Abstract
Background: Body mass index (BMI), waist circumference (WC), and the waist-stature ratio (WSR) are considered to be possible proxies for adiposity.
Objective: The objective was to investigate the relations between BMI, WC, WSR, and percentage body fat (measured by dual-energy X-ray absorptiometry) in adults in a large nationally representative US population sample from the National Health and Nutrition Examination Survey (NHANES).
Design: BMI, WC, and WSR were compared with percentage body fat in a sample of 12,901 adults.
Results: WC, WSR, and BMI were significantly more correlated with each other than with percentage body fat (P < 0.0001 for all sex-age groups). Percentage body fat tended to be significantly more correlated with WC than with BMI in men but significantly more correlated with BMI than with WC in women (P < 0.0001 except in the oldest age group). WSR tended to be slightly more correlated with percentage body fat than was WC. Percentile values of BMI, WC, and WSR are shown that correspond to percentiles of percentage body fat increments of 5 percentage points. More than 90% of the sample could be categorized to within one category of percentage body fat by each measure.
Conclusions: BMI, WC, and WSR perform similarly as indicators of body fatness and are more closely related to each other than with percentage body fat. These variables may be an inaccurate measure of percentage body fat for an individual, but they correspond fairly well overall with percentage body fat within sex-age groups and distinguish categories of percentage body fat.
INTRODUCTION
Epidemiologic studies commonly use body mass index (BMI), calculated from weight and height [weight (kg)/height2 (m)], as an indicator of overweight and obesity. US and international definitions of overweight and obesity for adults are based on BMI (1, 2). Weight and height can be measured relatively simply and accurately.
BMI is a measure of weight adjusted for height and does not measure body composition directly. Obesity refers to an excess of body fat. The underlying assumption of using BMI to define obesity is that at a given height, higher weight is associated with increased fatness (3). However, BMI is an imperfect measure of body fatness (4, 5), largely because it does not directly measure fat mass. Dual-energy X-ray absorptiometry (DXA) is one of the most accurate and precise methods available to directly measure total body fat and lean soft tissue mass, but it requires specialized DXA systems and X-ray exposure. Partly because of the limitations of BMI, the use of other simple measures to evaluate adiposity, such as waist circumference (WC) or the waist-stature ratio (WSR), has also been suggested (6–8).
The objective of this study was to investigate the relations between BMI, WC, WSR, and percentage body fat (from DXA) in adults in a large nationally representative US population sample from the National Health and Nutrition Examination Survey (NHANES). We compare these measures with each other. We also estimate the percentile values of BMI, WC, and WSR that approximately correspond to specified values of percentage body fat.
SUBJECTS AND METHODS
In NHANES, a representative cross-sectional sample of the US civilian, noninstitutionalized population was selected by using a complex, multistage probability design. Beginning in 1999, NHANES is a continuous survey that includes an interview in the household followed by an examination in a mobile examination center. Adolescents aged 12–19 y, persons aged ≥60 y, blacks, and Mexican Americans were oversampled to produce more precise estimates for these groups. Data from NHANES 1999–2004 were used. NHANES 1999–2004 underwent institutional review board approval and included written informed consent.
Age was calculated in years at the time of the interview and was grouped for analysis as 20–39, 40–59, 60–79, and ≥80 y. Race and ethnicity were self-reported, and, for the purposes of this study, race-ethnicity groups were classified as non-Hispanic white, non-Hispanic black, Mexican American, and “other” race-ethnicity. Weight, height (stature), and WC were measured by using standardized techniques and equipment (9). WC was measured just above the iliac crest. WSR was calculated as WC (cm)/height (m).
Whole-body percentage body fat was calculated as total body fat mass divided by total mass (from DXA) × 100. Whole-body DXA scans were acquired by using a Hologic QDR 4500A fan-beam densitometer (Hologic Inc, Bedford, MA) (9). The scan for each survey participant was reviewed and analyzed by the University of California, San Francisco (UCSF), Department of Radiology, using standard radiologic techniques and study-specific protocols developed for NHANES. Hologic Discovery software, version 12.1, was used to analyze the scans. Beyond planned exclusions, a number of participants were missing valid DXA data for a variety of reasons. The percentage of participants with valid data decreased with increasing age, primarily because of an increase in implants such as pacemakers, stents, and hip replacements. These artifacts can affect the accuracy of the DXA results. Metal appears as dense bone, and soft tissue implants such as breast augmentation appear as additional lean soft tissue mass. In addition, the proportion of participants with valid data was lower at higher BMI levels, in part because of truncal adiposity. The DXA scanner cannot penetrate much thicker than 15 cm, after which the accuracy of segmenting the bone is limited.
Our analyses used the 5 NHANES 1999–2004 DXA Multiple Imputation Data Files as released by the National Center for Health Statistics (10). In part because data were not missing completely at random, missing DXA values were imputed in these public-use data sets. Because missing DXA data were related to age, BMI, weight, and height and possibly to other characteristics, participants with missing data could no be treated as a random subset of the original sample. Otherwise, analytic results could be biased toward participants with the least amount of missing data. Multiple imputation (11) was carried out to allow analyses to reflect the additional variability due to the use of imputed values for the missing data. With multiple imputation, M (in this case, M = 5) versions of the imputed values are created randomly and independently under the imputation model, resulting in M completed data sets. Each data set is analyzed using the analysis that would be used with complete data, and the M sets of results are combined, with the variability across the M analyses measuring the additional variability due to missing data.
The characteristics of the missing data and the imputation process for the NHANES 1999–2004 DXA Multiple Imputation Data Files are both described in detail in the technical documentation (12). Briefly, however, a sequential regression multivariate imputation procedure (13) was implemented separately within 10 age-by-sex groups. A large number of predictors were used, including the non-DXA variables analyzed in this article as well as body measurements, indicators of health, variables on diet and use of medications, blood test results, variables related to the design of the NHANES sample, and other demographic, socioeconomic, and geographic variables. In addition, the correlations between DXA measurements for different parts of the body were taken into account. Thus, when measurements were observed for some parts but not for others, the observed measurements were used to predict the missing values.
The information used in the imputation process helps to adjust subsequent analyses for the fact that the persons with missing DXA data are not a completely random subset of the original NHANES sample. The multiple imputations help to reflect uncertainty in relations between the missing DXA values and other variables that are analyzed with them.
Analytic sample
This report uses data for participants aged ≥20 y. There were 12,936 nonpregnant participants in this age range who had complete weight and height data. Of these participants, 3005 were missing some or all DXA data and 2970 had some or all imputed DXA data for a final analytic sample size of 12,901 nonpregnant adult participants with both BMI data and percentage body fat data. Of these, 345 were missing data on WC, so the analyses based on WC used data on 12,556 participants, of whom 2678 had some or all imputed DXA data.
Statistical methods
We calculated sample-weighted Pearson correlation coefficients between each pair of the variables percentage body fat, BMI, WC, and WSR within each age-sex group. For purposes of statistically testing differences between correlation coefficients, these correlations were transformed by using Fisher's z transformation. For each imputation data set, the within-imputation component of variance for a difference between 2 transformed correlation coefficients was computed by using a (stratified) jackknife method leaving out one primary sample unit (PSU) at a time (14). These variances were combined with a between-imputation component of variance for the differences in the transformed correlations over the 5 imputation data sets (11); t tests were used to test for equality between 2 transformed correlations, and the df was determined according to Barnard and Rubin (15). Forty-seven df (number of PSUs − the number of sampling strata) was used as the complete-data df in this determination.
Standard BMI categories are well established and widely used. However, categories of percentage fat are not well standardized. According to a World Health Organization expert committee, “there is no agreement about cut-off points for the percentage of body fat that constitutes obesity” (16; p 420). Thus, we calculated the weighted prevalence, averaged over the multiply imputed data sets, of arbitrary categories of percentage body fat within age and sex groups using arbitrary increments of 5 percentage points. Because the distribution of percentage body fat differed considerably between men and women, the ranges covered were different for men than for women. For descriptive purposes, we estimated the age and sex-specific percentile values of BMI, WC, and WSR that would correspond to the percentage fat categories in the sense that they identify the same percentiles and proportion of the distribution and thus produce approximately the same prevalence estimates as the percentage fat categories. We used these levels to create categories of BMI, WC, and WSR that were prevalence-matched to the percentage fat categories. The overall classification by age- and sex-specific categories was evaluated by calculating the percentage of the population that fell into the corresponding category by any 2 measures (exact agreement) and using separate logistic regression to model the dependence of exact agreement between each pair of measures on sex, age group, and race-ethnicity group. We also calculated the percentage that agreed to within one category. The BMI, WC, and WSR categories were determined empirically to match the percentage fat categories. This empirical determination was not taken into account in the estimation of the SEs in our analysis involving the BMI, WC, and WSR categories; therefore, these SEs were most likely slightly underestimated.
Analyses were conducted with PC-SAS (version 9.1; SAS Institute, Cary, NC) and SUDAAN (version 9.03; Research Triangle Institute, Research Triangle Park, NC). All statistical analyses used sample weights and accounted for the sample design and the multiple imputations. Estimates were averaged over the 5 sets of imputations. Statistical significance was determined based on a P value <0.05 with Bonferroni adjustment.
RESULTS
Basic descriptive information about the analytic sample is shown in Table 1. Differences in mean values between men and women were tested by using a 2-sample t test for complex survey data (14). Pearson correlations between percentage fat, BMI, WC, and WSR are shown in Table 2 by sex and age group. Correlations by race-ethnicity group within sex and age groups were similar to those seen overall (data not shown). All correlations were significantly greater than zero (P < 0.0001). For men, the correlations between percentage fat and BMI ranged from 0.789 (20–39 y of age) to 0.716 (≥80 y of age). The corresponding values for women were 0.839 and 0.724. For comparisons between pairs of correlations, statistical significance was based on a P value of 0.00045, which was equivalent to a P value of < 0.05 after Bonferroni correction. For men, percentage fat was significantly more highly correlated with WC or with WSR than with BMI (P < 0.00001, except in the oldest age group in which the differences were not statistically significant). For women, percentage fat was significantly more highly correlated with BMI than with WC (P < 0.00001), except in the oldest age group in which the difference was not statistically significant (P = 0.037). For women, percentage fat tended to be more highly correlated with BMI than with WSR (P < 0.05), but the difference was statistically significant only for women aged 40–59 y (P < 0.00001). WSR tended to be slightly more correlated with percentage fat than was WC alone; the differences were statistically significant only in the youngest age group for both men (P < 0.0001) and women (P < 0.0001). For both men and women and within each age group, WC and BMI were significantly more highly correlated with each other than either was with percentage fat (P < 0.00001 for all sex-age groups). Similarly, WSR and BMI were significantly more highly correlated with each other than either was with percentage fat (P < 0.00001 for all sex-age groups).
TABLE 1.
Descriptive information (weighted estimates) for the analytic sample
| Men | Women | |
| Unweighted sample size | 6477 | 6424 |
| Weighted percentage (%) | 48.9 | 51.1 |
| Age group (% of total) | ||
| 20–39 y | 41.2 | 36.4 |
| 40–59 y | 38.9 | 38.9 |
| 60–79 y | 17.1 | 20.0 |
| ≥80 y | 2.8 | 4.7 |
| Race-ethnicity group (% of total) | ||
| Non-Hispanic white | 72.0 | 71.6 |
| Non-Hispanic black | 10.0 | 11.5 |
| Mexican American | 8.1 | 6.4 |
| Other | 9.9 | 10.6 |
| Percentage body fat (%) | 28.1 ± 0.101 | 39.9 ± 0.162 |
| BMI (kg/m2) | 27.9 ± 0.10 | 28.2 ± 0.142 |
| Waist circumference (cm) | 99.5 ± 0.25 | 93.1 ± 0.372 |
| Waist-stature ratio | 56.5 ± 0.14 | 57.5 ± 0.232 |
Mean ± SE (all such values).
Significantly different from men, P < 0.05 (2-sample t test for complex survey data).
TABLE 2.
Pearson correlations of percentage body fat, BMI, waist circumference (WC), and waist-stature ratio (WSR) by sex and age group1
| Sex and age group | Percentage body fat with BMI | Percentage body fat with WC | Percentage body fat with WSR | BMI with WC | BMI with WSR | WC with WSR |
| Men | ||||||
| 20–39 y | 0.789a | 0.855b | 0.870c | 0.941d | 0.944d | 0.961e |
| 40–59 y | 0.755a | 0.819b | 0.823b | 0.921c | 0.933c | 0.947c |
| 60–79 y | 0.738a | 0.785b | 0.801b | 0.927c | 0.926c | 0.942d |
| ≥80 y | 0.716a | 0.736a | 0.756a | 0.904b,c | 0.903b | 0.933c |
| Women | ||||||
| 20–39 y | 0.839a | 0.804b | 0.819a | 0.928c | 0.936d | 0.973e |
| 40–59 y | 0.798a | 0.768b | 0.780a,b | 0.912c | 0.922c | 0.969d |
| 60–79 y | 0.763a | 0.697b | 0.700b | 0.882c | 0.886c | 0.959d |
| ≥80 y | 0.724a | 0.650a | 0.657a | 0.852b | 0.856b | 0.955c |
Within each sex-age group, values with different superscript letters are significantly different, P = 0.00045 (equivalent to P < 0.05 after Bonferroni correction). Comparisons were not made between sex-age groups. For the statistical testing of differences between correlation coefficients, correlations were transformed by using Fisher's z transformation, and t tests were used to test for equality between 2 transformed correlations.
The distribution of percentage fat categories and the corresponding values for BMI, WC, and WSR are shown by age group in Table 3 for men and in Table 4 for women. We identified cutoffs for BMI, WC, and WSR that corresponded to the same percentiles of the distribution as did the percentage fat values and thus were matched to percentage fat categories in the sense that these cutoffs would categorize the same proportion of people within each BMI or waist or WSR category as did the corresponding percentage fat category, although not necessarily the same individuals. For example, 1.9% of men aged 20–39 y had percentage fat values ≥40; the corresponding BMI cutoff of 43 shown in Table 3 identified the highest 1.8% of BMI values, a WC cutoff of 136 cm or more identified the highest 2.0% of WC values, and a WSR cutoff of 75 identified the highest 1.8% of WSR values. Although the prevalence estimates could not always be matched exactly, the cutoffs shown in Tables 3 and 4 are the closest rounded values, and generally the prevalences matched within 1 percentage point or less. These values suggest that, for men in the age group 20–39 y, cutoffs of a BMI of 25, a WC of 90 cm, or a WSR of 51 represent approximately the same percentile of their respective distributions as a percentage fat cutoff of 25%. However, in the oldest age group, a percentage fat cutoff of 25 was equivalent to the same percentile as a cutoff of a BMI of 22 or a WC of 89 cm. At higher values of percentage fat, the range of BMI values corresponding to a 5-percentage-point increase in body fat was wider than at lower values of percentage fat. For example, for men aged 20–39 y, the range of BMIs corresponding to a range in percentage body fat from 20 to <25% was 23 to <25, but the range of BMI values corresponding to a range in percentage body fat from 35% to 40% was wider, 35 to <43. Similar results were observed for WC and WSR as well.
TABLE 3.
Weighted prevalences of specified percentage body fat categories by age group and corresponding percentiles of BMI, waist circumference (WC), and waist-stature ratio (WSR): men
| Percentage body fat |
|||||||
| <15 | 15 to <20 | 20 to <25 | 25 to <30 | 30 to <35 | 35 to <40 | ≥40 | |
| Prevalence | |||||||
| 20–39 y | 3.8 ± 0.41 | 15.7 ± 0.8 | 23.1 ± 1.0 | 30.3 ± 1.1 | 17.9 ± 1.0 | 7.4 ± 0.7 | 1.9 ± 0.3 |
| 40–59 y | 0.4 ± 0.1 | 5.8 ± 0.7 | 16.9 ± 1.0 | 37.4 ± 1.3 | 27.6 ± 1.4 | 9.9 ± 1.0 | 2.0 ± 0.4 |
| 60–79 y | 0.3 ± 0.1 | 1.4 ± 0.3 | 10.8 ± 0.8 | 29.9 ± 1.4 | 35.3 ± 1.3 | 17.9 ± 1.3 | 4.3 ± 0.6 |
| ≥80 y | 0.0 ± 0.0 | 2.4 ± 0.8 | 9.7 ± 1.3 | 31.4 ± 2.0 | 35.6 ± 2.4 | 17.7 ± 2.0 | 3.2 ± 1.0 |
| Corresponding BMI percentiles | |||||||
| 20–39 y | <19 | 19 to <23 | 23 to <25 | 25 to <30 | 30 to <35 | 35 to <43 | ≥43 |
| 40–59 y | <18 | 18 to <22 | 22 to <25 | 25 to <29 | 29 to <34 | 34 to <43 | ≥43 |
| 60–79 y | <18 | 18 to <20 | 20 to <23 | 23 to <27 | 27 to <32 | 32 to <38 | ≥38 |
| ≥80 y | <19 | 19 to <22 | 22 to <25 | 25 to <29 | 29 to <34 | ≥34 | |
| Corresponding WC percentiles | |||||||
| 20–39 y | <73 | 73 to <82 | 82 to <90 | 90 to <102 | 102 to <114 | 114 to <136 | ≥136 |
| 40–59 y | <71 | 71 to <83 | 83 to <92 | 92 to <104 | 104 to <117 | 117 to <136 | ≥136 |
| 60–79 y | <74 | 74 to <80 | 80 to <91 | 91 to <102 | 102 to <114 | 114 to <129 | ≥129 |
| ≥80 y | — | <79 | 79 to <89 | 89 to < 98 | 98 to <108 | 108 to <123 | ≥123 |
| Corresponding WSR percentiles | |||||||
| 20–39 y | <42 | 42 to <47 | 47 to <51 | 51 to <58 | 58 to <65 | 65 to <75 | ≥75 |
| 40–59 y | <41 | 41 to <47 | 47 to <52 | 52 to <59 | 59 to <66 | 66 to <77 | ≥77 |
| 60–79 y | <43 | 43 to <47 | 47 to <52 | 52 to <58 | 58 to <65 | 65 to <74 | ≥74 |
| ≥80 y | — | <46 | 46 to <52 | 52 to <58 | 58 to <64 | 64 to <71 | ≥71 |
Mean ± SE (all such values).
TABLE 4.
Weighted prevalences of specified percentage body fat categories by age group and corresponding percentiles of BMI, waist circumference (WC), and waist-stature ratio (WSR): women
| Percentage body fat |
|||||||
| <25 | 25 to <30 | 30 to <35 | 35 to <40 | 40 to <45 | 45 to <50 | ≥50 | |
| Prevalence | |||||||
| 20–39 y | 4.2 ± 0.61 | 10.7 ± 1.1 | 20.6 ± 1.1 | 24.4 ± 1.3 | 22.6 ± 1.1 | 12.5 ± 0.9 | 4.9 ± 0.6 |
| 40–59 y | 1.6 ± 0.4 | 4.9 ± 0.7 | 12.6 ± 1.0 | 24.3 ± 1.1 | 30.6 ± 1.2 | 19.5 ± 1.1 | 6.6 ± 0.7 |
| 60–79 y | 0.4 ± 0.2 | 1.4 ± 0.3 | 7.6 ± 0.8 | 19.8 ± 1.3 | 36.6 ± 1.4 | 26.8 ± 1.2 | 7.3 ± 0.7 |
| ≥80 y | 1.8 ± 1.1 | 3.2 ± 1.0 | 13.7 ± 1.6 | 20.9 ± 2.1 | 37.8 ± 2.6 | 19.5 ± 2.1 | 3.1 ± 1.1 |
| Corresponding BMI percentiles | |||||||
| 20–39 y | <19 | 19 to <21 | 21 to <23 | 23 to <27 | 27 to <34 | 34 to <42 | ≥42 |
| 40–59 y | <18 | 18 to <20 | 20 to <23 | 23 to <26 | 26 to <33 | 33 to <41 | ≥41 |
| 60–79 y | <17 | 17 to <19 | 19 to <22 | 22 to <25 | 25 to <30 | 30 to <38 | ≥38 |
| ≥80 y | <18 | 18 to <19 | 19 to <22 | 22 to <24 | 24 to <29 | 29 to <38 | ≥38 |
| Corresponding WC percentiles | |||||||
| 20–39 y | <69 | 69 to <74 | 74 to <81 | 81 to <90 | 90 to <104 | 104 to <120 | ≥120 |
| 40–59 y | <69 | 69 to <73 | 73 to <80 | 80 to <90 | 90 to <104 | 104 to <121 | ≥121 |
| 60–79 y | <66 | 66 to <72 | 72 to <80 | 80 to <89 | 89 to <102 | 102 to <119 | ≥119 |
| ≥80 y | <68 | 68 to <72 | 72 to <81 | 81 to <89 | 89 to <103 | 103 to <116 | ≥116 |
| Corresponding WSR percentiles | |||||||
| 20–39 y | <42 | 42 to <45 | 45 to <49 | 49 to <55 | 55 to <64 | 64 to <74 | ≥74 |
| 40–59 y | <42 | 42 to <45 | 45 to <49 | 49 to <56 | 56 to <64 | 64 to <74 | ≥74 |
| 60–79 y | <42 | 42 to <45 | 45 to <50 | 50 to <56 | 56 to <64 | 64 to <74 | ≥74 |
| ≥80 y | <43 | 43 to <46 | 46 to <52 | 52 to <58 | 58 to <66 | 66 to <75 | ≥75 |
Mean ± SE (all such values).
We applied the age- and sex-specific cutoffs shown in Tables 3 and 4 to create BMI, WC, and WSR categories corresponding to the prevalence of the percentage fat categories shown in Tables 3 and 4. Thus, all 4 sets of categories (percentage fat categories, BMI categories, WC categories, and WSR categories) represent similar estimated prevalences within each age-sex group. We then assessed the agreement between percentage fat, BMI, WC, and WSR categories by calculating the percentage of the population that fell into the corresponding categories by 2 different measures and also the percentage that agreed to within one category by 2 different measures. For example, a woman in the age range 20–39 y with an estimated percentage body fat of 35% and a BMI of 23 would fall into corresponding categories by these 2 measures, as shown in Table 4. However, if the BMI was 22, the woman would fall into a lower BMI category and thus be considered to fall into different categories by these 2 measures, but to agree within one category. The results for exact agreement and agreement to within one category are presented in Table 5.
TABLE 5.
Percentage exact agreement between percentage fat categories shown in Tables 3 (men) and 4 (women) and BMI, waist circumference (WC), and waist-stature ratio (WSR) categories based on the percentile cutoffs shown in Tables 3 and 41
| Percentage body fat with BMI | Percentage body fat with WC | Percentage body fat with WSR | BMI with WC | BMI with WSR | WC with WSR | |
| Exact | ||||||
| Men | 46 ± 0.7a | 51 ± 0.8b | 53 ± 0.8b | 65 ± 0.8c | 65 ± 0.8c | 71 ± 0.8d |
| Women | 49 ± 0.9a | 42 ± 0.9b | 43 ± 0.8b | 59 ± 0.8c | 60 ± 0.8c | 73 ± 0.9d |
| Within one category | ||||||
| Men | 93 ± 0.4a | 97 ± 0.2b | 97 ± 0.3c | 99 ± 0.2d | 99 ± 0.2d | 100 ± 0.1d |
| Women | 94 ± 0.5a | 91 ± 0.6b | 92 ± 0.6c | 98 ± 0.2d | 98 ± 0.2d | 100 ± 0.0e |
All values are means ± SEs. Within each row, values with different superscript letters are significantly different, P = 0.001 (equivalent to P < 0.05 after Bonferroni correction); t tests were used to test for equality.
Overall, 46% of men and 49% of women were in the same category by percentage fat and by BMI. Results for the agreement of WC categories with percentage body fat categories were similar to those for the agreement of BMI categories with percentage body fat categories, with estimates slightly higher for men (51% agreement of WC categories with percentage body fat categories compared with 46% agreement of BMI categories with percentage body fat categories; P < 0.00002 for the difference) and slightly lower for women (42% agreement of WC categories with percentage body fat categories compared with 49% agreement of BMI categories with percentage body fat categories; P < 0.00001 for the difference). Estimates of agreement for WSR with percentage body fat were similar to those for WC and differences between estimates of agreement with percentage body fat for WC and estimates of agreement with percentage body fat for WSR were not statistically significant (P = 0.23 for the difference for men and P = 0.43 for women) As was also seen for the correlation coefficients, BMI categories and WC categories or WSR categories showed better agreement with each other than either did with percentage fat categories (P < 0.0001). For men, the percentage who agreed in classification to within one category ranged from 93% to 100% across all measures. For women, the range was slightly lower, from 91% to 100%. Approximately 33% of the respondents [34.7% of men (95% CI: 33.3, 36.0) and 30.0% of women (95% CI: 28.5, 31.5)] fell into the same category by 3 measures: percentage fat, BMI, and WSR.
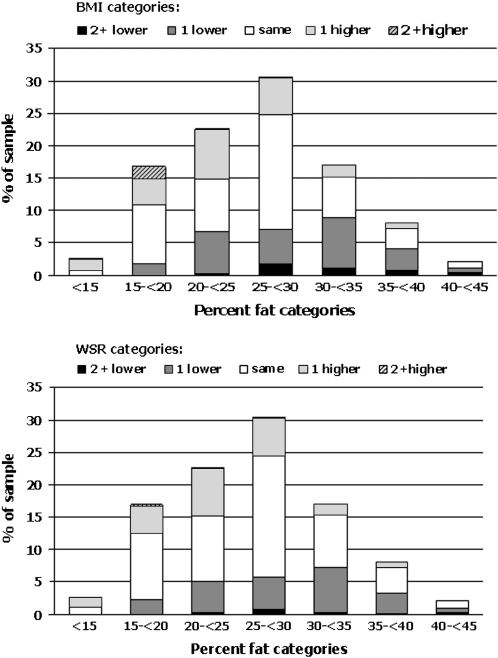
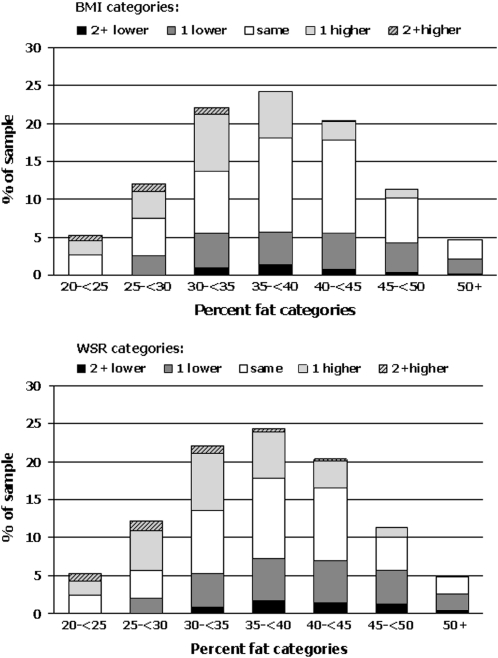
As examples, more detailed information on the distribution of agreement, based on the cutoffs in Tables 3 and 4, is shown graphically for non-Hispanic white men aged 20–39 y (Figure 1) and for non-Hispanic white women aged 20–39 y (Figure 2). These figures show the proportion of the sample in the indicated percentage fat categories; within each percentage fat category, they show the proportion of the total sample that are in the same BMI category, or one category lower or higher, or 2 or more categories lower or higher. Thus, for example, in Figure 1, 30.6% of the men in this subgroup fell into the percentage fat category of 25 to <30%. Slightly more than 50% of these men (17.6% of the men in this subgroup) fell into the corresponding BMI category, 5.7% fell into the next higher BMI category, 0.1% fell into ≥2 higher BMI categories, 5.3% fell into the next lower BMI category, and 1.8% fell into ≥2 BMI categories lower. The corresponding values for WSR categories were 18.9% (same), 5.9% (one higher), 0.1% (≥2 higher), 4.9% (one lower), and 0.8% (≥2 lower).
FIGURE 1.
Agreement of BMI and waist-stature (WSR) categories shown in Table 3 with percentage fat categories for non-Hispanic white men aged 20–39 y.
FIGURE 2.
Agreement of BMI and waist-stature (WSR) categories shown in Table 4 with percentage fat categories for non-Hispanic white women aged 20–39 y.
In sex-specific logistic models adjusted for age group and race-ethnic group, both the agreement of BMI categories with percentage fat (P = 0.0004 for men, P = 0.0623 for women) and the agreement of WC categories with percentage fat (P = 0.0016 for men, P = 0.0518 for women) tended to vary significantly by race-ethnicity categories. For both men and women, the agreement of BMI categories with percentage fat categories was significantly lower for non-Hispanic black men (odds ratio: 0.76; 95% CI: 0.65, 0.90) and women (odds ratio: 0.81; 95% CI: 0.70, 0.94) than for non-Hispanic whites. For WC categories, the agreement also tended to be lower for non-Hispanic blacks than for non-Hispanic whites, although this was statistically significant only for women (odds ratio: 0.84; 95% CI: 0.74, 0.96) and not for men (odds ratio: 0.88; 95% CI: 0.75, 1.02). For the WSR categories, there were no significant differences between race-ethnicity groups for men (odds ratio: 1.01; 95% CI: 0.86, 1.19) or for women (odds ratio: 0.92; 95% CI: 0.77, 1.11). Agreement for Mexican Americans did not differ significantly from non-Hispanic whites in any analyses. Because of the tendency for agreement to be significantly lower for non-Hispanic blacks than for other race-ethnicity groups, specific cutoffs for BMI and WC for non-Hispanic black men and women are shown in Table 6 and Table 7, respectively. For example, the data in this table show that among non-Hispanic black men aged 20–39 y, a BMI of 27 to <32 corresponds more closely to the percentage fat category of 25 to <30% than does the overall BMI range of 25 to <30 shown in Table 3, which suggests that at a given BMI, percentage fat is somewhat lower in non-Hispanic blacks than in the full sample or in non-Hispanic whites.
TABLE 6.
Percentile cutoffs for BMI and waist circumference (WC) corresponding to specified percentage body fat categories for non-Hispanic black men by age group
| Percentage body fat |
|||||||
| <15 | 15 to <20 | 20 to <25 | 25 to <30 | 30 to <35 | 35 to <40 | ≥40 | |
| Corresponding BMI percentiles | |||||||
| 20–39 y | <21 | 21 to <24 | 24 to <27 | 27 to <32 | 32 to <40 | 40 to <50 | ≥50 |
| 40–59 y | <19 | 19 to <23 | 23 to <26 | 26 to <31 | 31 to <37 | 37 to <48 | ≥48 |
| 60–79 y | <18 | 18 to <21 | 21 to <24 | 24 to <29 | 29 to <34 | 34 to <39 | ≥39 |
| ≥80 y | — | —1 | <23 | 23 to <26 | 26 to <29 | 29 to <36 | ≥36 |
| Corresponding WC percentiles | |||||||
| 20–39 y | <75 | 75 to <83 | 83 to <91 | 91 to <103 | 103 to <119 | 119 to <140 | ≥140 |
| 40–59 y | <73 | 73 to <84 | 84 to <93 | 93 to <107 | 107 to <120 | 120 to <148 | ≥148 |
| 60–79 y | <74 | 74 to <82 | 82 to <93 | 93 to <103 | 103 to <117 | 117 to <131 | ≥131 |
| ≥80 y | — | —1 | <89 | 89 to <100 | 100 to <108 | 108 to <127 | ≥127 |
Insufficient data.
TABLE 7.
Percentile cutoffs for BMI and waist circumference (WC) corresponding to specified percentage body fat categories for non-Hispanic black women by age group
| Percentage body fat |
|||||||
| <25 | 25 to <30 | 30 to <35 | 35 to <40 | 40 to <45 | 45 to <50 | ≥50 | |
| Corresponding BMI percentiles | |||||||
| 20–39 y | <19 | 19 to <22 | 22 to <25 | 25 to <30 | 30 to <36 | 36 to <46 | ≥46 |
| 40–59 y | <19 | 19 to <21 | 21 to <24 | 24 to <28 | 28 to <35 | 35 to <43 | ≥43 |
| 60–79 y | <20 | 20 to <22 | 22 to <24 | 24 to <28 | 28 to <34 | 34 to <41 | ≥41 |
| ≥80 y | —1 | <21 | 21 to <23 | 23 to <26 | 26 to <33 | 33 to <40 | ≥40 |
| Corresponding WC percentiles | |||||||
| 20–39 y | <67 | 67 to <76 | 76 to <84 | 84 to <93 | 93 to <108 | 108 to <127 | ≥127 |
| 40–59 y | <67 | 67 to <76 | 76 to <85 | 85 to <93 | 93 to <107 | 107 to <121 | ≥121 |
| 60–79 y | <74 | 74 to <79 | 79 to <84 | 84 to <96 | 96 to <107 | 107 to <121 | ≥121 |
| ≥80 y | —1 | <75 | 75 to <82 | 82 to <92 | 92 to <104 | 104 to <122 | ≥122 |
Insufficient data.
DISCUSSION
In this large population-based, nationally representative sample, WC, WSR, BMI, and DXA-derived percentage body fat were all highly correlated with each other within sex-age groups. BMI, WC, and WSR all performed very similarly as indirect measures of body fat, and they were more closely related to each other than with percentage body fat. Percentage fat tended to be slightly but significantly more correlated with WC than with BMI among men, but significantly more correlated with BMI than with WC among women; the differences were slight. Generally, similar correlations of BMI with percentage body fat have been found in other studies (17–22). Others (19, 23) have also found that WC is slightly more correlated with fat than was BMI among men but slightly less so among women.
We estimated values of BMI, WC, and WSR that identified the same percentiles of the distribution as did arbitrary percentage body fat categories and thus identified the same proportion of the population. Approximately 40–50% of respondents were classified into equivalent categories of WC, WSR, or BMI, and >90% were classified similarly to within one category. The purpose of presenting these values is to describe the distributions of these variables and not to propose that these cutoff values be used for categorization. Further research is needed to show how best to use BMI, WC, or WSR to classify individuals according to percentage fat. However, the relatively good agreement between these variables suggests that BMI, WC, and WSR may serve well in classifying individuals into broad categories corresponding to percentage fat categories. Agreement in classification by WC or WSR relative to BMI was higher, in the range of 60–70%. In >90% of cases, and often in 99% or 100% of cases, classifications differed by only one category.
As shown previously (17, 18), and as would be expected from considerations of body composition (24, 25), percentage fat does not increase linearly with body weight. Thus, a given difference in BMI, WC, or WSR at low levels reflects a larger change in percentage fat than does the same difference in BMI, WC, or WSR at high levels.
BMI is widely used in epidemiologic studies to assess the risks of health outcomes associated with different levels of body weight. Some studies have suggested that WC, either singly or in combination with BMI, may have a stronger relation to some health outcomes than BMI alone (6, 26–28). In the NHANES data, both BMI and WC had a similar relation to percentage body fat and both were more highly correlated with each other than with percentage body fat. It is not clear whether percentage body fat is the most relevant variable in terms of relation of body composition with health outcomes; some other aspect of body composition such as lean mass or visceral adipose tissue might be equally or more important. Bosy-Westphal et al (23) found that, for practical purposes at the population level, BMI, WC, and percentage fat all predicted metabolic risk factors equally well. Similar findings have been reported by Dalton et al (29). Vazquez et al (30) found that BMI and WC performed equally well in predicting incident diabetes. Shen et al (31) found that WC was more highly related to health risk factors than was percentage body fat. Although WC has been suggested to be a better measure of visceral adipose tissue (32), some evidence suggests that it may also primarily be related to total body fat rather than to visceral adiposity per se (33). Different health outcomes may have different relations to body composition and to these various highly correlated measures, so that the results may vary depending on the outcomes examined and on other characteristics of the study samples.
WSR has been suggested to be a better indicator of adiposity than WC alone (7, 8). In the NHANES data, WSR tended to be a slightly better indicator of percentage fat than was WC alone, although the differences were not large. The cutoff value of 50 for WSR, suggested by Ashwell and Hsieh (8), is close to the percentile that corresponds to percentage of 25% for men or of 35% for women; differences could arise in part from measuring WC at a different anatomic location.
Other approaches have been taken to finding values of percentage fat comparable with BMI categories from samples with both weight and height measures and body fat measures. Norgan and Ferro-Luzzi (34) used prediction equations to predict percentage body fat (estimated from underwater weighing) at different BMI levels for men and found cutoff values of 15%, 22%, 29%, and 42% corresponding to BMI values of 20, 25, 30, and 40—roughly similar to our estimates. Several studies have used receiver operating characteristic curves to assess different anthropometric measures relative to percentage body fat (5, 17, 35). That approach, however, requires specifying a fixed percentage body fat as the outcome; at present, there are no standard or widely accepted categories of percentage body fat, as evidenced in part by the fact that each of these articles used different cutoffs.
The relation of BMI to percentage fat varies by sex, age, and race-ethnicity group (22, 36), so that the percentage fat that a given BMI represents will tend to vary across sex, age, and race-ethnicity. Considerable discussion has addressed the public health and policy issues of using different BMI cutoffs for different ethnicity groups that have different relations of BMI to body fat and to health risks (36–45). Our findings confirm that the same BMI categories are associated with lower levels of body fat in non-Hispanic blacks than in other race-ethnic groups (36, 46, 47) and indicate that this is also the case for WC. Other research has also suggested that the health risks associated with a given BMI level may be lower for blacks than for whites (44, 46, 48–51). In general, the selection of BMI cutoffs is related to health outcomes, but the method used to establish exact cutoffs has been called “largely arbitrary” (16). The BMI, WC, or WSR cutoffs that identify similar levels of body fat across age, sex, and ethnicity groups may differ from the BMI, WC, or WSR cutoffs that identify similar levels of health risk across age, sex, and ethnicity groups.
Our study had some limitations. Percentage fat was based only on DXA measurements, not on more complex body-composition models such as a 4-compartment model (52–56). WC was measured just above the iliac crest, and this may limit the comparability of our results with WC measured in other anatomic locations (57). Multiple imputation methods were used to adjust for missing DXA data. As with any method that adjusts analyses for missing data, the validity of results depends on the validity of the assumptions about the missing data.
The results presented herein show the values of BMI, WC, and WSR that will divide the population into categories prevalence-matched to those identified by the percentage body fat categories. These are presented for descriptive purposes and not as a proposed approach to use in categorizing these variables. However, they may assist in showing the distributions of BMI, WC, and WSR relative to the distribution of percentage fat. These values vary by age, sex, and to some extent by race-ethnicity group. In general, BMI, WC, WSR, and percentage body fat are all closely related, and, as percentage body fat increases, BMI, WC, and WSR all increase. BMI and WC or WSR showed somewhat higher agreement with each other than either did with percentage fat. For men, WC and WSR agreed slightly better than did BMI with categories of percentage fat. For women, however, BMI agreed with categories of percentage fat better than did WC or WSR. Although an estimate of body fat based on BMI, WC, or WSR for an individual may be inaccurate, overall BMI, WC, and WSR values correspond fairly well within groups and distinguish categories of body fatness.
Acknowledgments
The authors' responsibilities were as follows—KMF: study design and writing of the first draft of the manuscript; JAS, LGB, and ACL: acquisition and interpretation of data from the DXA scans; NS, LGB, ACL, and KMF: multiple imputation of DXA data; and BIG and NS: statistical analysis. All authors: analysis and interpretation of the data and critical revision of the manuscript for important intellectual content. None of the authors had a personal or financial conflict of interest.
REFERENCES
- 1.Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Am J Clin Nutr 1998;68:899–917 [DOI] [PubMed] [Google Scholar]
- 2.WHO Obesity: preventing and managing the global epidemic: report of a WHO consultation. World Health Organ Tech Rep Ser 2000;894:1–253 [PubMed] [Google Scholar]
- 3.Benn RT. Some mathematical properties of weight-for-height indices used as measures of adiposity. Br J Prev Soc Med 1971;25:42–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roche AF, Sievogel RM, Chumlea WC, Webb P. Grading body fatness from limited anthropometric data. Am J Clin Nutr 1981;34:2831–8 [DOI] [PubMed] [Google Scholar]
- 5.Wellens RI, Roche AF, Khamis HJ, Jackson AS, Pollock ML, Siervogel RM. Relationships between the body mass index and body composition. Obes Res 1996;4:35–44 [DOI] [PubMed] [Google Scholar]
- 6.Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr 2004;79:379–84 [DOI] [PubMed] [Google Scholar]
- 7.Ashwell M, Lejeune S, McPherson K. Ratio of waist circumference to height may be better indicator of need for weight management. BMJ 1996;312:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr 2005;56:303–7 [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics National Health and Nutrition Examination Survey: body composition procedures manual. Available from: http://www.cdc.gov/nchs/data/nhanes/bc.pdf (cited 8 October 2008)
- 10.National Center for Health Statistics NHANES 1999-2004 DXA Multiple Imputation Data Files. Available from: http://www.cdc.gov/nchs/about/major/nhanes/dxx/dxa.htm. (cited 8 October 2008)
- 11.Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley, 1987 [Google Scholar]
- 12.National Center for Health Statistics National Health and Nutrition Examination Survey: technical documentation for the 1999-2004 dual energy X-ray absorptiometry (DXA) multiple imputation data files. Available from: http://www.cdc.gov/nchs/data/nhanes/dxa/dxa_techdoc.pdf (cited 8 October 2008)
- 13.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol 2001;27:85–95 [Google Scholar]
- 14.Korn EL, Graubard BI. Analysis of health surveys. New York, NY: John Wiley & Sons, Inc, 1999 [Google Scholar]
- 15.Barnard J, Rubin DB. Miscellanea. Small-sample degrees of freedom with multiple imputation. Biometrika 1999;86:948–55 [Google Scholar]
- 16.Expert WHO Committee on Physical Status Physical status: the use and interpretation of anthropometry. World Health Organ Tech Rep Ser 1995;854. [PubMed] [Google Scholar]
- 17.Blew RM, Sardinha LB, Milliken LA, et al. Assessing the validity of body mass index standards in early postmenopausal women. Obes Res 2002;10:799–808 [DOI] [PubMed] [Google Scholar]
- 18.Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 2000;72:694–701 [DOI] [PubMed] [Google Scholar]
- 19.Lean ME, Han TS, Deurenberg P. Predicting body composition by densitometry from simple anthropometric measurements. Am J Clin Nutr 1996;63:4–14 [DOI] [PubMed] [Google Scholar]
- 20.Piers LS, Soares MJ, Frandsen SL, O'Dea K. Indirect estimates of body composition are useful for groups but unreliable in individuals. Int J Obes Relat Metab Disord 2000;24:1145–52 [DOI] [PubMed] [Google Scholar]
- 21.Deurenberg P, Weststrate JA, Seidell JC. Body mass index as a measure of body fatness: age- and sex-specific prediction formulas. Br J Nutr 1991;65:105–14 [DOI] [PubMed] [Google Scholar]
- 22.Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups?. Am J Epidemiol 1996;143:228–39 [DOI] [PubMed] [Google Scholar]
- 23.Bosy-Westphal A, Geisler C, Onur S, et al. Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes 2006;30:475–83 [DOI] [PubMed] [Google Scholar]
- 24.Flegal KM. Anthropometric evaluation of obesity in epidemiologic research on risk factors: blood pressure and obesity in the Health Examination Survey. PhD dissertation. Cornell University, Ithaca, NY, 1982 [Google Scholar]
- 25.Garrow JS, Webster J. Quetelet's index (W/H2) as a measure of fatness. Int J Obes 1985;9:147–53 [PubMed] [Google Scholar]
- 26.Bigaard J, Tjonneland A, Thomsen BL, Overvad K, Heitmann BL, Sorensen TI. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Obes Res 2003;11:895–903 [DOI] [PubMed] [Google Scholar]
- 27.Bigaard J, Frederiksen K, Tjonneland A, et al. Waist circumference and body composition in relation to all-cause mortality in middle-aged men and women. Int J Obes 2005;29:778–84 [DOI] [PubMed] [Google Scholar]
- 28.Visscher TL, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JC. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: the Rotterdam study. Int J Obes Relat Metab Disord 2001;25:1730–5 [DOI] [PubMed] [Google Scholar]
- 29.Dalton M, Cameron AJ, Zimmet PZ, et al. Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med 2003;254:555–63 [DOI] [PubMed] [Google Scholar]
- 30.Vazquez G, Duval S, Jacobs DR, Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiol Rev 2007;29:115–28 [DOI] [PubMed] [Google Scholar]
- 31.Shen W, Punyanitya M, Chen J, et al. Waist circumference correlates with metabolic syndrome indicators better than percentage fat. Obesity (Silver Spring) 2006;14:727–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lemieux S, Prud'homme D, Bouchard C, Tremblay A, Despres JP. A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am J Clin Nutr 1996;64:685–93 [DOI] [PubMed] [Google Scholar]
- 33.Harris TB, Visser M, Everhart J, et al. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women. The Health, Aging and Body Composition Study. Ann N Y Acad Sci 2000;904:462–73 [DOI] [PubMed] [Google Scholar]
- 34.Norgan NG, Ferro-Luzzi A. Weight-height indices as estimators of fatness in men. Hum Nutr Clin Nutr 1982;36:363–72 [PubMed] [Google Scholar]
- 35.Curtin F, Morabia A, Pichard C, Slosman DO. Body mass index compared to dual-energy x-ray absorptiometry: evidence for a spectrum bias. J Clin Epidemiol 1997;50:837–43 [DOI] [PubMed] [Google Scholar]
- 36.Fernandez JR, Heo M, Heymsfield SB, et al. Is percentage body fat differentially related to body mass index in Hispanic Americans, African Americans, and European Americans?. Am J Clin Nutr 2003;77:71–5 [DOI] [PubMed] [Google Scholar]
- 37.Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63 [DOI] [PubMed] [Google Scholar]
- 38.Misra A. Revisions of cutoffs of body mass index to define overweight and obesity are needed for the Asian-ethnic groups. Int J Obes Relat Metab Disord 2003;27:1294–6 [DOI] [PubMed] [Google Scholar]
- 39.Pan WH, Flegal KM, Chang HY, Yeh WT, Yeh CJ, Lee WC. Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: implications for definitions of overweight and obesity for Asians. Am J Clin Nutr 2004;79:31–9 [DOI] [PubMed] [Google Scholar]
- 40.Stevens J. Ethnic-specific revisions of body mass index cutoffs to define overweight and obesity in Asians are not warranted. Int J Obes Relat Metab Disord 2003;27:1297–9 [DOI] [PubMed] [Google Scholar]
- 41.Stevens J, Nowicki EM. Body mass index and mortality in asian populations: implications for obesity cut-points. Nutr Rev 2003;61:104–7 [DOI] [PubMed] [Google Scholar]
- 42.Aloia JF, Vaswani A, Ma R, Flaster E. Body composition in normal black women: the four-compartment model. J Clin Endocrinol Metab 1996;81:2363–9 [DOI] [PubMed] [Google Scholar]
- 43.Aloia JF, Vaswani A, Ma R, Flaster E. Comparison of body composition in black and white premenopausal women. J Lab Clin Med 1997;129:294–9 [DOI] [PubMed] [Google Scholar]
- 44.Stevens J, Plankey MW, Williamson DF, et al. The body mass index-mortality relationship in white and African American women. Obes Res 1998;6:268–77 [DOI] [PubMed] [Google Scholar]
- 45.Stevens J, Juhaeri, Cai J, Jones DW. The effect of decision rules on the choice of a body mass index cutoff for obesity: examples from African American and white women. Am J Clin Nutr 2002;75:986–92 [DOI] [PubMed] [Google Scholar]
- 46.Aloia JF, Vaswani A, Mikhail M, Flaster ER. Body composition by dual-energy X-ray absorptiometry in black compared with white women. Osteoporos Int 1999;10:114–9 [DOI] [PubMed] [Google Scholar]
- 47.Evans EM, Rowe DA, Racette SB, Ross KM, McAuley E. Is the current BMI obesity classification appropriate for black and white postmenopausal women?. Int J Obes (Lond) 2006;30:837–43 [DOI] [PubMed] [Google Scholar]
- 48.Abell JE, Egan BM, Wilson PW, Lipsitz S, Woolson RF, Lackland DT. Age and race impact the association between BMI and CVD mortality in women. Public Health Rep 2007;122:507–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sanchez AM, Reed DR, Price RA. Reduced mortality associated with body mass index (BMI) in African Americans relative to Caucasians. Ethn Dis 2000;10:24–30 [PubMed] [Google Scholar]
- 50.Stevens J, Keil JE, Rust PF, Tyroler HA, Davis CE, Gazes PC. Body mass index and body girths as predictors of mortality in black and white women. Arch Intern Med 1992;152:1257–62 [PubMed] [Google Scholar]
- 51.Wienpahl J, Ragland DR, Sidney S. Body mass index and 15-year mortality in a cohort of black men and women. J Clin Epidemiol 1990;43:949–60 [DOI] [PubMed] [Google Scholar]
- 52.Ball SD, Altena TS, Swan PD. Comparison of anthropometry to DXA: a new prediction equation for men. Eur J Clin Nutr 2004;58:1525–31 [DOI] [PubMed] [Google Scholar]
- 53.Salamone LM, Fuerst T, Visser M, et al. Measurement of fat mass using DEXA: a validation study in elderly adults. J Appl Physiol 2000;89:345–52 [DOI] [PubMed] [Google Scholar]
- 54.van der Ploeg GE, Withers RT, LaForgia J. Percent body fat via DEXA: comparison with a four-compartment model. J Appl Physiol 2003;94:499–506 [DOI] [PubMed] [Google Scholar]
- 55.Withers RT, LaForgia J, Pillans RK, et al. Comparisons of two-, three-, and four-compartment models of body composition analysis in men and women. J Appl Physiol 1998;85:238–45 [DOI] [PubMed] [Google Scholar]
- 56.Withers RT, LaForgia J, Heymsfield SB. Critical appraisal of the estimation of body composition via two-, three-, and four-compartment models. Am J Hum Biol 1999;11:175–85 [DOI] [PubMed] [Google Scholar]
- 57.Wang J, Thornton JC, Bari S, et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr 2003;77:379–84 [DOI] [PubMed] [Google Scholar]