubMed] [Google Scholar]
- Raben A, Vasilaras TH, Moller AC, Astrup A 2002 Sucrose compared with artificial sweeteners: different effects on ad libitum food intake and body weight after 10 wk of supplementation in overweight subjects. Am J Clin Nutr 76:721–729 [DOI] [PubMed] [Google Scholar]
- Brown CM, Dulloo AG, Yepuri G, Montani JP 2008 Fructose ingestion acutely elevates blood pressure in healthy young humans. Am J Physiol 294:R730–R737 [DOI] [PubMed] [Google Scholar]
- Raben A, Macdonald I, Astrup A 1997 Replacement of dietary fat by sucrose or starch: effects on 14 d ad libitum energy intake, energy expenditure and body weight in formerly obese and never-obese subjects. Int J Obes Relat Metab Disord 21:846–859 [DOI] [PubMed] [Google Scholar]
- Teff KL, Elliott SS, Tschop M, Kieffer TJ, Rader D, Heiman M, Townsend RR, Keim NL, D'Alessio D, Havel PJ 2004 Dietary fructose reduces circulating insulin and leptin, attenuates postprandial suppression of ghrelin, and increases triglycerides in women. J Clin Endocrinol Metab 89:2963–2972 [DOI] [PubMed] [Google Scholar]
- Shoham DA, Durazo-Arvizu R, Kramer H, Luke A, Vupputuri S, Kshirsagar A, Cooper RS 2008 Sugary soda consumption and albuminuria: results from the National Health and Nutrition Examination Survey, 1999–2004. PLoS ONE 3:e3431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchal de Calvi A 1864 R′echerches sur les Accidents diab′etiques, et essai d’une th′eorie g′en′erale du diab‘ete. Paris: Asselin [Google Scholar]
- Chakravarti S 1907 Discussion on diabetes in the tropics. IV. Br Med J 19:1056–1057 [Google Scholar]
- Sandwith PM 1907 Discussion on diabetes in the tropics. VI. Br Med J 19:1059–1060 [Google Scholar]
- Cantle J 1907 Discussion on diabetes in the tropics. Br Med J 19:1063 [Google Scholar]
- Hrdlička A 1908 Physiological and medical observations among the Indians of Southwestern United States and Northern Mexico. Washington D.C.: U.S. Government Printing Office [Google Scholar]
- Prior IA, Rose BS, Davidson F 1964 Metabolic maladies in New Zealand Maoris. Br Med J 1:1065–1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright-St Clair RE 1969 Early accounts of Maori diet and health. 1. N Z Med J 70:327–331 [PubMed] [Google Scholar]
- Rose BS 1975 Gout in Maoris. Semin Arthritis Rheum 5:121–145 [DOI] [PubMed] [Google Scholar]
- McLaughlin EC, Wilson I 1945 New Zealand dietary studies. III. Dietary survey among the Maoris. NZ Med J 44:93–98 [Google Scholar]
- Hoy W, Kelly A, Jacups S, McKendry K, Baker P, MacDonald S, Wang Z, Punguatji N, Kerinauia J, Tipiloura E, Tipiloura E, Harrison C 1999 Stemming the tide: reducing cardiovascular disease and renal failure in Australian Aborigines. Aust N Z J Med 29:480–483 [DOI] [PubMed] [Google Scholar]
- Stein JH, West KM, Robey JM, Tirador DF, McDonald GW 1965 The high prevalence of abnormal glucose tolerance in the Cherokee Indians of North Carolina. Arch Intern Med 116:842–845 [PubMed] [Google Scholar]
- Salsbury CG 1947 Incidence of certain diseases among the Navajos. Arizona Med 4:29–31 [PubMed] [Google Scholar]
- Hoffman FL 1928 Cancer among North American Indians: the health progress of the North American Indian. The Indian as a life insurance risk. Newark, NJ: Prudential Press [Google Scholar]
- Joslin EP 1940 The universality of diabetes: a survey of diabetic morbidity in Arizona. JAMA 115:2033–2038 [Google Scholar]
- Bell AC, Swinburn BA, Amosa H, Scragg R, Sharpe SJ 1999 The impact of modernisation on the diets of adults aged 20–40 years from Samoan church communities in Auckland. Asia Pac J Public Health 11:4–9 [DOI] [PubMed] [Google Scholar]
- Lee AJ, O'Dea K, Mathews JD 1994 Apparent dietary intake in remote aboriginal communities. Aust J Public Health 18:190–197 [DOI] [PubMed] [Google Scholar]
- Mills CA 1930 Diabetes mellitus: sugar consumption in its etiology. Arch Intern Med 46:582–584 [Google Scholar]
- Albertsson MD 1953 Diabetes in Iceland. Diabetes 2:184–186 [DOI] [PubMed] [Google Scholar]
- Simmonds HA, McBride MB, Hatfield PJ, Graham R, McCaskey J, Jackson M 1994 Polynesian women are also at risk for hyperuricaemia and gout because of a genetic defect in renal urate handling. Br J Rheumatol 33:932–937 [DOI] [PubMed] [Google Scholar]
- Saile F 1930 Uber den EinfluB der vegetarischen Ernahrung auf den Blutdruck. Med Klin 25:929–931 [Google Scholar]
- Jackson WP, Campbell GD, Joffe BI, Goldberg MD 1978 Hyperglycaemia among vegetarians. S Afr Med J 53:880–881 [PubMed] [Google Scholar]
- Fernando HM 1907 Discussion on diabetes in the tropics. Discussion. Br Med J 19:1060 [Google Scholar]
- Ziemann H 1907 Discussion on diabetes in the tropics. Discussion. Br Med J 19:1061 [Google Scholar]
- Adams J 1930 Some racial differences in blood pressure and morbidity in a group of white and colored workers. Am J Med Sci 184:342–350 [Google Scholar]
- Saunders G, Bancroft H 1942 Blood pressure in African Americans. Nutr Rev 23:410–423 [Google Scholar]
- Tulloch JA 1961 The prevalence of diabetes mellitus in Jamaica. Diabetes 10:286–288 [DOI] [PubMed] [Google Scholar]
- Dresser C 1979 Food consumption profiles of white and black persons aged 1–74 years: United States 1971–1974. Vital and Health Statistics Series 11, no. 210. Hyattsville, MD: National Center for Health Statistics [PubMed] [Google Scholar]
- Kerr GR, Amante P, Decker M, Callen PW 1983 Supermarket sales of high-sugar products in predominantly Black, Hispanic, and white census tracts of Houston, Texas. Am J Clin Nutr 37:622–631 [DOI] [PubMed] [Google Scholar]
- Cohen AM, Bavly S, Poznanski R 1961 Change of diet of Yemenite Jews in relation to diabetes and ischaemic heart-disease. Lancet 2:1399–1401 [DOI] [PubMed] [Google Scholar]
- Healey LA, Skeith MD, Decker JL, Bayani-Sioson PS 1967 Hyperuricemia in Filipinos: interaction of heredity and environment. Am J Hum Genet 19:81–85 [PMC free article] [PubMed] [Google Scholar]
- Kagan A, Harris BR, Winkelstein Jr W, Johnson KG, Kato H, Syme SL, Rhoads GG, Gay ML, Nichaman MZ, Hamilton HB, Tillotson J 1974 Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: demographic, physical, dietary and biochemical characteristics. J Chronic Dis 27:345–364 [DOI] [PubMed] [Google Scholar]
- Bray GA, Nielsen SJ, Popkin BM 2004 Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr 79:537–543 [DOI] [PubMed] [Google Scholar]
- Ludwig DS, Peterson KE, Gortmaker SL 2001 Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 357:505–508 [DOI] [PubMed] [Google Scholar]
- Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, D'Agostino RB, Gaziano JM, Vasan RS 2007 Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 116:480–488 [DOI] [PubMed] [Google Scholar]
- McNaughton SA, Mishra GD, Brunner EJ 2008 Dietary patterns, insulin resistance and incidence of type 2 diabetes in the Whitehall II study. Diabetes Care 31:1343–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montonen J, Jarvinen R, Knekt P, Heliovaara M, Reunanen A 2007 Consumption of sweetened beverages and intakes of fructose and glucose predict type 2 diabetes occurrence. J Nutr 137:1447–1454 [DOI] [PubMed] [Google Scholar]
- Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, Rosenberg L 2008 Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med 168:1487–1492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzano LA, Li TY, Joshipura KJ, Hu FB 2008 Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care 31:1311–1317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsouli SG, Liberopoulos EN, Mikhailidis DP, Athyros VG, Elisaf MS 2006 Elevated serum uric acid levels in metabolic syndrome: an active component or an innocent bystander? Metabolism 55:1293–1301 [DOI] [PubMed] [Google Scholar]
- Choi HK, Ford ES 2007 Prevalence of the metabolic syndrome in individuals with hyperuricemia. Am J Med 120:442–447 [DOI] [PubMed] [Google Scholar]
- Choi HK, Ford ES, Li C, Curhan G 2007 Prevalence of the metabolic syndrome in patients with gout: the Third National Health and Nutrition Examination Survey. Arthritis Rheum 57:109–115 [DOI] [PubMed] [Google Scholar]
- Saggiani F, Pilati S, Targher G, Branzi P, Muggeo M, Bonora E 1996 Serum uric acid and related factors in 500 hospitalized subjects. Metabolism 45:1557–1561 [DOI] [PubMed] [Google Scholar]
- Ford ES, Li C, Cook S, Choi HK 2007 Serum concentrations of uric acid and the metabolic syndrome among US children and adolescents. Circulation 115:2526–2532 [DOI] [PubMed] [Google Scholar]
- Denzer C, Muche R, Mayer H, Heinze E, Debatin KM, Wabitsch M 2003 Serum uric acid levels in obese children and adolescents: linkage to testosterone levels and pre-metabolic syndrome. J Pediatr Endocrinol Metab 16:1225–1232 [DOI] [PubMed] [Google Scholar]
- Buchanan KD 1972 Diabetes mellitus and gout. Semin Arthritis Rheum 2:157–163 [DOI] [PubMed] [Google Scholar]
- Hochberg MC, Thomas J, Thomas DJ, Mead L, Levine DM, Klag MJ 1995 Racial differences in the incidence of gout. The role of hypertension. Arthritis Rheum 38:628–632 [DOI] [PubMed] [Google Scholar]
- McKechnie JK 1964 Gout, hyperuricaemia and carbohydrate metabolism. S Afr Med J 38:182–185 [PubMed] [Google Scholar]
- Chan KH, Segasothy M 2004 Gouty arthritis in Australian Aboriginals: more common than previously suspected. Med J Aust 181:172 [DOI] [PubMed] [Google Scholar]
- Tuomilehto J, Zimmet P, Wolf E, Taylor R, Ram P, King H 1988 Plasma uric acid level and its association with diabetes mellitus and some biologic parameters in a biracial population of Fiji. Am J Epidemiol 127:321–336 [DOI] [PubMed] [Google Scholar]
- Bo S, Cavallo-Perin P, Gentile L, Repetti E, Pagano G 2001 Hypouricemia and hyperuricemia in type 2 diabetes: two different phenotypes. Eur J Clin Invest 31:318–321 [DOI] [PubMed] [Google Scholar]
- Muscelli E, Natali A, Bianchi S, Bigazzi R, Galvan AQ, Sironi AM, Frascerra S, Ciociaro D, Ferrannini E 1996 Effect of insulin on renal sodium and uric acid handling in essential hypertension. Am J Hypertens 9:746–752 [DOI] [PubMed] [Google Scholar]
- Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN 2008 Uric acid and the development of metabolic syndrome in women and men. Metabolism 57:845–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu S, Song J, Choi BY, Lee SJ, Kim WS, Chang Y, Kim DI, Suh BS, Sung KC 2007 Incidence and risk factors for metabolic syndrome in Korean male workers, ages 30 to 39. Ann Epidemiol 17:245–252 [DOI] [PubMed] [Google Scholar]
- Nakagawa T, Tuttle KR, Short RA, Johnson RJ 2005 Fructose-induced hyperuricemia as a casual mechanism for the epidemic of the metabolic syndrome. Nat Clin Pract Nephrol 1:80–86 [DOI] [PubMed] [Google Scholar]
- Carnethon MR, Fortmann SP, Palaniappan L, Duncan BB, Schmidt MI, Chambless LE 2003 Risk factors for progression to incident hyperinsulinemia: the Atherosclerosis Risk in Communities Study, 1987–1998. Am J Epidemiol 158:1058–1067 [DOI] [PubMed] [Google Scholar]
- Niskanen L, Laaksonen DE, Lindstrom J, Eriksson JG, Keinanen-Kiukaanniemi S, Ilanne-Parikka P, Aunola S, Hamalainen H, Tuomilehto J, Uusitupa M 2006 Serum uric acid as a harbinger of metabolic outcome in subjects with impaired glucose tolerance: the Finnish Diabetes Prevention Study. Diabetes Care 29:709–711 [DOI] [PubMed] [Google Scholar]
- Masuo K, Kawaguchi H, Mikami H, Ogihara T, Tuck ML 2003 Serum uric acid and plasma norepinephrine concentrations predict subsequent weight gain and blood pressure elevation. Hypertension 42:474–480 [DOI] [PubMed] [Google Scholar]
- Lonardo A, Loria P, Leonardi F, Borsatti A, Neri P, Pulvirenti M, Verrone AM, Bagni A, Bertolotti M, Ganazzi D, Carulli N 2002 Fasting insulin and uric acid levels but not indices of iron metabolism are independent predictors of non-alcoholic fatty liver disease. A case-control study. Dig Liver Dis 34:204–211 [DOI] [PubMed] [Google Scholar]
- Boyko EJ, de Courten M, Zimmet PZ, Chitson P, Tuomilehto J, Alberti KG 2000 Features of the metabolic syndrome predict higher risk of diabetes and impaired glucose tolerance: a prospective study in Mauritius. Diabetes Care 23:1242–1248 [DOI] [PubMed] [Google Scholar]
- Lin KC, Tsai ST, Lin HY, Chou P 2004 Different progressions of hyperglycemia and diabetes among hyperuricemic men and women in the kinmen study. J Rheumatol 31:1159–1165 [PubMed] [Google Scholar]
- Nakanishi N, Okamoto M, Yoshida H, Matsuo Y, Suzuki K, Tatara K 2003 Serum uric acid and risk for development of hypertension and impaired fasting glucose or type II diabetes in Japanese male office workers. Eur J Epidemiol 18:523–530 [DOI] [PubMed] [Google Scholar]
- Dehghan A, van Hoek M, Sijbrands EJ, Hofman A, Witteman JC 2008 High serum uric acid as a novel risk factor for type 2 diabetes. Diabetes Care 31:361–362 [DOI] [PubMed] [Google Scholar]
- Perry IJ, Wannamethee SG, Walker MK, Thomson AG, Whincup PH, Shaper AG 1995 Prospective study of risk factors for development of non-insulin dependent diabetes in middle aged British men. BMJ 310:560–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohlson LO, Larsson B, Bjorntorp P, Eriksson H, Svardsudd K, Welin L, Tibblin G, Wilhelmsen L 1988 Risk factors for type 2 (non-insulin-dependent) diabetes mellitus. Thirteen and one-half years of follow-up of the participants in a study of Swedish men born in 1913. Diabetologia 31:798–805 [DOI] [PubMed] [Google Scholar]
- Nan H, Qiao Q, Soderberg S, Pitkaniemi J, Zimmet P, Shaw J, Alberti G, Uusitalo U, Pauvaday V, Chitson P, Tuomilehto J 2008 Serum uric acid and incident diabetes in Mauritian Indian and Creole populations. Diabetes Res Clin Pract 80:321–327 [DOI] [PubMed] [Google Scholar]
- Brand FN, McGee DL, Kannel WB, Stokes 3rd J, Castelli WP 1985 Hyperuricemia as a risk factor of coronary heart disease: the Framingham Study. Am J Epidemiol 121:11–18 [DOI] [PubMed] [Google Scholar]
- Herman JB, Goldbourt U 1982 Uric acid and diabetes: observations in a population study. Lancet 2:240–243 [DOI] [PubMed] [Google Scholar]
- Herman JB, Medalie JH, Goldbourt U 1976 Diabetes, prediabetes and uricaemia. Diabetologia 12:47–52 [DOI] [PubMed] [Google Scholar]
- Medalie JH, Papier CM, Goldbourt U, Herman JB 1975 Major factors in the development of diabetes mellitus in 10,000 men. Arch Intern Med 135:811–817 [PubMed] [Google Scholar]
- Balkau B, King H, Zimmet P, Raper LR 1985 Factors associated with the development of diabetes in the Micronesian population of Nauru. Am J Epidemiol 122:594–605 [DOI] [PubMed] [Google Scholar]
- Chien KL, Chen MF, Hsu HC, Chang WT, Su TC, Lee YT, Hu FB 2008 Plasma uric acid and the risk of type 2 diabetes in a Chinese community. Clin Chem 54:310–316 [DOI] [PubMed] [Google Scholar]
- Choi HK, De Vera MA, Krishnan E 2008 Gout and the risk of type 2 diabetes among men with a high cardiovascular risk profile. Rheumatology (Oxford) 47:1567–1570 [DOI] [PubMed] [Google Scholar]
- Taniguchi Y, Hayashi T, Tsumura K, Endo G, Fujii S, Okada K 2001 Serum uric acid and the risk for hypertension and type 2 diabetes in Japanese men: the Osaka Health Survey. J Hypertens 19:1209–1215 [DOI] [PubMed] [Google Scholar]
- Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G 2004 Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med 350:1093–1103 [DOI] [PubMed] [Google Scholar]
- Snowdon DA, Phillips RL 1985 Does a vegetarian diet reduce the occurrence of diabetes? Am J Public Health 75:507–512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung TT, Schulze M, Manson JE, Willett WC, Hu FB 2004 Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med 164:2235–2240 [DOI] [PubMed] [Google Scholar]
- Schulze MB, Manson JE, Willett WC, Hu FB 2003 Processed meat intake and incidence of type 2 diabetes in younger and middle-aged women. Diabetologia 46:1465–1473 [DOI] [PubMed] [Google Scholar]
- Zhang C, Schulze MB, Solomon CG, Hu FB 2006 A prospective study of dietary patterns, meat intake and the risk of gestational diabetes mellitus. Diabetologia 49:2604–2613 [DOI] [PubMed] [Google Scholar]
- van Dam RM, Willett WC, Rimm EB, Stampfer MJ, Hu FB 2002 Dietary fat and meat intake in relation to risk of type 2 diabetes in men. Diabetes Care 25:417–424 [DOI] [PubMed] [Google Scholar]
- Song Y, Manson JE, Buring JE, Liu S 2004 A prospective study of red meat consumption and type 2 diabetes in middle-aged and elderly women: the women’s health study. Diabetes Care 27:2108–2115 [DOI] [PubMed] [Google Scholar]
- Choi HK, Curhan G 2004 Beer, liquor, and wine consumption and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum 51:1023–1029 [DOI] [PubMed] [Google Scholar]
- Ka T, Moriwaki Y, Inokuchi T, Yamamoto A, Takahashi S, Tsutsumi Z, Yamamoto T 2006 Effects of allopurinol on beer-induced increases in plasma concentrations and urinary excretion of purine bases (uric acid, hypoxanthine, and xanthine). Horm Metab Res 38:188–192 [DOI] [PubMed] [Google Scholar]
- Campbell GD, Batchelor EL, Goldberg MD 1967 Sugar intake and diabetes. Diabetes 16:62–63 [DOI] [PubMed] [Google Scholar]
- Duncan BB, Chambless LE, Schmidt MI, Folsom AR, Szklo M, Crouse 3rd JR, Carpenter MA 1995 Association of the waist-to-hip ratio is different with wine than with beer or hard liquor consumption. Atherosclerosis Risk in Communities Study Investigators. Am J Epidemiol 142:1034–1038 [DOI] [PubMed] [Google Scholar]
- Jacob S 2005 [Patient with beer belly or hypertension. Check for a metabolic syndrome!]. MMW Fortschritte der Medizin 147:45 [PubMed] [Google Scholar]
- Wannamethee SG, Shaper AG, Perry IJ, Alberti KG 2002 Alcohol consumption and the incidence of type II diabetes. J Epidemiol Community Health 56:542–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbrook RL, Barrett-Connor E, Wingard DL 1990 A prospective population-based study of alcohol and non-insulin dependent diabetes mellitus. Am J Epidemiol 132:902–909 [DOI] [PubMed] [Google Scholar]
- Balkau B, Randrianjohany A, Papoz L, Eschwege E 1991 A prospective study of alcohol use and non-insulin-dependent diabetes mellitus. Am J Epidemiol 134:1469–1470 [DOI] [PubMed] [Google Scholar]
- Choi HK, Curhan G 2007 Coffee, tea, and caffeine consumption and serum uric acid level: the Third National Health and Nutrition Examination Survey. Arthritis Rheum 57:816–821 [DOI] [PubMed] [Google Scholar]
- Campos H, Baylin A 2007 Coffee consumption and risk of type 2 diabetes and heart disease. Nutr Rev 65:173–179 [DOI] [PubMed] [Google Scholar]
- Tofovic SP, Kusaka H, Jackson EK, Bastacky SI 2001 Renal and metabolic effects of caffeine in obese (fa/fa(cp)), diabetic, hypertensive ZSF1 rats. Ren Fail 23:159–173 [DOI] [PubMed] [Google Scholar]
- Liu S, Choi HK, Ford E, Song Y, Klevak A, Buring JE, Manson JE 2006 A prospective study of dairy intake and the risk of type 2 diabetes in women. Diabetes Care 29:1579–1584 [DOI] [PubMed] [Google Scholar]
- Johnson RJ, Gaucher EA, Sautin YY, Henderson GN, Angerhofer AJ, Benner SA 2008 The planetary biology of ascorbate and uric acid and their relationship with the epidemic of obesity and cardiovascular disease. Med Hypotheses 71:22–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao X, Curhan G, Forman JP, Ascherio A, Choi HK 2008 Vitamin C intake and serum uric acid concentration in men. J Rheumatol 35:1853–1858 [PMC free article] [PubMed] [Google Scholar]
- Huang HY, Appel LJ, Choi MJ, Gelber AC, Charleston J, Norkus EP, Miller 3rd ER 2005 The effects of vitamin C supplementation on serum concentrations of uric acid: results of a randomized controlled trial. Arthritis Rheum 52:1843–1847 [DOI] [PubMed] [Google Scholar]
- Zhang C, Williams MA, Frederick IO, King IB, Sorensen TK, Kestin MM, Dashow EE, Luthy DA 2004 Vitamin C and the risk of gestational diabetes mellitus: a case-control study. J Reprod Med 49:257–266 [PubMed] [Google Scholar]
- Feskens EJ, Virtanen SM, Rasanen L, Tuomilehto J, Stengard J, Pekkanen J, Nissinen A, Kromhout D 1995 Dietary factors determining diabetes and impaired glucose tolerance. A 20-year follow-up of the Finnish and Dutch cohorts of the Seven Countries Study. Diabetes Care 18:1104–1112 [DOI] [PubMed] [Google Scholar]
- Afkhami-Ardekani M, Shojaoddiny-Ardekani A 2007 Effect of vitamin C on blood glucose, serum lipids, serum insulin in type 2 diabetes patients. Indian J Med Res 126:471–474 [PubMed] [Google Scholar]
- Lindholm LH, Persson M, Alaupovic P, Carlberg B, Svensson A, Samuelsson O 2003 Metabolic outcome during 1 year in newly detected hypertensives: results of the Antihypertensive Treatment and Lipid Profile in a North of Sweden Efficacy Evaluation (ALPINE study). J Hypertens 21:1563–1574 [DOI] [PubMed] [Google Scholar]
- Verdecchia P, Reboldi G, Angeli F, Borgioni C, Gattobigio R, Filippucci L, Norgiolini S, Bracco C, Porcellati C 2004 Adverse prognostic significance of new diabetes in treated hypertensive subjects. Hypertension 43:963–969 [DOI] [PubMed] [Google Scholar]
- Ekong EB, Jaar BG, Weaver VM 2006 Lead-related nephrotoxicity: a review of the epidemiologic evidence. Kidney Int 70:2074–2084 [DOI] [PubMed] [Google Scholar]
- Emmerson BT 1963 Chronic lead nephropathy: the diagnostic use of calcium EDTA and the association with gout. Australas Ann Med 12:310–324 [DOI] [PubMed] [Google Scholar]
- Bener A, Obineche E, Gillett M, Pasha MA, Bishawi B 2001 Association between blood levels of lead, blood pressure and risk of diabetes and heart disease in workers. Int Arch Occup Environ Health 74:375–378 [DOI] [PubMed] [Google Scholar]
- Mazzali M, Kim YG, Suga S, Gordon KL, Kang DH, Jefferson JA, Hughes J, Kivlighn SD, Lan HY, Johnson RJ 2001 Hyperuricemia exacerbates chronic cyclosporine nephropathy. Transplantation 71:900–905 [DOI] [PubMed] [Google Scholar]
- Kang DH, Finch J, Nakagawa T, Karumanchi SA, Kanellis J, Granger J, Johnson RJ 2004 Uric acid, endothelial dysfunction and pre-eclampsia: searching for a pathogenetic link. J Hypertens 22:229–235 [DOI] [PubMed] [Google Scholar]
- Bainbridge SA, Roberts JM 2008 Uric acid as a pathogenic factor in preeclampsia. Placenta 29(Suppl A):S67–S72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JM, Bodnar LM, Lain KY, Hubel CA, Markovic N, Ness RB, Powers RW 2005 Uric acid is as important as proteinuria in identifying fetal risk in women with gestational hypertension. Hypertension 46:1263–1269 [DOI] [PubMed] [Google Scholar]
- Clausen T, Slott M, Solvoll K, Drevon CA, Vollset SE, Henriksen T 2001 High intake of energy, sucrose, and polyunsaturated fatty acids is associated with increased risk of preeclampsia. Am J Obstet Gynecol 185:451–458 [DOI] [PubMed] [Google Scholar]
- Ogryzlo MA 1965 Hyperuricemia induced by high fat diets and starvation. Arthritis Rheum 8:799–822 [DOI] [PubMed] [Google Scholar]
- Gross LS, Li L, Ford ES, Liu S 2004 Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. Am J Clin Nutr 79:774–779 [DOI] [PubMed] [Google Scholar]
- McPherson JD, Shilton BH, Walton DJ 1988 Role of fructose in glycation and cross-linking of proteins. Biochemistry 27:1901–1907 [DOI] [PubMed] [Google Scholar]
- Ahmed N, Furth AJ 1992 Failure of common glycation assays to detect glycation by fructose. Clin Chem 38:1301–1303 [PubMed] [Google Scholar]
- Bell RC, Carlson JC, Storr KC, Herbert K, Sivak J 2000 High-fructose feeding of streptozotocin-diabetic rats is associated with increased cataract formation and increased oxidative stress in the kidney. Br J Nutr 84:575–582 [PubMed] [Google Scholar]
- 2002 Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care 25:202–212 [DOI] [PubMed] [Google Scholar]
- Banting F 1929 The history of insulin. Edinburgh Med J 36:1–18 [Google Scholar]
- Glushakova O, Kosugi T, Roncal C, Mu W, Heinig M, Cirillo P, Sanchez-Lozada LG, Johnson RJ, Nakagawa T 2008 Fructose induces the inflammatory molecule ICAM-1 in endothelial cells. J Am Soc Nephrol 19:1712–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosco JS, Greenleaf JE, Kaye RL, Averkin EG 1970 Reduction of serum uric acid in young men during physical training. Am J Cardiol 25:46–52 [DOI] [PubMed] [Google Scholar]
- Joslin EP, Dublin LI, Marks HH 1934 Studies in diabetes mellitus. II. Its incidence and the factors underlying its variations. Am J Med Sci 187:433–457 [Google Scholar]
- Brands MW, Garrity CA, Holman MG, Keen HL, Alonso-Galicia M, Hall JE 1994 High-fructose diet does not raise 24-hour mean arterial pressure in rats. Am J Hypertens 7:104–109 [DOI] [PubMed] [Google Scholar]
- D'Angelo G, Elmarakby AA, Pollock DM, Stepp DW 2005 Fructose feeding increases insulin resistance but not blood pressure in Sprague-Dawley rats. Hypertension 46:806–811 [DOI] [PubMed] [Google Scholar]
- Rebello T, Hodges RE, Smith JL 1983 Short-term effects of various sugars on antinatriuresis and blood pressure changes in normotensive young men. Am J Clin Nutr 38:84–94 [DOI] [PubMed] [Google Scholar]
- Visvanathan R, Chen R, Horowitz M, Chapman I 2004 Blood pressure responses in healthy older people to 50 g carbohydrate drinks with differing glycemic effects. Br J Nutr 92:335–340 [DOI] [PubMed] [Google Scholar]
- He FJ, Marrero NM, MacGregor GA 2008 Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension 51:629–634 [DOI] [PubMed] [Google Scholar]
- Harnack L, Stang J, Story M 1999 Soft drink consumption among US children and adolescents: nutritional consequences. J Am Diet Assoc 99:436–441 [DOI] [PubMed] [Google Scholar]
- Dennison BA, Rockwell HL, Baker SL 1997 Excess fruit juice consumption by preschool-aged children is associated with short stature and obesity. Pediatrics 99:15–22 [PubMed] [Google Scholar]
- Tordoff MG, Alleva AM 1990 Effect of drinking soda sweetened with aspartame or high-fructose corn syrup on food intake and body weight. Am J Clin Nutr 51:963–969 [DOI] [PubMed] [Google Scholar]
- Anderson JW, Story LJ, Zettwoch NC, Gustafson NJ, Jefferson BS 1989 Metabolic effects of fructose supplementation in diabetic individuals. Diabetes Care 12:337–344 [DOI] [PubMed] [Google Scholar]
- James J, Thomas P, Cavan D, Kerr D 2004 Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ 328:1237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritenbaugh C, Teufel-Shone NI, Aickin MG, Joe JR, Poirier S, Dillingham DC, Johnson D, Henning S, Cole SM, Cockerham D 2003 A lifestyle intervention improves plasma insulin levels among Native American high school youth. Prev Med 36:309–319 [DOI] [PubMed] [Google Scholar]
- Forshee RA, Storey ML, Allison DB, Glinsmann WH, Hein GL, Lineback DR, Miller SA, Nicklas TA, Weaver GA, White JS 2007 A critical examination of the evidence relating high fructose corn syrup and weight gain. Crit Rev Food Sci Nutr 47:561–582 [DOI] [PubMed] [Google Scholar]
- Prior IA, Rose BS, Harvey HP, Davidson F 1966 Hyperuricaemia, gout, and diabetic abnormality in Polynesian people. Lancet 1:333–338 [DOI] [PubMed] [Google Scholar]
- Beckett J 1964 Social change in Pukapuka. J Polynes Soc 73:411–430 [Google Scholar]
- Page LB, Damon A, Moellering Jr RC 1974 Antecedents of cardiovascular disease in six Solomon Islands societies. Circulation 49:1132–1146 [DOI] [PubMed] [Google Scholar]
- Jeremy R, Rhodes FA 1971 Studies of serum urate levels in New Guineans living in different environments. Med J Aust 1:897–899 [DOI] [PubMed] [Google Scholar]
- Bayard V, Chamorro F, Motta J, Hollenberg NK 2007 Does flavanol intake influence mortality from nitric oxide-dependent processes? Ischemic heart disease, stroke, diabetes mellitus, and cancer in Panama. Int J Med Sci 4:53–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzkaya N, Weissmann N, Harrison DG, Dikalov S 2005 Interactions of peroxynitrite with uric acid in the presence of ascorbate and thiols: implications for uncoupling endothelial nitric oxide synthase. Biochem Pharmacol 70:343–354 [DOI] [PubMed] [Google Scholar]
- George J, Carr E, Davies J, Belch JJ, Struthers A 2006 High-dose allopurinol improves endothelial function by profoundly reducing vascular oxidative stress and not by lowering uric acid. Circulation 114:2508–2516 [DOI] [PubMed] [Google Scholar]
- Waring WS, McKnight JA, Webb DJ, Maxwell SR 2007 Lowering serum urate does not improve endothelial function in patients with type 2 diabetes. Diabetologia 50:2572–2579 [DOI] [PubMed] [Google Scholar]
- Waring WS, Convery A, Mishra V, Shenkin A, Webb DJ, Maxwell SR 2003 Uric acid reduces exercise-induced oxidative stress in healthy adults. Clin Sci (Lond) 105:425–430 [DOI] [PubMed] [Google Scholar]
- Waring WS, McKnight JA, Webb DJ, Maxwell SR 2006 Uric acid restores endothelial function in patients with type 1 diabetes and regular smokers. Diabetes 55:3127–3132 [DOI] [PubMed] [Google Scholar]
- Wexler BC 1982 Allantoxanamide-induced myocardial necrosis in Sprague-Dawley vs spontaneously hypertensive rats. Proc Soc Exp Biol Med 170:476–485 [DOI] [PubMed] [Google Scholar]
- Wexler BC, Greenberg BP 1977 Effect of increased serum urate levels on virgin rats with no arteriosclerosis versus breeder rats with preexistent arteriosclerosis. Metabolism 26:1309–1320 [DOI] [PubMed] [Google Scholar]
- Johnson RJ, Feig DI, Nakagawa T, Sanchez-Lozada LG, Rodriguez- Iturbe B 2008 Pathogenesis of essential hypertension: historical paradigms and modern insights. J Hypertens 26:381–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner BM, Meyer TW, Hostetter TH 1982 Dietary protein intake and the progressive nature of kidney disease: the role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis in aging, renal ablation, and intrinsic renal disease. N Engl J Med 307:652–659 [DOI] [PubMed] [Google Scholar]
- Zammit VA, Waterman IJ, Topping D, McKay G 2001 Insulin stimulation of hepatic triacylglycerol secretion and the etiology of insulin resistance. J Nutr 131:2074–2077 [DOI] [PubMed] [Google Scholar]
- Unger RH 2003 Minireview: weapons of lean body mass destruction: the role of ectopic lipids in the metabolic syndrome. Endocrinology 144:5159–5165 [DOI] [PubMed] [Google Scholar]
- Doring A, Gieger C, Mehta D, Gohlke H, Prokisch H, Coassin S, Fischer G, Henke K, Klopp N, Kronenberg F, Paulweber B, Pfeufer A, Rosskopf D, Volzke H, Illig T, Meitinger T, Wichmann HE, Meisinger C 2008 SLC2A9 influences uric acid concentrations with pronounced sex-specific effects. Nat Genet 40:430–436 [DOI] [PubMed] [Google Scholar]
- Vitart V, Rudan I, Hayward C, Gray NK, Floyd J, Palmer CN, Knott SA, Kolcic I, Polasek O, Graessler J, Wilson JF, Marinaki A, Riches PL, Shu X, Janicijevic B, Smolej-Narancic N, Gorgoni B, Morgan J, Campbell S, Biloglav Z, Barac-Lauc L, Pericic M, Klaric IM, Zgaga L, Skaric-Juric T, Wild SH, Richardson WA, Hohenstein P, Kimber CH, Tenesa A, Donnelly LA, Fairbanks LD, Aringer M, McKeigue PM, Ralston SH, Morris AD, Rudan P, Hastie ND, Campbell H, Wright AF 2008 SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat Genet 40:437–442 [DOI] [PubMed] [Google Scholar]
- Kang DH, Han L, Ouyang X, Kahn AM, Kanellis J, Li P, Feng L, Nakagawa T, Watanabe S, Hosoyamada M, Endou H, Lipkowitz M, Abramson R, Mu W, Johnson RJ 2005 Uric acid causes vascular smooth muscle cell proliferation by entering cells via a functional urate transporter. Am J Nephrol 25:425–433 [DOI] [PubMed] [Google Scholar]
- Neel JV 1962 Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet 14:353–362 [PMC free article] [PubMed] [Google Scholar]
- Eaton SB, Konner M 1985 Paleolithic nutrition. A consideration of its nature and current implications. N Engl J Med 312:283–289 [DOI] [PubMed] [Google Scholar]
- Deer N 1949–50 The history of sugar. London: Chapman and Hall [Google Scholar]
- Reaven GM 1999 Insulin resistance, the key to survival: a rose by any other name. Diabetologia 42:384–385 [DOI] [PubMed] [Google Scholar]
- Kennedy ET 2005 The global face of nutrition: what can governments and industry do? J Nutr 135:913–915 [DOI] [PubMed] [Google Scholar]
- Glynn RJ, Campion EW, Silbert JE 1983 Trends in serum uric acid levels 1961–1980. Arthritis Rheum 26:87–93 [DOI] [PubMed] [Google Scholar]
- Arromdee E, Michet CJ, Crowson CS, O'Fallon WM, Gabriel SE 2002 Epidemiology of gout: is the incidence rising? J Rheumatol 29:2403–2406 [PubMed] [Google Scholar]
- Choi HK, Curhan G 2005 Gout: epidemiology and lifestyle choices. Curr Opin Rheumatol 17:341–345 [PubMed] [Google Scholar]
- 2008 Standards of medical care in diabetes–2008. Diabetes Care 31(Suppl 1):S12–S54 [DOI] [PubMed] [Google Scholar]
- Howard BV, Wylie-Rosett J 2002 Sugar and cardiovascular disease: a statement for healthcare professionals from the Committee on Nutrition of the Council on Nutrition, Physical Activity, and Metabolism of the American Heart Association. Circulation 106:523–527 [DOI] [PubMed] [Google Scholar]
- Jabara C, Valdes A 1993 World sugar policies and developing countries. In: The economics and politics of world sugar policies. Ann Arbor, MI: The University of Michigan Press [Google Scholar]
- 2003 Statistical Abstract of the US, no 214. Washington, DC: U.S. Census Bureau [Google Scholar]