Abstract
Study Objectives:
The present study investigated the effectiveness of a school-based intervention in increasing sleep knowledge and improving adolescent sleep problems.
Design:
A randomized, controlled trial using 2 groups (program class, classes-as-usual: [CAU]) assessed over 3 time points (pre-program, post-program, 6-week follow-up).
Participants/Setting:
Eighty-one students (mean age = 15.6 ± 0.6 y; 33% male) from 2 schools in South Australia. Schools provided one class to participate in the sleep intervention program (N = 41) and a second class to act as a control class (N = 40).
Intervention:
Four 50-minute classes across a 4-week period. Classes consisted of educating adolescents on promoting and maintaining a healthy lifestyle based on a cognitive-behavior therapy framework.
Measurements and Results:
Data were collected pre-program, post-program, and at 6-week follow-up using an online questionnaire. Qualitative student and teacher data were collected at post-program. Baseline data indicated sleep problems were prevalent (53.1% insufficient sleep on school nights [ < 8 h] and 77.8% discrepant school/weekend rise times [ > 2 h]). These 2 criteria identified 36 adolescents with a delayed sleep timing (DST; Program, N = 21; CAU, N = 15). The program increased sleep knowledge (P = 0.001); however, analyses revealed no significant effects on target sleep variables as compared with the CAU class for the entire group (all P > 0.05). For DST adolescents, there was a significant interaction for reducing the discrepancy between school and weekend out of bed times (P = 0.002). There was no impact on other sleep parameters or depressed mood.
Conclusions:
School-based sleep interventions for adolescents are a novel method for addressing a prevalent problem. Future programs should develop ways to motivate adolescents to change sleep practices.
Citation:
Moseley L; Gradisar M. Evaluation of a school-based intervention for adolescent sleep problems. SLEEP 2009;32(3):334–341.
Keywords: Adolescent sleep, sleep education, school intervention, sleep-wake cycle, circadian rhythms
DURING ADOLESCENCE THE DISCREPANCY BETWEEN SCHOOL NIGHT SLEEP AND WEEKEND SLEEP GROWS MARKEDLY WITH AGE.1 NUMEROUS STUDIES across cultures have demonstrated adolescent sleep practices lead to later bedtimes and subsequent inadequate sleep on school nights because of forced rise times.1–4 This ongoing pattern of inadequate sleep on school nights influences adolescent sleep behavior on weekends, with delayed rise times allowing for an increase in total amount of sleep on weekends.1,3–5 The delay in adolescent sleep onset and offset has historically been attributed to psychosocial factors.1 However, persistence of the sleep delay occurs due to underlying biologic regulatory processes that appear to change significantly from childhood to adolescence.1,6,7 The combination of delayed bedtime on weekends and sleeping-in on weekend mornings also results in a delay of the sleep circadian rhythm in and of itself.8,9 With growing evidence that chronic inadequate sleep results in negative daytime consequences (e.g., daytime sleepiness, depressed mood),10,11 interventions designed to reverse adolescent delayed sleep timing may help alleviate these problems.12
Treatment of sleep problems in adults generally consist of a combination of behavioral and cognitive strategies, and to date, treatment of adolescent sleep problems largely rely on the adaptation of successful treatment methods used with adults.12,13 Comprehensive treatments are likely to include combinations of sleep hygiene education,14 including the regularization of bedtime/waketime routine across the week15; early morning bright light exposure16,17; stimulus control therapy18; and cognitive therapy to address unhelpful sleep beliefs.19 In exceptional circumstances, psychopharmacological treatments are used but are not recommended until behavioral and cognitive treatments have been exhausted.19 However, despite the fact that cognitive-behavioral strategies have extensive empirical support for adults, support for their application to adolescent sleep problems is limited.
Despite the potential benefit of treatment, screening is rare for sleep problems in adolescents in primary healthcare settings.20 In addition, the existing literature indicates that adolescents who do attend therapy for sleep problems show inconsistent treatment attendance, high dropout rates, poor treatment adherence, and variable motivation.12 Thus, novel methods, such as school-based sleep education programs, have potential to circumvent such problems.
The benefits of school-based prevention programs have been demonstrated for a variety of disorders.21–23 Although largely untested in the area of sleep, recent studies exploring the effectiveness of school-based sleep interventions have shown promise.24–26 However, these programs have largely focused on promoting good sleep hygiene despite the observation that empirical evidence for sleep hygiene as the sole treatment is limited.27 Other limitations, including selection bias (given low response rates, e.g. 44.5%), a lack of control group comparison,26 small sample sizes, compliance issues, and lack of follow-up data,24,25 suggest the need for improved implementation and evaluation of such programs in schools.
Researchers in other fields (e.g., drug prevention) have noted that acquisition of knowledge is rarely enough in itself to change behavior.28 However, interactive, multisession prevention programs that encourage student participation have been shown to be more effective than brief didactic programs (e.g., < 3 lecture-style classes) in changing target behavior28–30 due to higher levels of student engagement facilitating application of new knowledge, as well as attitudinal and behavioral change.28–30 The present study was developed to evaluate a controlled, interactive, multi-session, school-based sleep intervention for senior secondary students (mean age = 15.6 ± 0.6 y), particularly for those adolescents with a delay in their sleep timing. The study's aims were to (1) increase sleep knowledge, and (2) effect a change in behavior that would improve sleep parameters (e.g., sleep latency, total sleep time, regularize bedtimes), and associated improvements in daytime functioning (e.g., daytime sleepiness, depressed mood).
METHODS
Participants
Participants were 81 students in year 11 psychology classes (54 females, 27 males, mean age = 15.6 ± 0.6 y) from one private and one public secondary school in Adelaide, South Australia. Both schools each provided one class to participate in the sleep-intervention program (Program, N = 41) and a second class to act as a control class (classes-as-usual [CAU], N = 40). This age group was selected because of the worsening trend of sleep problems in adolescents with increasing age,2 and the practical concern that the program not clash with existing curriculum for final-year students.
Two criteria were used to identify 36 adolescents with a delayed sleep timing (DST; Program, N = 21; CAU, N = 15). These criteria were (1) discrepant out of bed times (school vs. weekend mornings > 2 h),31 and (2) an insufficient amount of sleep on school nights.2,32 These criteria were used as it was likely that these weekend sleeping-in practices contributed to delayed sleep timing and hence insufficient sleep duration on school nights.9 Furthermore, DST adolescents reported longer sleep latencies (school nights: 45.0 min; weekends: 31.7 min) compared to good sleepers (school nights: 30.3 min; weekends: 18.8 min), suggesting the DST group experienced sleep-onset insomnia associated with their delayed sleep timing. Ethics approval for the research project was obtained from the Flinders University Social and Behavioral Ethics Committee, and the Department of Education and Children's Services Ethics Committee.
Design
The study aimed to test the effectiveness of the sleep-intervention program using a randomized, controlled trial of 2 groups (program class/ classes-as-usual) assessed over 3 timepoints (pre-program, post-program, 6-week follow-up). Outcome measures were sleep behavior measures, daytime sleepiness, and depressed mood. Additional in-class measures included a behavioral intention to change questionnaire, a pre-program and post-program quiz, and qualitative feedback form.
Procedure
Following approval of the implementation of the program in schools, classes from each school were randomly allocated as either program or control classes. The return rate of consent forms was excellent (96.6%). The program, named Improving Adolescent Well-Being: Day and Night, was developed and administered by the researcher (LM) who was a qualified secondary school teacher and registered psychologist. An outline of the program is provided in Appendix 1. The 4-lesson program used a cognitive-behavior therapy framework providing education relating to adolescent well-being and healthy lifestyle, outlining behavioral and cognitive strategies that students were encouraged to implement to improve their general well-being, and goal-setting in order to maintain treatment gains beyond the program. It is important to note that the sleep-related content of the program was embedded within a wider context of well-being (e.g., health eating, exercise) to reduce selection bias, as well as demand effects on self-report outcome measures. The sleep-related components included instruction in (i) adolescent sleep needs and practices; (ii) consequences of poor sleep practices; (iii) good sleep hygiene practices; (iv) regularization of sleep/wake schedule and early morning bright light exposure; (v) stimulus control therapy instructions; and (vi) sleep-compatible cognitive and behavioral strategies. Students were encouraged to use strategies to improve sleep-onset insomnia,15,18 delayed sleep timing,15–17 anxious thoughts at bedtime,19 and general sleep hygiene.14 CAU students continued with their regular classes. Once all follow-up data were collected, a program debriefing was held for all classes (i.e., program and CAU). Program attendance rates were high (of students that provided data, 82.9% attended all 4 classes, 12.2% missed 1 session, 4.9% missed 2 sessions). The program was conducted in March-April 2007; follow-up data collection occurred in May 2007.
Measures
On-Line Program Outcome Measures
A online questionnaire battery comprised of a Sleep Patterns Questionnaire,33 the Pediatric Daytime Sleepiness Scale,34 and the Depression Anxiety Stress Scale (short form)35 was completed by adolescents. Students were asked a variety of questions relating to their sleep practices over the preceding 7-day period, including their typical go to bed time (GTB), sleep onset latency (SOL), total sleep time (TST), and out of bed time (OOB), for both the school week (Sunday to Thursday) and the weekend (Friday and Saturday). Sleep onset latencies > 30 min were classified as problematic.36 Daytime sleepiness was measured via the Paediatric Daytime Sleepiness Scale (PDSS).34 The PDSS has eight items targeting aspects of daytime sleepiness pertinent to adolescents (e.g., How often do you get sleepy or drowsy while doing your homework?). Statements are rated on a 5-point Likert scale (0 = Never to 4 = Always), with higher scores indicating greater daytime sleepiness. Excessive daytime sleepiness was defined as a PDSS score ≥ 20.34 The PDSS demonstrated adequate internal reliability in the present study (Cronbach α = 0.64). Depressed mood was measured using the depression subscale of The Depression Anxiety Stress Scale-21 (DASS-21).35 This is a reliable and valid short form of the 42-item scale.37 The depression subscale consists of seven statements (e.g., I couldn't seem to experience any positive feeling at all). Each statement is rated on a 4-point Likert scale as to how often the statement has applied to the participant over the past week (0 = Did not apply to me at all to 3 = Applied to me very much). Higher scores indicate higher levels of this mood state. The DASS-21 demonstrated good internal consistency in the present study (Cronbach α = 0.85). Overall, online questionnaires have been shown to be comparable to pen-and-paper versions,38 especially when researchers are present39 as occurred in the present study.
In-Class Measures: Program Class Only
Students completed a brief 25-item quiz to assess their “well-being” knowledge (which included 13 items assessing sleep knowledge) during the first lesson of the program. Students judged the statements as either true or false or don't know. Students had no prior knowledge that they were going to undertake the quiz at pre- or post-program, and thus did not practice for the quiz on either occasion. Students were given feedback of both their quiz results after follow-up data collection. In lesson 2, students in program classes completed a Behavior Intentions Questionnaire (BIQ) developed for the present study. The BIQ was based on the 5 stages of change as outlined in the Transtheoretical Model of Behavior Change.40 Adolescents were asked to indicate their intention to change each of 6 target behaviors using commitment language phrases statements that indicated their level of commitment to behavioral change41 (0 = I don't plan to, 1 = I want to, 2 = I need to, 3 = I will, 4 = I already do, 5 = I tried to). Behavior items regarding sleep practices included regularization of sleep routine (e.g., intention to “get up at the same time everyday—even on weekends”) among others. This questionnaire was completed following the second lesson, which encouraged students to make changes in line with their personal needs during the coming week. Finally, students in the program classes provided qualitative feedback on (1) their perceived learning experiences, (2) most beneficial aspects of the program, and (3) suggestions for future improvements of the program. As class teachers were present during program classes they also provided similar qualitative feedback.
Statistical Analyses
Of a possible 88 students, 5 were excluded from the final sample because consent forms were not returned (Program: N=1, CAU: N=2) or because they did not complete pre-program measures due to absence (Program: N=1, CAU: N=1). Prior to analyses, data for all variables were inspected for missing values, normality, and outliers. As a result of data screening, the data from one student in the program class were excluded from analyses because scores on many items were significant outliers, and data from a student in the control class were excluded because the pattern of responses was considered unreliable. The final sample consisted of 81 students (Program: N=41, CAU: N=40). Three variables were significantly skewed (i.e., TST, SOL, and depressed mood) and therefore required transformations (i.e., square root for SOL and depressed mood; reflected square root for TST) before mixed-model analyses.42
All quantitative data analyses were conducted using the Statistical Package for the Social Sciences (SPSS v.15, SPSS Inc., Chicago, USA). Unpaired-samples t-tests were used to investigate baseline differences between the 2 groups, with differences in results between the pre- and post-program quiz tested using paired-samples t-tests. An alpha level of 0.05 was set. Effect sizes using Cohen's d were calculated and reported.43 Linear mixed-model analyses were used to analyze the 2 (group: Program; CAU) x 3 (time: pre-program, post-program, 6-week follow-up) mixed-model design. Mixed-model analyses have the advantage of being able to handle missing data in a flexible and robust manner.42,44 Therefore, all participants that provided baseline data (regardless of missing data at one or more assessment points) were included in the data analyses. Qualitative program evaluation data were categorized by the researcher according to emerging themes.45
RESULTS
Pre-Program Measures
Means and standard deviations (SD) for sleep, daytime sleepiness, and mood for all students are presented in Table 1. At baseline, 95% of the total sample reported at least one type of sleep problem. Specifically, 60% reported a sleep onset latency > 30 min, and 35% reported excessive daytime sleepiness. More than half the sample (53%) reported insufficient sleep on school nights (< 8 h), with 78% students also reporting discrepant out of bed times (school vs. weekend mornings; > 2 h). No significant differences were found at pre-program (Time 1) between classes on these target outcome variables.
Table 1.
Adolescent Sleep Characteristics, Daytime Sleepiness and Depressed Mood for Program and Control Classes at Times 1 (Pre-Program), 2 (Post-Program), and 3 (6-Week Follow-Up).
| Program |
Control (CAU) |
|||||
|---|---|---|---|---|---|---|
| Time 1 M (SD) N=41 | Time 2 M (SD) N=40 | Time 3 M (SD) N=34 | Time 1 M (SD) N=40 | Time 2 M (SD) N=34 | Time 3 M (SD) N=32 | |
| Sleep Measures | ||||||
| Total Sleep Time − school nights (h) | 7.62 (1.0) | 7.81 (1.0) | 7.74 (1.0) | 7.61 (0.9) | 7.99 (0.8) | 7.76 (0.7) |
| Sleep Onset Latency − school nights (min) | 32.6 (27.8) | 31.8 (30.2) | 30.0 (29.5) | 41.3 (34.6) | 33.6 (24.3) | 37.5 (29.4) |
| Discrepant School/Weekend Out of Bed (h) | 2.91 (1.4) | 2.51 (1.3) | 2.76 (1.0) | 2.93 (1.4) | 2.61 (1.4) | 2.54 (1.4) |
| Daytime Measures | ||||||
| PDSS | 17.1 (4.7) | 17.5 (4.4) | 16.7 (5.1) | 17.4 (4.6) | 17.0 (4.5) | 17.9 (4.7) |
| DASS21 − Depressed mood | 7.7 (7.3) | 8.2 (6.8) | 10.2 (7.8) | 10.0 (9.0) | 11.1 (10.3) | 12.3 (10.2) |
Note: Data are descriptive statistics and therefore are not same as the adjusted means given in linear mixed modeling output; Untransformed means provided for Total Sleep Time, Sleep Onset Latency, and Depressed mood to assist with interpretation.
A comparison of baseline scores for students identified with DST yielded no significant differences between the program and CAU groups on target outcome variables (all P > 0.05). Means and SD scores for DST adolescents are found in Table 2.
Table 2.
Delayed Sleep Timing (DST) Adolescents' Sleep Characteristics, Daytime Sleepiness and Depressed Mood for Program and Control Classes at Times 1 (Pre-Program), 2 (Post-Program), and 3 (6-Week Follow-Up).
| Program |
Control (CAU) |
|||||
|---|---|---|---|---|---|---|
| Time 1 M (SD) N=21 | Time 2 M (SD) N=21 | Time 3 M (SD) N=17 | Time 1 M (SD) N=15 | Time 2 M (SD) N=12 | Time 3 M (SD) N=13 | |
| Sleep Measures | ||||||
| Total Sleep Time − school nights (h) | 6.89 (0.8) | 7.30 (1.0) | 7.13 (0.9) | 6.93 (0.9) | 7.39 (0.7) | 7.56 (0.6) |
| Sleep Onset Latency − school nights (min) | 42.9 (35.0) | 37.9 (39.0) | 39.7 (38.6) | 48.0 (43.6) | 36.3 (25.2) | 35.0 (28.8) |
| Discrepant School/Weekend Out of Beda (h) | 3.50 (0.8) | 2.97 (1.2) | 2.89 (1.1) | 3.91 (1.1) | 3.42 (1.5) | 2.83 (1.6) |
| Daytime Measures | ||||||
| PDSS | 17.9 (4.4) | 19.0 (4.2) | 17.5 (5.7) | 18.0 (4.7) | 17.8 (4.0) | 18.8 (4.3) |
| DASS21 − Depressed mood | 9.1 (8.0) | 10.0 (7.7) | 12.9 (7.3) | 12.0 (10.5) | 14.2 (11.8) | 13.9 (10.7) |
Note: Alphabetical superscript indicates significant interaction effect for:
Class*Time; Data are descriptive statistics and therefore are not same as the adjusted means given in linear mixed modeling output; Untransformed means provided for Total Sleep Time, Sleep Onset Latency, and Depressed Mood to assist with interpretation.
Evaluation of Program Versus CAU on Sleep Parameters and Mood
Linear mixed-model analyses revealed no significant interactions (all F ≤ 0.60, all P ≥ 0.44) or main effects for class (all F ≤ 2.3, all P ≥ 0.135) for all variables. Main effects for time were also not significant (all F ≤ 2.44, all P ≥ 0.12).
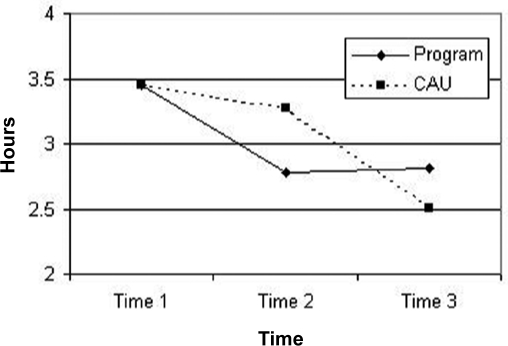
For students identified with DST, the linear mixed-model analyses revealed a significant “class” x “time” interaction for “out of bed” time, F1,23.27=8.56, P = 0.008. There was a medium, within-subjects effect on reducing the discrepancy between school and weekend out of bed time for the program class (d = 0.65), compared to a negligible effect for the control class (d = 0.15) (Figure 1). At post-program there was a medium between-subjects effect on this discrepancy (d = 0.36), however, both groups came together at the 6-week follow-up (d = −0.05). All other interaction and main effects were not significant (all F ≤ 2.56, all P ≥ 0.12).
Figure 1.
Graphic representation of the discrepancy between school/weekend out of bed' times by class and time for DST adolescents only. Note: Means from linear mixed-model regression (LMMR) analyses controlling for time 1 (baseline) means (i.e., LMMR equates baseline means, therefore means at all timepoints will differ from means reported in Table 2). This figure is to demonstrate the interaction between groups and over time. For means derived from direct measurement, refer to Table 2.
Program Group “In Class” Analyses
There was a statistically significant increase in the total number of correct answers to sleep-related items from pre-program (M =7.21, SD =1.80) to post-program [M = 8.52, SD = 1.60], t37 = 3.45, P = 0.001. From the Behavioral Intentions Questionnaire, adolescents in the program class indicated that although keen to increase total sleep time to 9 hours (e.g., “I don't plan to” = 2.6%, vs. “I need to” = 40.5%, “I will” = 16.7%), many students were not keen to regularize weekend wake up times (“I don't plan to” = 34.2%), or utilize morning bright light exposure (“I don't plan to” = 31.6%). In comparison, students were far more committed to improving other aspects of well-being (e.g., exercise and healthy eating; “I don't plan to” = 5.3%, “I need to” = 26.3%, “I will” = 23.7%).
Program Feedback
Students were asked to provide qualitative feedback following the program on what they had learned. A large proportion (41.9%) reported having learned sleep-related aspects of the course as their primary outcome (e.g., “I knew sleep was important; but I value it more now and think it is just as important as diet and exercise”). A small group (9.3%) indicated they learned strategies that could be applied in their personal life to improve their general well-being; 2 students (4.7%) reported that, although they had learned strategies, there were impediments such as low motivation to applying their learning (e.g., “About how I need to improve on my current life style but I can't be bothered”).
Students were also asked to report the aspects of the program they had found most beneficial. Nearly a quarter of students (23.3%) reported that information relating to sleep needs of adolescents had been most beneficial (“Probably the bit about what happens to the brain and the body when you don't get enough sleep as it made me wonder what would happen to my own body if I didn't get enough sleep”), with 11.6% of students reporting that learning the benefits of sleeping 9 hours per night had been most useful. Encouragingly, 14% of students indicated that behavioral suggestions to improve their sleep had been helpful and applied in some way during the program (e.g., “I definitely tried to improve my sleeping patterns over the past few weeks. On nights that I could, I would go to bed at 11 and actually fall asleep within half an hour. I also tried taking ‘power naps’ instead of my usual 3-hour naps. I liked these and I think I may continue to do them.”). In addition to the students above, 9.3% students endorsed all aspects of the sleep-related program. Some students (14%) reported finding none of the sleep-related content beneficial (e.g., “I can't change sleep patterns and go to school and work and study at the same time”), and 7% of students indicated that sleep content of the program was not applicable to them because they did not have sleep problems.
Finally, students were offered an opportunity to provide suggestions for future improvements to the program. While a third of students provided no suggestions, other students' suggestions were generally classified under 2 main themes. A quarter of students indicated that they would have preferred more interactive class activities and hands-on tasks to increase the level of interest during lessons, and approximately 10% reported that they would have found out-of-class activities (e.g., set homework) useful in applying new information into their life.
Teacher Feedback
Class teachers' feedback echoed student feedback that more hands-on activities would have enhanced learning, and that more formal follow-up of implementation of strategies during the previous week would have enhanced participants' motivation to try recommended strategies, particularly those that related to increasing average sleep on school night. One teacher expressed the view that instruction of the program had benefited by being given by a trained teacher and indicated that the complexity of conducting clinical research as well as teaching the classes with senior students required the organizational skills of an experienced teacher. Given their concerns that their students were often sleepy in class, both teachers were very enthusiastic about the need for such programs for senior students.
DISCUSSION
The present study was the first to use a school-based sleep intervention with a cognitive-behavior framework to improve adolescents' sleep problems, and it was the first to use a controlled design with long-term follow-up. In contrast to previous school-based studies,24–26 sleep knowledge was also assessed pre- and post-program for intervention classes with an increase in sleep knowledge observed. The program also resulted in a behavioral change—specifically by improving adolescents' out of bedtimes at post-program for those with a delayed sleep timing (DST).
Baseline data indicated that sleep problems were prevalent among this sample of Australian adolescents (15 to 17 years). Pre-program sleep measures showed that, like their North American counterparts,2 a sizable proportion of the adolescents in this sample reported excessive daytime sleepiness (34.6%). This is not surprising, as more than 50% of students reported difficulty getting to sleep and insufficient sleep on school nights, and more than 75% of the sample slept in on weekend mornings ( > 2 h) as a way to compensate for reduced school night sleep. These results tend to confirm that Australian adolescents' sleep practices reflect those of their peers across the world,1 supporting the need for sleep education programs.
Unlike previous attempts of engaging adolescents in group therapy for sleep problems,12 the present study had a considerably higher retention rate (83% vs. 42%). The program enabled students to increase their knowledge about relevant sleep-related information. This is consistent with the observation by Tobler28 that prevention programs are often successful in improving knowledge. Students were not aware that they would be retested at the end of the program, suggesting their increase in knowledge reflects internalization of program content rather than rote learning for testing purposes. However, it must be noted that changes in sleep knowledge were not controlled for (i.e., the control class did not do the quiz). Therefore we cannot completely exclude alternative explanations (e.g., practice effects) for the increase in sleep knowledge. Future evaluations of controlled school-based interventions should assess the knowledge of control classes.
The present study found that the school-based sleep intervention resulted in a behavioral change, with a significantly reduced discrepancy between school week and weekend out of bed times (30 min) at post-program for adolescents with DST. The regularization of out of bed times is viewed as a healthy sleep behavior, being incorporated in both sleep hygiene and stimulus control instructions.14,15,18 Sleeping-in on weekends contributes to a delay in the circadian sleep rhythm,8,9 and this can lead to insufficient sleep on school nights due to a late sleep onset and forced early morning awakening. Thus, the simple behavioral strategy of regularizing bedtimes could be a key technique to alleviating adolescent sleep problems. However, despite this statistically significant effect, there was no impact on other sleep or daytime parameters (e.g., TST; daytime sleepiness, depressed mood), and the effect disappeared by the 6-week follow-up. It is also worth noting that the control class improved their out of bed times over the course of data collection, highlighting the importance of using control classes when evaluating school-based interventions. Finally, although the reduction in discrepant out of bed times was statistically significant, it was not clinically significant, with the mean discrepancy (2.97 h) still well above the cut-off of 2 h.8,9 Despite the limitations of these findings, the potential for school-based sleep interventions still remain, given qualitative information gleaned in the present study (e.g., behavioral intentions to change, student and teacher feedback).
Interestingly, results from the Behavior Intentions Questionnaire indicated that many students wanted more sleep, but they were honest in stating that they did not want to change their weekend and school morning behavior to do this. In fact, their responses would suggest that they were not convinced by the program that the behavioral strategies provided (e.g., get up same time every day) would result in more school night sleep. This suggests there was no need to disguise the sleep content with well-being information in order to reduce demand characteristics on self-reported outcome measures. Instead, non-sleep content could have been replaced with extra sleep content specifically intended to provide more convincing information to motivate adolescents to change sleep behaviors (i.e., no sleeping-in on weekends, and curtailing night time activities in order to achieve more increased TST on school nights). This “dose” increase in sleep education could lead to a greater statistical and clinical effect on target sleep parameters. Thus, it will be important to develop ways of increasing motivation as a primary learning objective in future curriculum development,40 given that these behaviors are unpopular to adolescents.
Nearly a quarter of students suggested that the program needed to incorporate more opportunities for interactive learning experiences,28 suggesting there was still room to engage students further in their learning. Suggestions included hands-on class activities and the use of set homework to transfer knowledge into practice. Feedback from teachers supported this view. Such activities could increase motivation to change for adolescents, thus increasing the likelihood of improving and maintaining healthier sleep patterns. Future studies would also be enhanced by using sleep diaries that require students to monitor their sleep over a 7-day period. In the present study, students were asked to reflect back on their sleep practice over the preceding school week and weekend. While this had the advantage of being a relatively simple way of capturing their average school night and weekend sleep, students may have inadvertently made errors in reporting their sleep practices. A sleep diary completed each morning would improve accuracy in student reports of their sleep practices,36 and have the added advantage of providing useful information to students about their sleep needs to guide and motivate them to make changes to their sleep routine during and after the sleep intervention program.
CONCLUSION
The present study demonstrated an increase in sleep knowledge and a subsequent change in sleep behavior (i.e., improving out of bed times) for adolescents with delayed sleep timing. Given this effect was not maintained in the long-term, the quantitative and qualitative findings from the present study suggest future school-based sleep interventions need (i) not be overly concerned about demand effects on sleep measures, and thus concentrate solely on sleep education, (ii) to motivate adolescents to make simple behavioral changes, rather than learn more complex techniques (i.e., cognitive strategies), (iii) to use teachers to deliver more interactive, “hands-on” exercises, and (iv) to evaluate programs with control classes and follow-ups. Nonetheless, school-based sleep programs are a promising model for intervention for adolescent sleep problems given their high retention rate, cost-effectiveness, and potential for promoting healthy sleep knowledge and practice.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors wish to thank the Faculty of Social Sciences, Flinders University for their financial assistance, Dr Nathan Weber for his assistance with the on-line administration of the questionnaires, the Principals of Concordia College and Unley High School for approving the implementation of the program in their schools, teachers Ms. Ruth Eckert, Ms. Kezia Rhode, Ms. Nikki Krieg, and Mr. Graham Clark for accommodating the program in their courses, and all the students involved in the study.
Financial support: Faculty of Social Sciences, Flinders University.
APPENDIX 1
Overview of Adolescent Well-Being: Day and Night Education Program
Pre-Program Measures: On-line Questionnaires
Lesson 1—Well-Being in Adolescence: Making good choices day and night
Objectives:
to provide information about developmental trends in adolescent well-being
to inform students of factors that compromise well-being, including inadequate sleep
Lesson Content
Defining ‘well-being’
Positive well-being in adolescence
Risk factors to adolescent well being
Developmental trends in adolescence: regarding diet, exercise, sleep, mood
Promoting well-being – impact of balance in diet, exercise, and sleep on well-being
Strategies
Class discussions: peer reflection
Personal reflection: contemplation of personal changes that may increase well-being
Lesson 2—Enhancing Well-Being: Things to do both day and night
Objectives:
to provide behavioral strategies that enhance student well-being.
to encourage students to make behavioral changes in line with their personal needs.
Lesson Content
Benefits of exercise, healthy diet and sleep on well-being
Information regarding human sleep cycle, circadian rhythms, adolescent sleep needs and impact of sleep deprivation
Strategies
Daytime choices: outlining behaviors that can improve well-being including regular exercise, healthy food choices, reducing caffeine intake, cutting out naps.
Nightime choices: outlining behaviors that can improve well-being including increasing total sleep time to average 9 hours, regularizing sleep schedule across whole week, using good sleep hygiene practices, also providing tips for sleep onset insomnia including stimulus control instructions and early morning bright light exposure.
Questionnaire: measuring personal commitment to changing any of 6 specific target behaviors including sleep specific items, increasing total sleep time to average 9 hours and regularizing sleep schedule across whole week.
Personal Action: promoting change in behavior in line with responses
Lesson 3—Thinking Well: Ways of thinking that improve well-being
Objectives:
to highlight the role thinking plays in determining mood and well-being.
to learn to identify and challenge unhelpful thinking styles in order to facilitate improved well-being and commitment to positive lifestyle changes.
Content
Common thinking errors: outlining thinking errors that impact on mood and behavior (e.g., black and white thinking, filtering etc.)
Identifying common thinking errors: using scenarios and role plays
Challenging thinking errors: benefits in changing unhelpful thinking on mood and behavior
Strategies
Role plays and scenarios: to highlight effects of unhelpful thinking
Small group discussion: peer reflection
Cognitive challenging: using ABCDE analysis worksheet
Personal Action: encouraging continued change in behavior and thoughts in order to maintain improvements in well-being
Lesson 4—Staying Well: Maintaining Well-Being during Senior School
Objectives:
to review learning from Lessons 1 to 3
to provide additional strategies (study skills, goal-setting) to assist students maintain well being in the longer term.
to provide opportunity for students to set personal short-term and longer-term goals.
Content
Study skills: outlining methods to improve personal organization including time management tips, procrastination ‘busters’ and study skills hints
Balance: revision of benefits of maintaining regular exercise, healthy eating, good sleep practices, and helpful thinking throughout senior secondary school and particularly in times of academic stress
Goal setting: introduction of goal setting principles in order to stay focused on short, mid and long term goals
Strategies
Goal setting activity: setting personal short-term goals and developing a plan of action
Revision of Daytime and Nighttime choices: see Lesson 2
Personal Action: committing to maintenance of changes in behavior and/or thoughts as commenced during program in order to maintain improved well-being
Learning and applying ‘Take Home’ message –
Be Active-Stay organized- Eat well-Sleep right-Change unhelpful thoughts-Keep it balanced
Post Program Measures: On-line Questionnaires
Program Classes also: Program Evaluation and Quiz
Follow-up Measures: On-line Questionnaires
Debrief Lesson
REFERENCES
- 1.Carskadon MA, Acebo C. Regulation of sleepiness in adolescents: Update, insights and speculation. Sleep. 2002;25:606–14. doi: 10.1093/sleep/25.6.606. [DOI] [PubMed] [Google Scholar]
- 2.National Sleep Foundation. 2006 Sleep in America Poll. Washington, DC: National Sleep Foundation; 2006. Retrieved November 8, 2007 from [ http://www.sleepfoundation.org/atf/cf/{F6BF2668-A1B4-4FE8-8D1A-A5D39340D9CB}/2006_summary_of_findings.pdf pdf] [Google Scholar]
- 3.Hansen MI, Schiff A, Zee PC, Dubocovich ML. The impact of school daily schedule on adolescent sleep. Pediatrics. 2005;115:1555–62. doi: 10.1542/peds.2004-1649. [DOI] [PubMed] [Google Scholar]
- 4.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–81. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 5.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–62. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 6.Laberge L, Carrier J, Lesperance P, et al. Sleep and circadian phase characteristics of adolescent and young adult males in a naturalistic summertime condition. Chronobiol Int. 2000;17:489–501. doi: 10.1081/cbi-100101059. [DOI] [PubMed] [Google Scholar]
- 7.Tzinschinsky O, Wolfson AR, Darley C, Brown C, Acebo C, Carskadon MA. Sleep habits and salivary melatonin onset in adolescents. Sleep Res. 1995;24:543. [Google Scholar]
- 8.Burgess HJ, Eastman CI. The dim light melatonin onset following fixed and free sleep schedules. J Sleep Res. 2005;14:229–37. doi: 10.1111/j.1365-2869.2005.00470.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang C-K, Speilman A. The effect of a delayed weekend sleep pattern on sleep and morning functioning. Psychol Health. 2001;16:715–25. [Google Scholar]
- 10.Acebo C, Wolfson AR. Inadequate sleep in children and adolescents. In: Kushida CA, editor. Sleep deprivation. New York: Marcel Dekker; 2005. pp. 151–71. [Google Scholar]
- 11.Millman RP. Excessive sleepiness in adolescents and young adults: Causes, consequences, and treatment strategies. Pediatrics. 2005;115:1174–86. doi: 10.1542/peds.2005-0772. [DOI] [PubMed] [Google Scholar]
- 12.Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clin Psychol Rev. 2005;25:629–44. doi: 10.1016/j.cpr.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Richardson GS, Malin HV. Circadian rhythm sleep disorders: Pathophysiology and treatment. J Clin Neurophysiol. 1996;13:17–31. doi: 10.1097/00004691-199601000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003;7:215–25. doi: 10.1053/smrv.2001.0246. [DOI] [PubMed] [Google Scholar]
- 15.Manber R, Bootzin RR, Acebo C, Carskadon MA. The effects of regularizing sleep-wake schedules on daytime sleepiness. Sleep. 1996;19:432–41. doi: 10.1093/sleep/19.5.432. [DOI] [PubMed] [Google Scholar]
- 16.Lack LC, Wright, HR Clinical management of delayed sleep phase disorder. Behav Sleep Med. 2007;5:57–76. doi: 10.1207/s15402010bsm0501_4. [DOI] [PubMed] [Google Scholar]
- 17.Rosenthal NE, Joseph-Vanderpool JR, Levendosky AA, et al. Phase-shifting effects of bright morning light as treatment for delayed sleep phase syndrome. Sleep. 1990;13:354–61. [PubMed] [Google Scholar]
- 18.Smith MT, Perlis ML. Who is a candidate for cognitive-behavioural therapy for insomnia? Health Psychol. 2006;25:15–9. doi: 10.1037/0278-6133.25.1.15. [DOI] [PubMed] [Google Scholar]
- 19.Dahl RE, Lewin, DS Pathways to adolescent health sleep regulation and behavior. J. Adolesc. Health. 2002;31:175–84. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 20.Wassell A, Soueidan A, Al Etat A, Fahmy S. Do primary care physicians screen for sleep? Sleep. 2006;29:A355. [Google Scholar]
- 21.Wade TD, Davidson, S, O'Dea JA. A preliminary controlled evaluation of a school-based media literacy program and self-esteem program for reducing eating disorder risk factors. Int J Eat Disord. 2003;33:371–83. doi: 10.1002/eat.10136. [DOI] [PubMed] [Google Scholar]
- 22.Orlando M, Ellickson PL, McCaffrey DF, Longshore DL. Mediation analysis of a school-based drug prevention program: Effects of Project ALERT. Prev Sci. 2005;6:35–46. doi: 10.1007/s11121-005-1251-z. [DOI] [PubMed] [Google Scholar]
- 23.Possel P, Baldus C, Horn AB, Groen G, Hautzinger M. Influence of general self-efficacy on the effects of a school-based universal primary prevention program of depressive symptoms in adolescents: A randomized and controlled follow-up study. J. Child Psychol Psychiatry. 2005;46:982–94. doi: 10.1111/j.1469-7610.2004.00395.x. [DOI] [PubMed] [Google Scholar]
- 24.Rossi CM, Campbell AL, Vo OT, Marco CA, Wolfson AR. Middle school sleep-smart program: a pilot evaluation. Sleep. 2002;25:A279. [Google Scholar]
- 25.Vo OT, LeChasseur K, Wolfson A, Marco C. Sleepy pre-teens: second pilot of Sleep-Smart Program in 7th graders. Sleep. 2003;26:A411. [Google Scholar]
- 26.de Sousa IC, Araujo JF, de Azevedo CVM. The effect of a sleep hygiene education program on the sleep-wake cycle of Brazilian adolescent students. Sleep Biol Rhythms. 2007;5:251–8. [Google Scholar]
- 27.Chesson AI, Anderson WM, Littner M, et al. Practice parameters for the nonpharmacological treatment of chronic insomnia. Sleep. 1999;22:1128–33. doi: 10.1093/sleep/22.8.1128. [DOI] [PubMed] [Google Scholar]
- 28.Tobler NS. Lessons learned. J Prim Prev. 2000;20:261–74. [Google Scholar]
- 29.Clarke GN, Hawkins W, Murphy M, Sheeber L. School-based primary prevention of depressive symptomatology in adolescents: Findings from two studies. J Adolesc Res. 1993;8:183–204. [Google Scholar]
- 30.Stice E, Shaw H. Eating disorder prevention programs: a meta-analytic review. Psychol Bull. 2004;130:206–27. doi: 10.1037/0033-2909.130.2.206. [DOI] [PubMed] [Google Scholar]
- 31.American Academy of Sleep Medicine. International classification of sleep disorders. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. diagnostic and coding manual. [Google Scholar]
- 32.Carskadon MA, Acebo C, Jenni, OG Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–91. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 33.Gradisar M, Terrill G, Johnston A, Douglas P. Adolescent sleep and working memory performance. Sleep Biol Rhythms. 2008;6:146–54. [Google Scholar]
- 34.Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Badia P. The Pediatric Sleepiness Scale (PDSS): Sleep habits and school outcomes in middle-school children. Sleep. 2003;26:455–8. [PubMed] [Google Scholar]
- 35.Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 36.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein, KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 37.Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and community sample. Psychol Assess. 1998;10:176–81. [Google Scholar]
- 38.Kraut R, Olson J, Banaji M, Bruckman A, Cohen J, Couper M. Psychological research online: Report of board of scientific affairs' advisory group on the conduct of research on the internet. Am Psychol. 2004;59:105–17. doi: 10.1037/0003-066X.59.2.105. [DOI] [PubMed] [Google Scholar]
- 39.Gosling SD, Vazire S, Srivastava S, John OP. Should we trust web-based studies? A comparative analysis of six preconceptions about internet questionnaires. Am Psychol. 2004;59:93–104. doi: 10.1037/0003-066X.59.2.93. [DOI] [PubMed] [Google Scholar]
- 40.Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviours. In: Hersen M, Eisler RM, Miller PM, editors. Progress in behaviour modification. Sycamore, IL: Sycamore Press; 1992. pp. 184–214. [PubMed] [Google Scholar]
- 41.Amrheim PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol. 2003;71:862–78. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- 42.Tabachnick BB, Fidell LS. Using multivariate statistics. Needham Heights MA: Allyn – Bacon; 2001. [Google Scholar]
- 43.Thalheimer W, Cook S. How to calculate effect sized from published research articles: a simplified methodology. 2003 Apr; Retrieved November 20 2007 from [ http://work-learning.com/effect_sizes.htm]
- 44.Gueoruieva R, Krystal JH. Move over ANOVA: Progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004;61:310–7. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- 45.Fossey E, Harvey C, McDermott F, Davidson L. Understanding and evaluating qualitative research. Aust N Z J Psychiatry. 2002;36:717–32. doi: 10.1046/j.1440-1614.2002.01100.x. [DOI] [PubMed] [Google Scholar]