Abstract
Laparoscopic partial adrenalectomy is a surgical option for select patients with hereditary pheochromocytoma. We present a case of a pediatric patient with von Hippel-Lindau disease (VHL) and both an adrenal pheochromocytoma and an extra-adrenal pheochromocytoma, who underwent concurrent partial adrenalectomy and extra-adrenal pheochromocytoma resection utilizing robotic assistance. To the best of our knowledge, this is the first report of partial adrenalectomy with concurrent extra-adrenal pheochromocytoma resection.
Introduction
Patients with von Hippel-Lindau disease (VHL) are at risk for developing hereditary adrenal pheochromocytomas in both adrenal glands.1 Partial adrenalectomy may provide patients with tumor control while preserving adrenocortical function, thus decreasing the risk of subsequent adrenal insufficiency, as well as the morbidity of lifelong adrenal steroid replacement. Indications for partial adrenalectomy include bilateral and hereditary adrenal tumors, as well as tumors in a solitary adrenal gland. The safety and feasibility of partial adrenalectomy using minimally-invasive techniques has been reported by several groups.1–5 Although a single report of robotic partial adrenalectomy has been described for an adult with VHL,6 it has not been described in the pediatric population or for an extra-adrenal pheochromocytoma. We present a case of a pediatric VHL patient with both an adrenal and an extra-adrenal mass, who was managed utilizing robotic assistance in a single procedure.
Case Report
A 14-year-old boy with VHL was found to have bilateral adrenal masses on surveillance abdominal imaging. A computed tomography (CT) scan demonstrated a large complex mass measuring 3.0 cm adjacent to the left adrenal gland, and a smaller 0.9-cm nodule near the apex of the left adrenal gland (Fig. 1). An I131-metaiodobenzylguanidine scintigraphy scan confirmed increased activity in the left adrenal gland. The patient was asymptomatic and normotensive, but had elevated serum catecholamines (norepinephrine and normetanephrine levels were 2.5 times the normal range). Preoperative blockade was performed using metyrosine and phenoxybenzamine. The patient and family elected for adrenal-sparing surgery utilizing a minimally-invasive approach. The decision was made to utilize robotic assistance because it was felt that it might facilitate precise dissection of the adrenal tumor and adjacent extra-adrenal tumor to help spare the adrenal gland.
FIG. 1.

CT scan demonstrating a 3.0-cm left extra-adrenal mass (solid arrow) with a 0.9-cm left adrenal nodule in the apex of the left adrenal gland (dashed arrow).
The patient was moved into modified flank position, pneumoperitoneum was achieved with a Veress needle, and trocars were placed, including a 12-mm trocar for the camera between the umbilicus and left costal margin, and two 8-mm robotic trocars (Intuitive Surgical, Sunnyvale, CA) along the left costal margin. Assistant ports consisted of a 12-mm trocar inferior to the camera port and a 5-mm trocar superior to the camera port.
The robot was docked and the colon and spleen were mobilized using a transabdominal approach to fully expose the adrenal gland. Using a flexible laparoscopic ultrasonography probe, the extra-adrenal and adrenal tumors were located and the margins of resection of the partially endophytic adrenal tumor were defined (Fig. 2). The adrenal vein was dissected and ligated using Hem-o-lok clips. The extra-adrenal tumor was removed using robotic Maryland bipolar forceps, monopolar scissors, and Hem-o-lok clips. Partial adrenalectomy was then performed for the apical adrenal tumor. The robotic monopolar scissors were used to sharply and bluntly dissect the enucleation plane between the tumor and normal adrenal tissue. The robotic bipolar forceps and monopolar scissors were used to maintain hemostasis while cutting through adrenal tissue to maintain a clear view of the plane of tumor resection. The adrenal tumors were placed in a specimen retrieval bag for removal.
FIG. 2.

Intraoperative view of robotic partial adrenalectomy. The clear view of the operative field and precision afforded by the robotic system facilitated dissection of the tumor from the normal adrenal gland.
The operative time was 180 minutes and the blood loss was 150 mL. The patient had an uneventful hospital course and no complications, but remained in the hospital on the pediatric endocrinology service for blood pressure monitoring until discharge on postoperative day 4. Final pathologic examination revealed a pheochromocytoma surrounded by ganglion and peripheral nerve tissue for both the extra-adrenal mass and the partial adrenalectomy specimen (Fig. 3). Surgical margins were free of tumor in both specimens.
FIG. 3.
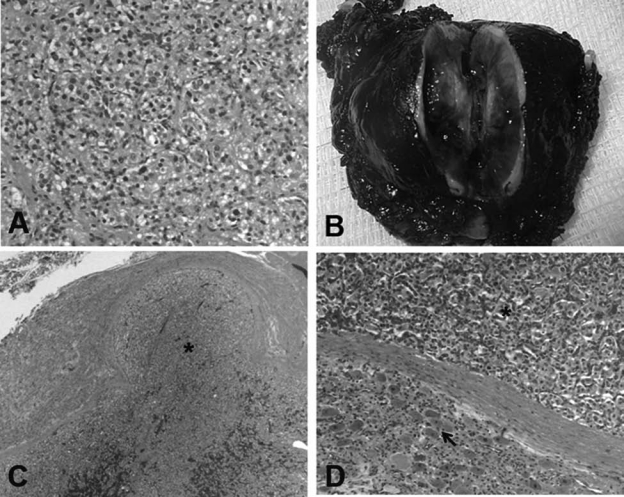
Adrenal and extra-adrenal pheochromocytoma. (A) Representative section of adrenal tumor showing small nests of polygonal cells with amphophilic cytoplasm and round nuclei. Immunohistochemical studies performed showed positivity for chromogranin and synaptophysin, while sustentacular cells are highlighted by S-100 (data not shown) (hematoxylin and eosin, original magnification 10×). (B) Gross and histologic appearance of the extra-adrenal mass. (C) The tumor (asterisk) is surrounded by ganglion and peripheral nerve tissue (hematoxylin and eosin, original magnification 2×). The histologic features are consistent with an extra-adrenal pheochromocytoma. (D) Higher magnification view of ganglion cells (arrow) juxtaposed to the pheochromocytoma (asterisk) (hematoxylin and eosin, original magnification 10×).
Discussion
The safety and efficacy of robotic adrenalectomy has been described previously.7 However, there is only a single case report of robot-assisted partial adrenalectomy,6 and there are no reports in the literature of robotic resection of an extra-adrenal pheochromocytoma. Our report of robotic partial adrenalectomy is unique in that it was done on a pediatric patient with robotic resection of a large extra-adrenal pheochromocytoma concurrently with a partial adrenalectomy. To the best of our knowledge, we are the first to describe robotic extra-adrenalectomy and robotic partial adrenalectomy in a pediatric patient managed concurrently in a single procedure.
The potential advantages of robotic assistance for complex partial adrenalectomy cases include a magnified three-dimensional image and articulating robotic instruments, that may facilitate precise dissection, tumor excision, and hemostasis. We recognize that a complex partial adrenalectomy such as this could be performed laparoscopically by surgeons skilled in this technique, and we have reported our own experience with laparoscopic partial adrenalectomy.1,2 We are not advocating robotic assistance for all partial adrenalectomy procedures. We feel that robotic assistance may have helped in this case via the precise dissection and tumor excision that is possible with this modality, and it helped us to spare the adrenal gland.
Robotic partial adrenalectomy for hereditary adrenal pheochromocytoma is feasible in the setting of an adjacent extra-adrenal pheochromocytoma and a pediatric patient.
Abbreviations Used
- CT
computed tomography
- VHL
von Hippel-Lindau disease
Acknowledgment
This work was funded by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research.
References
- 1.Walther MM. Herring J. Choyke PL. Linehan WM. Laparoscopic partial adrenalectomy in patients with hereditary forms of pheochromocytoma. J Urol. 2000;164:14–17. [PubMed] [Google Scholar]
- 2.Diner EK. Franks ME. Behari A. Linehan WM. Walther MM. Partial adrenalectomy: The National Cancer Institute experience. Urology. 2005;66:19–23. doi: 10.1016/j.urology.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 3.Janetschek G. Finkenstedt G. Gasser R. Waibel UG. Peschel R. Bartsch G. Neumann HP. Laparoscopic surgery for pheochromocytoma: Adrenalectomy, partial resection, excision of paragangliomas. J Urol. 1998;160:330–334. doi: 10.1016/s0022-5347(01)62886-6. [DOI] [PubMed] [Google Scholar]
- 4.Sasagawa I. Suzuki Y. Itoh K. Izumi T. Miura M. Suzuki H. Tomita Y. Posterior retroperitoneoscopic partial adrenalectomy: Clinical experience in 47 procedures. Eur Urol. 2003;43:381–385. doi: 10.1016/s0302-2838(03)00087-3. [DOI] [PubMed] [Google Scholar]
- 5.Walz MK. Peitgen K. Diesing D, et al. Partial versus total adrenalectomy by the posterior retroperitoneoscopic approach: Early and long-term results of 325 consecutive procedures in primary adrenal neoplasias. World J Surg. 2004;28:1323–1329. doi: 10.1007/s00268-004-7667-y. [DOI] [PubMed] [Google Scholar]
- 6.Julien JS. Ball D. Schulick R. Robot-assisted cortical-sparing adrenalectomy in a patient with Von Hippel-Lindau disease and bilateral pheochromocytomas separated by 9 years. J Laparoendosc Adv Surg Tech A. 2006;16:473–477. doi: 10.1089/lap.2006.16.473. [DOI] [PubMed] [Google Scholar]
- 7.Winter JM. Talamini MA. Stanfield CL. Chang DC. Hundt JD. Dackiw AP. Campbell KA. Schulick RD. Thirty robotic adrenalectomies: A single institution's experience. Surg Endosc. 2006;20:119–124. doi: 10.1007/s00464-005-0082-0. [DOI] [PubMed] [Google Scholar]


