Abstract
Background
In the otherwise atheoretical diagnostic manual, the DSM-III and IV bereavement exclusion for the diagnosis of major depression (MDD) stands out as the sole exception to the rule. No other life event excludes the diagnosis of any other axis I disorder. Since this diagnostic convention has important diagnostic and treatment implications, it is important to evaluate the validity of this exception. By comparing multiple features of bereavement related to non-bereavement related MDD, this prospective community study critically evaluates the validity of the bereavement exclusion
Results
The prevalence of conditional criteria was common in the total sample (N=685) and did not differ between bereaved and non-bereaved groups. The global ‘symptom profile’ of depressed individuals was similar in both groups. ‘Duration’ was found to be longer in the bereaved group. Among all conditional criteria required by DSM-IV to accept bereavement related episodes under the category of MDD, only ‘marked dysfunction’ predicted treatment. Neither the ‘four conditional symptoms’ nor the ‘duration’ criterion predicted marked dysfunction. The ‘risk for recurrence’ was similar whether the first episode was bereavement related or not.
Limitations
‘Psychotic symptoms’ were not assessed, and ‘marked dysfunction’ was not assessed on a continuous scale. The number of DSM-IV excluded episodes was too small to allow for generalization.
Conclusion
Our results suggest that the conditional criteria do not seem to serve the purpose of the originators of the bereavement exclusion criteria. The ‘conditional symptoms’ and the ‘duration’ criterion seem not to be markers of severity. We propose that the descriptive and etiologically neutral approach the DSM presumes in reaching a diagnosis should be applied in the case of MDD until more convincing data point to the contrary.
Keywords: bereavement, depression, conditional criteria, DSM
Introduction
One of the assets of the Diagnostic and Statistics Manual (DSM) (APA, 1994) is its purely descriptive approach to defining diagnoses. This approach has helped practitioners bypass the yet unresolved issues of causality in most psychiatric disorders. In this context, major depression, if not “due” to a medical illness, is diagnosed irrespective of its possible etiology. Accordingly, the diagnosis of a major depressive episode is not put in question if there is a potential (perceived or probable) precipitant. Yet, one chief exception to this a-theoretical approach is the restriction imposed on bereavement-related depressions.
In essence, the DSM-IV requires that a diagnosis of major depression cannot be established after the death of a loved one unless the depression criteria are met for at least two months (instead of the normally required two weeks), that these regular criteria include specifically psychomotor retardation, morbid preoccupation with worthlessness, suicidal ideation or attempts, or psychotic features, or that the depressive episode is associated with marked functional impairment (APA, 1994). Thus, in the current DSM diagnostic system, a bereavement-related depressive syndrome has to be either of longer duration, be paired with specific symptomatic manifestations, or be more impairing than when precipitated by an emotional break-up, loss of money or exposure to other potential traumata, to deserve the appellation of major depression. This exclusion of bereavement-related depressive episodes from the inventory of the DSM classification of major depression is in clear contradiction with the descriptive and etiologically neutral approach that the DSM follows in reaching a diagnosis.
Several investigators (Clayton, 1990; Brent et al., 1992, 1993; Futterman et al., 1990; Harlow et al., 1991; Zisook and & Schuchter, 1991) have documented high prevalence of major depressive episodes among widows and widowers. Although bereavement, as a single precipitant, is a well established risk factor to the onset of major depressive syndromes (Bornstein et al., 1973; Clayton et al., 1972; Clayton, 1979, 1998; Futterman et al., 1990; Harlow et al., 1991; Van Eerdewegh et al., 1982; Zisook and Schuchter, 1991), yet it remains the only life event that impedes the diagnosis of major depression in the current DSM system.
Several researchers (Brent et al., 1993, 1994a; Brent, 1994b; Karam, 1994; Weller et al., 1991; Zisook and Schuchter, 1991, 1993; Zisook et al., 1994, 1997, 1998, and 2007b; Zisook and Kendler 2007a) have argued against maintaining bereavement as an exclusion criterion. Others (Prigerson et al., 1994, 1995, 1996; Zisook & Schuchter, 1993; Zisook et al., 1997, 1998) have explored bereavement-related disorders in the guise of complicated grief that evolved to traumatic grief, post traumatic stress disorder (PTSD) or depression. Horowitz et al. (1997) and Prigerson et al. (1996, 1999) argued for bereavement to constitute a ‘pathological grief’ category, distinct and independent from depression in the DSM (APA, 1987). They stipulated that pathology is common after bereavement, but should be classified in the DSM as complicated grief disorder (CGD). Prigerson et al. (1999) further proposed diagnostic criteria for ‘traumatic grief’ which evolved from the concept and criteria of CGD (Horowitz et al. 1997) to include symptoms such as intrusive thoughts, yearning and searching for the deceased.
On the other hand, Karam (1994) contended that although bereavement-related depression includes clear ideation related to the deceased, this should not necessarily exclude it from the repertoire of depression. Otherwise, and by the same token, since many situation-specific stressors exist, a plethora of related depressions would have to be each classified according to their respective precipitants depending on the ideation and preoccupation with the perceived precipitant. Thus, one could imagine having: complicated divorce disorder, complicated loss of job disorder, etc, whereby each disorder has its own specific cluster of ideations.
The DSM’s additional requirements/criteria for the inclusion of bereavement precipitated depressions in the registry of major depression seem not to have an empirical basis, and to the current authors’ knowledge (personal communication with authors from the DSM-IV task force) are linked to a series of articles by Paula Clayton. In these studies (Clayton et al. 1972; 1979; Bornstein et al. 1973), a sample of bereaved spouses were selected from newspaper obituaries and death certificate records, and interviewed within 30 days of the death of their spouses, and were followed four and thirteen months later. The prevalence of bereavement-related depressions was significantly high at one month (35%), decreased to 25% at 4 months and to 17% at 13 months. However, this drop in the prevalence should not serve to advocate the exclusion of bereavement-related depression from the DSM-IV major depression category, knowing that there is a consensus in the psychiatric literature that the course of most DSM-IV depressions are vastly expected to resolve within a period of six months (Coryell et al., 1994).
In questioning the nature and validity of the exclusion criteria set in the DSM-IV for bereavement-related depression, results from Brent et al.’s (1994 a) follow-up study of bereaved older adolescents showed that depressive episodes, following or predating bereavement, displayed a similar clinical profile that was different from the non-depressed bereaved with regards to worthlessness, psychomotor retardation, suicidal ideation and psychotic features. The criterion of dysfunction was studied by Clayton (1974) by assessing the frequency of consultation and hospitalization in a sample of bereaved spouses. Although there were no differences between bereaved and controls in rates of consultation and hospitalization, the bereaved group did have a higher frequency of depressive symptoms. As for the duration criterion, Zisook and Shuchter (1993) found that the duration longer than 2 months and the conditional symptoms are not uncommon among widows and widowers following the death of a spouse.
This paper seeks to question specifically the validity of the DSM-IV exclusion/inclusion criteria by investigating prevalence, symptom profile, duration, marked dysfunction, treatment seeking and recurrence of bereavement and non-bereavement related depressions. If the symptom profiles, duration, rate of marked dysfunction, treatment-seeking and course are dissimilar, perhaps the bereavement-exclusion is valid; if they are similar in the two groups of depressed individuals, it may be time to re-think the wisdom of continuing the bereavement exclusion into DSM-V.
Methods
Design and Objective
A prospective study was conducted in two phases: Phase I (1989) and Phase II (1991). This study was initially designed to look at the immediate and long-term effects of war on the mental health of adults in Lebanon (Karam et al., 1998). Data from this larger study were analyzed with the specific goal of looking at the issue of bereavement-related depressions and more specifically at the validity of excluding them unless they met specific conditional criteria. We studied all conditional symptoms except for psychotic symptoms, which were not assessed by our instrument. We also looked at the other two conditional criteria (duration and dysfunction); however, our data only included information about marked dysfunction as present or absent, and was not assessed on a continuum from mild to marked. This limitation was addressed by looking at different types of episodes as explained in the analysis section below.
Sample
Clusters were randomly chosen from four different regions in Lebanon differentially exposed to war. From these clusters, households were selected using the random digit method. All residents aged 18–65 years were separately interviewed. Six hundred fifty eight respondents were initially interviewed in Phase I. For the purpose of this study, only depressed respondents were looked at: 193 respondents from Phase I (365 episodes) and the selected inhabitants of the two most exposed regions were followed in Phase II (N=206) with 78 respondents (a total of 163 episodes in Phase I), having had at least one episode of depression in Phase I. A detailed description of the methodology can be found elsewhere (Karam, 1992; Karam, 1994).
Instruments
The Arabic version of the Diagnostic Interview Schedule (DIS), adapted by our group, (Karam et al., 1991) was used in both Phases I and II. The DIS was based on the DSM-III-R criteria for diagnosis (APA, 1987). In addition to the traditional DIS structure, we inquired about the date of onset, number of symptoms, duration, bereavement status, dysfunction and employment history of each depressive episode. War exposure was measured using the War Events Questionnaire (developed by IDRAAC) to collect information on war exposure. Numerical weights were assigned to the witnessing of war events. A summary measure was calculated taking into account these weights (total war score) (Karam et al., 1999). All interviews were conducted in the homes of the respondents by clinical psychologists who had thorough training in the use of these instruments.
Analysis
Several analyses were conducted. All episodes needed to have at least the required 5 symptoms and last for at least 2 weeks. Dysfunction as a requirement is analyzed separately. This was done since dysfunction could theoretically affect the multiple comparisons we planned to carry; in addition we had a single question on dysfunction (Q: Did you have marked dysfunction; A: Yes/No) and, thus, without a severity scale for dysfunction, comparisons could be misleading.
We first assessed the frequency of the individual depressive symptoms from Phase I episodes.
-
In the second set of analyses, we compared the profiles of bereavement-related to those of non-bereavement-related depressive episodes (of Phase I), with respect to the frequency of the conditional criteria and frequency of treatment, on four different subsets of episodes of depression.
“All episodes” refer to all episodes of Depression regardless of the presence or absence of conditional symptoms, dysfunction, and duration (but at least 2 weeks).
“Short duration episodes” refer to episodes of Depression that last less than 8 weeks (but more than 2 weeks).
“PWS-free episodes” refer to episodes of Depression that do not endorse any of the conditional symptoms (Psychomotor retardation, Worthlessness, and Suicidal ideas or attempts).
“The DSM-Excluded Episodes” refer only to the episodes of Depression that do not endorse the conditional symptoms and last less than 8 weeks (but more than 2 weeks)
In the third analysis, we looked more closely at treatment seeking behavior. We assessed the predictive power of all the conditional criteria (conditional symptoms, duration and marked dysfunction) with respect to treatment for both bereavement-related and non-bereavement related depressions of Phase I.
In the fourth analysis we looked at the age of onset and exposure to war of respondents whose first depression episode was bereavement-related versus those whose first episode was non-bereavement-related. Exposure to war was assessed through a total war score which was not normally distributed and thus logarithmic transformation was used.
In the last analyses we explored the prognosis of respondents whose first depressive episode was bereavement-related versus those whose first episode was non-bereavement-related, with respect to rates of recurrence within Phase I (1989) and prospectively from Phase I to Phase II (1990).
Chi-squares and t-tests were used to test for the difference between bereavement-related and non-bereavement-related episodes. Tests of significance were set at alpha = 0.05.
Results
Prevalence of all conditional criteria in the total sample
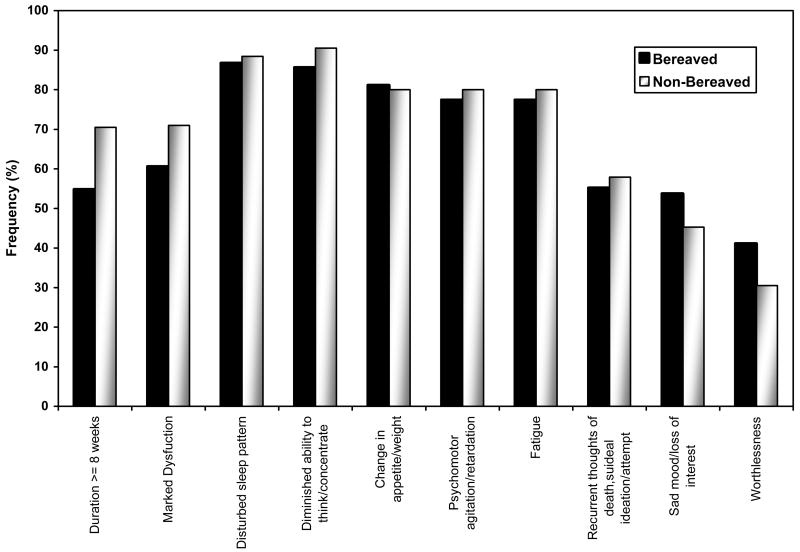
Our results showed that the conditional criteria: conditional symptoms (psychomotor retardation, worthlessness, suicidal thoughts/attempts), duration of more than 8 weeks or marked dysfunction, were quite common among depressive episodes (Figure 1).
Figure 1.
Frequency of symptoms, duration and dysfunction in the bereaved and non-bereaved sub-groups (number of episodes =365).
Comparing bereavement related to non-bereavement related groups
All episodes
The total number of depressive episodes in Phase I was 365 with 95 episodes related to bereavement. There were no significant differences in the prevalence of conditional symptoms, in dysfunction or treatment between the bereaved and non-bereaved groups. The only difference was found for the duration criterion (Table 1): a higher percentage of the bereavement-related episodes had a duration longer than 8 weeks.
Table 1.
Frequency of conditional criteria, treatment, and marked dysfunction in bereavement-related and non-bereavement-related depressive episodes
| Episodes | ||||||||
|---|---|---|---|---|---|---|---|---|
| All a | Shorter duration b | PWS-free c | Restricted d | |||||
| Bereavement Status* | Bereaved | Non Bereaved | Bereaved | Non Bereaved | Bereaved | Non Bereaved | Bereaved | Non Bereaved |
| N | 95 | 270 | 28 | 122 | 34 | 78 | 12 | 35 |
| Psychomotor retardation (P) | 46 (48%) | 116 (43%) | 11 (39%) | 49 (40%) | - | - | - | - |
| Worthlessness (W) | 29 (30%) | 111 (41%) | 12 (43%) | 55 (45%) | - | - | - | - |
| Suicidal ideas/attempts (S) ** | 8 (8%) | 32 (12%) | 1 (4%) | 6(5%) | - | - | - | - |
| P or W or S | 61 (64%) | 192 (71%) | 16 (57%) | 86 (70%) | - | - | - | - |
| Duration ≥ 8 weeks (D) | 67 (71%) * | 148 (55%) | - | - | 22 (65%) | 42 (54%) | - | - |
| P or W or S or D | 83 (87%) | 234 (87%) | - | - | - | - | - | - |
| Treatment | 28 (30%) | 82 (30%) | 5 (18%) | 35 (29%) | 10 (30%) | 16 (21%) | 1(8%) | 10 (29%) |
| Marked Dysfunction | 66 (71%) | 163 (61%) | 19 (68%) | 65 (54%) | 23 (70%) | 39 (51%) | 9 (75%) | 19 (54%) |
Significant difference at 5% confidence level
Rates of suicidal attempts for non-bereavement and bereavement are 5.2% and 4.2% respectively for all episodes; and 2.5% and 3.6% respectively for episodes with duration of less than 8 weeks.
All depressive episode
Depressive episode status < than 8 weeks but larger then 2 weeks
Depressive episode that have no psychomotor retardation, no worthlessness and no suicidal ideation attempt
Depressive episode that have no psychomotor retardation, no worthlessness and no suicidal ideation attempt and episode <8 weeks but > 2 weeks
Short duration episodes
There were 122 non-bereavement-related episodes and 28 bereavement-related episodes that had a duration of less than eight weeks. There was no significant difference between the two groups with respect to the prevalence of the conditional (symptoms, duration), marked dysfunction and treatment.
PWS-free episodes
There were 78 non-bereavement-related episodes and 34 bereavement-related episodes that did not endorse any of the conditional symptoms. No significant differences were found in terms of duration, marked dysfunction and treatment.
DSM-excluded episodes
There were 35 non-bereavement-related episodes (data about treatment and dysfunction was missing in one episode) and 12 bereavement-related episodes in this category. Again there were no significant differences between the non-bereavement-related and bereavement-related groups with regards to marked dysfunction and treatment.
Predictors of treatment
A logistic regression model was run to explore the predictors of treatment. Neither the four conditional symptoms nor duration predicted treatment in the total sample, in the non-bereavement-related or in the bereavement-related subgroups. Marked dysfunction on the other hand was the only variable that predicted treatment for the total and non-bereavement-related samples, but not in the bereavement-related sample (Table 2). Bereavement status did not predict treatment. Further analysis (available upon request) indicated that none of the other conditional symptoms predicted marked dysfunction.
Table 2.
Predictors of treatment
| Conditional Symptomsa | Durationb | Dysfunctionc | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Total sampled | 1.5 (0.9–2.5) | 0.1 | 1.2 (0.7–1.9) | 0.5 | 3.3 (1.9–5.6) | <0.0005 |
| Bereavement | 0.9 (0.3–2.3) | 0.9 | 2.5 (0.8–7.7) | 0.1 | 2.3 (0.8–7.1) | 0.1 |
| Non-bereavement | 1.8 (0.9–3.4) | 0.09 | 1.0 (0.6–1.7) | 0.9 | 3.7 (2.0–6.8) | <0.0005 |
Reference is episode with none of the four conditional symptoms (Psychomotor retardation, worthlessness, suicidal ideas and suicidal attempts).
Reference is episode with duration < 8 weeks but > 2 weeks
Reference is episodes with no dysfunction
Whole sample with a variable of at least one of the four symptoms, 8≥weeks & dysfunction.
Recurrence, age of onset and exposure to war
To test for recurrence, subjects were divided into two groups: those whose first episode was not attributed to bereavement (group NB) and those whose first episode was (group B).
All subjects
In Phase I there were 136 respondents in group NB and 57 in group B. There were no significant differences in age of onset (26.7±11.7 versus 29.2±12.0, p= 0.18), in intensity of war exposure (3.5±1.1 versus 3.5±1.2, p= 0.98) or the risk of recurrence neither in Phase I nor in the prospective follow-up between the two groups (Table 3). Fifty-one respondents from the group NB and 27 of the group B were followed up in Phase II. There was no statistical difference with respect to recurrence in this phase between the two categories (Table 4).
Table 3.
Prognosis/course of bereavement-related and non-bereavement first depressive episode
| Conditional criteria | Episodes | |||||||
|---|---|---|---|---|---|---|---|---|
| All a | Short Duration b | PSW free c | Restricted d | |||||
| Bereavement | Bereaved | Non Bereaved | Bereaved | Non Bereaved | Bereaved | Non Bereaved | Bereaved | Non Bereaved |
| N | 57 | 136 | 18 | 58 | 24 | 35 | 8 | 13 |
| At least one recurrence | 70% | 66% | 78% | 62% | 67% | 69% | 88% | 71% |
| Age of Onset†† | 29.2(12.0) | 26.7(11.7) | 27.0 (11.6) | 26.2(13.3) | 30.1(11.3) | 31.4(15.0) | 23.4(7.8) | 31.0(17.0) |
| Exposure to war†† | 3.5(1.2) | 3.5(1.1) | 3.7 (1.1) | 3.4(1.1) | 3.3(1.2) | 3.6(0.9) | 3.6(0.9) | 3.6(1.1) |
Mean (±SD)
All depressive episode
Depressive episode status < than 8 weeks but larger then 2 weeks
Depressive episode that have no psychomotor retardation, no worthlessness and no suicidal ideation attempt
Depressive episode that have no psychomotor retardation, no worthlessness and no suicidal ideation attempt and episode <8 weeks but > 2 weeks
Table 4.
Recurrence in Phase II in bereavement and non-bereavement related groups
| All First Episodes |
|||||||
|---|---|---|---|---|---|---|---|
| Not Bereaved | Bereaved | P-value | |||||
| N | n | (%) | N | n | (%) | ||
| All Subjects | 51 | 31 | (60.8%) | 27 | 17 | (63.0%) | NS |
| PWS-free subjects a | 15 | 07 | (46.7%) | 09 | 04 | (44.4%) | NS |
| Shorter duration subjects b | 13 | 06 | (46.2%) | 08 | 02 | (25.0%) | NS |
| Restricted Subjects c | 05 | 03 | (60.0%) | 05 | 02 | (40.0%) | NS |
Subjects whose all phase I episodes were free from any of the “four symptoms”.
Subjects whose all phase I episodes were <8 weeks each
Subjects whose all phase I episodes were <8 weeks each & free from any of the “four symptoms”.
Short duration subjects
There were 58 respondents in group NB and 18 in group B whose first episode lasted less than 8 weeks (but more than 2 weeks). No significant differences were found between the two groups with respect to age of onset (26.2±13.3 versus 27.0±11.6, p= 0.82), exposure to war (3.4±1.1 versus 3.7±1.1, p= 0.46) or having a recurrence in Phase I. In additional analysis (not shown) there were 13 NB and 8 B respondents whose all depressive episodes in Phase I lasted less than 8 weeks: No significant difference in recurrence in Phase II between these two subgroups (Tables 3& 4).
PWS-free subjects
There were 35 respondents in group NB and 24 in group B whose first episode did not include any of the conditional symptoms. No significant differences were found between the two groups with respect to age of onset of depression (31.4±15.0 versus 30.1±11.3, p= 0.72), exposure to war (3.6±0.9 versus 3.3±1.2, p= 0.37) or the risk of recurrence in either Phases I or II. Furthermore when only subjects whose all episodes in Phase I were PWS free were considered, no significant difference were found in the recurrence rates of the 15 NB vs. 9 B subjects in Phase II (Tables 3 & 4).
DSM-excluded episodes
There were 13 respondents in group NB and 8 in group B whose first episode was “excluded”. Again no differences were found between the two groups with respect to age of onset (31.0±17.0 versus 23.4±7.8, p= 0.25), exposure to war (3.6±1.1 versus 3.6±0.9, p= 0.98) or having a recurrence in Phases I or II (Tables 3 & 4). We looked too at the subset of respondents from both groups (NB and B) who did not meet any of the exclusion criteria in all their episodes in Phase I: Again no significant difference was found between these two groups (NB and B) with respect to having a new episode in Phase II (results not shown).
Discussion
This study aimed at questioning the validity of excluding bereavement-related depressions from the repertoire of major depression in the DSM-IV, unless they meet one of the specific conditional criteria (psychomotor retardation, worthlessness, suicidality, psychotic symptoms, marked dysfunction, or a duration of more than two months) (APA, 1994); the underlying assumption being these conditional criteria would narrow down the number of bereavement-related depressions that would qualify for the diagnosis of major depression and thus warrant clinical attention and treatment. The conditional criteria would consequently select fewer cases but at the same time the more severe ones.
Our study looked empirically at the frequency of the conditional symptoms and have shown that, in fact, they are common among depressed individuals (meeting at least any five criteria for at least two weeks, we did not look at psychotic symptoms) whether their depression is related to bereavement or not. Marked dysfunction was common too among bereavement related depressions; an exception was found in the duration criterion, where bereavement-related depressions had longer duration (more than two months) than non-bereavement depressive episodes. So if the purpose of including the conditional criteria is to reduce the number of diagnosed depressions related to bereavement, then the criterion of at least two months duration does not really serve this purpose. Moreover, regardless of the duration (more or less than eight weeks) the conditional symptoms and marked dysfunction occurred as frequently whether the depressive episodes were bereavement-related or not. Conversely, the duration of the episodes that did not endorse any of the conditional symptoms or marked dysfunction were not different between bereavement-related and non-bereavement-related subgroups.
On the other hand, among the conditional criteria, only marked dysfunction predicted treatment seeking behavior, but the rates of marked dysfunction were in fact similar for the bereavement-related and the non-bereavement-related groups. None of the conditional symptoms predicted marked dysfunction nor treatment.
It is worth noting here that in the DSM-excluded episodes (not meeting any conditional criteria), both bereavement-related and non-bereavement-related groups seek treatment equally. The issue remains however whether and how dysfunction should continue to be an essential part of the diagnosis in general, which is already a matter of debate (Sartorius, 2007). Our objection is at the heart of another ongoing debate of future DSM classifications and beyond the goal of this article. It is possible that regulators may decide that only depressions accompanied by dysfunction or marked dysfunction would warrant specific types of clinical attention and treatment or disability benefits, and thus a dimensional approach would clearly offer a solution. We mentioned this here as a possible solution for the dilemma facing the DSM regulations.
Since depressive disorders are among the most commonly occurring health problems in the World and Lebanon (Karam et al., 2006; WHO-WMH, 2004), the importance of identifying “true” depressive episodes as such not only lies in the issue of dysfunction and its relation to treatment but also in the prognosis of the individuals that suffer from depression and the consequent burden. The prospective design of this study allowed for the follow-up of a group of bereaved and non-bereaved respondents, who met at least 5 DSM-IV criteria for major depression; none of which met the duration criteria of at least 8 weeks nor any of the conditional symptoms. No differences were found in the risk of recurrence, and the bereaved and non-bereaved individuals seem to have similar prognosis when meeting any five DSM-IV criteria of depression for at least two weeks, even if none of the criteria met are conditional. This finding further points out to the uncertainty of considering specific symptoms as conditional to the diagnosis of major depression in cases where bereavement is presumed to be the precipitant. It is worth noting here that, surprisingly, “Guilt” is mentioned among the conditional symptoms in the DSM IV “Bereavement” section (p. 684 only), but not in the “Major Depression” section (p. 339). It would be interesting to see whether guilt has or not a particular impact on the course of bereavement related depressions.
One interesting aspect about our sample is that it is a homogeneous group of adults with comparable demographic variables, living in the same areas of Lebanon, who were all assessed during the same period of time and have been subjected to similar stressful war events. The log-war scores of the bereavement-related and non-bereavement-related samples as calculated through the War Event Questionnaire (Karam et al., 1999) were indeed comparable in both groups.
In a recent article, Wakefield et al (2007) attempted to argue that the bereavement exclusion for a major depression should be extended to other losses. The authors demonstrated how similar were bereavement-related and other-loss-related depressive episodes of equal severity: they found that “uncomplicated” episodes did not differ in demographic variables and clinical indicators, regardless of whether they were bereavement triggered or other loss-triggered. Similarly, “complicated episodes” were also comparable in both bereaved and other loss triggered group.
Despite these interesting findings, it is important to mention the limitations encountered in this study. First, marked dysfunction was assessed as present or absent and not on a continuous scale that would have allowed to define a sub-sample of episodes with marked dysfunction among depressed dysfunctional individuals. We tried to get around that limitation by defining four types of episodes (“All” “DSM-excluded episodes” “PWS free” and “Short”), analyzing dysfunction each time closely. Second, some analyses were done on small samples (the sample of “restricted episodes” and the sample of respondents that were studied prospectively for the risk of recurrence), therefore some of the findings cannot be generalized before being replicated. Third, psychotic symptoms were not assessed in our data, which could potentially be a missing variable. Fourth, is the age of sample, as many bereavement-related depressions may occur in individuals older than age 65 years. Another limitation is that bereavement-related episodes occurred less frequently, as expected, at peacetime. One could argue that the study was carried out in non-western cultures, yet our experience through collaborative work using same instruments with US and European centers point to similar presentation of Depression in Lebanon (Karam et al 2006; 2008).
Nevertheless, despite the limitations, it remains that one of the strengths worth mentioning is that this study was undertaken in the normal milieu and not through referrals or a clinic. The findings of this study do not support the validity of the DSM-IV conditional criteria for bereavement-related depressions. On the contrary, they highlight the similarity between bereavement-related depressions and all others. This is seen in terms of their symptom profile (including the conditional symptoms), their natural course (recurrence), their marked dysfunction and their treatment seeking behavior. However, further research is needed to confirm that all the conditional criteria are indeed markers of severity. This does not mean that all depressions look the same independently of genetics, precipitants, cultures, age, gender etc. (Cerel et al., 2006), but the assertion made in an earlier publication (Karam, 1994) holds true today: we need to reevaluate the appropriateness of the bereavement exclusion criteria.
The current study presents a paradigm that has yet to be explored against a proper control. Future research with larger samples is very much needed to answer once and for all the upcoming DSM-V’s very important question of bereavement-related depressions with solid, updated and empirically based data.
Footnotes
Author Disclosure
Acknowledgements: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3,Revised. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4, Revised. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Bornstein PE, Clayton PJ, Halikas A, Maurice WL, Robins E. The depression of widowhood after thirteen months. Br J Psychiatry. 1973;122:561–566. doi: 10.1192/bjp.122.5.561. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz GM, Allman C, Friend A, Schweers J, Roth C, Balach L, Harrington K. Psychiatric effects of exposure to suicide among the friends and acquaintances of adolescent suicide victims. J Am Acad Child Adolesc Psychiatry. 1992;31(4):629–639. doi: 10.1097/00004583-199207000-00009. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz GM, Allman C, Liotus L, Schweers J, Roth C, Balach L, Canobbio R. Bereavement or Depression? The Impact of the Loss of a Friend to Suicide. J Am Acad Child Adolesc Psychiatry. 1993;32(6):1189–1197. doi: 10.1097/00004583-199311000-00012. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz GM, Liotus L, Schweers J, Canobbio R. Major depression or uncomplicated bereavement? A follow-up of youth exposed to suicide. J Am Acad Child Adolesc Psychiatry. 1994a;33(2):231–239. doi: 10.1097/00004583-199402000-00012. [DOI] [PubMed] [Google Scholar]
- Brent DA. Resolved: Several Weeks of Depressive Symptoms after Exposure to a Friend’s Suicide is ‘Major Depressive Disorder’. Journal J Am Acad Child Adolesc Psychiatry. 1994b;33(4):582–587. doi: 10.1097/00004583-199405000-00017. [DOI] [PubMed] [Google Scholar]
- Cerel J, Fristad MA, Verducci J, Weller RA, Weller EB. Childhood bereavement: Psychopathology in the 2 years post parental death. J Am Acad Child Adolesc Psychiatry. 2006;45(6):681–689. doi: 10.1097/01.chi.0000215327.58799.05. [DOI] [PubMed] [Google Scholar]
- Clayton PJ, Halikas JA, Maurice WL. The depression of widowhood. Br J Psychiatry. 1972;120:71–78. doi: 10.1192/bjp.120.554.71. [DOI] [PubMed] [Google Scholar]
- Clayton PJ. Mortality and morbidity in the first year of widowhood. Arch Gen Psychiatry. 1974;30:747–750. doi: 10.1001/archpsyc.1974.01760120013002. [DOI] [PubMed] [Google Scholar]
- Clayton PJ. The sequelae and nonsequelae of conjugal bereavement. Am J Psychiatry. 1979;136(12):1530–1534. doi: 10.1176/ajp.136.12.1530. [DOI] [PubMed] [Google Scholar]
- Clayton PJ. Bereavement and depression. J Clin Psychiatry. 1990;51(suppl):34–38. [PubMed] [Google Scholar]
- Clayton PJ. The model of stress: The bereavement reaction. In: Dohrenwend BP, editor. Adversity, Stress, and Psychopathology. Oxford University Press; New York, NY: 1998. pp. 96–110. [Google Scholar]
- Coryell W, Akiskal H, Leon AC, Winokur G, Maser JD, Mueller TI, Keller MB. The time course of nonchronic major depressive disorder. Uniformity across episodes and samples. NIMH Collaborative Program on the Psychobiology of Depression-Clinical Studies. Arch Gen Psychiatry. 1994;51(5):405–410. doi: 10.1001/archpsyc.1994.03950050065007. [DOI] [PubMed] [Google Scholar]
- Futterman A, Gallagher D, Thompson LW, Lovett S, Gilewski M. Retrospective assessment of marital adjustment and depression during the first two years of spousal bereavement. Psychol Aging. 1990;5(2):277–283. doi: 10.1037//0882-7974.5.2.277. [DOI] [PubMed] [Google Scholar]
- Harlow SD, Goldberg EL, Corntock GW. A longitudinal study of the prevalence of depressive symptomatology in elderly widowed and married women. Arch Gen Psychiatry. 1991;48(12):1065–1068. doi: 10.1001/archpsyc.1991.01810360029004. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ, Siegel B, Holen A, Bonanno GA, Milbrath C, Stinson CH. Diagnostic criteria for complicated grief disorder. Am J Psychiatry. 1997;154(7):904–910. doi: 10.1176/ajp.154.7.904. [DOI] [PubMed] [Google Scholar]
- Karam EG, Barakeh M, Nasser Karam A, El-Khoury N. The Arabic Diagnostic Interview Schedule DIS. Revue Médicale Libanaise. 1991;3:28–30. [Google Scholar]
- Karam EG. Annales de Psychologie et des Sciences de l’Education. Université St. Joseph; Beyrouth: 1992. Depression et guerres du liban. Methodologie d’une recherche; pp. 99–106. [Google Scholar]
- Karam EG. The nosological status of bereavement-related depressions. Br J Psychiatry. 1994;165:48–52. doi: 10.1192/bjp.165.1.48. [DOI] [PubMed] [Google Scholar]
- Karam EG, Howard D, Karam A, Ashkar A, Shaaya M, El-Khoury N. Major depression and external stressors: The Lebanon wars. Eur Arch Psychiatry Clin Neurosci. 1998;248:225–230. doi: 10.1007/s004060050042. [DOI] [PubMed] [Google Scholar]
- Karam EG, Al-Atrash R, Saliba S, Melhem N, Howard D. The war events questionnaire. Soc Psychiatry Psychiatr Epidemiol. 1999;34(5):265–274. doi: 10.1007/s001270050143. [DOI] [PubMed] [Google Scholar]
- Karam EG, Mneimneh ZN, Karam AN, Fayyad JA, Nasser SC, Chatterji S, Kessler RC. Prevalence and treatment of mental disorders in Lebanon: a national epidemiological survey. Lancet. 2006;367:1000–1006. doi: 10.1016/S0140-6736(06)68427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karam EG, Mneimneh ZN, Dimassi H, Fayyad JA, Karam AN, Nasser SC, Chatterji S, Kessler RC. Lifetime Prevalent of Mental Health Disorders: First Onset, Treatment and Exposure to War. PLoS Medicine. 2008 doi: 10.1371/journal.pmed.0050061. press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigerson HG, Reynolds CF, Frank E, Kupfer DJ, George CJ, Houck PR. Stressful life events, social rhythms, and depressive symptoms among the elderly: An examination of hypothesized causal linkages. Psychiatry Res. 1994;51(1):33–49. doi: 10.1016/0165-1781(94)90045-0. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Frank E, Kasl SV, Reynolds CF, III, Anderson B, Zubenko GS, Houck PR, George CJ, Kupfer DJ. Complicated grief and bereavement-related depression as distinct disorders: Preliminary empirical validation in elderly bereaved spouses. Am J Psychiatry. 1995;152(1):22–30. doi: 10.1176/ajp.152.1.22. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Bierhals AJ, Kasl SV, Reynolds CF, Shear MK, Newsom JT, Jacobs S. Complicated grief as a disorder distinct from bereavement-related depression and anxiety: A replication study. Am J Psychiatry. 1996;153(11):1484–1486. doi: 10.1176/ajp.153.11.1484. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Shear MK, Jacobs SC, Reynolds CF, III, Maciejewski PK, Davidson JR, Rosenheck R, Pilkonis PA, Wortman CB, Williams JBW, Widiger TA, Frank E, Kupfer DJ, Zisook S. Consensus criteria for traumatic grief. A preliminary empirical test. Br J Psychiatry. 1999;174(1):67–73. doi: 10.1192/bjp.174.1.67. [DOI] [PubMed] [Google Scholar]
- Sartorius N. A new way of reducing the prevalence of mental disorders? World Psychiatry. 2007;6(3):162–163. [PMC free article] [PubMed] [Google Scholar]
- Van Eerdewegh MM, Bieri MD, Parrilla RH, Clayton PJ. The bereaved child. Br J Psychiatry. 1982;140:23–29. doi: 10.1192/bjp.140.1.23. [DOI] [PubMed] [Google Scholar]
- Wakefield JC, et al. Extending the Bereavement Exclusion for Major Depression to other Losses. Evidence from the National Comorbidity Survey. Arch Gen Psychiatry/vol. 2007;64:433–440. doi: 10.1001/archpsyc.64.4.433. [DOI] [PubMed] [Google Scholar]
- Weller RA, Weller EB, Fristad MA, Bowes JM. Depression in recently bereaved prepubertal children. Am J Psychiatry. 1991;148(11):1536–1540. doi: 10.1176/ajp.148.11.1536. [DOI] [PubMed] [Google Scholar]
- WHO World Mental Health Survey Consortium. Prevalence, Severity, and Unmet Need for Treatment of Mental Disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Zisook S, Shuchter SR. Depression through the first year after the death of a spouse. Am J Psychiatry. 1991;148(10):1346–1352. doi: 10.1176/ajp.148.10.1346. [DOI] [PubMed] [Google Scholar]
- Zisook S, Shuchter SR. Uncomplicated bereavement. J Clin Psychiatry. 1993;54(Suppl):365–372. [PubMed] [Google Scholar]
- Zisook S, Shuchter SR, Sledge PA, Paulus M, Judd LL. The spectrum of depressive phenomena after spousal bereavement. J Clin Psychiatry. 1994;55(4 suppl):29–36. [PubMed] [Google Scholar]
- Zisook S, Paulus M, Shuchter SR, Judd LL. The many faces of depression following spousal bereavement. J Affect Disord. 1997;45:85–95. doi: 10.1016/s0165-0327(97)00062-1. [DOI] [PubMed] [Google Scholar]
- Zisook S, Chentsova-Dutton Y, Schuchter SR. PTSD Following bereavement. Ann Clin Psychiatry. 1998;10(4):157–163. doi: 10.1023/a:1022342028750. [DOI] [PubMed] [Google Scholar]
- Zisook S, Kendler KS. Is bereavement-related depression different than non-bereavement –related depression ? Psychological Medicine. 2007a:1–31. doi: 10.1017/S0033291707009865. [DOI] [PubMed] [Google Scholar]
- Zisook S, Sheer K, Kendler KS. A validity of the bereavement exclusion criterion for the diagnosis of Major Depression Episode World. Psychiatry. 2007b;6:00–00. [PMC free article] [PubMed] [Google Scholar]