Abstract
BACKGROUND:
The Thrombolysis In Myocardial Infarction (TIMI) risk index for the prediction of 30-day mortality was developed and validated in patients with ST-segment elevation myocardial infarction (STEMI) who were being treated with thrombolytics in randomized clinical trials. When tested in clinical registries of patients with STEMI, the index performed poorly in an older (65 years and older) Medicare population, but it was a good predictor of early death among the more representative population on the National Registry of Myocardial Infarction-3 and -4 databases. It has not been tested in a population outside the United States or among non-STEMI patients.
METHODS:
The TIMI risk index was applied to the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study cohort of 11,510 acute MI patients from Ontario. The model’s discriminatory capacity and calibration were tested in all patients and in subgroups determined by age, sex, diagnosis and reperfusion status.
RESULTS:
The TIMI risk index was strongly associated with 30-day mortality for both STEMI and non-STEMI patients. The C statistic was 0.82 for STEMI and 0.80 for non-STEMI patients, with overlapping 95% CI. The discriminatory capacity was somewhat lower for patients older than 65 years of age (0.74). The model was well calibrated.
CONCLUSIONS:
The TIMI risk index is a simple, valid and moderately accurate tool for the stratification of risk for early death in STEMI and non-STEMI patients in the community setting. Its routine clinical use is warranted.
Keywords: Coronary disease, Myocardial infarction, Risk factors
Abstract
CONTEXTE :
L’indice de risque TIMI (Thrombolysis In Myocardial Infarction) relativement à la prédiction de la mortalité au bout de 30 jours a été mis au point et validé chez des patients ayant subi un infarctus du myocarde (IM) avec sus-décalage du segment ST et traités par thrombolyse dans le cadre d’essais cliniques avec hasardisation. Lorsque l’indice a été vérifié dans des registres cliniques de patients ayant subi un IM avec sus-décalage du ST, celui-ci s’est révélé un mauvais prédicteur dans une population âgée (plus de 65 ans), protégée par le régime Medicare, mais s’est révélé un bon prédicteur de mortalité précoce dans une population plus représentative des patients inscrits dans les bases de données du National Registry of Myocardial Infarction 3 et 4. L’indice n’a pas été vérifié dans des populations vivant à l’extérieur des États-Unis ou chez des patients ayant subi un IM sans sus-décalage du ST.
MÉTHODE :
L’indice de risque TIMI a été appliqué à une cohorte de 11 510 patients de l’Ontario, ayant subi un infarctus aigu du myocarde et participant à l’étude Enhanced Feedback for Effective Cardiac Treatment (EFFECT). La capacité discriminante du modèle et son calage ont été vérifiés chez tous les patients et dans des sous-groupes de patients déterminés selon l’âge, le sexe, le diagnostic et le degré de reperfusion.
RÉSULTATS :
L’indice de risque TIMI a été fortement associé à la mortalité au bout de 30 jours tant chez les patients ayant subi un IM avec sus-décalage du ST que chez ceux ayant subi un IM sans sus-décalage du ST. La valeur C statistique était de 0,82 dans les cas de sus-décalage et de 0,80 dans les cas d’absence de sus-décalage, avec chevauchement de l’intervalle de confiance à 95 %. La capacité discriminante était un peu plus faible chez les patients âgés de 65 ans et plus (0,74), mais le modèle était bien calé.
CONCLUSION :
L’indice de risque TIMI est un outil simple, valide et assez précis de classification du risque de mortalité précoce chez les patients ayant subi un IM avec ou sans sus-décalage du segment ST, dans la collectivité. Son application en pratique clinique est justifiée.
Risk stratification is part of clinical prognostication. Acute myocardial infarction (AMI) is associated with high early mortality, and the Thrombolysis In Myocardial Infarction (TIMI) risk index is one of the more recent models developed to identify high-risk patients.
The TIMI Investigators have used randomized clinical trial findings to develop risk stratification models for patients with unstable angina (UA)/non-ST-segment elevation myocardial infarction (non-STEMI) (1) and STEMI (2). From the ‘TIMI risk score for STEMI’, a simplified ‘TIMI risk index’ was developed (3). The TIMI risk index is based on age, heart rate (HR) and systolic blood pressure (SBP) alone, so it may be calculated at the time of first contact with the medical system. It has been advocated as a means of rapid and early triage of patients with STEMI. Proponents see the potential to improve outcomes, especially when a range of resources is available for an out-of-hospital diagnosis, which can lead to prehospital administration of fibrinolytics or rapid transport and access to primary percutaneous coronary intervention (PCI) (4).
The TIMI risk index initially failed to show that it could be generalized to the wider population. Discrimination and calibration were poor among nearly 50,000 older (older than 65 years) Medicare patients on the Cooperative Cardiovascular Project (CCP) database (5), with deaths being underestimated in each of the five predetermined risk categories. Risk categories were based on the quintiles of the TIMI risk index from the validation study in the Intravenous nPA for Treatment of Infarcting Myocardium Early (InTIME II) trial (3) of fibrinolysis in patients with STEMI. The authors of the CCP study cautioned that prognostic models developed in clinical trial populations had limited value in the general population.
Subsequently, the TIMI risk index was tested in more than 150,000 patients with STEMI from the National Registry of Myocardial Infarction (NRMI)-3 and -4 databases (6). Although the NRMI captures only in-hospital mortality and data are provided by hospitals that choose to participate, the age structure of the registry patients is more representative of the general population. The discriminatory capacity of the simple TIMI risk index was good, and the proportions of observed deaths in groups based on 10-point ranges, rather than the randomized clinical trial-derived quintiles, were broadly concordant with those expected. The authors of the NRMI study suggest that the TIMI risk index could be used in the prehospital setting or at presentation as a practical tool for rapid risk stratification of patients with AMI.
We sought to evaluate the utility of the TIMI risk index in the predetermined 10-point range classification used in the NRMI-3 and -4 databases for the prediction of 30-day mortality in a Canadian population-based cohort. Because the components of the score (age, SBP and HR) are common predictors found in cardiovascular risk models, we aimed to test the performance of the index in both STEMI and non-STEMI patients.
METHODS
The Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study (7) is a randomized controlled trial of the effectiveness of ‘report cards’ on indicators of quality in improving the care of patients with cardiovascular disease in Ontario. In brief, patients hospitalized between April 1, 1999, and March 31, 2001, with a ‘most responsible’ diagnosis of AMI were identified from the Canadian Institute for Health Information Discharge Abstract Database (8) using the International Classification of Diseases, 9th revision (9), code 410. Patients with AMI as an in-hospital complication were excluded. A random sample of approximately 125 patient records was drawn from 103 (of 104 eligible) participating hospitals in Ontario.
Validation of an AMI case before data abstraction required that two of the following three variables be present: characteristic electrocardiogram (ECG) changes; pain of assumed ischemic origin; or elevated cardiac enzymes or markers. The early data collection period predated the redefinition of AMI based on cardiac troponin testing (10), which was not routinely performed throughout Ontario during the study period. Vital status at 30 days was obtained via record linkage to the Ontario Registered Persons Database, and the number of coronary interventions within 30 days was obtained from the Ontario Myocardial Infarction Database. This study design provided a population-based cohort for the study of AMI outcomes.
The EFFECT study cohort for the present validation study was restricted to those with the necessary information for calculation of the TIMI risk index and those who met the published criteria for inclusion. Excluded patients were those whose HR were outside the range of 50 beats/min to 150 beats/min (3) or those who were in cardiogenic shock (6) on admission, because they were considered to be in need of specific intervention.
Research ethics boards approved the study protocol at each of the participating health centres.
Definitions
A diagnosis of STEMI was based on findings from the ECG recorded on admission, or a subsequent diagnostic ECG and confirmation by a physician’s signature or note in the medical record. Peak values for cardiac markers of greater than the upper limit of normal for the local laboratory or, if not available, creatine kinase levels of greater than twice the upper limit of normal were considered positive. Reperfusion therapy was either thrombolysis or primary PCI (less than 3%) as the primary intervention within 12 h of arrival.
Statistical methods
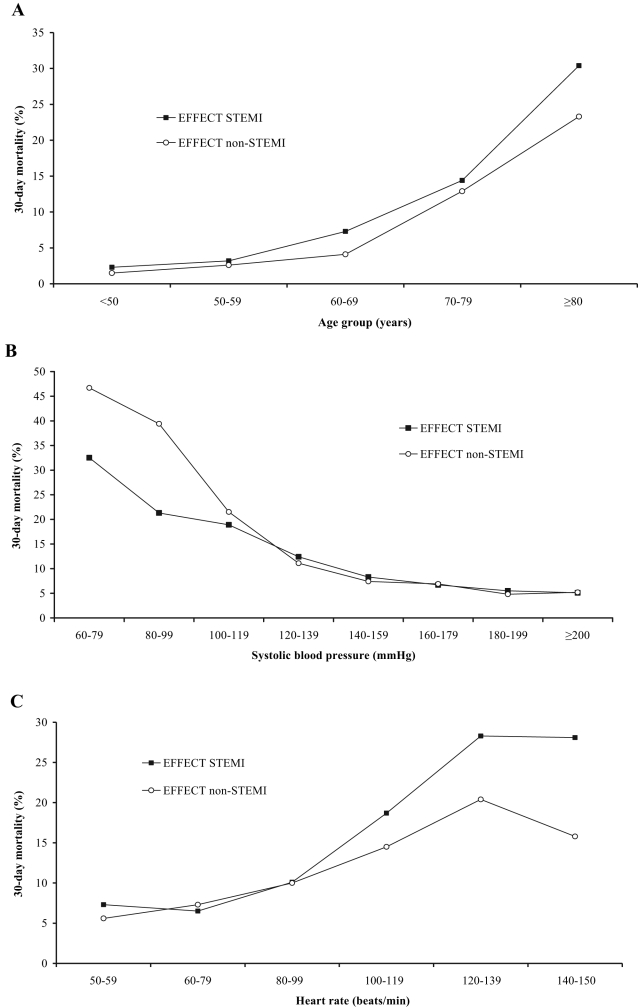
Thirty-day mortality was plotted for both STEMI and non-STEMI patients against the increments of age, SBP and HR used by the authors of the index (3).
The TIMI risk index for each patient was calculated using an equation (HR × [age/10]2/SBP) and used as a continuous variable to describe receiver operating characteristic curves (11). The discriminatory capacity of the index for 30-day mortality in all patients, as well as in subgroups determined by age (65 years or younger and older than 65 years of age), sex, diagnosis of STEMI or non-STEMI and reperfusion status for STEMI patients, is reported as the C statistic and 95% CI. The continuous score was also used in logistic regression analyses to determine the risk for 30-day mortality.
Scores were also divided into the 10-point range groups used in the NRMI-3 and -4 databases (6). The distribution of the risk groups in the EFFECT study population was assessed, and differences in distribution among groups were tested with the Mann-Whitney U test. Differences in 30-day mortality across risk groups were assessed using the χ2 test for trends. The 30-day mortality observed in each 10-point range risk group for the EFFECT study cohort was plotted against that predicted to test the calibration of the TIMI risk index.
RESULTS
The TIMI risk index was calculated for 98.9% of the 11,510 patients in the EFFECT study AMI database (n=198 missing data). Less than 1% of data were missing in any component variable of the risk index. Vital status to 30 days was available for all patients. Crude 30-day mortality was 12.1% for the whole cohort and 11.8% for the 11,376 patients with the variables needed to calculate the TIMI risk index.
Thirty-day mortality was high (31.0%) among the 1023 patients excluded. This high-risk group included those with vital signs outside the predetermined range (n=646), those in cardiogenic shock (n=257) on admission, and those missing either HR or SBP data; 19.4% of excluded patients died within two days of arrival, compared with 3.7% of the included patients. Excluded patients were an average of six years older, and 59% were diagnosed with STEMI.
There were 10,487 patients in the study cohort, 5057 (48%) of whom were diagnosed with STEMI. Patients with STEMI were younger, and were more likely to be male and current smokers. They were less likely to have a comorbid disease or a previous coronary event than those with non-STEMI (Table 1). The majority of STEMI patients (58.5%) were given reperfusion therapy, and the differences in demographics and medical history between these patients and those not given reperfusion therapy were the same as those noted for STEMI and non-STEMI patients.
TABLE 1.
Baseline characteristics of the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study patients
| EFFECT study (n=10,487) | Non-STEMI (n=5430) | STEMI (n=5057) | STEMI, given RT (n=2958) | STEMI, no RT (n=2099) | |
|---|---|---|---|---|---|
| Women, % | 35.8 | 38.7 | 32.7 | 28.2 | 39.3 |
| Median age, years (IQR) | 69.5 (57–78) | 72 (61–80) | 66 (55–76) | 62 (53–72) | 71.5 (60–80) |
| Patients >65 years of age, % | 60.4 | 67.6 | 52.7 | 43.9 | 65.2 |
| Medical history, % | |||||
| Prior myocardial infarction | 22.8 | 28.0 | 17.2 | 13.7 | 22.1 |
| Prior percutaneous coronary intervention | 3.2 | 3.6 | 2.8 | 2.8 | 2.8 |
| Prior coronary artery bypass graft | 6.7 | 9.1 | 4.2 | 2.7 | 6.2 |
| Congestive heart failure | 4.8 | 6.4 | 3.0 | 1.5 | 5.1 |
| Diabetes | 26.0 | 29.6 | 22.0 | 18.5 | 27.0 |
| Current smoker | 32.6 | 27.6 | 38.0 | 42.8 | 31.4 |
| Hypertension | 45.9 | 49.0 | 42.6 | 38.9 | 47.8 |
| Cerebrovascular accident | 7.9 | 9.0 | 6.8 | 3.8 | 11.0 |
| Characteristics on admission | |||||
| Anterior myocardial infarction, % | – | – | 55.8 | 52.6 | 60.3 |
| Median heart rate, beats/min (IQR) | 81 (69–98) | 84 (71–100) | 79 (67–94) | 75 (64–88) | 84 (71–101) |
| Median systolic blood pressure, mmHg (IQR) | 148 (128–169) | 150 (130–170) | 146 (127–167) | 147 (128–168) | 144 (126–165) |
| Procedures within 30 days, % | |||||
| Angiography | – | 24.0 | 30.0 | – | – |
| Percutaneous coronary intervention | – | 8.2 | 14.5 | – | – |
| Coronary artery bypass graft | – | 5.7 | 5.0 | – | – |
IQR Interquartile range; RT Reperfusion therapy; STEMI ST-segment elevation myocardial infarction
Figure 1 shows the relationships between the component factors of the TIMI risk index (age, SBP, HR) and 30-day mortality. There was a similar association between decile of age and mortality for STEMI and non-STEMI patients, with the curve steepening after the seventh decile. The inverse relationship between SBP and mortality was more pronounced for non-STEMI patients at the lower levels, while an HR greater than 100 beats/min was associated with higher mortality for patients with STEMI than with non-STEMI.
Figure 1).
Relationship between age (A), systolic blood pressure (B), heart rate (C) and mortality at 30 days among patients with ST-segment elevation myocardial infarction (STEMI) and non-STEMI in the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study population
TIMI risk index
The median TIMI risk index for the EFFECT study patients was 25.5 (interquartile range [IQR] 17 to 32) overall, 19.8 (IQR 14 to 28) for the STEMI patients given reperfusion therapy, 28.7 (IQR 19 to 41) for STEMI patients not given reperfusion therapy and 27.9 (IQR 19 to 40) for non-STEMI patients. Grouping by the predetermined 10-point ranges revealed strong, graded relationships, with 30-day mortality across risk groups that were significant for both STEMI (1.4% to 66.7%) and non-STEMI (0% to 51.4%) patients.
Risk of 30-day mortality increased by 6% for each point of the TIMI risk index overall, and by between 5% and 8% for subgroups (STEMI and non-STEMI patients, and STEMI patients given and not given reperfusion therapy).
Distribution of risk
The distribution of risk in the EFFECT study population was significantly different between STEMI and non-STEMI patients, and between patients given reperfusion therapy and those not given reperfusion therapy (P≤0.001). The distribution profile for patients with STEMI who were given reperfusion therapy closely approximated that of the InTIME II trial patients, and that of the NRMI-3 and -4 database patients given reperfusion therapy, with a strong skew to the right (Figure 2). Risk was more normally distributed for both the EFFECT study STEMI patients not given reperfusion therapy and non-STEMI patients as it was for NRMI -3 and -4 database patients not given reperfusion therapy.
Figure 2).
Distribution in the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study population of Thrombolysis In Myocardial Infarction (TIMI) risk index scores by the predefined 10-point range compared with distribution in the Intravenous nPA for Treatment of Infarcting Myocardium Early (In-TIME II) trial ST-segment elevation myocardial infarction (STEMI) patients treated with thrombolysis and National Registry of Myocardial Infarction (NRMI)-3 and -4 database patients treated and not treated with reperfusion therapy (RT)
Discrimination
The C statistic for the TIMI risk index modelled as a continuous variable was 0.81 (95% CI 0.79 to 0.82) (Table 2). The capacity to discriminate between high- and low-risk patients was good (approximately 0.80) in both STEMI patient groups, regardless of whether reperfusion therapy was given, and in non-STEMI patients. The C statistic was poorer for women and patients older than 65 years of age, although the 95% CI overlapped in each of the subgroups.
TABLE 2.
Predictive value (C statistic) of the Thrombolysis In Myocardial Infarction (TIMI) risk index for 30-day mortality in the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study population
| 30-day mortality, % | C statistic (95% CI) | |
|---|---|---|
| All patients | 10.2 | 0.81 (0.79–0.82) |
| STEMI | 9.1 | 0.82 (0.80–0.84) |
| Reperfusion attempted | 6.3 | 0.80 (0.77–0.84) |
| Reperfusion not attempted | 15.2 | 0.79 (0.76–0.82) |
| Anterior myocardial infarction | 12.0 | 0.80 (0.77–0.82) |
| Inferior myocardial infarction or other | 7.4 | 0.84 (0.81–0.87) |
| Non-STEMI | 10.5 | 0.80 (0.78–0.82) |
| Age | ||
| <65 years of age | 2.7 | 0.77 (0.73–0.82) |
| ≥65 years of age | 15.2 | 0.74 (0.72–0.75) |
| Sex | ||
| Men | 8.2 | 0.82 (0.81–0.84) |
| Women | 13.8 | 0.76 (0.74–0.78) |
STEMI ST-segment elevation myocardial infarction
Calibration
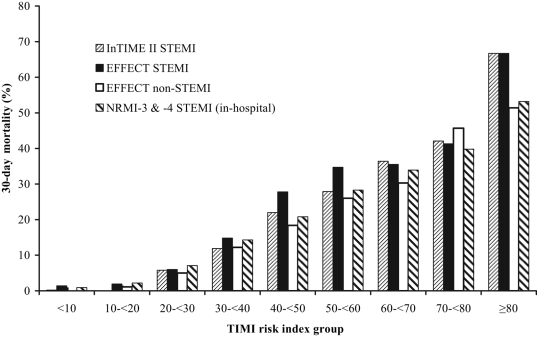
Thirty-day mortality was higher in eight of the nine risk groups for the EFFECT study STEMI patients than for non-STEMI patients. Overall, mortality among the EFFECT study patients with STEMI was very similar to that of the InTIME II trial and NRMI-3 and -4 database patients, although it was higher in the middle range of 10-point risk score groups (Figure 3).
Figure 3).
Thirty-day mortality for the Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study patients with ST-segment elevation myocardial infarction (STEMI) and non-STEMI compared with the Intravenous nPA for Treatment of Infarcting Myocardium Early (In-TIME II) trial patients, and with in-hospital mortality for National Registry of Myocardial Infarction (NRMI)-3 and -4 database patients. TIMI Thrombolysis In Myocardial Infarction
DISCUSSION
The present study confirms that the TIMI risk index, grouped into 10-point ranges, is capable of discriminating between patients at low and high risk for early death after STEMI, regardless of whether they have been treated with reperfusion therapy.
The good performance of the risk index in this unselected Canadian population, despite higher 30-day mortality than among the InTIME II trial participants in whom it was developed (10.2% versus 6.0%), is likely related to the similar distribution of risk (12). The poor performance of the index in the CCP population was accompanied by a distribution based on quintiles of risk from the InTIME II trial that was highly skewed, with no patients being in the lowest risk category and the majority being in the highest risk group (5). Because age is an important component of the TIMI risk index, a skewed distribution in a selected elderly population is expected. The distribution of 10-point range risk groups for STEMI patients treated with reperfusion therapy in the NRMI-3 and -4 databases closely approximated that of the InTIME II trial, with a similar skew to the right, while the profiles of patients who did not receive reperfusion therapy showed a more normal distribution. Similarly, the risk distribution for the EFFECT study STEMI patients who were treated with reperfusion therapy was very close to that of the InTIME II trial patients; however, the risk distribution of patients not given reperfusion therapy was indistinguishable from that of non-STEMI patients.
The relatively high prognostic discrimination of the TIMI risk index in the EFFECT study for patients with STEMI not given reperfusion therapy was surprising. In the NRMI-3 and -4 databases, there was a clear difference between this group and the group given reperfusion therapy (C statistic 0.71 versus 0.81) (6). The NRMI population was, on average, two years older, the prevalence of comorbidities was greater, and mortality was higher, for those who were given reperfusion therapy and those who were not, than among the EFFECT study STEMI patients. The poorer performance of the TIMI risk index in the NRMI population not given reperfusion therapy may indicate that there is an age threshold beyond which the risk index is less useful, as demonstrated in the CCP patients. Indeed, the poorest C statistic among the EFFECT study subgroups was for patients aged older than 65 years, although the 95% CI overlapped.
TIMI risk index in non-STEMI patients
We found that the TIMI risk index has good prognostic discrimination among patients with non-STEMI; this is the first time that it has been validated for this patient group in a large population-based study. This extends the usefulness of the risk index, because it can be applied to patients with presumed AMI, but without definitive ST-segment elevation in the baseline ECG.
TIMI risk index and acute coronary syndromes
Testing of the TIMI risk index across the whole spectrum of acute coronary syndromes (ACS) has been reported from only one small study (13). Among 710 patients admitted to a single site, the C statistic for 30-day mortality was 0.65 for UA, 0.75 for non-STEMI and 0.85 for STEMI. The overall discriminatory capacity was best for patients younger than 65 years of age compared with older patients (C statistic 0.88 versus 0.71). The investigators in the present study used the five risk groups derived from the InTIME II trial quintiles. The CIs were not provided, and there was only one death among patients with UA. Thus, the validity of the TIMI risk index as a valid tool for the prediction of risk across the spectrum of ACS, especially among the lower-risk UA patients, is yet to be demonstrated.
The value of the index will be improved if it is found to be valid for both UA and AMI. Its strength is that it may be calculated at first contact using the most basic of routinely collected information (age, SBP, HR), making it potentially valuable in the triage of patients with ischemic chest pain. The ‘early invasive’ strategy favoured for high-risk UA and non-STEMI patients (14,15) can be guided by currently available models, such as the TIMI risk score for UA and non-STEMI (1) or the Global Registry of Acute Coronary Events (GRACE) ACS (16), which rely on the addition of baseline laboratory and ECG data. Given that one in eight of the EFFECT study patients with non-STEMI had a risk of death within 30 days in excess of 25%, risk assessment by some means is important for this group of patients.
Clinical application of the TIMI risk index
The TIMI risk index has been developed and validated retrospectively. Whether very early risk stratification of patients with suspected AMI would be a useful adjunct to clinical decision-making has not been tested, nor is it known whether such information would influence either physicians’ actions in the assessment and immediate management of patients or patient outcomes. For communities with options that include prehospital thrombolysis, direct transport or rapid transfer to a PCI-capable centre, early risk stratification of STEMI patients using the TIMI risk index patients may aid in choosing the reperfusion therapy.
Limitations to the study
The EFFECT study had a smaller population than either the CCP or the NRMI-3 and -4 databases; therefore, the CIs are broader. Differences between groups, such as those of patients 65 years of age or younger and older than 65 years of age, may be clinically important, but did not achieve statistical significance.
The data were collected retrospectively, so as in most clinical databases, there was some missing information, although this figure was less than 2%.
CONCLUSIONS
The TIMI risk index is a simple tool for the prediction of 30-day mortality after AMI. In the present population-based validation study, the TIMI risk index showed good discrimination and calibration among patients with STEMI and non-STEMI. Although its discriminatory capacity was a little attenuated among patients older than 65 years of age, our results suggest that its use for early risk stratification among patients with suspected AMI in routine clinical practice is warranted.
Acknowledgments
The EFFECT study was conducted under the auspices of the Canadian Cardiovascular Outcomes Research Team (CCORT). CCORT is funded by grants from the Canadian Institutes of Health Research and the Heart and Stroke Foundation of Canada.
REFERENCES
- 1.Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA. 2000;284:835–42. doi: 10.1001/jama.284.7.835. [DOI] [PubMed] [Google Scholar]
- 2.Morrow DA, Antman EM, Charlesworth A, et al. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000;102:2031–7. doi: 10.1161/01.cir.102.17.2031. [DOI] [PubMed] [Google Scholar]
- 3.Morrow DA, Antman EM, Giugliano RP, et al. A simple risk index for rapid initial triage of patients with ST-elevation myocardial infarction: An InTIME substudy. Lancet. 2001;358:1571–5. doi: 10.1016/S0140-6736(01)06649-1. [DOI] [PubMed] [Google Scholar]
- 4.Ryan TJ. The Thrombolysis In Myocardial Infarction risk index. J Am Coll Cardiol. 2004;44:790–2. doi: 10.1016/j.jacc.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Rathore SS, Weinfurt KP, Gross CP, Krumholz HM. Validity of a simple ST-elevation acute myocardial infarction risk index: Are randomized trial prognostic estimates generalizable to elderly patients? Circulation. 2003;107:811–6. doi: 10.1161/01.cir.0000049743.45748.02. [DOI] [PubMed] [Google Scholar]
- 6.Wiviott SD, Morrow DA, Frederick PD, et al. Performance of the Thrombolysis In Myocardial Infarction risk index in the National Registry of Myocardial Infarction-3 and -4: A simple index that predicts mortality in ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2004;44:783–9. doi: 10.1016/j.jacc.2004.05.045. [DOI] [PubMed] [Google Scholar]
- 7.Tu JV, Donovan LR, Lee DS, et al. Quality of Cardiac Care in Ontario. EFFECT (Enhanced Feedback for Effective Cardiac Treatment), 2004. < www.ccort.ca/effect.asp> (Version current at November 10, 2006).
- 8.Canadian Institute for Health Information. Discharge Abstract Database. <http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=services_dad_e> (Version current at December 6, 2006).
- 9.World Health Organization . Ninth Revision. Washington: Public Health Service, US Department of Health and Human Services; 1988. International Classification of Diseases. [Google Scholar]
- 10.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–69. doi: 10.1016/s0735-1097(00)00804-4. (Erratum in 2001;37:973). [DOI] [PubMed] [Google Scholar]
- 11.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 12.Morrow DA, Antman EM, Murphy SA, et al. The Risk Score Profile: A novel approach to characterising the risk of populations enrolled in clinical studies. Eur Heart J. 2004;25:1139–45. doi: 10.1016/j.ehj.2004.04.036. [DOI] [PubMed] [Google Scholar]
- 13.Ilkhanoff L, O’Donnell CJ, Camargo CA, O’Halloran TD, Giugliano RP, Lloyd-Jones DM. Usefulness of the TIMI risk index in predicting short- and long-term mortality in patients with acute coronary syndromes. Am J Cardiol. 2005;96:773–7. doi: 10.1016/j.amjcard.2005.04.059. [DOI] [PubMed] [Google Scholar]
- 14.Boden WE. “Routine invasive” versus “selective invasive” approaches to non-ST-segment elevation acute coronary syndromes management in the post-stent/platelet inhibition era”. J Am Coll Cardiol. 2003;41(Suppl S):113S–22S. doi: 10.1016/s0735-1097(02)02963-7. [DOI] [PubMed] [Google Scholar]
- 15.Bavry AA, Kumbhani DJ, Quiroz R, Ramchandani SR, Kenchaiah S, Antman EM. Invasive therapy along with glycoprotein IIb/IIIa inhibitors and intracoronary stents improves survival in non-ST-segment elevation acute coronary syndromes: A meta-analysis and review of the literature. Am J Cardiol. 2004;93:830–5. doi: 10.1016/j.amjcard.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 16.Granger CB, Goldberg RJ, Dabbous O, et al. Global Registry of Acute Coronary Events Investigators Predictors of hospital mortality in the Global Registry of Acute Coronary Events. Arch Intern Med. 2003;163:2345–53. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]