Abstract
Tumor progression ensues within a three-dimensional microenvironment that consists of cellular and non-cellular components. The extracellular matrix (ECM) and hypoxia are two non-cellular components that potently influence metastasis. ECM remodeling and collagen cross-linking stiffen the tissue stroma to promote transformation, tumor growth, motility and invasion, enhance cancer cell survival, enable metastatic dissemination, and facilitate the establishment of tumor cells at distant sites. Matrix degradation can additionally promote malignant progression and metastasis. Tumor hypoxia is functionally linked to altered stromal-epithelial interactions. Hypoxia additionally induces the expression of pro-migratory, survival and invasion genes, and up-regulates expression of ECM components and modifying enzymes, to enhance tumor progression and metastasis. Synergistic interactions between matrix remodeling and tumor hypoxia influence common mechanisms that maximize tumor progression and cooperate to drive metastasis. Thus, clarifying the molecular pathways by which ECM remodeling and tumor hypoxia intersect to promote tumor progression should identify novel therapeutic targets.
Keywords: Collagen cross-linking, Hypoxia, Matrix remodeling, Matrix stiffness, Metastasis, Tumor progression
Introduction
Tissue context profoundly influences malignant transformation and tumor progression [1]. This concept was vividly demonstrated experimentally by Mintz and colleagues who showed that the normal mouse embryonic tissue microenvironment could repress expression of the tetracarcinoma tumor phenotype [2, 3]. Bissell and colleagues then demonstrated that the normal chicken embryonic microenvironment could suppress transformation mediated by the Rous Sarcoma Virus (RSV) tumor oncogene, and that wounding promoted tumor progression [3]. Experimental data presented by multiple laboratories have since confirmed these seminal observations and demonstrated that the tissue stroma can either promote or restrict tumor progression [4–7]. More recently, the individual or combined activities of cellular components of the stroma have been shown to modulate various stages of tumor progression. These include, activated endothelial and lymphatic cells, altered fibroblasts, infiltrating immune cells, modified adipocytes and even stimulated mesenchymal stem cells [8–12]. Non-cellular aspects of the tumor microenvironment, such as hypoxia and an altered extracellular matrix (ECM), have additionally been shown to contribute to tumor progression either directly by destabilizing tissue integrity and promoting tumor cell motility, invasion and survival, or indirectly by inducing tumor angiogenesis and enhancing tumor cell survival and selection [4, 13, 14]. Here, we focus on the mammary gland and discuss the critical role of non-cellular microenvironmental factors in normal tissue homeostasis, and in tumor evolution and metastasis. We outline how a synergistic interaction between ECM remodeling and hypoxia, two non-cellular components of the tissue microenvironment, can cooperatively drive tumor metastasis by influencing common molecular targets that may therefore constitute tractable drug targets.
The importance of non-cellular components of the tissue microenvironment on tissue homeostasis
ECM structure determines tissue context
Normal organ and tissue function is determined by the reciprocal communication between cells and their surrounding stroma [15]. The non-cellular component of the stroma includes soluble factors, such as growth factors and cytokines, and an insoluble protein network to which these soluble factors can bind called the extracellular matrix (ECM) [16]. The ECM is a three-dimensional (3D) structure surrounding cells [17]. There are two major categories of ECM. The first type is the basement membrane (BM), which interacts directly with the epithelium and endothelium, and consists primarily of collagen IV, laminins, entactin/nidogen and heparan sulfate proteoglycans [18–20]. The second type is the interstitial matrix, which makes up the bulk of the ECM in the body. The interstitial matrix consists of many collagens including type I and III, which together with fibronectin contribute to the mechanical strength of the tissue [21]. The interstitial matrix additionally consists of tenascin and proteoglycans that provide tissue hydration, growth factor and cytokine binding functions, and cross-link the matrix to enhance its integrity [22]. Although originally thought of as merely a support system for the cells within the tissue, the ECM is now recognized as a central regulator of cell and tissue behavior by providing contextual information for cells to respond to stimuli [23–25]. Indeed, while the basic characteristics and composition of the basement membrane and interstitial matrix are constant across tissues, variations in ECM component and isoform expression [26], and post-translational modifications, contribute to differences in ECM organization and structure and ensure tissue specificity [22, 27].
ECM topology reflects the organization, orientation and post-translational modifications of the matrix. These parameters determine the mechanical properties of the ECM and modulate cell and tissue phenotype by influencing cytoskeletal remodeling and receptor signaling to influence cell behavior [18, 28]. The architecture of the tissue ECM is influenced by its topology and its biochemical composition [29–32]. Matrix concentration and post-translational modifications, such as glycosylation and cross-linking, significantly affect the mechanical properties of the ECM, including its viscoelasticity or stiffness (which can be measured in Pascals; Pa) [28]. Both the stiffness and topology of the ECM regulate the growth, remodeling, differentiation, migration and phenotype of a wide variety of cell and tissue types [14, 33]. Consistently, mechanical force mediated at the cellular and tissue level specifies tissue organization and cell migration during early embryogenesis, and modulates tissue function and homeostasis in the adult organism [29, 30]. Much of the force mediating these behaviors is functionally linked to ECM architecture and cell-generated actomyosin-dependent contractility [29, 30]. Although it is not clear how ECM topology and stiffness regulate cell fate, it is fast becoming clear that these matrix parameters are likely as important as its biochemical composition, and can profoundly affect cell behavior and influence gene expression to regulate processes as disparate as stem cell differentiation and tumor phenotype [24, 33–39].
Matrix stiffness regulates cell phenotype and function
The importance of matrix stiffness in tissue-specific differentiation is exemplified by the fact that cells grown as monolayers (two dimensional; 2D) on top of either a plastic substrate or a glass cover slip, either with or without ECM ligand, fail to assemble tissue-like structures (3D) and do not express differentiated proteins upon stimulation [14, 28]. These phenotypic disparities can be explained, in part, by the fact that the consistency of living tissues is dramatically softer than conventional 2D substrata such as tissue culture plastic (polystyrene) or borosilicate glass. Specifically, soft tissues such as the breast, liver and lung range between 150 and 3,000 Pa, whereas plastic has a stiffness approaching the GPa range, which is infinitely stiff, and borosilicate glass, is, by comparison 1–2 GPa [14, 28]. Consistently, if epithelial cells and melanocytes are grown in the context of a 3D compliant ECM microenvironment (150–400 Pa) they assemble into tissue-like structures and express differentiated proteins when given the correct soluble stimuli [9, 40, 41]. The architecture of the interstitial tissue matrix in vivo also differs substantially from that found typically in tissue culture plastic experiments, and this too can have dramatic effects on cell behavior [42]. For instance, epithelial cells in a tissue either interact with “other” cells and basally contact a BM (which itself has a complex 3D topology), and tissue fibroblasts are surrounded by interstitial collagen fibrils that can be heavily glycosylated and cross-linked with diameters that range from 0.1 microns upwards to 10 microns. Furthermore, the orientation of these collagen fibers can critically regulate cell and tissue behavior [30, 36]. This 3D contextual information is lost when cells are grown in 2D.
Changes in matrix stiffness and ECM remodeling play a crucial role in embryonic mammary gland development, influence branching mammary gland morphogenesis, and facilitate lactation (functional differentiation) and involution (apoptosis), to orchestrate normal mammary gland homeostasis [18]. Substrate compliancy independently regulates mammary epithelial cell (MEC) shape, mammary tissue morphogenesis, and endogenous BM assembly [14]. For example, functional and morphological differentiation of primary MECs in response to lactogenic hormones can proceed only when mixed mammary cell populations isolated from pre-lactating mice are plated on floating (compliant) collagen gels and permitted to assemble an endogenous BM [28, 43, 44]. Consistently, MEC acini morphogenesis and functional differentiation is not supported by mechanically loaded or cross-linked (stiff) collagen gels because they are too rigid to allow cell rounding and endogenous BM assembly [28].
The ECM stiffness can regulate cell and tissue behavior by initiating biochemical signaling cascades in cells through interactions with a number of specialized transmembrane ECM receptors including integrins, Discoid Domain Receptors (DDRs) and syndecans [45–49]. These are mechanosensors critical for mediating outside-in cell signaling to regulate cell behavior. Integrins are perhaps the best characterized ECM receptors that are important for adhesion interactions. They are an excellent model with which to understand how an altered ECM could promote tumor progression. Integrins consist of 24 distinct transmembrane heterodimers that relay cues from the surrounding ECM to regulate cell growth, survival, motility, invasion and differentiation [48]. By virtue of their ability to interact with the ECM externally, and with cytoplasmic adhesion plaque proteins and the cytoskeleton intracellularly, integrins are able to transmit dynamic cues from the tissue microenvironment to influence cell behavior. Integrin-ECM interactions regulate cell fate by activating multiple biochemical signaling circuits and altering cell and nuclear shape [50–52]. This occurs either through direct interactions between ECM receptors and actin linker proteins or cytoskeletal reorganization induced by activating cytoskeletal remodeling enzymes, such as RhoGTPases [50–52].
Hypoxia regulates normal tissue homeostasis
Hypoxia (low oxygen) is another important non-cellular component of the physiological tissue microenvironment. Similar to ECM stiffness, hypoxia, potently influences cell phenotype, genotype, differentiation and fate [53–58]. Hypoxia itself is a potent regulator of ECM composition, topology and stiffness. Hypoxia-mediated gene expression, signaling and matrix remodeling are critical for embryonic development and wound healing [57–59]. For example, hypoxia regulates the cellular events that occur during the first trimester of pregnancy when fetal trophoblast cells invade the maternal uterine spiral arteries leading to loss of the vascular cells from the vessel wall and remodeling of the ECM [60]. Hypoxic regulation of invasion and ECM remodeling is critical for placental development to ensure that sufficient blood can reach the developing fetus. Furthermore, hypoxia regulates lung branching morphogenesis during embryonic development [61], and oxygen deprivation can stimulate mammary epithelial cell branching morphogenesis in vitro through increased HGF expression [62].
Hypoxic conditions stimulate blood cell proliferation and blood vessel formation, and modulate expression of ECM components and remodeling enzymes thereby maintaining tissue homeostasis. Hypoxia-driven changes in gene expression are mediated primarily by hypoxia-inducible factor (HIF)-1 [63]. For example, hypoxia increases ECM accumulation in mesenchymal cells in a HIF-1 dependent fashion, which is required for chondrogenesis and joint development during fetal growth [64]. Moreover, HIF-1 deficient trophoblast stem cells exhibit reduced adhesion and migration toward vitronectin compared with wild-type cells [65], and the defective trophoblast invasion observed in the absence of HIF-1 was associated with decreased cell surface localization of integrin αvβ3 and reduced levels of focal adhesions containing αvβ3 integrin [65]. Thus, hypoxia stimulates cell adhesion and migration, as well as angiogenesis and ECM remodeling, and can cooperate with ECM stiffness to synergistically influence cell behavior.
The importance of non-cellular components of the tissue microenvironment on tumor evolution
ECM structural changes during tumorigenesis
Transformation can be regulated by the microenvironment, as was clearly demonstrated by early experiments exploring the role of RSV in tumor behavior [3]. These and other studies emphasize that tumors are organs whose formation is governed by 3D tissue context [4–7]. Epithelial cancers, such as breast cancer, can be caused by somatic gene mutations but are additionally influenced by sustained alterations of the microenvironment including those associated with ECM remodeling. In fact, the composition of the ECM varies during the development of pathologies such as cancer, and the aberrant expression and organization of matrix components produced by stromal cells in response to stress can direct the malignant behavior of epithelial cells [8, 16, 66].
Many ECM components and remodeling enzymes are elevated in cancer patients [13, 18, 67–69]. In the normal breast tissue, tightly controlled MMPs remodel the breast ECM to promote mammary gland growth and involution. In tumors, however, this stringent control of MMP expression and activity is lost [70]. Overexpression of MMPs 3, 11, 12 and 13 have been demonstrated in the tumor stroma, along with MMP-2 in transformed mammary epithelial cells [71]. Polymorphisms in the promoter region of MMP-3 resulting in elevated expression are associated with increased tumor incidence in patients [72]. Moreover, ectopic expression of MMP-3 within the MECs of transgenic mice induced desmoplasia, precocious branching morphogenesis and malignant transformation of the tissue [73]. Thus, aberrant MMP activity is not merely symptomatic of transformed tissue but additionally plays a causative role. Fibrillar collagens (types I, II, III, V and IX [21]) normally have a low turnover but their metabolism is increased during the ECM remodeling that characterizes tumor evolution [16]. Type I collagen synthesis and remodeling is required for growth factor-induced angiogenesis, endothelial cell invasion and vessel formation, which are necessary to maintain tumor growth [74]. Indeed, the synthesis, concentration and circulating levels (serum concentration) of degradation products of type I collagen are increased during breast, lung, ovarian, prostate and skin malignancy [68, 69, 75–77].
The architecture of tumor-associated ECM is fundamentally different from that of the normal tissue stroma [78]. In particular, whereas type I collagen is in a parallel orientation with respect to the epithelial cells, it is less organized in the stroma surrounding a transformed tissue [79]. While one may expect increased ECM synthesis to encapsulate and limit tumor progression, ECM deposition can in fact enable tumor cell invasion by providing critical biochemical cues that promote chemotaxis or that enhance cell migration by stiffening the matrix [14, 28] as has been observed along type I collagen fibers in invading breast tumors using intravital imaging [80]. Furthermore, elevated ECM deposition and remodeling can directly increase interstitial pressure and impede fluid drainage, as illustrated by the curved matrix sheets formed in melanomas, and these forces can severely compromise the efficacy of drug delivery [16, 78, 81–84].
Matrix stiffness drives transformation
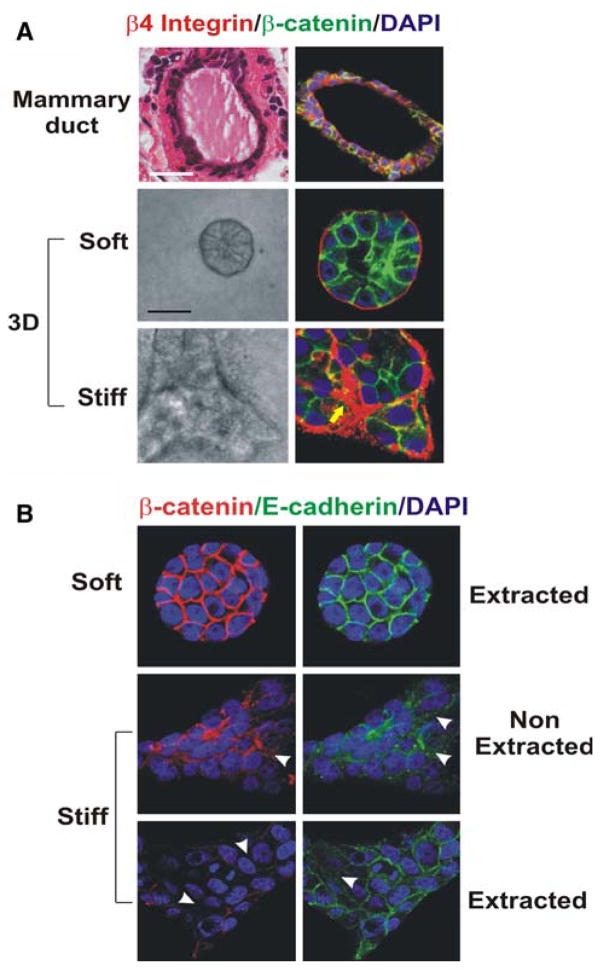
Matrix stiffening is induced by increased collagen deposition and ECM cross-linking, and can promote malignant transformation by enhancing growth factor signaling and destabilizing tissue integrity [14, 28]. For example, human mammary epithelial cells (HMECs) grown on a highly rigid matrix develop a malignant morphology that is characterized by destabilized E-cadherin adherens junctions, absence of tissue polarity and an invasive behavior (Fig. 1) [14]. Increased matrix stiffness has been observed in fibrotic lungs, in scar tissue, in tissue exposed to high doses of radiation, in aged skin and in women with dense breasts; all conditions that predispose these individuals and tissues to a higher cancer risk. Consistently, tumors are characteristically stiffer than their normal adjacent tissue, and while increased cell mass undoubtedly contributes to the increase in tissue force in tumors, altered stiffness is often detected as a global increase in the physical properties of the transformed tissue [85, 86].
Fig. 1.
Mammary epithelial growth and morphogenesis is regulated by matrix stiffness. (a) 3D cultures of normal mammary epithelial cells (MECs) within collagen gels of different concentration. Stiffening the ECM through an incremental increase in collagen concentration (soft gels: 1 mg/ml Collagen I, 140 Pa; stiff gels 3.6 mg/ml Collagen I, 1,200 Pa) results in the progressive perturbation of morphogenesis, and the increased growth and modulated survival of MECs. Altered mammary acini morphology is illustrated by the destabilization of cell–cell adherens junctions and disruption of basal tissue polarity indicated by the gradual loss of cell–cell localized β-catenin (green) and disorganized β4 integrin (red) visualized through immunofluorescence and confocal imaging. (b) Confocal immunofluorescence images of MEC colonies on soft and stiff gels (140 vs. >5,000 Pa) stained for β-catenin (red) and E-cadherin (green), and counterstained with DAPI (blue) after triton X-100 extraction. β-catenin could be extracted from the sites of cellcell interaction in MEC colonies formed on a stiff but not on a soft gel, indicating that adherens junctions are less stable in MEC structures formed on stiff gels. White arrows indicate diffuse staining patterns of β-catenin and E-cadherin (Modified from Kass et al. [18])
Indeed, over the years imaging methods such as ultra sound sono elastography and MR imaging elastography have been exploited to monitor tissues for evidence of transformation based upon differential stiffness profiles of not only the tumor itself, but also of the surrounding non-transformed tissue [86]. These findings suggest that the stiffening associated with tumor progression is linked to changes in the ECM structure that track with the tumor phenotype. These include elevated levels of collagen, linearization of the collagen fibrils, higher amounts of matrix cross-linking enzymes, and enhanced expression of proteoglycans implicated in matrix cross-linking including lumican and biglycan [87]. Tumor stiffness has additionally been attributed to the elevated interstitial pressure due to leaky blood vessels and lymphatics [88].
Mechanical interactions between cancer cells and ECM can accelerate neoplastic transformation [14, 89, 90]. For instance, normal tissues can be induced to become cancerous in vivo by altering ECM structure [73]. The idea that structural or mechanical changes in the microenvironment actively contribute to tumor formation is not a novel concept. Early experiments demonstrated that implantation of a rigid piece of material (metal or plastic) can trigger cancer formation whereas introduction of the same material as a powder did not induce tumor formation in animals [91]. Conversely, there are many studies in experimental systems to suggest that cancers can be induced to become quiescent, differentiate, die or form normal tissues, if provided with the correct set of 3D signals conveyed by the microenvironment[90]. Decades of research has shown that combining epithelial tumor cells with normal mesenchyme (stroma), embryonic tissues, or with ECMs that are deposited as a result of these interactions, reverts their cancerous phenotype and restores their normal tumor morphology [90, 92–96]. For example, stoma from healthy animals can prevent neoplastic transformation of grafted epithelial cancer cells and encourage their normal growth [93, 94]. The growth and differentiation of mammary epithelial tumors can be reverted to normal by modulating cell adhesion to the ECM [4]. These studies suggest that it may be possible to prevent tumor progression by “normalizing” the ECM microenvironment [90, 94].
Hypoxia drives pro-tumor ECM remodeling
Hypoxia is present in all solid tumors over 1 cm3, and is clinically associated with metastasis and poor patient outcome [54, 57]. Transformation of cells may also be driven by hypoxia, which induces oncogene expression, enhances DNA mutation rate, and selects for cells with increased apoptotic thresholds [54, 97–99]. In addition hypoxia can drive tumor evolution through increased matrix deposition, cross-linking and remodeling. Hypoxia increases collagen biosynthesis [100, 101], collagen fibril deposition [102, 103], and collagen remodeling [103], and processing [104]. For example, hypoxia up-regulates the P4H αI subunit of collagen prolyl 4-hydroxylase (P4H) which is the rate-limiting subunit for the hydroxylation of proline residues of procollagens [104]. The formation of hydroxyproline is an essential post-transcriptional process for stabilization of the helical trimer of procollagen polypeptides. Prolonged hypoxic incubation of fetal rat lung fibroblasts enhanced this post-transcriptional step of collagen synthesis and accelerated the deposition of collagen molecules and fibrils [102]. In addition, cytoplasmic P4Hs play a critical role in the regulation of the HIFα [105].
In addition, hypoxia increases expression of matrix remodeling enzymes, including MMPs [106]. Micro-array analysis revealed that expression of a secreted protein, lysyl oxidase (LOX), was consistently over-expressed by hypoxic human tumor cells [107]. LOX initiates the covalent cross-linking of collagens and elastins, thereby increasing insoluble matrix deposition and tensile strength [108]. LOX expression is induced by hypoxia-inducible factor (HIF)-1 and is associated with experimental hypoxia in vitro and in vivo, and clinically in breast and head and neck cancer patients [13]. LOX is synthesized in fibrogenic cells as a pre-pro-enzyme that is cleaved and glycosylated prior to its secretion [108]. After secretion, the LOX pro-enzyme is proteolytically processed by procollagen C-proteinase (bone morphogenic protein-1) which releases the 32-kDa biologically active mature form of the protein. Procollagen C-proteinase (bone morphogenic protein-1) is also hypoxia-induced [107], and cleaves pro-collagens thereby permitting processing and collagen fibril assembly, in addition to activating LOX.
LOX mediates stiffness-induced transformation
The importance of collagen remodeling, cross-linking and stiffening to tumor progression was emphasized by our recent unpublished work in which we primed the mammary stroma of nude mice with fibroblasts expressing a constitutively active LOX (Levental et al., unpublished). In these studies, LOX-dependent collagen cross-linking of the mammary fat pad promoted the linearization of the interstitial collagens, stiffened the gland and induced the neoplastic progression of Ha-Ras pre-malignant HMECs. Consistently, we found that the elastic modulus (indentor) and the storage modulus (shear) (i.e. stiffness) of the mammary tissue in MMTV-Her2/neu transgenic mice increased incrementally, coincident with and prior to the establishment of large, invasive tumors. Although the tissue stiffening could be attributed in part to an increase in cell mass, we noted that both the tumor and the surrounding stroma were significantly stiffer than normal tissue [14]. Moreover, second generation harmonics imaging as well as polarized light scanning of picrosirius-stained tissues revealed that tissue stiffening correlated with collagen linearization. Importantly, we found that collagen linearization was associated with elevated levels of the collagen cross-linker LOX, which we could detect in the stroma prior to tumor formation. Matrix stiffening and cross-linking were additionally associated with enhanced mechano-responsiveness of the epithelium, as evidenced by elevated activated focal adhesion kinase, and p130 Cas. Intriguingly, inhibiting LOX-dependent collagen cross-linking in Her2/neu mice, tempered collagen linearization, reduced gland stiffening and enhanced the latency and decreased the incidence of breast transformation. These data imply that altering the cell’s mechano homeostasis could promote the malignant behavior of an epithelium in culture and promote transformation in vivo, and that inhibiting matrix stiffening could temper reducing matrix stiffness can diminish breast transformation in vivo.
Metastasis driven by non-cellular components of the tumor microenvironment
3D context dictates malignant progression
Deregulated growth is not sufficient to make a tissue cancerous. What makes a growing cancer malignant is its ability to break down tissue architecture, invade through disrupted boundaries, and metastasize to distant organs. Malignant progression is completely dependent upon the 3D context of the tissue microenvironment. In fact, the multistep process of metastasis can only be successful if the 3D microenvironment is permissive for tumor cell invasion, metastatic dissemination and metastatic growth. Non-cellular components of the tumor microenvironment, such as the ECM and hypoxia, critically drive tumor progression through increased ECM deposition, cross-linking and remodeling. This ECM remodeling creates a micro-environmental context that enhances tumor cell survival, migration, growth, tumor angiogenesis and lymph angiogenesis [67, 109, 110]. Indeed, hypoxia and matrix remodeling that lead to a progressive stiffening of the ECM are associated with tumor progression, and many ECM components and remodeling enzymes are associated with metastasis in cancer patients [13, 18, 67–69].
The 3D organization and architecture of the ECM and stroma are dynamic [16, 18]. Ultrastructural studies, immunohistochemistry, and biochemical analysis have demonstrated changes in stroma, ECM composition and architecture occur at critical steps during malignant progression [109, 111]. The dramatic changes in the organization and composition of the ECM during tumor progression alter tumor behavior and contribute to tumor metastasis. For instance, the mammary gland matrix stiffens progressively during tumor progression and this mechanical alteration is associated with increased collagen, fibronectin and tenascin deposition, and elevated collagen cross-linking and linearization [14]. Matrix stiffness in association with growth factors, enhances cell survival and increases cell contractility [14]. Matrix stiffness and/or exogenous force independently induce cell-generated contractility to promote focal adhesion maturation and enhance integrin-dependent signaling, thus compromising multicellular tissue morphogenesis and promoting a tumor-like behavior in mammary cells [14]. This suggests that matrix stiffness likely promotes breast tumorigenesis through altering integrins and their adhesion interactions. Conversely, blocking integrin or growth factor-dependent cell contractility can revert the malignant phenotype in culture [40]. Consistent with these findings, ectopic expression of β1 integrin mutants with increased transmembrane molecular associations (V737 N, G744 N), elevated cellular contractility and forced focal adhesion maturation increase integrin/growth factor-dependent signaling, again to compromise multi-cellular tissue morphogenesis and promote tumorigenic behavior in culture and in vivo [14].
ECM structural changes disrupt cell–cell relations
Deregulated cell growth and loss of cell–cell relations correlate with compromised structural integrity of the basement membrane (BM) [92]. Tumor cell growth can be suppressed and cells can be induced to re-form polarized epithelium when they come into contact with intact BM in vivo or are cultured on intact BM in vitro [92, 95, 96, 112]. Structural alterations in the BM occur early on in cancer, even before the development of a palpable tumor [113]. These include gaps, thickening, loosening of cells from each other and the surrounding stroma [90], and can be considered a hallmark of malignant invasion because tumors surrounded by an intact BM generally do not penetrate into surrounding tissues [114–116].
Loss of cell–cell contact occurs during epithelial-to-mesenchyme transition (EMT), and is a key step in malignant progression of many epithelial cancer cells [117]. EMT often occurs as a consequence of transcriptional repression of E-cadherin mediated by transcription factors such as TWIST, Snail and Slug [117]. Hypoxia drives EMT through hypoxia-inducible factor (HIF) [118], uPAR [119] and TWIST [120]. TWIST expression is increased by mechanical force [121], and EMT can be induced by TGF-β released as a result of hydrostatic compression [122–126]. Intriguingly, murine MECs expressing oncogenic Ras expressed higher levels and secreted more ILEI, a novel interleukin-related protein, following EMT induction by TGF-β [127]. ILEI knock-down normalized the morphology and gene expression of the MECs and prevented the transformation and metastasis of normal epithelial cells [127]. Importantly, EMT induces cytoskeletal reorganization and alters cell adhesion to increase tensional force illustrating how an exogenous mechanical force can modulate cellular tension through a positive feed-forward mechanism [32, 128].
Transformed MECs often exert greater cell-generated force in response to physical interactions with the ECM [14]. These cellular forces are mediated through actomyosin contractility and cytoskeletal remodeling that are induced by ERK and Rho GTPase signaling. Matrix stiffening can establish a mechanical autocrine loop in which Rho GTPases are activated by the transmission of force through transmembrane integrin receptor interactions with the ECM and that can be suppressed by tension dissipation in the cytoskeleton [28, 90]. Mechanotransduction modulates cell behavior by altering the function and activity of multiple signaling pathways including those regulated by ERK, MAPK, calcium, SRC, and G-coupled receptor proteins [28, 90]. Force can significantly enhance growth factor signaling and even modify the requirement of cytokine binding for receptor activation [28, 90, 129]. ECM rigidity enhances cell contractibility largely by activating RhoGTPases, and by so doing drives cell spreading and growth, promotes ECM fibril alignment and can further increase ECM stiffness and induce matrix tension by facilitating cell pulling through ECM adhesions [14]. Furthermore, Rho can alter cell and tissue tension by promoting EMT [130]. Finally, tensional stress can facilitate cell invasion by elevating MMP-9 release and activation [131].
ECM remodeling and hypoxia enable invasion, metastatic growth and dissemination
The acquisition of the metastatic phenotype is not simply the result of deregulated signal transduction pathways, but instead is achieved through a stepwise selection process driven by microenvironmental pressures including hypoxia and ECM remodeling. For example, invasion into surrounding tissue requires destruction of the BM and remodeling of the ECM. This is governed by microenvironmental cues that determine ECM degradation and synthesis. Hypoxia can disrupt tissue integrity and enhance cell motility and invasion directly by repressing E-cadherin and enhancing N-cadherin expression and hepatocyte growth factor (HGF)-MET receptor signaling [132]. Hypoxia can disrupt tissue integrity indirectly by promoting cell-ECM interactions through enhancement of αvβ3 integrin membrane localization [65], or by fostering ECM remodeling through up-regulation of uPAR and uPAR-dependent MMP activation [132]. In addition, hypoxia can induce ECM stiffening through elevated expression of LOX and LOX-dependent collagen cross-linking [13]. In addition, hypoxia indirectly enhances tumor dissemination by directly regulating the expression and activity of hypoxia-induced vascular endothelial growth factor (VEGF) to promote angiogenesis and lymphangiogenesis, and increase vascular permeability to promote both intravasation at the primary tumor site and extravasation at the distant metastatic site [132].
Disordered ECM architecture is a characteristic of the tumor invasive front where increased matrix deposition and remodeling is observed [133, 134]. Hypoxia enhances the proteolytic activity at the invasive tumor front and alters interactions between integrins and components of the ECM, enabling tumor cell invasion [132]. Invasive branching of breast cancer cells growing in 3D matrix is observed in oxygen-deprived conditions due to hypoxia-induced HGF expression [62]. Furthermore, hypoxia-induced LOX is needed for invasive branching of oxygen-deprived human cancer cells in 3D matrix and its expression is elevated at the leading edge of invading cells [13]. LOX expression is not only associated with hypoxia but is also associated with metastasis and decreased survival in human cancer patients [13]. Inhibition of LOX expression or activity was found to prevent in vitro invasion and in vivo metastasis in an orthotopic model of breast cancer [13]. LOX activity outside of the cell resulted in matrix remodeling and activation of focal adhesion kinase (FAK) enabling cell motility. LOX inhibition resulted in decreased cell–matrix adhesion interactions critical for invasive migration and metastatic dissemination. A dependence on LOX expression for metastatic growth was additionally observed and may be explained by LOX’s role in the formation and maintenance of the metastatic niche (see below). LOX-induced matrix cross-linking can activate MMPs (ErlerBennewith et al., unpublished). Increased MMP activity results in both matrix remodeling and release of chemokines, cytokines and growth factors trapped within the ECM [16]. Taken together, these studies demonstrate that hypoxia can enhance ECM remodeling thereby enabling tumor cell invasion.
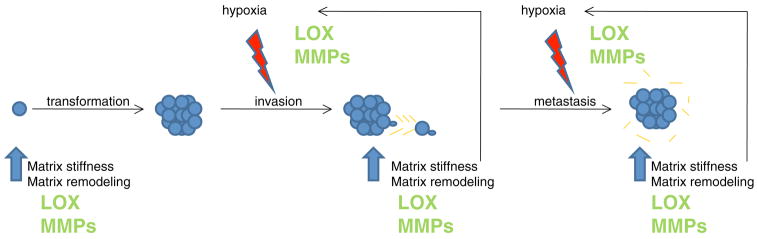
Angiogenesis is required for metastatic dissemination and to sustain metastatic growth. Mechanical interactions between capillary cells and ECM control capillary cell growth and angiogenesis through Rho signaling [135]. Angiogenesis is also potently induced by hypoxia through increased expression of vascular endothelial growth factor, erythropoietin, and other pro-angiogenic factors [54]. Under physiological non-hypoxic conditions, angiogenesis can be driven by mechanical forces. For example, capillary endothelial cells subjected to mechanical stretch demonstrate elevated MMP-2 and HIF-1α expression, and MMP-2 activity [136]. These findings additionally suggest that ECM remodeling can increase hypoxic responses, a phenomenon supported by the presence of hypoxia as a result of increased ECM remodeling and fibrosis during wound-healing [58]. Hypoxia in turn increases the expression and activity of genes involved in fibrosis and ECM remodeling, resulting in a feed-forward mechanism that increases matrix stiffness and drives tumor progression (Fig. 2). This synergistic relationship is further exemplified by the fact that tumor-associated compression stress can induce tumor angiogenesis by directly increasing expression of VEGF or indirectly by blocking the vasculature surrounding the tumor mass to promote hypoxia and VEGF secretion [137].
Fig. 2.
Schematic to demonstrate the interplay between hypoxia and matrix remodeling, using lysyl oxidase (LOX) as an example. LOX expression is increased in pre-malignant tissue, where it cross-links collagens in the ECM increasing matrix stiffness and enabling ECM remodeling. This allows for malignant transformation and primary tumor growth. As the tumor grows larger, regions become subjected to hypoxic conditions. In response to hypoxia, tumor cells increase expression of proteins involved in collagen biosynthesis and processing, including LOX. This results in increased matrix deposition, collagen cross-linking, matrix remodeling and matrix stiffness, which in turn encourage a hypoxic environment. LOX secreted by hypoxic tumor cells is additionally involved in the formation of a pre-metastatic niche at distant sites of future metastasis. Increased collagen cross-linking and matrix remodeling attract bone marrow-derived cells to the site, which create a niche permissive for metastatic tumor cell attachment and growth. Again, subsequent matrix remodeling and increased stiffness at these metastatic sites would enhance hypoxia, which in turn elevates expression of proteins involved in collagen biosynthesis and processing, further increasing matrix remodeling and matrix stiffness. This feed forward mechanism is further enhanced by matrix metalloproteinase (MMP) activity. MMP expression and activity is elevated by both increased matrix stiffness and by hypoxia. Thus, the symbiotic interaction between ECM remodeling and hypoxia, two non-cellular components of the tissue microenvironment, can cooperatively drive tumor metastasis by influencing common targets
The importance of cellular components of the tissue microenvironment on tumor progression
Metastatic progression depends on stromal cell involvement
The non-tumor cellular component of the microenvironment consists of activated and/or recruited host cells such as fibroblasts and immune cells [8, 138]. It is the reciprocal interactions between these host cells, the tumor cells and the ECM that drive tumor progression including metastatic dissemination [16, 109]. Altering stromal cells alone can induce cancer [5], and mutations in stromal cells contribute to the formation of epithelial tumors [139]. Thus, persistence of abnormal signals from the stroma can create an interdependent cancerous tissue [16]. In addition, solid tumor growth cannot be sustained unless the tumor resets the balance between ECM remodeling/degradation and ECM synthesis, and growth cannot be maintained without sufficient blood supply [79]. To do this, the tumor must recruit stromal cells (fibroblasts, inflammatory cells and vascular cells) to increase ECM deposition, MMP-mediated matrix degradation, and increase angiogenesis [16]. Stromal cells therefore play a critical role in tumor evolution and metastasis [140].
Alterations in matrix compliance, such as changes in stiffness, influence MEC malignant behavior directly through mechanotransduction pathways (described above) or indirectly by activating resident fibroblasts to release cytokines, growth factors and ECM degrading enzymes [28, 141–143]. Fibroblasts are the predominant cell population in the stroma, and are the largest producers of ECM components (collagen I and fibronectin, in particular) [110]. Each organ has their own specific set of fibroblasts that regulate normal tissue homeostasis [144]. Fibroblasts associated with the tumor stroma are myofibroblasts, peritumor fibroblasts, and cancer associated fibroblasts (CAFs) [16]. CAFs can stimulate oncogenic signaling and malignancy in non-tumorigenic epithelial cells [145]. In addition, CAFs produce abundant quantities of collagen changing the biochemistry and structure of the ECM, which can encourage tumor development and progression [146, 147]. One of hallmarks of fibroblasts is that they are surrounded by dense accumulations of fibrillar collagen [110, 148]. This desmoplastic response is frequently seen cancers such as breast, pancreatic, prostate, colon and lung, and is associated with the recruitment of inflammatory cells and with the induction of angiogenesis [16]. Furthermore, hypoxia is associated with desmoplasia and poor prognosis in breast cancer patients [149].
Stromal cells mediate pro-metastatic ECM remodeling
Fibroblasts
Fibroblasts and vascular cells create a similar fibrotic environment during wound healing to enable tissue repair. In fact, both tissue fibrosis and inflammation increase cancer risk in patients [138], and there is an increased incidence of tumor formation at sites of scarred tissue [150]. Interestingly, wounding in RSV infected chickens induces tumor formation [151] possibly by stimulating TGF-β which can [151] increase collagen production and smooth muscle actin expression in fibroblasts and induce tissue desmoplasia [152]. In this regard, cancer has been defined as a wound that fails to heal [1, 153], because tumor progression and the wound-response are both characterized by ECM remodeling, hypoxia, angiogenesis, and the recruitment of a repertoire of non-transformed host cells.
Fibroblasts themselves are strongly regulated by their 3D environment. For example, fibroblasts embedded within 3D compliant floating collagen gels are quiescent [154] in contrast to fibroblasts growing on rigid 2D substrata. However, a mechanical challenge can stimulate the fibroblasts, to increase mechanical loading and alter fibroblast behavior [28]. This is because mechanical loading induces fibroblasts to up regulate the synthesis, secretion and deposition of many ECM components and their cross-linking enzymes such as LOX, and by so doing increases the local stiffness of the matrix and enhances the tensile properties of the gel [28]. These matrix modifications further activate fibroblasts and result in a feed-forward mechanism to maximize tumor progression. Hypoxia results in similar activation of fibroblasts, and increases the expression of ECM components and remodeling enzymes, such as LOX, to further enhances tissue desmoplasia and promote metastatic progression [54, 149, 155].
Leukocytes
Innate immune cells are strong mediators of disease progression because they release potent soluble factors that enable growth, motility and angiogenesis [16, 138]. Leukocytes play a key role in tumor progression. They are loaded with chemokines, cytokines, reactive oxygen species, proteases, TNF-α, interleukins and interferons [16]. These factors are all known to mediate inflammation responses, recruit/activate innate immune cells, tissue remodeling and angiogenesis [16]. For instance, leukocytes produce abundant MMPs, which remodel the ECM and release chemokines, cytokines and growth factors, such as TNF-α, bFGF and VEGF which are sequestered to ECM molecules or tethered to cells [156, 157, 106, 108]. In particular, MMP2 and MMP9 activate latent TGF-β in ECM which drives EMT, induces tissue desmoplasia and elevates LOX expression [158]. In addition, leukocyte-mediated matrix modifications stimulate cell–cell and cell–matrix adhesion molecules thereby increasing invasion, angiogenesis and inflammation [156, 157]. While the majority of matrix remodeling creates an environment permissive for malignant conversion and cancer development, peptides released from collagen remodeling can also exert anti-angiogenic effects. These released factors include endostatin released from the NC1 fragment of type XVIII collagen [159], restin released from type XV collagen [160], arrestin released from type IV collagen [161], and all three chains of type IV collagen [27, 161, 162]. Thus, protease-generated cleavage products released from the interstitial ECM and BM can act as either suppressors or activators of angiogenesis.
TAMs
Tumor-associated macrophages (TAMs) are determinants of malignant progression [16]. TAMs are present in many cancer types including melanoma, cervical squamous cell carcinoma and mammary adenocarcinoma [163–166]. Furthermore, TAMs are associated with metastasis and poor patient outcome [167]. TAM-induced ECM remodeling increases angiogenic and lymphangiogenic responses thereby promoting tumor growth, survival and dissemination [168, 169]. In addition, TAMs enhance tumor cell invasion [80, 165] as revealed by elegant intravital imaging that showed how TAMs secrete growth factors to direct tumor cell migration towards blood vessels and enable intravasation [80]. Interestingly, TAMs are known to accumulate in regions of hypoxia raising the intriguing possibility that hypoxia might additionally promote tumor metastasis by recruiting factors that stimulate TAM recruitment [167, 170].
ECM remodeling and recruited BMDCs establish the pre-metastatic niche
Recent in vivo data has suggested that formation of a pre-metastatic niche is essential for the growth and survival of extravasating metastatic tumor cells [171]. These studies showed that factors secreted by primary tumor cells stimulate the recruitment of bone marrow-derived cells (BMDCs) to sites of future metastasis. The bone marrow-derived cells express VEGFR-1, c-kit, CD133, CD34 and integrin VLA-4, and increase angiogenesis at the pre-metastatic sites thereby creating tissue-specific niches that permit the growth and survival of metastatic tumor cells. Consistently, targeted inhibition of VEGFR-1 prevented niche formation and inhibited subsequent metastatic progression. Such localized tissue pre-conditioning may thus represent a key step during tumor metastasis that could be targeted therapeutically.
Elevated fibronectin expression in fibroblasts and fibroblast-like cells resident at pre-metastatic sites appears to be a critical factor in the development of the pre-metastatic niche. The key tumor-secreted factors that determine metastatic sites and mediate pre-metastatic niche formation have yet to be identified, although TNF-α, TGF-β and VEGF-α signaling have all been implicated [172]. MMPs might also play a role in the formation of the metastatic niche. For example, VEGF-R1 signaling is required for the pre-metastatic induction of MMP-9 expression in endothelial cells and macrophages of the lungs by distant primary tumors [173]. This is thought to make the lung microenvironment more hospitable for the subsequent invasion and survival of metastatic cells. Indeed, pericyte recruitment and angiogenesis are not observed in tumor-bearing mice with MMP-9 knock-out bone marrow cells [174], whereas stromal-derived MMP-2 and MMP-9 facilitate the establishment and growth of metastatic tumors [175].
Exactly what determines where these niches form remains unresolved. Studies have shown that cell growth rate is increased at sites where mechanical stresses concentrate [176] and that continuous mechanical perturbation induces tumors in rodents [91]. Furthermore, there are many accounts of cancer forming at sites of repeated physical injury, and chronic wounding can promote malignant transformation and foster tumor metastasis [90]. These observations raise the intriguing possibility that pre-metastatic niches might occur at sites exposed to repetitive mechanical strain.
Recently, we found that LOX secreted by hypoxic tumor cells plays a critical role in vivo in the formation of the pre-metastatic niche [ErlerBennewith et al., unpublished]. We could show that the activity of tumor-secreted LOX at pre-metastatic sites is required for BMDC recruitment. In vitro data suggested this effect was likely mediated through LOX-dependent matrix remodeling and MMP activity induced by collagen cross-linking. BMDC recruitment enabled pre-metastatic niche formation that was able to support metastatic growth, and this process could be disrupted by administering LOX-targeting therapies. These studies stress the importance of ECM remodeling and the interplay between the tumor cells and the stroma in transformation and metastasis, and highlight the therapeutic potential of targeting the tissue stroma to prevent tumor progression.
Future directions
There is a critical reciprocal and functional link between multiple non-cellular micro-environmental components that control tumor evolution and metastatic progression. These include the ECM and hypoxia, which are potent driving forces of tumor progression. Emerging evidence indicate that changes at the primary tumor, including those driven by stiffness and hypoxia, profoundly influence distant metastatic sites. Preliminary studies suggest that a complex interplay between matrix remodeling and tumor hypoxia likely “primes” the metastatic niche. Nevertheless, in order to develop effective anti-metastatic therapies, it will be critical to understand and identify the key molecular mechanisms whereby tissue context, as exemplified by mechanical force and hypoxia, regulate tumor metastasis.
Acknowledgments
We apologize to those authors whose excellent work could not be cited due to space limitations. This work was supported by DOD BCRP W81XWH-05-1-330, NCI CA078731, and DOE A107165 (VMW); and by The Institute of Cancer Research, and Cancer Research UK (JTE).
Abbreviations
- 2D,3D
2- and 3-dimensional
- Pa
Pascals
- ECM
Extracellular matrix
- MMP
Matrix metalloproteinase
- LOX
Lysyl oxidase
- HIF
Hypoxia-inducible factor
- CAF
Cancer-associated fibroblast
- TAM
Tumor-associated macrophage
- TGF
Tissue growth factor
- BMDC
Bone marrow-derived cell
- MEC
Mammary epithelial cell
- HMEC
Human mammary epithelial cell
Contributor Information
Janine T. Erler, Hypoxia and Metastasis Team, Section of Cell and Molecular Biology, The Institute of Cancer Research, 237 Fulham Road, London SW3 6JB, UK, e-mail: Janine.erler@icr.ac.uk
Valerie M. Weaver, Departments of Surgery, Anatomy, Bioengineering and Therapeutic Sciences, Center for Bioengineering and Tissue Regeneration and Institute for Regenerative Medicine, University of California San Francisco, 513 Parnassus Avenue, San Francisco, CA 94143-0456, USA, e-mail: WeaverV@surgery.ucsf.edu; valeriem.weaver@gmail.com
References
- 1.Bissell MJ, Radisky D. Putting tumours in context. Nat Rev Cancer. 2001;1:46–54. doi: 10.1038/35094059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mintz B, Illmensee K. Normal genetically mosaic mice produced from malignant teratocarcinoma cells. Proc Natl Acad Sci USA. 1975;72:3585–3589. doi: 10.1073/pnas.72.9.3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dolberg DS, Bissell MJ. Inability of Rous sarcoma virus to cause sarcomas in the avian embryo. Nature. 1984;309:552–556. doi: 10.1038/309552a0. [DOI] [PubMed] [Google Scholar]
- 4.Weaver VM, Petersen OW, Wang F, Larabell CA, Briand P, Damsky C, et al. Reversion of the malignant phenotype of human breast cells in three-dimensional culture and in vivo by integrin blocking antibodies. J Cell Biol. 1997;137:231–245. doi: 10.1083/jcb.137.1.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barcellos-Hoff MH, Ravani SA. Irradiated mammary gland stroma promotes the expression of tumorigenic potential by unirradiated epithelial cells. Cancer Res. 2000;60:1254–1260. [PubMed] [Google Scholar]
- 6.Wiseman BS, Werb Z. Stromal effects on mammary gland development and breast cancer. Science. 2002;296:1046–1049. doi: 10.1126/science.1067431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burdelya LG, Komarova EA, Hill JE, Browder T, Tararova ND, Mavrakis L, et al. Inhibition of p53 response in tumor stroma improves efficacy of anticancer treatment by increasing antiangiogenic effects of chemotherapy and radiotherapy in mice. Cancer Res. 2006;66:9356–9361. doi: 10.1158/0008-5472. CAN-06-1223. [DOI] [PubMed] [Google Scholar]
- 8.Bhowmick NA, Moses HL. Tumor-stroma interactions. Curr Opin Genet Dev. 2005;15:97–101. doi: 10.1016/j.gde.2004.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haass NK, Smalley KS, Herlyn M. The role of altered cell-cell communication in melanoma progression. J Mol Histol. 2004;35:309–318. doi: 10.1023/B:HIJO.0000032362.35354.bb. [DOI] [PubMed] [Google Scholar]
- 10.Karnoub AE, Dash AB, Vo AP, Sullivan A, Brooks MW, Bell GW, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449:557–563. doi: 10.1038/nature06188. [DOI] [PubMed] [Google Scholar]
- 11.Coussens LM, Raymond WW, Bergers G, Laig-Webster M, Behrendtsen O, Werb Z, et al. Inflammatory mast cells up-regulate angiogenesis during squamous epithelial carcinogenesis. Genes Dev. 1999;13:1382–1397. doi: 10.1101/gad.13.11.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iyengar P, Combs TP, Shah SJ, Gouon-Evans V, Pollard JW, Albanese C, et al. Adipocyte-secreted factors synergistically promote mammary tumorigenesis through induction of anti-apoptotic transcriptional programs and proto-oncogene stabilization. Oncogene. 2003;22:6408–6423. doi: 10.1038/sj.onc. 1206737. [DOI] [PubMed] [Google Scholar]
- 13.Erler JT, Bennewith KL, Nicolau M, Dornhofer N, Kong C, Le QT, et al. Lysyl oxidase is essential for hypoxia-induced metastasis. Nature. 2006;440:1222–1226. doi: 10.1038/nature04695. [DOI] [PubMed] [Google Scholar]
- 14.Paszek MJ, Zahir N, Johnson KR, Lakins JN, Rozenberg GI, Gefen A, et al. Tensional homeostasis and the malignant phenotype. Cancer Cell. 2005;8:241–254. doi: 10.1016/j.ccr.2005. 08.010. [DOI] [PubMed] [Google Scholar]
- 15.Bissell MJ, Aggeler J. Dynamic reciprocity: how do extracellular matrix and hormones direct gene expression? Prog Clin Biol Res. 1987;249:251–262. [PubMed] [Google Scholar]
- 16.Tlsty TD, Coussens LM. Tumor stroma and regulation of cancer development. Annu Rev Pathol. 2006;1:119–150. doi: 10.1146/annurev.pathol.1.110304.100224. [DOI] [PubMed] [Google Scholar]
- 17.Aumailley M, Gayraud B. Structure and biological activity of the extracellular matrix. J Mol Med. 1998;76:253–265. doi: 10.1007/s001090050215. [DOI] [PubMed] [Google Scholar]
- 18.Kass L, Erler JT, Dembo M, Weaver VM. Mammary epithelial cell: influence of extracellular matrix composition and organization during development and tumorigenesis. Int J Biochem Cell Biol. 2007;39:1987–1994. doi: 10.1016/j.biocel.2007.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinkus R, Lorenzen J, Schrader D, Lorenzen M, Dargatz M, Holz D. High-resolution tensor MR elastography for breast tumour detection. Phys Med Biol. 2000;45:1649–1664. doi: 10.1088/0031-9155/45/6/317. [DOI] [PubMed] [Google Scholar]
- 20.Myllyharju J, Kivirikko KI. Collagens, modifying enzymes and their mutations in humans, flies and worms. Trends Genet. 2004;20:33–43. doi: 10.1016/j.tig.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Vuorio E, de Crombrugghe B. The family of collagen genes. Annu Rev Biochem. 1990;59:837–872. doi: 10.1146/annurev.bi.59.070190.004201. [DOI] [PubMed] [Google Scholar]
- 22.Bosman FT, Stamenkovic I. Functional structure and composition of the extracellular matrix. J Pathol. 2003;200:423–428. doi: 10.1002/path.1437. [DOI] [PubMed] [Google Scholar]
- 23.Howe A, Aplin AE, Alahari SK, Juliano RL. Integrin signaling and cell growth control. Curr Opin Cell Biol. 1998;10:220–231. doi: 10.1016/S0955-0674(98)80144-0. [DOI] [PubMed] [Google Scholar]
- 24.Weaver VM, Lelievre S, Lakins JN, Chrenek MA, Jones JC, Giancotti F, et al. beta4 Integrin-dependent formation of polarized three-dimensional architecture confers resistance to apoptosis in normal and malignant mammary epithelium. Cancer Cell. 2002;2:205–216. doi: 10.1016/S1535-6108(02)00125-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bissell MJ, Radisky DC, Rizki A, Weaver VM, Petersen OW. The organizing principle: microenvironmental influences in the normal and malignant breast. Differentiation. 2002;70:537–546. doi: 10.1046/j.1432-0436.2002.700907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sugawara K, Tsuruta D, Ishii M, Jones JC, Kobayashi H. Laminin-332 and -511 in skin. Exp Dermatol. 2008;17:473–480. doi: 10.1111/j.1600-0625.2008.00721.x. [DOI] [PubMed] [Google Scholar]
- 27.Kalluri R. Basement membranes: structure, assembly and role in tumour angiogenesis. Nat Rev Cancer. 2003;3:422–433. doi: 10.1038/nrc1094. [DOI] [PubMed] [Google Scholar]
- 28.Paszek MJ, Weaver VM. The tension mounts: mechanics meets morphogenesis and malignancy. J Mammary Gland Biol Neoplasia. 2004;9:325–342. doi: 10.1007/s10911-004-1404-x. [DOI] [PubMed] [Google Scholar]
- 29.Discher DE, Janmey P, Wang YL. Tissue cells feel and respond to the stiffness of their substrate. Science. 2005;310:1139–1143. doi: 10.1126/science.1116995. [DOI] [PubMed] [Google Scholar]
- 30.Pedersen JA, Swartz MA. Mechanobiology in the third dimension. Ann Biomed Eng. 2005;33:1469–1490. doi: 10.1007/s10439-005-8159-4. [DOI] [PubMed] [Google Scholar]
- 31.Georges PC, Janmey PA. Cell type-specific response to growth on soft materials. J Appl Physiol. 2005;98:1547–1553. doi: 10.1152/japplphysiol.01121.2004. [DOI] [PubMed] [Google Scholar]
- 32.Janmey PA, Weitz DA. Dealing with mechanics: mechanisms of force transduction in cells. Trends Biochem Sci. 2004;29:364–370. doi: 10.1016/j.tibs.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Engler AJ, Sen S, Sweeney HL, Discher DE. Matrix elasticity directs stem cell lineage specification. Cell. 2006;126:677–689. doi: 10.1016/j.cell.2006.06.044. [DOI] [PubMed] [Google Scholar]
- 34.Zahir N, Lakins JN, Russell A, Ming W, Chatterjee C, Rozenberg GI, et al. Autocrine laminin-5 ligates alpha6beta4 integrin and activates RAC and NFkappaB to mediate anchor-age-independent survival of mammary tumors. J Cell Biol. 2003;163:1397–1407. doi: 10.1083/jcb.200302023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hotary KB, Allen ED, Brooks PC, Datta NS, Long MW, Weiss SJ. Membrane type I matrix metalloproteinase usurps tumor growth control imposed by the three-dimensional extracellular matrix. Cell. 2003;114:33–45. doi: 10.1016/S0092-8674(03) 00513-0. [DOI] [PubMed] [Google Scholar]
- 36.O’Brien LE, Jou TS, Pollack AL, Zhang Q, Hansen SH, Yurchenco P, et al. Rac1 orientates epithelial apical polarity through effects on basolateral laminin assembly. Nat Cell Biol. 2001;3:831–838. doi: 10.1038/ncb0901-831. [DOI] [PubMed] [Google Scholar]
- 37.Cukierman E, Pankov R, Stevens DR, Yamada KM. Taking cell-matrix adhesions to the third dimension. Science. 2001;294:1708–1712. doi: 10.1126/science.1064829. [DOI] [PubMed] [Google Scholar]
- 38.Yamada KM, Pankov R, Cukierman E. Dimensions and dynamics in integrin function. Braz J Med Biol Res. 2003;36:959–966. doi: 10.1590/S0100-879X2003000800001. [DOI] [PubMed] [Google Scholar]
- 39.Beacham DA, Cukierman E. Stromagenesis: the changing face of fibroblastic microenvironments during tumor progression. Semin Cancer Biol. 2005;15:329–341. doi: 10.1016/j.semcancer.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Bogenrieder T, Herlyn M. Cell-surface proteolysis, growth factor activation and intercellular communication in the progression of melanoma. Crit Rev Oncol Hematol. 2002;44:1–15. doi: 10.1016/S1040-8428(01)00196-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haass NK, Smalley KS, Li L, Herlyn M. Adhesion, migration and communication in melanocytes and melanoma. Pigment Cell Res. 2005;18:150–159. doi: 10.1111/j.1600-0749.2005. 00235.x. [DOI] [PubMed] [Google Scholar]
- 42.Yamada KM, Cukierman E. Modeling tissue morphogenesis and cancer in 3D. Cell. 2007;130:601–610. doi: 10.1016/j.cell.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 43.Emerman JT, Pitelka DR. Maintenance and induction of morphological differentiation in dissociated mammary epithelium on floating collagen membranes. In Vitro. 1977;13:316–328. doi: 10.1007/BF02616178. [DOI] [PubMed] [Google Scholar]
- 44.Barcellos-Hoff MH, Aggeler J, Ram TG, Bissell MJ. Functional differentiation and alveolar morphogenesis of primary mammary cultures on reconstituted basement membrane. Development. 1989;105:223–235. doi: 10.1242/dev.105.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leitinger B, Hohenester E. Mammalian collagen receptors. Matrix Biol. 2007;26:146–155. doi: 10.1016/j.matbio.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 46.Vogel WF, Abdulhussein R, Ford CE. Sensing extracellular matrix: an update on discoidin domain receptor function. Cell Signal. 2006;18:1108–1116. doi: 10.1016/j.cellsig.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 47.Avraamides CJ, Garmy-Susini B, Varner JA. Integrins in angiogenesis and lymphangiogenesis. Nat Rev Cancer. 2008;8(8):604–617. doi: 10.1038/nrc2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110:673–687. doi: 10.1016/S0092-8674(02) 00971-6. [DOI] [PubMed] [Google Scholar]
- 49.Morgan MR, Humphries MJ, Bass MD. Synergistic control of cell adhesion by integrins and syndecans. Nat Rev Mol Cell Biol. 2007;8:957–969. doi: 10.1038/nrm2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miranti CK, Brugge JS. Sensing the environment: a historical perspective on integrin signal transduction. Nat Cell Biol. 2002;4:E83–E90. doi: 10.1038/ncb0402-e83. [DOI] [PubMed] [Google Scholar]
- 51.Clark EA, Brugge JS. Integrins and signal transduction pathways: the road taken. Science. 1995;268:233–239. doi: 10.1126/science.7716514. [DOI] [PubMed] [Google Scholar]
- 52.Caswell PT, Norman JC. Integrin trafficking and the control of cell migration. Traffic. 2006;7:14–21. doi: 10.1111/j.1600-0854.2005.00362.x. [DOI] [PubMed] [Google Scholar]
- 53.Huang LE, Bindra RS, Glazer PM, Harris AL. Hypoxia-induced genetic instability—a calculated mechanism underlying tumor progression. J Mol Med. 2007;85:139–148. doi: 10.1007/s00109-006-0133-6. [DOI] [PubMed] [Google Scholar]
- 54.Lunt SJ, Chaudary N, Hill RP. The tumor microenvironment and metastatic disease. Clin Exp Metastasis. 2008 doi: 10.1007/s10585-008-9182-2. [DOI] [PubMed] [Google Scholar]
- 55.Parmar K, Mauch P, Vergilio JA, Sackstein R, Down JD. Distribution of hematopoietic stem cells in the bone marrow according to regional hypoxia. Proc Natl Acad Sci USA. 2007;104:5431–5436. doi: 10.1073/pnas.0701152104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Axelson H, Fredlund E, Ovenberger M, Landberg G, Pahlman S. Hypoxia-induced dedifferentiation of tumor cells–a mechanism behind heterogeneity and aggressiveness of solid tumors. Semin Cell Dev Biol. 2005;16:554–563. doi: 10.1016/j.semcdb.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 57.Hockel M, Vaupel P. Tumor hypoxia: definitions and current clinical, biologic, and molecular aspects. J Natl Cancer Inst. 2001;93:266–276. doi: 10.1093/jnci/93.4.266. [DOI] [PubMed] [Google Scholar]
- 58.Rodriguez PG, Felix FN, Woodley DT, Shim EK. The role of oxygen in wound healing: a review of the literature. Dermatol Surg. 2008 doi: 10.1111/j.1524-4725.2008.34254.x. [DOI] [PubMed] [Google Scholar]
- 59.Simon MC, Keith B. The role of oxygen availability in embryonic development and stem cell function. Nat Rev Mol Cell Biol. 2008;9:285–296. doi: 10.1038/nrm2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cartwright JE, Keogh RJ, Tissot van Patot MC. Hypoxia and placental remodelling. Adv Exp Med Biol. 2007;618:113–126. doi: 10.1007/978-0-387-75434-5_9. [DOI] [PubMed] [Google Scholar]
- 61.van Tuyl M, Liu J, Wang J, Kuliszewski M, Tibboel D, Post M. Role of oxygen and vascular development in epithelial branching morphogenesis of the developing mouse lung. Am J Physiol Lung Cell Mol Physiol. 2005;288:L167–L178. doi: 10.1152/ajplung.00185.2004. [DOI] [PubMed] [Google Scholar]
- 62.Pennacchietti S, Michieli P, Galluzzo M, Mazzone M, Giordano S, Comoglio PM. Hypoxia promotes invasive growth by transcriptional activation of the met protooncogene. Cancer Cell. 2003;3:347–361. doi: 10.1016/S1535-6108(03)00085-0. [DOI] [PubMed] [Google Scholar]
- 63.Semenza GL. Targeting HIF-1 for cancer therapy. Nat Rev Cancer. 2003;3:721–732. doi: 10.1038/nrc1187. [DOI] [PubMed] [Google Scholar]
- 64.Provot S, Schipani E. Fetal growth plate: a developmental model of cellular adaptation to hypoxia. Ann NY Acad Sci. 2007;1117:26–39. doi: 10.1196/annals.1402.076. [DOI] [PubMed] [Google Scholar]
- 65.Cowden Dahl KD, Robertson SE, Weaver VM, Simon MC. Hypoxia-inducible factor regulates alphavbeta3 integrin cell surface expression. Mol Biol Cell. 2005;16:1901–1912. doi: 10.1091/mbc.E04-12-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Radisky D, Hagios C, Bissell MJ. Tumors are unique organs defined by abnormal signaling and context. Semin Cancer Biol. 2001;11:87–95. doi: 10.1006/scbi.2000.0360. [DOI] [PubMed] [Google Scholar]
- 67.Mackie EJ, Chiquet-Ehrismann R, Pearson CA, Inaguma Y, Taya K, Kawarada Y, et al. Tenascin is a stromal marker for epithelial malignancy in the mammary gland. Proc Natl Acad Sci USA. 1987;84:4621–4625. doi: 10.1073/pnas.84.13.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kauppila S, Stenback F, Risteli J, Jukkola A, Risteli L. Aberrant type I and type III collagen gene expression in human breast cancer in vivo. J Pathol. 1998;186:262–268. doi: 10.1002/(SICI)1096-9896(1998110)186:3<262::AIDPATH191>3.0.CO;2–3. [DOI] [PubMed] [Google Scholar]
- 69.Zhu GG, Risteli L, Makinen M, Risteli J, Kauppila A, Stenback F. Immunohistochemical study of type I collagen and type I pN-collagen in benign and malignant ovarian neoplasms. Cancer. 1995;75:1010–1017. doi: 10.1002/1097-0142(19950215)75:4<1010::AID-CNCR2820750417>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 70.Strongin AY. Mislocalization and unconventional functions of cellular MMPs in cancer. Cancer Metastasis Rev. 2006;25:87–98. doi: 10.1007/s10555-006-7892-y. [DOI] [PubMed] [Google Scholar]
- 71.Jodele S, Blavier L, Yoon JM, DeClerck YA. Modifying the soil to affect the seed: role of stromal-derived matrix metalloproteinases in cancer progression. Cancer Metastasis Rev. 2006;25:35–43. doi: 10.1007/s10555-006-7887-8. [DOI] [PubMed] [Google Scholar]
- 72.Biondi ML, Turri O, Leviti S, Seminati R, Cecchini F, Bernini M, et al. MMP1 and MMP3 polymorphisms in promoter regions and cancer. Clin Chem. 2000;46:2023–2024. [PubMed] [Google Scholar]
- 73.Sternlicht MD, Lochter A, Sympson CJ, Huey B, Rougier JP, Gray JW, et al. The stromal proteinase MMP3/stromely-sin-1 promotes mammary carcinogenesis. Cell. 1999;98:137–146. doi: 10.1016/S0092-8674(00)81009-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Seandel M, Noack-Kunnmann K, Zhu D, Aimes RT, Quigley JP. Growth factor-induced angiogenesis in vivo requires specific cleavage of fibrillar type I collagen. Blood. 2001;97:2323–2332. doi: 10.1182/blood.V97.8.2323. [DOI] [PubMed] [Google Scholar]
- 75.Santala M, Simojoki M, Risteli J, Risteli L, Kauppila A. Type I and III collagen metabolites as predictors of clinical outcome in epithelial ovarian cancer. Clin Cancer Res. 1999;5:4091–4096. [PubMed] [Google Scholar]
- 76.Burns-Cox N, Avery NC, Gingell JC, Bailey AJ. Changes in collagen metabolism in prostate cancer: a host response that may alter progression. J Urol. 2001;166:1698–1701. doi: 10.1016/S0022-5347(05)65656-X. [DOI] [PubMed] [Google Scholar]
- 77.Ylisirnio S, Hoyhtya M, Makitaro R, Paaakko P, Risteli J, Kinnula VL, et al. Elevated serum levels of type I collagen degradation marker ICTP and tissue inhibitor of metalloproteinase (TIMP) 1 are associated with poor prognosis in lung cancer. Clin Cancer Res. 2001;7:1633–1637. [PubMed] [Google Scholar]
- 78.Clarijs R, Ruiter DJ, De Waal RM. Pathophysiological implications of stroma pattern formation in uveal melanoma. J Cell Physiol. 2003;194:267–271. doi: 10.1002/jcp.10214. [DOI] [PubMed] [Google Scholar]
- 79.Ruiter D, Bogenrieder T, Elder D, Herlyn M. Melanomastroma interactions: structural and functional aspects. Lancet Oncol. 2002;3:35–43. doi: 10.1016/S1470-2045(01)00620-9. [DOI] [PubMed] [Google Scholar]
- 80.Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell. 2006;124:263–266. doi: 10.1016/j.cell.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 81.Jain RK. Antiangiogenic therapy for cancer: current and emerging concepts. Oncology. 2005;19:7–16. Williston Park. [PubMed] [Google Scholar]
- 82.Clarijs R, Schalkwijk L, Ruiter DJ, de Waal RM. Lack of lymphangiogenesis despite coexpression of VEGF-C and its receptor Flt-4 in uveal melanoma. Invest Ophthalmol Vis Sci. 2001;42:1422–1428. [PubMed] [Google Scholar]
- 83.Clarijs R, Otte-Holler I, Ruiter DJ, de Waal RM. Presence of a fluid-conducting meshwork in xenografted cutaneous and primary human uveal melanoma. Invest Ophthalmol Vis Sci. 2002;43:912–918. [PubMed] [Google Scholar]
- 84.Hendrix MJ, Seftor EA, Hess AR, Seftor RE. Vasculogenic mimicry and tumour-cell plasticity: lessons from melanoma. Nat Rev Cancer. 2003;3:411–421. doi: 10.1038/nrc1092. [DOI] [PubMed] [Google Scholar]
- 85.Krouskop TA, Wheeler TM, Kallel F, Garra BS, Hall T. Elastic moduli of breast and prostate tissues under compression. Ultrason Imaging. 1998;20:260–274. doi: 10.1177/016173469802000403. [DOI] [PubMed] [Google Scholar]
- 86.Khaled W, Reichling S, Bruhns OT, Boese H, Baumann M, Monkman G, et al. Palpation imaging using a haptic system for virtual reality applications in medicine. Stud Health Technol Inform. 2004;98:147–153. doi: 10.1142/9789812702678_0055. [DOI] [PubMed] [Google Scholar]
- 87.Decitre M, Gleyzal C, Raccurt M, Peyrol S, Aubert-Foucher E, Csiszar K, et al. Lysyl oxidase-like protein localizes to sites of de novo fibrinogenesis in fibrosis and in the early stromal reaction of ductal breast carcinomas. Lab Invest. 1998;78:143–151. [PubMed] [Google Scholar]
- 88.Padera TP, Stoll BR, Tooredman JB, Capen D, di Tomaso E, Jain RK. Pathology: cancer cells compress intratumour vessels. Nature. 2004:427–695. doi: 10.1038/427695a. [DOI] [PubMed] [Google Scholar]
- 89.Huang S, Ingber DE. Cell tension, matrix mechanics, and cancer development. Cancer Cell. 2005;8:175–176. doi: 10.1016/j.ccr.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 90.Ingber DE. Can cancer be reversed by engineering the tumor microenvironment? Semin Cancer Biol. 2008;18:356–364. doi: 10.1016/j.semcancer.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bischoff F, Bryson G. Carcinogenesis through solid state surfaces. Prog Exp Tumor Res. 1964;5:85–133. doi: 10.1159/000385997. [DOI] [PubMed] [Google Scholar]
- 92.Ingber DE, Madri JA, Jamieson JD. Role of basal lamina in neoplastic disorganization of tissue architecture. Proc Natl Acad Sci USA. 1981;78:3901–3905. doi: 10.1073/pnas.78.6.3901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Maffini MV, Calabro JM, Soto AM, Sonnenschein C. Stromal regulation of neoplastic development: age-dependent normalization of neoplastic mammary cells by mammary stroma. Am J Pathol. 2005;167:1405–1410. doi: 10.1016/S0002-9440(10)61227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kenny PA, Bissell MJ. Tumor reversion: correction of malignant behavior by microenvironmental cues. Int J Cancer. 2003;107:688–695. doi: 10.1002/ijc.11491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Watanabe TK, Hansen LJ, Reddy NK, Kanwar YS, Reddy JK. Differentiation of pancreatic acinar carcinoma cells cultured on rat testicular seminiferous tubular basement membranes. Cancer Res. 1984;44:5361–5368. [PubMed] [Google Scholar]
- 96.Ingber DE, Madri JA, Jamieson JD. Basement membrane as a spatial organizer of polarized epithelia. Exogenous basement membrane reorients pancreatic epithelial tumor cells in vitro. Am J Pathol. 1986;122:129–139. [PMC free article] [PubMed] [Google Scholar]
- 97.Young SD, Marshall RS, Hill RP. Hypoxia induces DNA overreplication and enhances metastatic potential of murine tumor cells. Proc Natl Acad Sci USA. 1988;85:9533–9537. doi: 10.1073/pnas.85.24.9533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Erler JT, Cawthorne CJ, Williams KJ, Koritzinsky M, Wouters BG, Wilson C, et al. Hypoxia-mediated down-regulation of Bid and Bax in tumors occurs via hypoxia-inducible factor 1-dependent and -independent mechanisms and contributes to drug resistance. Mol Cell Biol. 2004;24:2875–2889. doi: 10.1128/MCB.24.7.2875-2889.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Graeber TG, Osmanian C, Jacks T, Housman DE, Koch CJ, Lowe SW, et al. Hypoxia-mediated selection of cells with diminished apoptotic potential in solid tumours. Nature. 1996;379:88–91. doi: 10.1038/379088a0. [DOI] [PubMed] [Google Scholar]
- 100.Tamamori M, Ito H, Hiroe M, Marumo F, Hata RI. Stimulation of collagen synthesis in rat cardiac fibroblasts by exposure to hypoxic culture conditions and suppression of the effect by natriuretic peptides. Cell Biol Int. 1997;21:175–180. doi: 10.1006/cbir.1997.0130. [DOI] [PubMed] [Google Scholar]
- 101.Lu SY, Wang DS, Zhu MZ, Zhang QH, Hu YZ, Pei JM. Inhibition of hypoxia-induced proliferation and collagen synthesis by vasonatrin peptide in cultured rat pulmonary artery smooth muscle cells. Life Sci. 2005;77:28–38. doi: 10.1016/j.lfs. 2004.11.026. [DOI] [PubMed] [Google Scholar]
- 102.Horino Y, Takahashi S, Miura T, Takahashi Y. Prolonged hypoxia accelerates the posttranscriptional process of collagen synthesis in cultured fibroblasts. Life Sci. 2002;71:3031–3045. doi: 10.1016/S0024-3205(02)02142-2. [DOI] [PubMed] [Google Scholar]
- 103.Kukacka J, Bibova J, Ruskoaho H, Pelouch V. Protein remodeling of extracellular matrix in rat myocardium during four-day hypoxia: the effect of concurrent hypercapnia. Gen Physiol Biophys. 2007;26:133–142. [PubMed] [Google Scholar]
- 104.Takahashi Y, Takahashi S, Shiga Y, Yoshimi T, Miura T. Hypoxic induction of prolyl 4-hydroxylase alpha (I) in cultured cells. J Biol Chem. 2000;275:14139–14146. doi: 10.1074/jbc.275.19.14139. [DOI] [PubMed] [Google Scholar]
- 105.Myllyharju J. Prolyl 4-hydroxylases, the key enzymes of collagen biosynthesis. Matrix Biol. 2003;22:15–24. doi: 10.1016/S0945-053X(03)00006-4. [DOI] [PubMed] [Google Scholar]
- 106.Le QT, Denko NC, Giaccia AJ. Hypoxic gene expression and metastasis. Cancer Metastasis Rev. 2004;23:293–310. doi: 10.1023/B:CANC.0000031768.89246.d7. [DOI] [PubMed] [Google Scholar]
- 107.Denko NC, Fontana LA, Hudson KM, Sutphin PD, Raychaudhuri S, Altman R, et al. Investigating hypoxic tumor physiology through gene expression patterns. Oncogene. 2003;22:5907–5914. doi: 10.1038/sj.onc.1206703. [DOI] [PubMed] [Google Scholar]
- 108.Kagan HM, Li W. Lysyl oxidase: properties, specificity, and biological roles inside and outside of the cell. J Cell Biochem. 2003;88:660–672. doi: 10.1002/jcb.10413. [DOI] [PubMed] [Google Scholar]
- 109.van den Hooff A. Stromal involvement in malignant growth. Adv Cancer Res. 1988;50:159–196. doi: 10.1016/S0065-230X (08)60437-6. [DOI] [PubMed] [Google Scholar]
- 110.Sappino AP, Schurch W, Gabbiani G. Differentiation repertoire of fibroblastic cells: expression of cytoskeletal proteins as marker of phenotypic modulations. Lab Invest. 1990;63:144–161. [PubMed] [Google Scholar]
- 111.Ronnov-Jessen L, Petersen OW, Bissell MJ. Cellular changes involved in conversion of normal to malignant breast: importance of the stromal reaction. Physiol Rev. 1996;76:69–125. doi: 10.1152/physrev.1996.76.1.69. [DOI] [PubMed] [Google Scholar]
- 112.Ingber DE, Madri JA, Jamieson JD. Neoplastic disorganization of pancreatic epithelial cell-cell relations. Role of basement membrane. Am J Pathol. 1985;121:248–260. [PMC free article] [PubMed] [Google Scholar]
- 113.Lu S, Huang M, Kobayashi Y, Komiyama A, Li X, Katoh R, et al. Alterations of basement membrane in di-isopropanolnitrosamine-induced carcinogenesis of the rat thyroid gland: an immunohistochemical study. Virchows Arch. 2000;436:595–601. doi: 10.1007/s004280000180. [DOI] [PubMed] [Google Scholar]
- 114.Ozzello L. The behavior of basement membranes in intraductal carcinoma of the breast. Am J Pathol. 1959;35:887–899. [PMC free article] [PubMed] [Google Scholar]
- 115.Luibel FJ, Sanders E, Ashworth CT. An electron microscopic study of carcinoma in situ and invasive carcinoma of the cervix uteri. Cancer Res. 1960;20:357–361. [PubMed] [Google Scholar]
- 116.Rubio CA, Biberfeld P. The basement membrane in experimentally induced atypias and carcinoma of the uterine cervix in mice. An immunofluorescence study. Virchows Arch A Pathol Anat Histol. 1979;381:205–209. doi: 10.1007/BF01257885. [DOI] [PubMed] [Google Scholar]
- 117.Lee JM, Dedhar S, Kalluri R, Thompson EW. The epithelial-mesenchymal transition: new insights in signaling, development, and disease. J Cell Biol. 2006;172:973–981. doi: 10.1083/jcb.200601018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Higgins DF, Kimura K, Bernhardt WM, Shrimanker N, Akai Y, Hohenstein B, et al. Hypoxia promotes fibrogenesis in vivo via HIF-1 stimulation of epithelial-to-mesenchymal transition. J Clin Invest. 2007;117:3810–3820. doi: 10.1172/JCI30487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lester RD, Jo M, Montel V, Takimoto S, Gonias SL. uPAR induces epithelial-mesenchymal transition in hypoxic breast cancer cells. J Cell Biol. 2007;178:425–436. doi: 10.1083/jcb.200701092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yang MH, Wu MZ, Chiou SH, Chen PM, Chang SY, Liu CJ, et al. Direct regulation of TWIST by HIF-1alpha promotes metastasis. Nat Cell Biol. 2008;10:295–305. doi: 10.1038/ncb1691. [DOI] [PubMed] [Google Scholar]
- 121.Farge E. Mechanical induction of twist in the Drosophila foregut/stomodeal primordium. Curr Biol. 2003;13:1365–1377. doi: 10.1016/S0960-9822(03)00576-1. [DOI] [PubMed] [Google Scholar]
- 122.Tschumperlin DJ, Shively JD, Kikuchi T, Drazen JM. Mechanical stress triggers selective release of fibrotic mediators from bronchial epithelium. Am J Respir Cell Mol Biol. 2003;28:142–149. doi: 10.1165/rcmb.2002-0121OC. [DOI] [PubMed] [Google Scholar]
- 123.Oft M, Peli J, Rudaz C, Schwarz H, Beug H, Reichmann E. TGF-beta1 and Ha-Ras collaborate in modulating the phenotypic plasticity and invasiveness of epithelial tumor cells. Genes Dev. 1996;10:2462–2477. doi: 10.1101/gad.10.19.2462. [DOI] [PubMed] [Google Scholar]
- 124.Miettinen PJ, Ebner R, Lopez AR, Derynck R. TGF-beta induced transdifferentiation of mammary epithelial cells to mesenchymal cells: involvement of type I receptors. J Cell Biol. 1994;127:2021–2036. doi: 10.1083/jcb.127.6.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hosobuchi M, Stampfer MR. Effects of transforming growth factor beta on growth of human mammary epithelial cells in culture. In Vitro Cell Dev Biol. 1989;25:705–713. doi: 10.1007/BF02623723. [DOI] [PubMed] [Google Scholar]
- 126.Akhurst RJ, Derynck R. TGF-beta signaling in cancer—a double-edged sword. Trends Cell Biol. 2001;11:S44–S51. doi: 10.1016/s0962-8924(01)02130-4. [DOI] [PubMed] [Google Scholar]
- 127.Waerner T, Alacakaptan M, Tamir I, Oberauer R, Gal A, Brabletz T, et al. ILEI: a cytokine essential for EMT, tumor formation, and late events in metastasis in epithelial cells. Cancer Cell. 2006;10:227–239. doi: 10.1016/j.ccr.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 128.Huang H, Kamm RD, Lee RT. Cell mechanics and mechanotransduction: pathways, probes, and physiology. Am J Physiol Cell Physiol. 2004;287:C1–C11. doi: 10.1152/ajpcell.00559.2003. [DOI] [PubMed] [Google Scholar]
- 129.Bershadsky AD, Balaban NQ, Geiger B. Adhesion-dependent cell mechanosensitivity. Annu Rev Cell Dev Biol. 2003;19:677–695. doi: 10.1146/annurev.cellbio.19.111301.153011. [DOI] [PubMed] [Google Scholar]
- 130.Bellovin DI, Simpson KJ, Danilov T, Maynard E, Rimm DL, Oettgen P, et al. Reciprocal regulation of RhoA and RhoC characterizes the EMT and identifies RhoC as a prognostic marker of colon carcinoma. Oncogene. 2006;25:6959–6967. doi: 10.1038/sj.onc.1209682. [DOI] [PubMed] [Google Scholar]
- 131.Reno F, Grazianetti P, Stella M, Magliacani G, Pezzuto C, Cannas M. Release and activation of matrix metalloproteinase-9 during in vitro mechanical compression in hypertrophic scars. Arch Dermatol. 2002;138:475–478. doi: 10.1001/archderm.138.4.475. [DOI] [PubMed] [Google Scholar]
- 132.Sullivan R, Graham CH. Hypoxia-driven selection of the metastatic phenotype. Cancer Metastasis Rev. 2007;26:319–331. doi: 10.1007/s10555-007-9062-2. [DOI] [PubMed] [Google Scholar]
- 133.van Kempen LC, Ruiter DJ, van Muijen GN, Coussens LM. The tumor microenvironment: a critical determinant of neoplastic evolution. Eur J Cell Biol. 2003;82:539–548. doi: 10.1078/0171-9335-00346. [DOI] [PubMed] [Google Scholar]
- 134.Berndt A, Borsi L, Hyckel P, Kosmehl H. Fibrillary co-deposition of laminin-5 and large unspliced tenascin-C in the invasive front of oral squamous cell carcinoma in vivo and in vitro. J Cancer Res Clin Oncol. 2001;127:286–292. doi: 10.1007/s004320000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mammoto A, Mammoto T, Ingber DE. Rho signaling and mechanical control of vascular development. Curr Opin Hematol. 2008;15:228–234. doi: 10.1097/MOH.0b013e3282fa7445. [DOI] [PubMed] [Google Scholar]
- 136.Milkiewicz M, Haas TL. Effect of mechanical stretch on HIF-1{alpha} and MMP-2 expression in capillaries isolated from overloaded skeletal muscles: laser capture microdissection study. Am J Physiol Heart Circ Physiol. 2005;289:H1315–H1320. doi: 10.1152/ajpheart.00284.2005. [DOI] [PubMed] [Google Scholar]
- 137.Harris AL. Hypoxia—a key regulatory factor in tumour growth. Nat Rev Cancer. 2002;2:38–47. doi: 10.1038/nrc704. [DOI] [PubMed] [Google Scholar]
- 138.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Moinfar F, Man YG, Arnould L, Bratthauer GL, Ratschek M, Tavassoli FA. Concurrent and independent genetic alterations in the stromal and epithelial cells of mammary carcinoma: implications for tumorigenesis. Cancer Res. 2000;60:2562–2566. [PubMed] [Google Scholar]
- 140.Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432:332–337. doi: 10.1038/nature03096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Yeung T, Georges PC, Flanagan LA, Marg B, Ortiz M, Funaki M, et al. Effects of substrate stiffness on cell morphology, cytoskeletal structure, and adhesion. Cell Motil Cytoskeleton. 2005;60:24–34. doi: 10.1002/cm.20041. [DOI] [PubMed] [Google Scholar]
- 142.Huang S, Ingber DE. The structural and mechanical complexity of cell-growth control. Nat Cell Biol. 1999;1:E131–E138. doi: 10.1038/13043. [DOI] [PubMed] [Google Scholar]
- 143.Ebihara T, Venkatesan N, Tanaka R, Ludwig MS. Changes in extracellular matrix and tissue viscoelasticity in bleomycin-induced lung fibrosis. Temporal aspects. Am J Respir Crit Care Med. 2000;162:1569–1576. doi: 10.1164/ajrccm.162.4.9912011. [DOI] [PubMed] [Google Scholar]
- 144.Chang HY, Sneddon JB, Alizadeh AA, Sood R, West RB, Montgomery K, et al. Gene expression signature of fibroblast serum response predicts human cancer progression: similarities between tumors and wounds. PLoS Biol. 2004;2:E7. doi: 10.1371/journal.pbio.0020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Olumi AF, Grossfeld GD, Hayward SW, Carroll PR, Tlsty TD, Cunha GR. Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res. 1999;59:5002–5011. doi: 10.1186/bcr138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bauer EA, Uitto J, Walters RC, Eisen AZ. Enhanced collagenase production by fibroblasts derived from human basal cell carcinomas. Cancer Res. 1979;39:4594–4599. [PubMed] [Google Scholar]
- 147.Knudson W, Biswas C, Toole BP. Interactions between human tumor cells and fibroblasts stimulate hyaluronate synthesis. Proc Natl Acad Sci USA. 1984;81:6767–6771. doi: 10.1073/pnas.81.21.6767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Willis RA. The unusual in tumour pathology. Can Med Assoc J. 1967;97:1466–1479. [PMC free article] [PubMed] [Google Scholar]
- 149.Colpaert CG, Vermeulen PB, Fox SB, Harris AL, Dirix LY, Van Marck EA. The presence of a fibrotic focus in invasive breast carcinoma correlates with the expression of carbonic anhydrase IX and is a marker of hypoxia and poor prognosis. Breast Cancer Res Treat. 2003;81:137–147. doi: 10.1023/A:1025702330207. [DOI] [PubMed] [Google Scholar]
- 150.Jacobs TW, Byrne C, Colditz G, Connolly JL, Schnitt SJ. Radial scars in benign breast-biopsy specimens and the risk of breast cancer. N Engl J Med. 1999;340:430–436. doi: 10.1056/NEJM199902113400604. [DOI] [PubMed] [Google Scholar]
- 151.Sieweke MH, Thompson NL, Sporn MB, Bissell MJ. Mediation of wound-related Rous sarcoma virus tumorigenesis by TGF-beta. Science. 1990;248:1656–1660. doi: 10.1126/science.2163544. [DOI] [PubMed] [Google Scholar]
- 152.Roberts AB, Sporn MB, Assoian RK, Smith JM, Roche NS, Wakefield LM, et al. Transforming growth factor type beta: rapid induction of fibrosis and angiogenesis in vivo and stimulation of collagen formation in vitro. Proc Natl Acad Sci USA. 1986;83:4167–4171. doi: 10.1073/pnas.83.12.4167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Unger M, Weaver VM. The tissue microenvironment as an epigenetic tumor modifier. Methods Mol Biol. 2003;223:315–347. doi: 10.1385/1-59259-329-1:315. [DOI] [PubMed] [Google Scholar]
- 154.Fringer J, Grinnell F. Fibroblast quiescence in floating collagen matrices: decrease in serum activation of MEK and Raf but not Ras. J Biol Chem. 2003;278:20612–20617. doi: 10.1074/jbc. M212365200. [DOI] [PubMed] [Google Scholar]
- 155.Erler JT, Giaccia AJ. Lysyl oxidase mediates hypoxic control of metastasis. Cancer Res. 2006;66:10238–10241. doi: 10.1158/0008-5472.CAN-06-3197. [DOI] [PubMed] [Google Scholar]
- 156.Egeblad M, Werb Z. New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer. 2002;2:161–174. doi: 10.1038/nrc745. [DOI] [PubMed] [Google Scholar]
- 157.de Visser KE, Korets LV, Coussens LM. Early neoplastic progression is complement independent. Neoplasia. 2004;6:768–776. doi: 10.1593/neo.04250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Dallas SL, Rosser JL, Mundy GR, Bonewald LF. Proteolysis of latent transforming growth factor-beta (TGF-beta)-binding protein-1 by osteoclasts. A cellular mechanism for release of TGF-beta from bone matrix. J Biol Chem. 2002;277:21352–21360. doi: 10.1074/jbc.M111663200. [DOI] [PubMed] [Google Scholar]
- 159.O’Reilly MS, Boehm T, Shing Y, Fukai N, Vasios G, Lane WS, et al. Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell. 1997;88:277–285. doi: 10.1016/S0092-8674(00)81848-6. [DOI] [PubMed] [Google Scholar]
- 160.Ramchandran R, Dhanabal M, Volk R, Waterman MJ, Segal M, Lu H, et al. Antiangiogenic activity of restin, NC10 domain of human collagen XV: comparison to endostatin. Biochem Biophys Res Commun. 1999;255:735–739. doi: 10.1006/bbrc.1999.0248. [DOI] [PubMed] [Google Scholar]
- 161.Colorado PC, Torre A, Kamphaus G, Maeshima Y, Hopfer H, Takahashi K, et al. Anti-angiogenic cues from vascular basement membrane collagen. Cancer Res. 2000;60:2520–2526. [PubMed] [Google Scholar]
- 162.Maeshima Y, Colorado PC, Torre A, Holthaus KA, Grunkemeyer JA, Ericksen MB, et al. Distinct antitumor properties of a type IV collagen domain derived from basement membrane. J Biol Chem. 2000;275:21340–21348. doi: 10.1074/jbc.M001956200. [DOI] [PubMed] [Google Scholar]
- 163.Coussens LM, Tinkle CL, Hanahan D, Werb Z. MMP-9 supplied by bone marrow-derived cells contributes to skin carcinogenesis. Cell. 2000;103:481–490. doi: 10.1016/S0092-8674(00)00139-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lin EY, Nguyen AV, Russell RG, Pollard JW. Colony-stimulating factor 1 promotes progression of mammary tumors to malignancy. J Exp Med. 2001;193:727–740. doi: 10.1084/jem. 193.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Lin EY, Gouon-Evans V, Nguyen AV, Pollard JW. The macrophage growth factor CSF-1 in mammary gland development and tumor progression. J Mammary Gland Biol Neoplasia. 2002;7:147–162. doi: 10.1023/A:1020399802795. [DOI] [PubMed] [Google Scholar]
- 166.Kobayashi A, Greenblatt RM, Anastos K, Minkoff H, Massad LS, Young M, et al. Functional attributes of mucosal immunity in cervical intraepithelial neoplasia and effects of HIV infection. Cancer Res. 2004;64:6766–6774. doi: 10.1158/0008-5472. CAN-04-1091. [DOI] [PubMed] [Google Scholar]
- 167.Lewis CE, Pollard JW. Distinct role of macrophages in different tumor microenvironments. Cancer Res. 2006;66:605–612. doi: 10.1158/0008-5472.CAN-05-4005. [DOI] [PubMed] [Google Scholar]
- 168.Skobe M, Hamberg LM, Hawighorst T, Schirner M, Wolf GL, Alitalo K, et al. Concurrent induction of lymphangiogenesis, angiogenesis, and macrophage recruitment by vascular endothelial growth factor-C in melanoma. Am J Pathol. 2001;159:893–903. doi: 10.1016/S0002-9440(10)61765-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Schoppmann SF, Birner P, Stockl J, Kalt R, Ullrich R, Caucig C, et al. Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral lymphangiogenesis. Am J Pathol. 2002;161:947–956. doi: 10.1016/S0002-9440(10)64255-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Knowles HJ, Harris AL. Macrophages and the hypoxic tumour microenvironment. Front Biosci. 2007;12:4298–4314. doi: 10.2741/2389. [DOI] [PubMed] [Google Scholar]
- 171.Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438:820–827. doi: 10.1038/nature04186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hiratsuka S, Watanabe A, Aburatani H, Maru Y. Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat Cell Biol. 2006;8:1369–1375. doi: 10.1038/ncb1507. [DOI] [PubMed] [Google Scholar]
- 173.Hiratsuka S, Nakamura K, Iwai S, Murakami M, Itoh T, Kijima H, et al. MMP9 induction by vascular endothelial growth factor receptor-1 is involved in lung-specific metastasis. Cancer Cell. 2002;2:289–300. doi: 10.1016/S1535-6108(02)00153-8. [DOI] [PubMed] [Google Scholar]
- 174.Chantrain CF, Shimada H, Jodele S, Groshen S, Ye W, Shalinsky DR, et al. Stromal matrix metalloproteinase-9 regulates the vascular architecture in neuroblastoma by promoting pericyte recruitment. Cancer Res. 2004;64:1675–1686. doi: 10.1158/0008-5472.CAN-03-0160. [DOI] [PubMed] [Google Scholar]
- 175.Masson V, de la Ballina LR, Munaut C, Wielockx B, Jost M, Maillard C, et al. Contribution of host MMP-2 and MMP-9 to promote tumor vascularization and invasion of malignant keratinocytes. FASEB J. 2005;19:234–236. doi: 10.1096/fj.04-2140fje. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Nelson CM, Jean RP, Tan JL, Liu WF, Sniadecki NJ, Spector AA, et al. Emergent patterns of growth controlled by multicellular form and mechanics. Proc Natl Acad Sci USA. 2005;102:11594–11599. doi: 10.1073/pnas.0502575102. [DOI] [PMC free article] [PubMed] [Google Scholar]