Abstract
Efficient vaccines potentiate antibody avidity and increase T cell longevity, which confer protection against microbial lethal challenge. A vaccine strategy was established by using Lactobacillus acidophilus to deliver Bacillus anthracis protective antigen (PA) via specific dendritic cell-targeting peptides to dendritic cells (DCs), which reside in the periphery and mucosal surfaces, thus directing and regulating acquired immunity. The efficiency of oral delivery of L. acidophilus expressing a PA-DCpep fusion was evaluated in mice challenged with lethal B. anthracis Sterne. Vaccination with L. acidophilus expressing PA-DCpep induced robust protective immunity against B. anthracis Sterne compared with mice vaccinated with L. acidophilus expressing PA-control peptide or an empty vector. Additionally, serum anti-PA titers, neutralizing PA antibodies, and the levels of IgA-expressing cells were all comparable with the historical recombinant PA plus aluminum hydroxide vaccine administered s.c. Collectively, development of this strategy for oral delivery of DC-targeted antigens provides a safe and protective vaccine via a bacterial adjuvant that may potentiate mucosal immune responses against deadly pathogens.
Keywords: anthrax, lactic acid bacteria, mucosal immunity, oral, vaccine
The next generation of oral vaccines should ideally be administered in a single, tolerable, efficacious dose that induces a robust neutralizing humoral and acquired immunity against specific microbial pathogens. Moreover, such vaccines must be safe, inexpensive, and stable. Ideally, vaccine delivery vectors would stimulate immune responses at sites where pathogens interact with mammalian hosts, thereby generating the first eminent barriers against infection. An additional advantage of oral vaccination not usually observed with s.c. or intramuscular injection is the simultaneous induction of both mucosal and systemic immunity against the antigen of interest.
Live attenuated vaccine vectors such as Samonella, Bortedella, and Listeria have been successfully used to deliver heterologous antigens (1–3). Although many of the properties related to their pathogenicity make them attractive candidates for inducing immune responses, the potential for reversion of attenuated strains to virulence is a significant safety concern. Moreover, these bacteria are highly immunogenic, which may prevent their use in vaccine regimens requiring multiple doses (4).
Probiotics are defined as “live microorganisms that when administered properly, confer a health benefit to the host” (5). Lactic acid bacteria (LAB) comprise a group of Gram-positive bacteria that include species of Lactobacillus, Lactococcus, Leuconostoc, Pediococcus, and Streptococcus. It is widely accepted that Lactobacillus species play a critical role as commensals in the gastrointestinal (GI) tract. Their ability to survive transit through the stomach, close association with the intestinal epithelium, immunomodulatory properties, and their safe consumption in large amounts make lactobacilli attractive candidates for development into live vehicles for delivery of immunogens to the intestinal mucosa (6). Furthermore, it was recently shown that specific Lactobacillus species induce regulated inflammatory responses against infection, increase IgA production, activate monocytic lineages (e.g., DCs) (7–11), and regulate the balance of Th1 and Th2 pathways (12). Moreover, adjuvant-like effects on mucosal and systemic immunity have been demonstrated by using specific Lactobacillus species (13, 14). For enhancement of epitope bioavailability conferred by the delivery vehicle, specific Lactobacillus species can be selected (6).
Systemic infection with Bacillus anthracis resulting from inhalation causes a 100% mortality rate (15). Pathogenesis is due primarily to the production of toxins by these bacteria once inside the host (16). These toxins consist of 3 distinct proteins, which include a host–cell-binding component, called protective antigen (PA), and 2 enzymes, edema factor (EF) with adenylate cyclase activity and lethal factor (LF) with zinc-metalloprotease activity (17). PA binds to its cell receptor where it is cleaved by a furin-like surface protease, heptamerizes, and binds EF and LF through homologous N-terminal domains. The PA-EF or PA-LF complexes are then endocytosed (18). Acidification within the endosomes leads to insertion of PA heptamers into the endosomal membrane and subsequent release of toxin enzymes into the cytosol where they direct cellular death. The current established vaccine against deadly B. anthracis is formulated with aluminum hydroxide (alhydrogel) as an adjuvant and is administered by multiple s.c. injections. This vaccine is far from ideal because it induces significant transient side effects in individuals, making it important to find an alternate vaccine strategy for B. anthracis infections.
The mucosa represents the site for the first dynamic interactions between microbes and the human host. Accordingly, a robust and highly specialized innate, as well as adaptive, mucosal immune system protects the mucosal membrane from pathogens (e.g., Salmonella) (19, 20). Although the mucosal site normally tolerates associated commensal microbiota, specific immunity is constantly induced against invading pathogens in mucosa-associated lymphoid tissues (MALT) through the homing specificity of activated effector lymphocytes (21, 22). Professional antigen presenting DCs have been identified in numerous tissue compartments, including the lamina propria (LP), the subepithelium, a T cell-rich zone of lymphoid tissue associated with the mucosa, and draining lymph nodes (23, 24). DCs located in or beneath the epithelium can sample and capture various bacterial antigens that cross the epithelial layer through M cells (25–28). Additionally, DCs within the LP, recruited by chemokines released by epithelial cells, reach the gut epithelia expressing occludin and claudin-1 molecules. These latter molecules facilitate penetration of these cells into the tight junctions between epithelial cells. DCs subsequently extend their probing dendrites into the lumen to sample commensal or microbial immunogens (14, 29–31). These cells then migrate into the lymphoid follicles wherein processed antigens are presented to B and T cells to initiate humoral (IgA) and T cell immune responses (10).
A strategy that specifically targeted a hepatitis C viral antigen to DCs by using 12-mer peptides elicited efficient antigen-specific immune responses in vivo (32, 33). It is noteworthy that the antigen–DC peptide fusions in this study did not modify the phenotype or the function of DCs, highlighting their proficiency at directing antigens to mature and immature DC subsets without inducing anergy in these cells. To extend and refine this vaccine platform, Lactobacillus acidophilus was selected to specifically deliver B. anthracis PA fused to a DC-targeting peptide (DCpep) to mucosal DCs. Our data clearly show that this vaccine strategy elicited robust protective immune responses against B. anthracis, resolving the infection in mice.
Results
Expression of rPA in L. acidophilus.
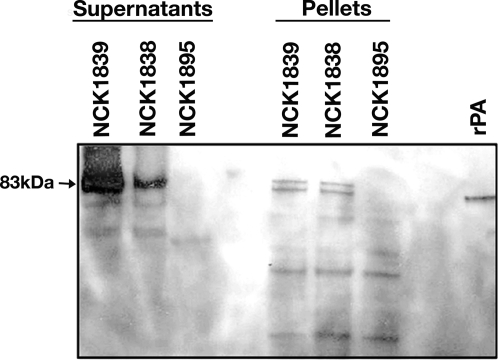
To establish a platform for oral vaccine delivery, the constructed plasmids were successfully transformed into L. acidophilus (Fig. 1 A and B and Table 1). The PA fusion proteins were secreted by L. acidophilus and were identified in the cell supernatants. Fig. 2 shows the lanes of an SDS/PAGE gel in which supernatants or cell pellets of cultures of L. acidophilus NCK1838 (PA-Ctrlpep), NCK1839 (PA-DCpep), and NCK1835 (empty vector) were loaded and subjected to Western blot analysis using anti-PA antibody. The identity of the 2 83-kDa bands in the culture supernatants were confirmed as the PA fusion proteins (Fig. 2).
Fig. 1.
Plasmids for expression of rPA peptide fusions. Map of constitutive rPA/DC-peptide fusions and control plasmid, pTRK895 (A) and schematic of the expression cassettes for DCpep and Ctrlpep, pTRK896 and pTRK895 (B), respectively. Replication determinants are shown as black arrows; transcriptional terminators are shown as black boxes; the erythromycin resistance gene is shown in dark gray; pag is shown in light gray; DC or Ctrl (control) peptide coding sequences are represented by the gray arrow (pag); promoters are shown in white.
Table 1.
Bacterial strains and plasmids
| Strain or plasmid | Relevant characteristics |
|---|---|
| L. acidophilus | |
| NCFM | Human intestinal isolate |
| NCK 1838 | NCFM w/ pTRK895 (PA-Ctrlpep) |
| NCK 1839 | NCFM w/ pTRK896 (PA-DCpep) |
| NCK 1895 | NCFM w/ pTRK882 (empty vector) |
| Escherichia coli | |
| MC-1061 | Strr, E. coli transformation host |
| Plasmids | |
| pTRK882 | 4.5-kb, Emr, constitutive expression vector, Ppgm promoter |
| pPAGctrl | 5.7-kb, AmpR source of pagctrl gene |
| pPAGDC | 5.7-kb, AmpR source of pagDC gene, encodes PADC |
| pTRK895 | 6.8-kb, Ermr, pTRK882::pagcon, constitutive expression of PA-ctrlpep |
| pTRK896 | 6.8-kb, Ermr, pTRK882::pagdc, constitutive expression of PA-DCpep |
Fig. 2.
Western blots of PA-DC and PA-Ctrl expressed proteins. Proteins were TCA-precipitated from the supernatants and the cell-free extracts of log-phase cultures of L. acidophilus NCK1838, NCK1839, and NCK1895 were resuspended in 50 mM NaOH and 10 μg was loaded and electrophoresed on a 12% polyacrylamide gel. Proteins were transferred onto a nitrocellulose membrane and probed with HRP-anti-PA antibody. Data are representative of a least 5 different experiments.
L. acidophilus Interactions with DCs.
To demonstrate that L. acidophilus strains expressing PA fusions and their controls can be captured by mouse DCs, Alexa Fluor 647-labeled bacteria were cocultured with DCs. Data show that mouse DCs efficiently captured labeled L. acidophilus strains, indicating that the endocytotic pathway of DCs was not impaired [supporting information (SI) Fig. S1A). Additionally, the cytokines released by DCs treated with these L. acidophilus strains were studied. Interestingly, low levels of IL-12 production was detected in DCs treated with L. acidophilus NCK 1839 expressing PA-DCpep (Fig. S1B). Other cytokines such as TNFα, IL-6, and IL-10 were induced at approximately the same levels in mouse DCs treated with all 3 recombinant L. acidophilus strains (Fig. S1B).
Vaccination with Recombinant L. acidophilus.
L. acidophilus strains expressing PA-Dcpep or PA-Ctrlpep or harboring the vector were grown to late log phase in deMan, Rogosa, and Sharpe (MRS) medium with erythromycin (ERM) and then pelleted, washed, and resuspended at 109 CFU in 250 μL in PBS. A/J mice were orally vaccinated with L. acidophilus NCK1839 (PA-DCpep), L. acidophilus NCK1838 (PA-Ctrlpep), or L. acidophilus NCK1895 (empty vector), and challenged with B. anthracis Sterne (5 × 104 CFU per mouse). The results showed that 12 of 16 mice (75%) vaccinated with L. acidophilus expressing PA-DCpep survived, whereas only 4 of 16 mice in the control group vaccinated with L. acidophilus expressing PA-Ctrlpep survived the lethal challenge with B. anthracis Sterne (Fig. 3 A–C). All other groups, including L. acidophilus containing null vector (n = 16) or PBS alone (n = 20), succumbed to the lethal challenge (Fig. 3 B and C). The current anthrax vaccine, rPA adsorbed to alhydrogel, given in a single s.c. injection, protected 16 of 20 mice from B. anthracis Sterne lethal challenge (Fig. 3 B and C). Thus, results from these studies further highlight the efficacy of employing probiotic lactic acid bacteria in vaccine platforms, whereupon microbial immunogens such as B. anthracis PA can be delivered by using small DC-targeting peptides fused to the C terminus of the antigen.
Fig. 3.
Protective immunity against B. anthracis Sterne. (A) Vaccination schedule. Groups of mice were orally vaccinated with L. acidophilus 1838, 1839, or 1895 (109 CFU in 250 μL). The oral route was repeated 3 times weekly. Two weeks later, the groups of mice were boosted twice. Seven days after the final boost, the mice were challenged i.p. with B. anthracis Sterne pXO1+/pXO2− (5 × 104 CFU per mouse). Survival was then monitored until day 40. (B and C) Mouse survival. Vaccinated and nonvaccinated mice were challenged i.p. with B. anthracis Sterne. Survival was then monitored until day 40. Data are representative of 2 independent experiments.
Anti-PA Antibody Analysis.
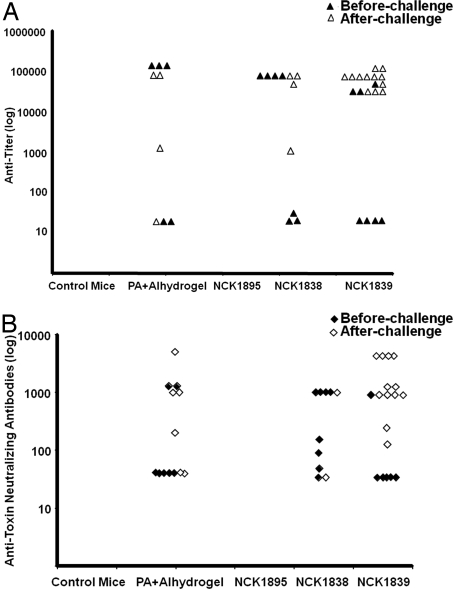
The production of anti-PA antibodies in vaccinated mice as well as in those mice that survived the challenge was analyzed by ELISA. Sera derived from the mice that survived challenge contained high titers of anti-PA antibodies, which were comparable with antibody levels from mice in the group vaccinated with rPA plus alhydrogel (Fig. 4A). Interestingly, mice vaccinated with L. acidophilus expressing PA-Ctrlpep also showed a range of anti-PA titers, but the titers were not sufficient to elicit the same degree of protective immunity to allow their survival.
Fig. 4.
Detection of Anti-PA antibodies. After the vaccination regime, sera were derived from each group of mice just before and after challenge with B. anthracis Sterne for assays of anti-PA antibodies (A) and the anti-toxin neutralizing antibodies (B). Each triangle or diamond represents the value of anti-PA antibody detected in the serum of each individual mouse. The antibody responses for the control mice and those treated with NCK1895 (empty vector) were below the detection limit. For some of the mice vaccinated with DC-pep or Ctrlpep, IgG levels were below the detection limits, and these values were not recorded on the figure. Each symbol of each value represents the serum derived from each mouse. All data are representative of 2 independent experiments.
B. anthracis Toxin-Neutralizing Antibodies.
To determine the levels of B. anthracis toxin-neutralizing anti-PA antibodies elicited by L. acidophilus expressing PA-DCpep versus its control, a toxin-neutralization assay was performed (34). This assay was performed to demonstrate that anti-PA antibodies released by peripheral immune cells were capable of preventing the association of PA to the B. anthracis lethal factor (LF) or the binding of lethal toxin (PA + LF) to cell receptors, thereby resulting in increased survival of B. anthracis lethal toxin-treated macrophages. Data show that toxin-neutralizing antibody titers were reported as the reciprocal of the dilution that showed ≥30% cellular protection. Interestingly, these results demonstrate that L. acidophilus expressing PA-DCpep elicited high levels of neutralizing anti-PA antibodies in vivo that may have been a critical factor in the protection of those mice against Sterne challenge (Fig. 4B)
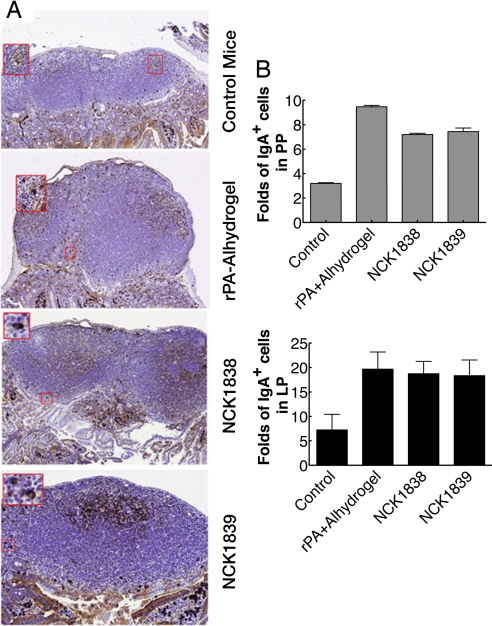
Detection of IgA+ Cells Within Small Intestine.
Immunostaining data of small intestinal sections showed higher expression of IgA+ plasma cells in the LP of villi and PP and occasional cells transmigrating the epithelium from all groups of mice compared with unvaccinated mice (Fig. 5 A and B). Additionally, there was extracellular labeling of secreted IgA in these areas that was especially prominent along the apical surface of some epithelial cells (Fig. 5A).
Fig. 5.
Detection of IgA-expressing cells within the small intestine. (A) After isolation of jejunum and ileum, these tissues were fixed in 10% formalin and processed into paraffin blocks. Serial tissue sections were then mounted on glass slides and IgA-expressing cells were detected with a rabbit anti-mouse IgA polyclonal and visualized with a goat anti-rabbit HRP secondary via scanning electron microscopy. Magnified areas are shown in red squares. (B) IgA+ cells of the lamina propria (LP) of villi and Peyer's patches (PP) were evaluated by a semiautomated quantitative image analysis system. Data are depicted as fold increases of IgA+-expressing plasma cells in LP and PP areas from all mice compared with unvaccinated controls. Data are representative of 3 independent experiments.
Induction of Cytokines.
Cytokines and chemokines released into the peripheral blood of all mice were assayed as described above. Data show that L. acidophilus expressing PA-DCpep orally administrated into mice before challenge induced the up-regulation of IL-10, IL-6, TNFα, and MCP-1 (1.4 ng/mL) whereas L. acidophilus expressing PA-Ctrlpep induced increased levels of only TNFα (Fig. 6A). Furthermore, cytokines in the sera derived from mice that survived challenge by B. anthracis after vaccination with L. acidophilus expressing PA-DCpep showed interesting trends before and after challenge, mainly in the production of IL-12, IL-6, TNFα, and IFNγ (Fig. 6B). Interestingly, IL-10 production was not sustained during the course of the infection in these mice (Fig. 6B). Although the production of IL-6, TNFα, and MCP-1 (43.7 pg/mL) was higher in mice that received L. acidophilus PA-Ctrlpep, IL-12p70, and IFNγ were conversely lower in these mice (Fig. 6B). As seen in Fig. 6B, IL-12p70, IL-6, TNFα, IFNγ, and MCP-1 (25 pg/mL) were induced at low levels in mice vaccinated s.c. with rPA plus alhydrogel; however, it rose significantly after Sterne challenge. Other cytokines such as IL-4 (≤ 0.1 pg/mL), IL-5 (≤ 0.2 pg/mL), and IL-2 (≤ 0.4 pg/mL) were expressed at very low levels in the sera of all vaccinated mice. Furthermore, data show that rPA fusion proteins expressed by L. acidophilus in vivo clearly elicited Th1 immune responses in mice that survived the Sterne challenge (Fig. 6C).
Fig. 6.
Induction of cytokines in vivo. (A and B) Cytokines released into the blood of mice that were bled before (A) and after (B) Sterne challenge were analyzed by using mouse inflammatory and Th1/Th2 cytometric bead array kits. Samples were then analyzed by a FACS CantoII flow cytometer. (C) T cell stimulation. rPA (1 μg/mL) treated and untreated DCs (104 per well) were cultured for 14 h at 37 °C. CD4+/CD8+ T cells (105 per well) derived from mice that survived the B. anthracis Sterne challenge were cocultured with treated and untreated DCs for 5 days. Cell supernatants were harvested and the cytokine release analyzed by a FACS CantoII flow cytometer. Data are representative of 3 experiments.
Discussion
The use of vaccines against infectious diseases has been one of the more profound accomplishments of the medical community (35). To date, there are significant efforts and interest in the development of mucosal vaccines against various microbes and notable pioneering accomplishments using lactic acid bacteria as live vectors for oral delivery (21, 36, 37). Accordingly, one scientific consensus is that the next generation of vaccines should ideally be given orally in single doses. Moreover, such vaccines should be safe, stable, inexpensive, easy to deliver, and induce balanced cellular and efficacious humoral and T cell mediated immune responses against microbial antigens. In this regard, we were able to successfully employ L. acidophilus to deliver targeted fusion proteins that consisted of the B. anthracis protective antigen fused to a short DC-targeting peptide. This oral vaccine candidate activated mucosal antigen-presenting cells (e.g., DCs), which in turn induced anti-PA neutralizing antibodies, IgA secretion, and T cell immunity against B. anthracis. This led to the robust protection of mice against Sterne challenge, whereas PA fused to a control peptide, which does not improve DC binding, showed only minor protection. These data showed that modifying and specifically targeting an antigen to DCs may enhance its uptake by these cells. When combined with Lactobacillus carrier, added adjuvanticity may lead optimal activation of these cells to elicit efficient immune responses against microbial challenge, specifically at mucosal surfaces. Interestingly, although some of the mice that received L. acidophilus expressing PA-Ctrlpep produced high titers of anti-PA antibodies before Sterne challenge, only 4 mice of 16 survived. These data may indicate that a vaccine formulation may require additional immunostimulatory (e.g., TNFα, IL-6, IL-12) and regulatory signals (e.g., IL-10) to elicit an efficient and robust protection against microbes such as B. anthracis. This could be in form of Th1 response (38) along with a regulated inflammation that can mobilize humoral and T cell immune responses against pathogens, as demonstrated in mice that received L. acidophilus expressing PA fused to a DC-binding peptide.
Studies are in progress to further optimize the plasmid vector to enhance the expression of the immunogenic fusions to reduce the high number of orally administered bacteria. We conclude that this highly innovative vaccine strategy provides various beneficial advances, including (i) specific activation of mucosal DCs, (ii) directional elicitation of humoral and T cell-mediated immunity by these cells, and (iii) the delivery system that can serve as a safe and potent adjuvant that induces regulated inflammatory responses within the microenvironment.
Of note, the critical advantage of vaccine delivery via probiotic lactic acid bacteria is in their ability to induce antigen-specific IgA responses in feces, saliva, bronchoalveolar, mesenteric lymph nodes, and the small intestine (6, 37). It was previously shown that some recombinant lactic acid bacteria vaccine candidates induced elevated levels of antigen-specific secretory IgA (6), the predominant Ig class at mucosal surfaces (21). Moreover, one feature of this class of IgA is that it resists proteases rendering these antibodies critical for mucosal immunity. Accordingly, our data clearly show that L. acidophilus expressing PA fusion protein significantly induced IgA in the small intestine, including PP, and LP. In this regard, it was recently demonstrated that the induction of IgA against microbes and foreign immunogens is T cell dependent (39, 40). PA-DCpep delivered by L. acidophilus elicited a Th1 pattern, indicating that efficient T cell-mediated immunity was critical for the induction of IgA within the small intestine. Interestingly, the higher levels of cytokines such as IL-10 induced in mice vaccinated with L. acidophilus expressing PA-DCpep before challenge with B. anthracis Sterne may play a role in concert with IL-4 and TGFβ in the induction of IgA and differentiation of B cells (41, 42). Additionally, IL-10 may have regulated not only the humoral but also the T cell immune responses in vivo, both of which contributed to a better immunological outcome, possibly leading to the protection of the majority of the animals against Sterne challenge. Nonetheless, future studies should determine the levels of these critical cytokines within the PP, and LP villi that may be induced by L. acidophilus expressing the candidate vaccine resulting in IgA secretion. Furthermore, L. acidophilus expressing the targeted PA-DCpep elicited elevated levels of total and neutralizing anti-PA antibodies in surviving mice. Interestingly, the induced level of neutralizing anti-PA antibodies in these mice correlated with increased animal survival, crafting the notion that humoral immune responses are critical for protection.
To date, studies are in progress to identify and characterize the molecular nature of the ligand to which DCpep binds. Our preliminary data show that this receptor can be isolated from DC lysates. Moreover, results indicate that the receptor for DCpep is strongly involved in the endocytotic pathway, allowing faster and more efficient transport of the immunogenic material into the cells without impairing DC functions. Hence, complete characterization of this ligand is now critical and is expected to elucidate important properties of the DC-targeting vaccine strategy that may now be delivered orally and safely via L. acidophilus for inducing protective immunity against B. anthracis and potentially other pathogens.
Materials and Methods
Animals.
A/J mice (age 6–8 weeks) were purchased from the National Cancer Institute (NCI) in Frederick, MD. Mice were housed in clean standard conditions in the animal care facility at the US Army Medical Research Institute of Infectious Diseases (USAMRIID). Research was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations related to animals and experiments involving animals. The principles stated in the Guide for the Care and Use of Laboratory Animals were followed. The research was conducted at USAMRIID, which is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International.
Expression of Recombinant B. anthracis PA-DC Peptide Fusion by L. acidophilus.
To express PA of B. anthracis (43) fused to DC peptide or the control peptide, 2 constructs were made. Each peptide encodes a PA C-terminal fusion to either a DC targeting peptide (FYPSYHSTPQRP) or a control peptide (EPIHPETTFTNN) designated pPAGDC and pPAGctrl, respectively (Fig. 1A). Subsequently, the recombinant PA (rPA) fusion genes were PCR-cloned into expression vector pTRK882, a shuttle vector based on the strong constitutive pgm promoter of L. acidophilus. Plasmids pPAGctrl and pPAGDC containing the PA-control peptide or PA-DC peptide fusions were first constructed. Primers PA-F(5′-ATGCGGATCCCAAAAAGGAGAACGTATATG-3′) and PA-R (5′-GCAATTAACCCTCACTAAAG-3′) were used to amplify the rPA fusion genes for cloning into pTRK882. rPA fusion genes were cloned into the BamHI and NotI sites of pTRK882 yielding pTRK895 and pTRK896. Subsequently, the constructed plasmids were transformed into L. acidophilus NCFM by electroporation (Table 1). Transformants were initially selected by ERM (Sigma) resistance and then screened by plasmid isolation, followed by restriction digestion (Fig. 1 A and B). The plasmids were additionally verified by nucleotide sequencing of the junction points between the vector and inserted DNA.
Western Blot Analyses.
To examine for rPA expression by L. acidophilus, cultures NCK1838 (PA-Control peptide), NCK1839 (PA-DCpeptide), and NCK1895 (empty vector) were grown to midlog phase (O.D. = 0.4–0.6) in MRS broth (Difco) supplemented with ERM, centrifuged, and the cell pellets and supernatants were collected for SDS/PAGE. Cultures of the constitutively expression constructs NCK1838, NCK1839, and NCK1895 were grown to midlog phase in MRS supplemented with ERM (5 μg/mL). Cell pellets were then lysed by bead-beating. Proteins from supernatants were precipitated by using trichloroacetic acid (TCA) and pelleted by centrifugation. The total protein (10 μg) from both supernatants and cell pellets were loaded onto a SDS/PAGE gel. rPA was used as a positive control and NCK1895 containing the empty vector pTRK882 served as a negative control, respectively. After electrophoresis, the proteins were transferred to a nitrocellulose membrane and probed with anti-PA antibody conjugated with HRP. Blots were then washed, treated with 3,3′,5,5′-tetramethyl benzidine (TMB) substrate (KPL), and visualized by a PhosphorImager.
Mouse DC Culture.
Mouse DCs were generated as previously described (44). Briefly, after removing bone marrow cells from mouse femurs, the cells were washed and cultured in complete RPMI medium 1640 plus 10% FCS and 25 ng/mL mouse recombinant GM-CSF at 37 °C. The phenotype of these DCs on day 8 was determined by a FACS CantoII flow cytometer (BD). Mouse DCs were positive for CD11c, CD11b, and MHC II. Subsequently, the endocytotic activity was determined by incubating mouse DCs with Alexa Fluor 647 (Invitrogen) -labeled L. acidophilus strains including NCK1895, NCK1838, and NCK1839 at a ratio of 1:10 for 1 h at 37 °C. As a control, a portion of DCs were incubated with Alexa Fluor 647-labeled L. acidophilus strains on ice. These cells were then washed with cold PBS/0.1% FCS and analyzed by flow cytometry (45).
In Vivo Vaccination.
L. acidophilus strains expressing PA-DCpep, PA-Ctrlpep, and a null vector control were grown at 37 °C in MRS broth supplemented with ERM (5 μg/mL) for 72 h in tightly capped flasks without shaking. Cells were centrifuged and washed twice in PBS before a final resuspension at 109 CFU/250 μL in PBS. Subsequently, groups of mice were orally vaccinated with L. acidophilus NCK 1839 (PA-DCpep), L. acidophilus NCK1838 (PA-Ctrlpep), and L. acidophilus NCK 1895 (empty vector) by gavage of 250 μL containing ≈109 CFU. Vaccination was repeated 3 times on a weekly basis. Two weeks later, the groups of mice were boosted twice. Seven days after the final boost, the mice were i.p. challenged with B. anthracis Sterne pXO1+/pXO2− (5 × 104 CFU per mouse) (46). Survival was monitored until day 40. Additionally, blood was taken from each mouse before and after challenge to determine the levels of anti-PA antibodies, PA-neutralizing antibodies, and cytokines released into the peripheral blood.
Anti-PA Antibody Analysis.
The anti-PA antibody response was measured by ELISA (34, 47). Briefly, microtiter plates were coated with rPA overnight at 4 °C. Plates were then blocked with milk (6%) in PBS. Subsequently, mouse sera were added to wells in 2 log serial dilutions (1:40 to 1:81920) and the plates incubated for 2 h at 37 °C. Plates were washed, and serum antibodies bound to rPA were detected by adding HRP-conjugated goat anti-mouse IgG (BD Biosciences). Plates were then incubated for 1 h at 37 °C. 3,3′,5,5′-Tetramethylbenzidine (TMB) substrate was added and incubated at 37 °C for 5–10 min. Absorbencies were determined at 405 nm after neutralization with 50 μL of hydrochloric acid (1 M).
B. anthracis Toxin-Neutralizing Antibodies.
To determine the levels of neutralizing anti-PA antibodies elicited by L. acidophilus expressing PA-DCpep versus its controls, a toxin-neutralization assay was used (34). This assay was performed to demonstrate that anti-PA antibodies released by peripheral blood immune cells were capable of preventing the association of PA to B. anthracis lethal factor (LF) or the binding of lethal toxin to cell receptors, thereby resulting in increased survival of B. anthracis lethal toxin-treated macrophages. Briefly, serially diluted mouse sera were incubated at 37 °C with B. anthracis lethal toxin (PA 100 ng/mL and LF 20 ng/mL). After 1 h, the mixture was added to J774A.1 macrophages (105 per well) in a 96-well plate. After 4 h incubation at 37 °C, 25 μL of MTT (1 mg/mL) dye was added and the cells were further incubated for 2 h. The reaction was stopped by adding an equal volume of lysis buffer [50% DMF and 20% SDS (pH 7.4)]. Plates were incubated overnight at 4 °C, and the absorbance was read at 570 nm in a multiwell plate reader.
Detection of IgA.
The level of IgA was determined within the small intestine. Briefly, for immunohistological studies, the jejunum and ileum were isolated from mice in each vaccinated group (2 mice per group) for staining of IgA-expressing cells. Subsequently, the tissues were fixed in 10% formalin and processed into paraffin blocks. Serial tissue sections (5-μm thick) were mounted on glass slides and IgA expressing cells were visualized with a rabbit anti-mouse IgA polyclonal antibodies (Zymed Laboratories) and a secondary goat anti-rabbit HRP antibody (DAKO). IgA+ regions of the small intestine, including the LP of villi and PP were evaluated by a semiautomated quantitative image analysis system of the immunohistochemically labeled tissues (ACIS II; DakoCytomation. From digitized images of the stained tissue sections, the percentage of pixels in each tissue that contained the immunostain chromogen was measured and expressed as a percentage of the scanned area (positive pixels/positive + negative pixels). The mean intensity of each chromogen-containing pixel was calculated and expressed as the mean pixel intensity.
Cytokine Analysis.
Cytokines released into the peripheral blood of mice that were bled by tail nick before and after B. anthracis Sterne challenge were analyzed by using mouse inflammatory and Th1/Th2 cytometric bead array kits (BD Biosciences). Briefly, the bead mixture (50 μL) was combined with the mouse sera (50 μL, vol/vol), or standards (50 μL), and phycoerythrin (50 μL). Subsequently, samples were incubated for 2 h at room temperature in the dark. These samples were washed, centrifuged, resuspended in wash buffer (300 μL) and then analyzed by a FACS CantoII flow cytometer (BD). Analysis software (BD CellQuest) allowed for calculation of cytokine values in sera at picogram-per-milliliter amounts.
T Cell Stimulation.
Highly purified, bone marrow-derived DCs were prepared as described above. The rPA-treated, and -untreated, DCs (104 per well) were seeded in round-bottomed microtiter plates and subsequently cultured for 12 h at 37 °C. T cells (105 per well) from mice that survived the B. anthracis Sterne challenge were isolated from mesenteric lymph nodes by using a negative magnetic bead method. These cells were then cocultured with PA-treated or -untreated DCs for 5 days. Afterward, cell supernatants were harvested and cytokine release analyzed by using CBA mouse TH1/TH2 kits on the FACS CantoII flow cytometer (BD).
Supplementary Material
Acknowledgments.
We thank Dr. K. Steele, D. Lane, Dr. R. Panchal, M. Kennedy, and W. Ribot for fruitful discussion and assistance in conducting various experiments related to this project. Work conducted at North Carolina State University was supported by National Institutes of Health Grant R21-AI059590 and the North Carolina Dairy Foundation. T.D. was supported by a National Science Foundation Integrated Graduate Education and Research Traineeship in Functional Genomics.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/cgi/content/full/0900029106/DCSupplemental.
References
- 1.Roberts M, Chatfield S, Pickard D, Li J, Bacon A. Comparison of abilities of Salmonella enterica serovar typhimurium aroA aroD and aroA htrA mutants to act as live vectors. Infect Immun. 2000;68:6041–6043. doi: 10.1128/iai.68.10.6041-6043.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stevenson A, Roberts M. Use of Bordetella bronchiseptica and Bordetella pertussis as live vaccines and vectors for heterologous antigens. FEMS Immunol Med Microbiol. 2003;37:121–128. doi: 10.1016/S0928-8244(03)00068-3. [DOI] [PubMed] [Google Scholar]
- 3.Saklani-Jusforgues H, Fontan E, Soussi N, Milon G, Goossens PL. Enteral immunization with attenuated recombinant Listeria monocytogenes as a live vaccine vector: Organ-dependent dynamics of CD4 T lymphocytes reactive to a Leishmania major tracer epitope. Infect Immun. 2003;71:1083–1090. doi: 10.1128/IAI.71.3.1083-1090.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pouwels PH, et al. Lactic acid bacteria as antigen delivery vehicles for oral immunization purposes. Int J Food Microbiol. 1998;41:155–167. doi: 10.1016/s0168-1605(98)00048-8. [DOI] [PubMed] [Google Scholar]
- 5.Ouwehand AC, Salminen S, Isolauri E. Probiotics: An overview of beneficial effects. Antonie Van Leeuwenhoek. 2002;82:279–289. [PubMed] [Google Scholar]
- 6.Wells JM, Mercenier A. Mucosal delivery of therapeutic and prophylactic molecules using lactic acid bacteria. Nat Rev Microbiol. 2008;6:349–362. doi: 10.1038/nrmicro1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miettinen M, Vuopio-Varkila J, Varkila K. Production of human tumor necrosis factor alpha, interleukin-6, and interleukin-10 is induced by lactic acid bacteria. Infect Immun. 1996;64:5403–5405. doi: 10.1128/iai.64.12.5403-5405.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marin ML, et al. Stimulation of cytokine production in clonal macrophage and T cell models by Streptococcus thermophilus: Comparison with Bifidobacterium sp. and Lactobacillus bulgaricus. J Food Prot. 1998;61:859–864. doi: 10.4315/0362-028x-61.7.859. [DOI] [PubMed] [Google Scholar]
- 9.Christensen HR, Frokiaer H, Pestka JJ. Lactobacilli differentially modulate expression of cytokines and maturation surface markers in murine dendritic cells. J Immunol. 2002;168:171–178. doi: 10.4049/jimmunol.168.1.171. [DOI] [PubMed] [Google Scholar]
- 10.Mohamadzadeh M, et al. Lactobacilli activate human dendritic cells that skew T cells toward T helper 1 polarization. Proc Natl Acad Sci USA. 2005;102:2880–2885. doi: 10.1073/pnas.0500098102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohamadzadeh M, Klaenhammer TR. Probiotics as biotherapeutic agents: Present knowledge and future prospects. Exp Rev Vaccines. 2008;7:1155–1164. [Google Scholar]
- 12.Mercenier A, Pavan S, Pot B. Probiotics as biotherapeutic agents: Present knowledge and future prospects. Curr Pharm Des. 2003;9:175–191. doi: 10.2174/1381612033392224. [DOI] [PubMed] [Google Scholar]
- 13.Kaila M, et al. Enhancement of the circulating antibody secreting cell response in human diarrhea by a human Lactobacillus strain. Pediatr Res. 1992;32:141–144. doi: 10.1203/00006450-199208000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Pamer EG. Immune responses to commensal and environmental microbes. Nat Immunol. 2007;8:1173–1178. doi: 10.1038/ni1526. [DOI] [PubMed] [Google Scholar]
- 15.Tournier JN, Mohamadzadeh M. Microenvironmental impact on lung cell homeostasis and immunity during infection. Exp Rev Vaccines. 2008;7:457–466. doi: 10.1586/14760584.7.4.457. [DOI] [PubMed] [Google Scholar]
- 16.Inglesby TV, et al. Anthrax as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. J Am Med Assoc. 1999;281:1735–1745. doi: 10.1001/jama.281.18.1735. [DOI] [PubMed] [Google Scholar]
- 17.Pannifer AD, et al. Crystal structure of the anthrax lethal factor. Nature. 2001;414:229–233. doi: 10.1038/n35101998. [DOI] [PubMed] [Google Scholar]
- 18.Scobie HM, Rainey GJ, Bradley KA, Young JA. Human capillary morphogenesis protein 2 functions as an anthrax toxin receptor. Proc Natl Acad Sci USA. 2003;100:5170–5174. doi: 10.1073/pnas.0431098100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acheson DW, Luccioli S. Microbial–gut interactions in health and disease. Mucosal immune responses. Best Pract Res Clin Gastroenterol. 2004;18:387–404. doi: 10.1016/j.bpg.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Niedergang F, Kweon MN. New trends in antigen uptake in the gut mucosa. Trends Microbiol. 2005;13:485–490. doi: 10.1016/j.tim.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Holmgren J, et al. Mucosal adjuvants and anti-infection and anti-immunopathology vaccines based on cholera toxin, cholera toxin B subunit and CpG DNA. Immunol Lett. 2005;97:181–188. doi: 10.1016/j.imlet.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Holmgren J, Czerkinsky C. Mucosal immunity and vaccines. Nat Med. 2005;11:S45–S53. doi: 10.1038/nm1213. [DOI] [PubMed] [Google Scholar]
- 23.Rescigno M. Intestinal epithelial cells control dendritic cell function. J Pediatr Gastroenterol Nutr. 2008;46(Suppl 1):E17–E19. doi: 10.1097/01.mpg.0000313831.09089.36. [DOI] [PubMed] [Google Scholar]
- 24.Rescigno M, Matteoli G. Lamina propria dendritic cells: For whom the bell TOLLs? Eur J Immunol. 2008;38:1483–1486. doi: 10.1002/eji.200838435. [DOI] [PubMed] [Google Scholar]
- 25.Kelsall BL, Strober W. The role of dendritic cells in antigen processing in the Peyer's patch. Ann NY Acad Sci. 1996;778:47–54. doi: 10.1111/j.1749-6632.1996.tb21113.x. [DOI] [PubMed] [Google Scholar]
- 26.Kelsall BL, Strober W. Distinct populations of dendritic cells are present in the subepithelial dome and T cell regions of the murine Peyer's patch. J Exp Med. 1996;183:237–247. doi: 10.1084/jem.183.1.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niess JH, et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science. 2005;307:254–258. doi: 10.1126/science.1102901. [DOI] [PubMed] [Google Scholar]
- 28.Niess JH, Reinecker HC. Lamina propria dendritic cells in the physiology and pathology of the gastrointestinal tract. Curr Opin Gastroenterol. 2005;21:687–691. doi: 10.1097/01.mog.0000181710.96904.58. [DOI] [PubMed] [Google Scholar]
- 29.Rescigno MP. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2:361–367. doi: 10.1038/86373. [DOI] [PubMed] [Google Scholar]
- 30.Kraehenbuhl JP, Corbett M. Immunology. Keeping the gut microflora at bay. Science. 2004;303:1624–1625. doi: 10.1126/science.1096222. [DOI] [PubMed] [Google Scholar]
- 31.Macpherson AJ, Uhr T. Induction of protective IgA by intestinal dendritic cells carrying commensal bacteria. Science. 2004;303:1662–1665. doi: 10.1126/science.1091334. [DOI] [PubMed] [Google Scholar]
- 32.Curiel TJ. Targeting mucosal dendritic cells with microbial antigens from probiotic lactic acid bacteria. J Immunol. 2004;172:7425–7431. [Google Scholar]
- 33.Mohamadzadeh M, Duong T, Hoover T, Klaenhammer TR. Targeting mucosal dendritic cells with microbial antigens from probiotic lactic acid bacteria. Exp Rev Vaccines. 2008;7:163–174. doi: 10.1586/14760584.7.2.163. [DOI] [PubMed] [Google Scholar]
- 34.Albrecht MT, et al. Human monoclonal antibodies against anthrax lethal factor and protective antigen act independently to protect against Bacillus anthracis infection and enhance endogenous immunity to anthrax. Infect Immun. 2007;75:5425–5433. doi: 10.1128/IAI.00261-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Plotkin SA. Vaccines: Past, present and future. Nat Med. 2005;11:S5–11. doi: 10.1038/nm1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robinson K. Infect Immun. 2004;72:2753–2761. doi: 10.1128/IAI.72.5.2753-2761.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robinson K, Chamberlain LM, Schofield KM, Wells JM, Le Page RW. Mucosal and cellular immune responses elicited by recombinant Lactococcus lactis strains expressing tetanus toxin fragment C. Nat Biotechnol. 1997;15:653–657. [Google Scholar]
- 38.Glomski IJ, Corre JP, Mock M, Goossens PL. IFN-gamma-producing CD4 T lymphocytes mediate spore-induced immunity to capsulated Bacillus anthracis. J Immunol. 2007;178:2646–2650. doi: 10.4049/jimmunol.178.5.2646. [DOI] [PubMed] [Google Scholar]
- 39.Lycke N, Eriksen L, Holmgren J. Protection against cholera toxin after oral immunization is thymus-dependent and associated with intestinal production of neutralizing IgA antitoxin. Scand J Immunol. 1987;25:413–419. doi: 10.1111/j.1365-3083.1987.tb02208.x. [DOI] [PubMed] [Google Scholar]
- 40.Hornquist CE, Ekman L, Grdic KD, Schon K, Lycke NY. Paradoxical IgA immunity in CD4-deficient mice. Lack of cholera toxin-specific protective immunity despite normal gut mucosal IgA differentiation. J Immunol. 1995;155:2877–2887. [PubMed] [Google Scholar]
- 41.Goodrich ME, McGee DW. Regulation of mucosal B cell immunoglobulin secretion by intestinal epithelial cell-derived cytokines. Cytokine. 1998;10:948–955. doi: 10.1006/cyto.1998.0385. [DOI] [PubMed] [Google Scholar]
- 42.Asano T. Molecular analysis of B-cell differentiation in selective or partial IgA deficiency. Clin Exp Immunol. 2004;136:284–290. doi: 10.1111/j.1365-2249.2004.02440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ivins BE, Welkos SL. Cloning and expression of the Bacillus anthracis protective antigen gene in Bacillus subtilis. Infect Immun. 1986;54:537–542. doi: 10.1128/iai.54.2.537-542.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pulendran B. Dendritic cells generated in the presence of GM-CSF plus IL-15 prime potent CD8+ Tc1 responses in vivo. Eur J Immunol. 2004;34:66–73. doi: 10.1002/eji.200324567. [DOI] [PubMed] [Google Scholar]
- 45.Mohamadzadeh M. Interleukin 15 skews monocyte differentiation into dendritic cells with features of Langerhans cells. J Exp Med. 2001;194:1013–1020. doi: 10.1084/jem.194.7.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect Immun. 1986;51:795–800. doi: 10.1128/iai.51.3.795-800.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zegers ND. Expression of the protective antigen of Bacillus anthracis by Lactobacillus casei: Towards the development of an oral vaccine against anthrax. J Appl Microbiol. 1999;87:309–314. doi: 10.1046/j.1365-2672.1999.00900.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.