Abstract
The Framingham risk score (FRS) is widely used in clinical practice to identify subjects at high risk for developing coronary heart disease (CHD). However, FRS may not accurately identify subjects at risk. We measured subclinical atherosclerosis in the coronary arteries and aorta with the presence of calcium (CAC and AC, respectively) and in the common carotid artery by intima-media thickness (CIMT) in 498 healthy subjects. The distribution of these subclinical atherosclerosis measures was evaluated across 3 strata of the FRS. CAC, AC and CIMT were significantly independently associated with FRS. The FRS increased with the number of arterial sites with atherosclerosis. Sixty-nine percent of the subjects categorized in the low risk group (FRS<10%), 95% of the intermediate risk group (FRS 10–20%), and 100% of the high risk group (FRS>20%) had 1 or more vascular imaging studies demonstrating subclinical atherosclerosis. Among the low risk group, subjects with atherosclerosis had a longer history of lifetime smoking compared to those without atherosclerosis. In conclusion, subclinical atherosclerosis is prominent across the spectrum of FRS. Evaluation of subclinical atherosclerosis in different arterial sites in addition to FRS may be useful in targeting subjects for lifestyle and other interventions.
Keywords: Subclinical atherosclerosis, Framingham risk score, Carotid IMT, Coronary artery calcium, Aortic calcium
Introduction
We used baseline data from an ethnically diverse sample of men and women without clinical CVD to evaluate the relation between the Framingham 10-year risk for CHD (FRS) and prevalent subclinical atherosclerosis at 3 arterial sites. We also evaluated if increasing numbers of arterial sites with evident atherosclerosis correlate to higher FRS.
Methods
The B-Vitamin Atherosclerosis Intervention Trial (BVAIT) is a randomized, double-blind, placebo-controlled, clinical trial designed to test whether B-vitamin supplementation will reduce the progression of early carotid artery atherosclerosis in subjects with elevated fasting homocysteine, but without clinically evident CVD. Briefly, potential subjects were prescreened by telephone and met initial screening eligibility if they were at least 40 years of age, postmenopausal (for women), and reported no evidence of diabetes, heart disease, stroke, or cancer.
A total of 2,355 subjects met telephone prescreening criteria, and attended at least 1 screening visit. At the screening visits, participants reported on smoking and alcohol use using structured questionnaires. Blood pressure and anthropometric measurements were obtained, body mass index (BMI) was calculated, and laboratory tests including fasting lipids and homocysteine levels were measured. Subjects were eligible for randomization to the trial (n=506) if they had fasting plasma total homocysteine levels ≥8.5 umol/L, and were excluded from randomization on the basis of any clinical signs or symptoms of cardiovascular disease, diabetes or fasting serum glucose ≥140 mg/dL, triglyceride levels ≥150 mg/dL, serum creatinine >1.6 mg/dL, systolic blood pressure ≥160 mmHg and /or diastolic blood pressure ≥100 mmHg, untreated thyroid disease, life threatening disease with prognosis <5 years, or alcohol intake >5 drinks per day or substance abuse.
Subjects who were randomized underwent carotid artery ultrasound and coronary artery and aortic CT scans prior to randomization and at scheduled intervals during the trial. All subjects provided written informed consent. The study was approved by the Institutional Review Board of the University of Southern California.
Participants fasted for at least 8 hours prior to blood draws. Briefly, total plasma cholesterol and triglyceride levels were measured using an enzymatic method of the Standardization Program of the National Centers for Disease Control and Prevention 1. High-density lipoprotein cholesterol levels were measured after lipoproteins containing apolipoprotein B were precipitated in whole plasma using heparin manganese chloride. Low-density lipoprotein cholesterol levels were estimated using the Friedewald equation.
For each subject, a Framingham score was calculated assigning gender-specific points for age, smoking, diabetes, blood pressure, LDL-cholesterol and HDL-cholesterol 2. The gender-specific Framingham risk equations were then used to calculate the predicted risk of developing CHD events over the next 10 years 2,3. Subjects were divided into 3 risk categories based on their 10-year FRS: low risk group (<10%), intermediate risk (10% – 20%), and high risk (>20%) according to the National Cholesterol Education Program (NCEP) Adult Treatment Panel III guidelines 4.
Multidetector spiral computed tomography methodology using an Mx-8000 4-S-CT scanner (Philips, formerly Marconi, Cleveland, Ohio) was used to image the coronary arteries and thoracic abdominal aorta. High resolution scanning of the heart was begun at the level of the carina (determined from a scout film) and proceeded caudally through the cardiac apex. A single breath-hold (during inspiration) procedure was used. Simultaneous acquisition of 4 slices and fast rotation time restricted the breath-hold time to less than 15 seconds. Prospective electrocardiographic triggering (set at 50% of the expected next RR interval) in sequential slice mode at 120 kV and 165 mAs was used for scanning of the heart. Contiguous, noninterlaced slices were acquired with a table increment of 20 mm every series of 4 slices. Two sets of 28 contiguous 5 mm slices were obtained and reconstructed in a 35 cm field of view that included a tissue-equivalent calibration phantom pad under the participant’s thorax 5,6. Following acquisition of the heart images, high resolution scanning of the abdomen was begun at the tip of the xyphoid process and proceeded caudally through the level of the umbilicus for a total scanning distance of 20.15 cm. A single breath-hold (during inspiration) procedure with a breath-hold time less than 15 seconds was used. Helical scanning mode at 120 kV and 180 mAs with a table speed of 3 cm/sec and pitch of 6 was used for scanning the abdomen. One set of 31 total slices 5 mm thick was reconstructed in a 30 cm field of view that included the calibration phantom pad under the participant’s abdomen spanning from the xyphoid process to below the umbilicus.
Scans were analyzed by image analysts using validated calcium scoring software 7. For each subject, total calcium scores were calculated, based on number of calcific lesions viewed, using scoring software based on the Agatston method 8.
High resolution B-mode ultrasound of the right carotid artery, for the purpose of measuring CIMT (details of the standardized procedure have been noted elsewhere 1,9), were obtained on all randomized subjects using a linear-array 7.5 MHz transducer attached to a Toshiba SSH-140 imaging system (Toshiba Corp., Tokyo, Japan ) 1. Far wall IMT of the common carotid artery was measured using an in-house developed software package1,9.
Dichotomized measures of CAC and AC were defined as a calcium score>0. Elevated carotid atherosclerosis was defined as CIMT>0.83 mm (the >75th percentile of the CIMT distribution in the total sample). Logistic regression models were used to assess the association of CAC, AC and elevated CIMT with gender and racial/ethnic group. The association between these 3 measures of subclinical atherosclerosis and 10-year FRS was also assessed by logistic regression. The mean 10-year FRS for each atherosclerosis outcome was compared between gender and across racial/ethnic groups using one way ANOVA. At each of the 3 arterial sites, the mean values of calcium or CIMT were compared in subjects with elevated atherosclerosis by racial/ethnic groups. For each subject, the number of atherosclerosis sites (CAC>0, AC>0 or CIMT>0.83 mm) was counted. One-way ANOVA was used to evaluate the association between the total number of atherosclerosis sites (independent variable) and 10-year FRS (dependent variables). Coronary and aortic calcium scores were log transformed and used as continuous variables in a linear regression model where all 3 atherosclerosis measures were tested for independence of association with 10-year FRS (the dependent variable in the model). Nominal scores (0.00001) were assigned to calcium scores of ‘0’.
Results
Baseline data on all 3 atherosclerosis measures were available on 498 of 506 randomized subjects. Table 1 summarizes the demographics and other cardiovascular risk factors of these subjects. The mean (SD) age of the participants was 61(10) years ranging from 40 to 88 years and 61% were male. The majority of the participants (66%) were non-Hispanic White, 14% were Black, 11% Hispanic and 9% were Asian. Thirty-seven percent of the subjects had smoked regularly in their lifetime. Overall, the study participants were overweight and total- and LDL-cholesterol were mildly elevated. However, HDL-cholesterol and blood pressure were within normal range.
Table 1.
Characteristics of the study participants (n=498)
| Characteristics | |
|---|---|
| Age (years) | 61 (10)* |
| Male | 303 (61%) |
| Female | 195 (39%) |
| White | 327 (66%) |
| Black | 72 (14%) |
| Hispanic | 55 (11%) |
| Asian | 44 (9%) |
| Body mass index (kg/m2) | 28 (4.9) |
| Smoking | 184 (37%) |
| Total cholesterol (mg/dl) | 211.6 (35) |
| High density lipoprotein cholesterol (mg/dl) | 57.3 (15.1) |
| Low density lipoprotein cholesterol (mg/dl) | 128.4 (30.7) |
| Systolic blood pressure (mmHg) | 127 (16) |
| Diastolic blood pressure (mmHg) | 79 (9) |
| †Framingham risk score (%) | 10.2 (7.5) |
Mean (standard deviation) for continuous variables
Framingham 10-year coronary heart disease risk
The overall mean (SD) 10-year FRS was 10.2% (7.5%). In men it was 13% (8%) whereas in women it was 6% (3%) (p<.0001). In men, 45% were in the low 10-year CHD risk group, 39% in the intermediate risk group and 16% in the high risk group, whereas 90% of the women were in the low risk group, 10% in the intermediate and none in the high risk group (chi-square p<.0001). The overlap in the prevalence of subclinical atherosclerosis across the 3 arterial sites is displayed in the Venn diagram (Fig. 1). Of 498 subjects with data from all 3 vascular beds, 106 (21%) had no atherosclerosis evident at any of the arterial sites, 164 (33%) had 1 arterial site involved, 160 (32%) had 2 arterial sites involved and 68 (14%) had all 3 arterial sites involved.
Figure 1.
Distribution of subclinical atherosclerosis measured at 3 vascular beds.
Note: Numbers in the Venn diagram represent the percentage of the total population included in the study (n=498).
CAC = Coronary artery calcium (> 0)
AC = Aortic calcium (> 0)
CIMT = Carotid artery intima-media thickness (>0.83 mm)
Males had a 3-fold greater risk of having CAC than women (OR=3.29; 95% CI=2.23–4.86, Table 2). Compared with Whites, Blacks and Hispanics were significantly less likely to have CAC (OR=0.30; 95% CI=0.16–0.54, OR=0.51; 95% CI=0.28–0.93, respectively).
Table 2.
Association between atherosclerosis outcomes, gender, and race.
| Odds ratio (95% Confidence interval) | p-value | |
|---|---|---|
| Coronary artery calcium | ||
| Female | 1.0 | |
| Male | 3.29 (2.23–4.86) | <.0001 |
| White | 1.0 | |
| Black | 0.30 (0.16–0.54) | <.0001 |
| Hispanic | 0.51 (0.28–0.93) | 0.03 |
| Asian | 1.14 (0.61–2.15) | 0.67 |
| Aortic calcium | ||
| Female | 1.0 | |
| Male | 0.85 (0.57–1.26) | 0.41 |
| White | 1.0 | |
| Black | 0.40 (0.24–0.67) | 0.0006 |
| Hispanic | 0.62 (0.34–1.14) | 0.13 |
| Asian | 1.07 (0.52–2.21) | 0.85 |
| Carotid artery intima-media thickness > 0.83mm | ||
| Female | 1.0 | |
| Male | 1.64(1.06–2.53) | 0.03 |
| White | 1.0 | |
| Black | 1.17 (0.66–07) | 0.60 |
| Hispanic | 0.68 (0.33–1.40) | 0.29 |
| Asian | 1.27 (0.64–2.55) | 0.49 |
Gender was not associated with the presence of AC. Compared with Whites, Blacks were 60% less likely to have AC (OR=0.40; 95% CI=0.24–0.67). The presence of AC in Hispanics and Asians did not differ from Whites. Compared to women, men were 1.64 times more likely to have thicker CIMT (OR=1.64, 95% CI=1.06–2.53). The racial groups did not differ according to the presence of elevated CIMT.
Overall, the prevalence of CAC and AC was 44% and 70%, respectively. By definition, 25% of the subjects had thicker CIMT (above the 75th percentile of the CIMT distribution). The Pearson’s correlation coefficients of CIMT and log-transformed calcium scores were: 0.21 between CIMT and CAC (p<.0001), 0.28 between CIMT and AC (p<.0001), and 0.37 between CAC and AC scores (p<.0001).
The mean 10-year FRS was significantly greater in each of the 3 atherosclerosis groups (p for difference<.0001 for all 3 conditions, Table 3). With each percent increase in the 10-year FRS the risk of having CAC increased by 14% (OR=1.14: 95% CI=1.10–1.18), AC by 15% (OR=1.15: 95% CI=1.10–1.21), and the risk of having CIMT >0.83 mm increased by 7% (OR=1.07: 95% CI=1.04–1.10) (Table 3).
Table 3.
Association of atherosclerosis outcomes with Framingham 10-year risk of coronary heart disease.
| Atherosclerosis outcomes | N (%) | Framingham risk score (%) Mean (standard deviation) | †Odds ratio (95% Confidence interval) |
|---|---|---|---|
| Coronary artery calcium | |||
| No | 281 (56%) | 7.7 (5.0) | |
| Yes | 217 (44%) | 13.5 (8.9) | 1.14 (1.10–1.18) |
| Aortic calcium | |||
| No | 151 (30%) | 6.9 (4.7) | |
| Yes | 347 (70%) | 11.6 (8.0) | 1.15 (1.10–1.21) |
| Carotid artery intima-media thickness | |||
| ≤0.83 mm | 374 (75%) | 9.2 (6.7) | |
| >0.83 mm | 124 (25%) | 13.2 (8.9) | 1.07 (1.04–1.10) |
Odds ratio per unit percent of Framingham risk score
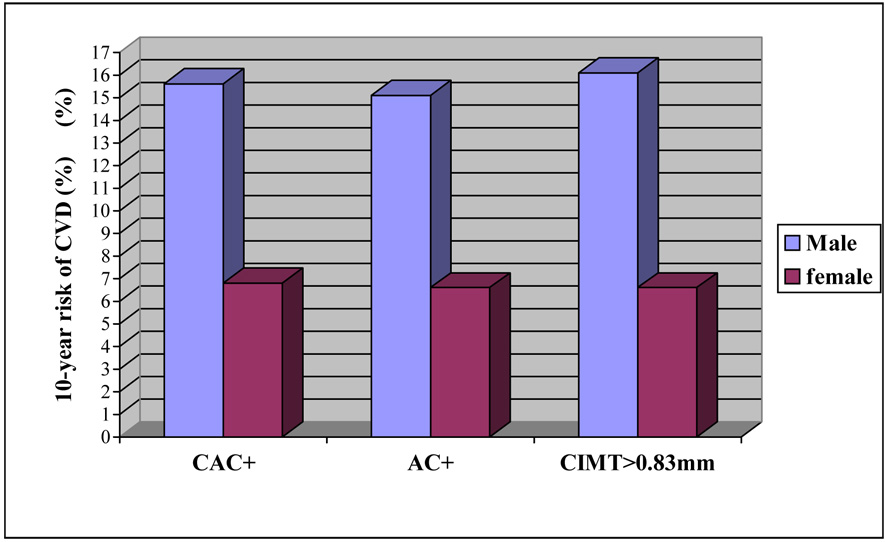
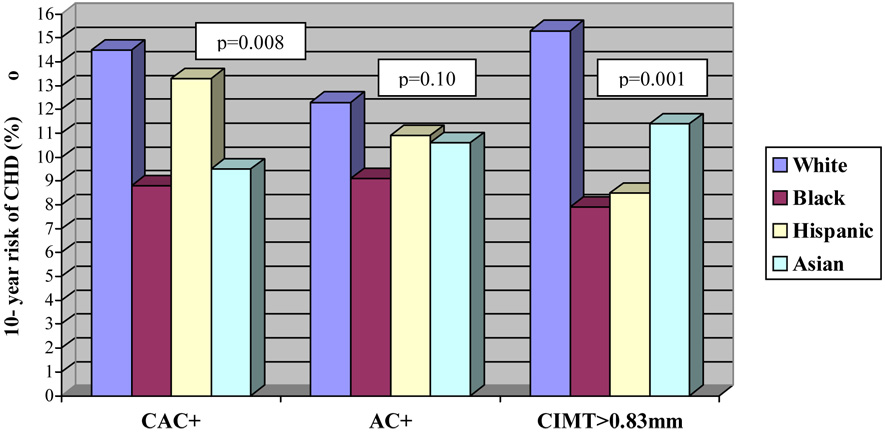
Among subjects with atherosclerosis measures, the mean 10-year FRS was significantly higher in men than in women for each of the 3 atherosclerotisis measures (p for difference<.0001 for each atherosclerosis measure, Fig. 2). Among prevalent CAC cases, mean (SE) 10-year FRS was significantly different across the racial/ethnic groups (p for difference = 0.008, Fig. 3), with the 10-year risk highest among Whites (14.5% (0.7%)), followed by Hispanics (13.3% (2%)), Asians (9.5% (1.8%)), and lowest in Blacks (8.8% (2.2%)). Among persons with CIMT > 0.83 mm, Whites had the highest 10-year FRS (15.3% (0.9%)), followed by Asians (11.4% (2.3%)), Hispanics (8.5% (2.7%)), and Blacks (7.9% (1.9%)) (p for difference across races= 0.001). However, among prevalent AC cases, the mean 10-year FRS did not significantly differ across the racial/ethnic groups (p=0.10).
Figure 2.
Framingham 10-year risk of CHD for 3 atherosclerosis measures by gender
Figure 3.
Framingham 10-year risk of CHD for 3 atherosclerosis measures by race
CAC, AC and CIMT were each independently related to the 10-year FRS (Table 4). The CAC score had the highest contribution (standardized β=0.32, p<.0001), whereas CIMT had the lowest contribution to the 10-year FRS (standardized β=0.15, p=0.0003).
Table 4.
Association between continuous atherosclerosis measures and Framingham 10-year risk of coronary heart disease
| Measures of atherosclerosis† | Framingham risk score | |
|---|---|---|
| Standardized β estimate | p-value | |
| *Coronary calcium | 0.32 | <.0001 |
| *Aortic calcium | 0.17 | <.0001 |
| Carotid artery intima-media thickness | 0.15 | 0.0003 |
Calcium scores were log transformed.
All 3 measures were considered continuous.
There was a positive linear relationship between the number of sites with atherosclerosis and the 10-year FRS (p for trend<.0001). Subjects who had evidence of atherosclerosis at any 1 of the 3 arterial sites had a mean (SE) 10-year FRS of 8.7% (0.5%), those who had any 2 of the 3 sites involved had a mean (SE) 10-year FRS of 12.5% (0.5%), and those who had evidence of atherosclerosis in all 3 arterial sites had a mean (SE) 10-year FRS of 15.6% (0.8%) (Fig. 4).
Figure 4.
Framingham 10-year risk of CHD by number of vascular beds with atherosclerosis
In the low risk category of FRS, 69% of subjects had subclinical atherosclerosis in at least 1 vascular bed (37% in 1, 24% in 2 and 8% in 3 vascular beds) (Fig. 5). Compared to the 31% of low risk subjects without atherosclerosis, subjects in the low risk category with any atherosclerosis were more likely to be female, less educated, had lower income, higher fasting homocysteine levels, and longer duration of lifetime smoking and increased frequency (number of cigarettes smoked/day) of smoking (all p<0.003; Table 5). Low risk subjects with atherosclerosis were also more likely to have a positive family history of CVD, however the difference was not statistically significant (p=0.13). In a multivariate linear regression model including all the factors that significantly differed between low risk subjects with and without atherosclerosis, only the number of years of smoking remained statistically significantly associated with presence of atherosclerosis (p=0.02).
Figure 5.
Framingham risk categories by number of vascular beds with atherosclerosis
Table 5.
Comparison of subjects in the low Framingham risk category with and without subclinical atherosclerosis
| Risk factors | Atherosclerosis not present (n=98) |
Atherosclerosis present (n=214) |
p-value | |
|---|---|---|---|---|
| Gender | 0.0006 | |||
| Male | 57(58%) | 80(37%) | ||
| Female | 41(42%) | 134(63%) | ||
| Education | 0.01 | |||
| Some college or less | 28(29%) | 93(37%) | ||
| College or more | 70 (71%) | 120(63%) | ||
| Income (per year) | 0.009 | |||
| <49,999 | 13(13%) | 57(28%) | ||
| 50,000 to 89,999 | 28(29%) | 62(31%) | ||
| 90,000 to 99,999 | 18(19%) | 35(17%) | ||
| 100,000 or more | 38(39%) | 48(24%) | ||
| Fasting homocysteine (umol/L), mean (standard deviation) | 8.8(1.9) | 9.9(4.9) | 0.006 | |
| †Lifetime smoking history | ||||
| Frequency, mean (standard deviation) | Average number of cigarettes smoked/day | 5.5(7.9) | 9.8(11.8) | 0.02 |
| Duration, mean (standard deviation) | Total number of years smoked | 12.8(8.0) | 21.0(13.8) | 0.001 |
| Family history | 0.13 | |||
| No | 82(85%) | 167(78%) | ||
| Yes | 14(15%) | 47(22%) |
Among smokers only (n = 92, 19 in the no atherosclerosis and 73 in the atherosclerosis group)
Discussion
Our data indicate that the CAC, AC, and CIMT are independently associated with the Framingham 10-year CHD risk estimate. We also report that the 10-year FRS increases steadily with increasing number of prevalent atherosclerosis sites in asymptomatic individuals.
The FRS is a useful tool for identifying subjects at relatively higher risk of CHD to implement primary prevention interventions. FRS has been shown to be significantly associated with CAC and CIMT in asymptomatic young adults 10,11. Epidemiologic studies have also documented that increased CIMT and CAC are directly associated with each other in asymptomatic adults as well as in subjects with CHD 12,13. One epidemiologic study also reported a close correlation between coronary and aortic calcification 14.
However, it is not known how the prevalence of atherosclerosis assessed across multiple vascular beds relates to FRS in the same study sample. We measured subclinical atherosclerosis in 3 vascular beds and observed significant correlation amongst CAC, AC and CIMT. The strongest correlation was found between CAC and AC (r = 0.37) and the weakest correlation was between CIMT and CAC (r = 0.21); correlations that likely reflect different stages of the same process.
A recent study among 292 subjects from the Framingham offspring cohort reported correlations of similar magnitude across 3 subclinical atherosclerosis measures 15. We also found that all 3 measures of subclinical atherosclerosis were independently associated with FRS, indicating possible differential pathogenesis of atherosclerosis across vascular beds. These results suggest the utility of evaluating more than one vascular bed for subclinical atherosclerosis.
Our finding of a strong positive correlation between the FRS and increasing prevalence of atherosclerosis is consistent with the Framingham offspring cohort study and with the Healthy Women Study (HWS). In 274 postmenopausal women participating in HWS, subclinical atherosclerosis measured by the presence of calcium in the coronary arteries and aorta and by CIMT in the carotid artery was associated with significantly higher levels of CVD risk factors assessed by the composite Framingham score 16. In the Cardiovascular Health Study, subclinical atherosclerosis in multiple vascular beds was independently associated with increased risk of clinical cardiovascular disease 17. It appears that assessing subclinical atherosclerosis in multiple arterial sites may yield a better estimate of disease risk than FRS alone. In an epidemiologic study, CHD prediction was improved when CAC was added to the conventional FRS 18.
Our data indicate substantial ethnic variation in the prevalence and severity of calcium scores (Table 2). Consistent with previous reports, we observed significantly lower prevalence of CAC among Black and Hispanic individuals compared to White subjects 19–22. Unlike CAC, ethnic variation in AC has not been examined thoroughly. In our data, the prevalence of AC was also significantly lower in Blacks compared to Whites. Consistent with these differences in calcium score, Black subjects also had significantly lower 10-year FRS compared to Whites. These data indicate that race is an important determinant of CHD risk prediction and calcium score, a finding not apparent with CIMT.
Although FRS is widely used for estimating CHD risk, evidence suggests a low predictive capability of FRS, particularly in the low risk category with FRS<10% 23–25. A considerable number of subjects in the low risk category of FRS tend to have subclinical atherosclerosis. In our data, 63% (n=312) of the subjects were in the low risk category; 69% of them (n=214) had evidence of subclinical atherosclerosis. Of the 68 subjects who had subclinical atherosclerosis in all 3 vascular beds, 35% had a 10-year FRS of CHD <10%, 41% were categorized in the intermediate risk group, and only 23% were categorized in the high risk group. Probable reasons for this underestimation of subclinical atherosclerosis could be the limitation of FRS, which does not account for some important CHD risk factors such as family history of CHD, previous history of CHD, race, obesity, and systemic diseases such as systemic lupus erythematosis or rheumatoid arthritis 11,23,24,26–28. We found that history of lifetime smoking, homocysteine levels and markers of socioeconomic status such as education and income play an important role in identifying persons with subclinical atherosclerosis amongst the low risk population identified by FRS.
A limitation to the generalizibility of these findings could be that trial inclusion required homocysteine levels ≥8.5 µmol/L. However, the mean (SD) fasting homocysteine levels of our study population was 9.6 (3.6) µmol/L and 75% of them had a serum homocysteine level ≤10.7 µmol/L, which is similar to a population based study of healthy men and women in the Atherosclerosis Risk in Communities Study where 75% of the population had homocysteine levels ≤10 µmol/L29. It is unlikely that our results were influenced by the selection criteria of homocysteine levels.
Acknowledgments
This work is supported by NIH R01-AG17160
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hodis HN, Mack WJ, Lobo RA, Shoupe D, Sevanian A, Mahrer PR, Selzer RH, Liu Cr CR, Liu Ch CH, Azen SP. Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2001;135:939–953. doi: 10.7326/0003-4819-135-11-200112040-00005. [DOI] [PubMed] [Google Scholar]
- 2.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 3.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 4.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) Jama. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 5.Detrano R, Kang X, Mahaisavariya P, Tang W, Colombo A, Molloi S, Garner D, Nickerson S. Accuracy of quantifying coronary hydroxyapatite with electron beam tomography. Invest Radiol. 1994;29:733–738. doi: 10.1097/00004424-199408000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Mahaisavariya P, Detrano R, Kang X, Garner D, Vo A, Georgiou D, Molloi S, Brundage BH. Quantitation of in vitro coronary artery calcium using ultrafast computed tomography. Cathet Cardiovasc Diagn. 1994;32:387–393. doi: 10.1002/ccd.1810320421. [DOI] [PubMed] [Google Scholar]
- 7.Yaghoubi S, Tang W, Wang S, Reed J, Hsiai J, Detrano R, Brundage B. Offline assessment of atherosclerotic coronary calcium from electron beam tomograms. Am J Card Imaging. 1995;9:231–236. [PubMed] [Google Scholar]
- 8.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 9.Selzer RH, Mack WJ, Lee PL, Kwong-Fu H, Hodis HN. Improved common carotid elasticity and intima-media thickness measurements from computer analysis of sequential ultrasound frames. Atherosclerosis. 2001;154:185–193. doi: 10.1016/s0021-9150(00)00461-5. [DOI] [PubMed] [Google Scholar]
- 10.Kieltyka L, Urbina EM, Tang R, Bond MG, Srinivasan SR, Berenson GS. Framingham risk score is related to carotid artery intima-media thickness in both white and black young adults: the Bogalusa Heart Study. Atherosclerosis. 2003;170:125–130. doi: 10.1016/s0021-9150(03)00244-2. [DOI] [PubMed] [Google Scholar]
- 11.Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, Lauer RM. Usefulness of the Framingham risk score and body mass index to predict early coronary artery calcium in young adults (Muscatine Study) Am J Cardiol. 2001;88:509–515. doi: 10.1016/s0002-9149(01)01728-3. [DOI] [PubMed] [Google Scholar]
- 12.Davis PH, Dawson JD, Mahoney LT, Lauer RM. Increased carotid intimal-medial thickness and coronary calcification are related in young and middle-aged adults. The Muscatine study. Circulation. 1999;100:838–842. doi: 10.1161/01.cir.100.8.838. [DOI] [PubMed] [Google Scholar]
- 13.Terry JG, Carr JJ, Tang R, Evans GW, Kouba EO, Shi R, Cook DR, Vieira JL, Espeland MA, Mercuri MF, Crouse JR., 3rd Coronary artery calcium outperforms carotid artery intima-media thickness as a noninvasive index of prevalent coronary artery stenosis. Arterioscler Thromb Vasc Biol. 2005;25:1723–1728. doi: 10.1161/01.ATV.0000173418.42264.19. [DOI] [PubMed] [Google Scholar]
- 14.Adler Y, Fisman EZ, Shemesh J, Schwammenthal E, Tanne D, Batavraham IR, Motro M, Tenenbaum A. Spiral computed tomography evidence of close correlation between coronary and thoracic aorta calcifications. Atherosclerosis. 2004;176:133–138. doi: 10.1016/j.atherosclerosis.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 15.Kathiresan S, Larson MG, Keyes MJ, Polak JF, Wolf PA, D'Agostino RB, Jaffer FA, Clouse ME, Levy D, Manning WJ, O'Donnell CJ. Assessment by cardiovascular magnetic resonance, electron beam computed tomography, and carotid ultrasonography of the distribution of subclinical atherosclerosis across Framingham risk strata. Am J Cardiol. 2007;99:310–314. doi: 10.1016/j.amjcard.2006.08.028. [DOI] [PubMed] [Google Scholar]
- 16.Sutton-Tyrrell K, Kuller LH, Matthews KA, Holubkov R, Patel A, Edmundowicz D, Newman A. Subclinical atherosclerosis in multiple vascular beds: an index of atherosclerotic burden evaluated in postmenopausal women. Atherosclerosis. 2002;160:407–416. doi: 10.1016/s0021-9150(01)00591-3. [DOI] [PubMed] [Google Scholar]
- 17.Kuller LH, Shemanski L, Psaty BM, Borhani NO, Gardin J, Haan MN, O'Leary DH, Savage PJ, Tell GS, Tracy R. Subclinical disease as an independent risk factor for cardiovascular disease. Circulation. 1995;92:720–726. doi: 10.1161/01.cir.92.4.720. [DOI] [PubMed] [Google Scholar]
- 18.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. Jama. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 19.Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, Ouyang P, Jackson S, Saad MF. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]
- 20.Budoff MJ, Georgiou D, Brody A, Agatston AS, Kennedy J, Wolfkiel C, Stanford W, Shields P, Lewis RJ, Janowitz WR, Rich S, Brundage BH. Ultrafast computed tomography as a diagnostic modality in the detection of coronary artery disease: a multicenter study. Circulation. 1996;93:898–904. doi: 10.1161/01.cir.93.5.898. [DOI] [PubMed] [Google Scholar]
- 21.Doherty TM, Tang W, Detrano RC. Racial differences in the significance of coronary calcium in asymptomatic black and white subjects with coronary risk factors. J Am Coll Cardiol. 1999;34:787–794. doi: 10.1016/s0735-1097(99)00258-2. [DOI] [PubMed] [Google Scholar]
- 22.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2006;113:30–37. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 23.Akosah KO, Schaper A, Cogbill C, Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the National Cholesterol Education Panel III guidelines perform? J Am Coll Cardiol. 2003;41:1475–1479. doi: 10.1016/s0735-1097(03)00187-6. [DOI] [PubMed] [Google Scholar]
- 24.Hecht HS. Impact of plaque imaging by electron beam tomography on the treatment of dyslipidemias. Am J Cardiol. 2001;88:406–408. doi: 10.1016/s0002-9149(01)01688-5. [DOI] [PubMed] [Google Scholar]
- 25.Michos ED, Vasamreddy CR, Becker DM, Yanek LR, Moy TF, Fishman EK, Becker LC, Blumenthal RS. Women with a low Framingham risk score and a family history of premature coronary heart disease have a high prevalence of subclinical coronary atherosclerosis. Am Heart J. 2005;150:1276–1281. doi: 10.1016/j.ahj.2005.02.037. [DOI] [PubMed] [Google Scholar]
- 26.Chung CP, Oeser A, Avalos I, Gebretsadik T, Shintani A, Raggi P, Sokka T, Pincus T, Stein CM. Utility of the Framingham risk score to predict the presence of coronary atherosclerosis in patients with rheumatoid arthritis. Arthritis Res Ther. 2006;8:R186. doi: 10.1186/ar2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chung CP, Oeser A, Avalos I, Raggi P, Stein CM. Cardiovascular risk scores and the presence of subclinical coronary artery atherosclerosis in women with systemic lupus erythematosus. Lupus. 2006;15:562–569. doi: 10.1177/0961203306071870. [DOI] [PubMed] [Google Scholar]
- 28.Michos ED, Nasir K, Rumberger JA, Vasamreddy C, Braunstein JB, Budoff MJ, Blumenthal RS. Relation of family history of premature coronary heart disease and metabolic risk factors to risk of coronary arterial calcium in asymptomatic subjects. Am J Cardiol. 2005;95:655–657. doi: 10.1016/j.amjcard.2004.10.045. [DOI] [PubMed] [Google Scholar]
- 29.Schreiner PJ, Wu KK, Malinow MR, Stinson VL, Szklo M, Nieto FJ, Heiss G. Hyperhomocyst(e)inemia and hemostatic factors: the atherosclerosis risk in communities study. Ann Epidemiol. 2002;12:228–236. doi: 10.1016/s1047-2797(01)00311-8. [DOI] [PubMed] [Google Scholar]