Abstract
Objectives
This study sought to define the extent of utilization of 12 types of electronic information system (EIS) function in U.S. nursing homes (NH), to relate EIS utilization to selected facility characteristics and to contrast these findings to previous estimates of EIS use in NH.
Design
This study used data from the National Nursing Home Survey (NNHS), a nationally representative, cross-sectional sample of U.S. NH.
Measurements
Data on current use of EIS in 12 functional areas, including administrative and resident care activities, were collected. Information was also collected on facility characteristics including ownership, bed size, and whether the facility was a member of a chain.
Results
Essentially all (99.6%) U.S. NH had ≥1 EIS, a figure that was driven by the nearly universal use of EIS for Minimum Data Set (MDS) reporting (96.4%) and for billing (95.4%). Nearly 43% of U.S. NH had EIS for medical records, including nurse's notes, physician notes, and MDS forms. EIS use ranged from a high of 79.6% for admission, transfer, and discharge to a low of 17.6% for daily care by certified nursing assistants (CNAs). Ownership, membership in a chain, and bed size were associated with use of selected EIS. Larger facilities and those that were part of a chain used more EIS than smaller standalone facilities.
Conclusion
In 2004, NH use of EIS for functions other than MDS and billing was highly variable, but considerably higher than previous estimates.
Introduction
Nursing homes (NH) have been thought to lag behind other health care settings in the adoption of health information technologies (HIT). 1 However, few studies have characterized the use of HIT or, more broadly, electronic information systems in NH, or the relationship between facility characteristics and use of electronic information systems at a national level. This article addresses basic gaps in existing knowledge of electronic information systems use by providing the first national estimates of their use in 12 functional areas in United States NH and contrasting these findings to published estimates in NH and in other health care settings.
Background
Rationale for Need
As in other provider settings, adoption of electronic information systems in NH has the potential to add value by improving efficiency in administrative and operational areas, and more importantly, by helping to integrate services and improve quality of care. 2 Because quantitative data that can be tracked over time are a core requirement for continuous quality improvement (CQI), it follows that improvement in systems that facilitate data collection and tracking for patient care can also facilitate CQI.
Challenges to Adoption
Well-described barriers to implementation of electronic information systems include lack of access to capital by providers, high initial costs with uncertain payoff, complex systems, and lack of data standards that permit exchange of data, privacy concerns, and legal issues. 3 Relatively few high-quality studies have demonstrated the value of electronic information systems for cost-effectiveness, efficiency, and quality of care. Nonetheless, there is potential for NH providers and resident populations to benefit substantially from electronic information systems. For this reason, benchmarks on use of electronic information systems in the NH setting are valuable. However, when evaluating the incorporation of information technologies into provider settings, one must adopt and apply standardized definitions of electronic information systems—a feature lacking in previous studies. This methodological issue can lead to difficulty in interpreting data within and between studies. Recently, standard definitions were released by the National Alliance for Health Information Technology (NAHIT). 4
With one notable exception—a report focused on medication administration records 5 —previous quantitative studies of electronic information systems in NH focused on single states 6,7 or particular segments of the industry, such as members of a trade association or interest group. 8,9,10 Other reports on electronic information systems use and barriers to use in the NH setting have provided important information but are based on case studies, expert panels, or qualitative methodologies that have limited generalizability and reproducibility. 1,11,12,13
Research Question
Responding to existing gaps in the literature and to methodological limitations of previous reports of electronic information systems in U.S. NH, we analyzed data on use of electronic information systems in U.S. NH from the first nationally representative study to collect this information.
Methods
Study Design and Data Collection
In the 2004 National Nursing Home Survey (NNHS), 1,500 facilities were selected from a sampling frame of approximately 16,000 U.S. NH at that time. The sampling frame was drawn from two sources: (1) the Centers for Medicare and Medicaid Services Provider of Services file of U.S. NH, and (2) state licensing lists. Of the 1,500 sampled facilities, 283 refused to participate and 43 were considered out of scope for one or more of the following reasons: the NH had gone out of business, it failed to meet the definition used in the survey, or it was a duplicate of another facility in the sample. A total of 1,174 NH participated, resulting in a response rate of 81%. 14
Use of Electronic Information Systems
The Facility Component of the NNHS survey consists of data collected during an in-person interview with the NH administrator. Respondents were presented with a card listing 12 functional areas, and asked to select all areas that were supported by electronic information systems in their facility. The wording of the question was, “Does {facility} currently use electronic information systems for any of the tasks on this card?” The 12 areas that were assessed were:
• Admission, discharge, and transfer
• Physician orders
• Medication orders and drug dispensing
• Laboratory/procedures information
• Patient medical records
• Medication administration information
• Minimum data set (MDS)
• Dietary
• Daily personal care by nursing assistants
• Billing/finance
• Staffing/scheduling information
• Human resources/personnel information.
No definition of electronic information systems was provided overall, or for any of the specific functional areas, with one exception: a help screen clarified for respondents that “patient medical records include nurse's notes, physician notes, and MDS forms.”
Each of the electronic information system functional utilization variables was coded as yes/no. A variable representing any use of electronic information system was derived from these 12 variables. A second variable representing use of electronic information systems to support functions other than billing and MDS was also created. Similarly, a variable representing the total number of electronic information systems used in each NH was derived by summing yes responses for each item (n = 12 functions maximum), and a corresponding variable was created representing the total number of systems supporting functions other than billing and MDS (n = 10 functions maximum). We also created three variables to represent different combinations of electronic information systems related to electronic health records (EHR). For the purposes of this report and to facilitate comparison with previous studies, a facility with electronic patient medical records was said to have “EHR A” capabilities; a facility with electronic patient medical records plus electronic information systems for three additional direct care functions (physician orders, medication orders/drug dispensing, and laboratory/procedures information) was said to have “EHR B” capabilities; and a facility with all of the electronic functions in EHR B plus medication administration information was said to have “EHR C” capabilities.
Facility Characteristics
The 2004 NNHS contained information on ownership status (for-profit vs. all others, including nonprofit, local, and state government and Veterans Affairs). The terms for-profit and not-for-profit are used to describe this variable. Variables describing whether the facility was a member of a chain (yes/no) and the number of beds (3–49, 50–99, and 100+) were also recorded.
Statistical Analysis
Analyses were conducted with the PROC SURVEYFREQ procedure in SAS, which takes into account the strata, cluster, and weight variables that define the complex sampling approach used in the NNHS. This procedure was used to generate proportions and to conduct chi-square tests. In various analyses, we examined facility characteristics in relation to use of individual electronic information systems, and we also examined these characteristics in relation to the total number of systems that were in place at the time of the survey. Reported p-values are for chi-square tests of differences in proportions of these cross-tabulated data. The finite population correction was used per National Center for Health Statistics recommendations for the NNHS Facility data file. Data are presented in a manner that applies to all U.S. NH in 2004, and estimates are based on at least 30 observations, because fewer observations could be unreliable.
Results
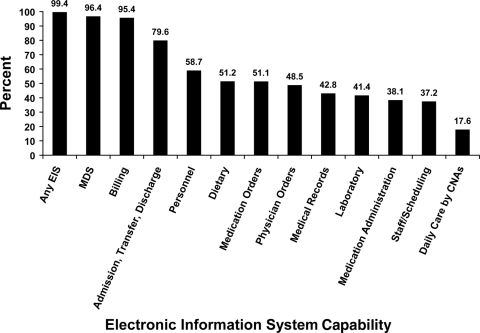
▶ summarizes selected facility characteristics of NH in the 2004 NNHS. Slightly more than half of U.S. NH were members of a chain, and 61.5% were for-profit. Electronic information systems data were available for 1,172 of 1,174 facilities in the NNHS, representing approximately 16,054 facilities nationwide in 2004. Essentially all (99.4%) NH had at least one electronic information system, a figure that was driven by the fact that nearly all facilities had systems for federally required MDS reporting (96.4%) and for billing (95.4%; ▶). After exclusion of MDS and billing, 91.6% of NH had at least one electronic information system, with nearly 80% of facilities using electronic systems for admission, discharge, and transfer. Beyond MDS data capture and billing, there was marked variability in the extent to which U.S. NH utilize electronic information systems for other tasks. For instance, only 17.6% of NH used electronic information systems for daily personal care by nursing assistants, and less than half used these systems to support physician orders, medical records, the laboratory, and medication administration.
Table 1.
Table 1 Selected Characteristics of Nursing Homes, United States, 2004
| Total |
||
|---|---|---|
| Percent | Weighted N | |
| Characteristic | ||
| Total ∗ | 100.0 | (16,081) |
| Member of Chain | ||
| Yes | 54.2 | (8,709) |
| No | 45.8 | (7,372) |
| Bed size | ||
| 3–49 | 13.9 | (2,242) |
| 50–99 | 37.3 | (6,005) |
| 100–199 | 42.5 | (6,840) |
| ≥200 | 6.2 | (994) |
| Ownership | ||
| For-profit | 61.5 | (9,889) |
| Nonprofit | 38.5 | (6,192) |
∗ Data are weighted using SAS SURVEYFREQ. Some categories may not add to 100.0 due to rounding.
Figure 1.
Use of electronic information systems in nursing homes: United States, 2004.
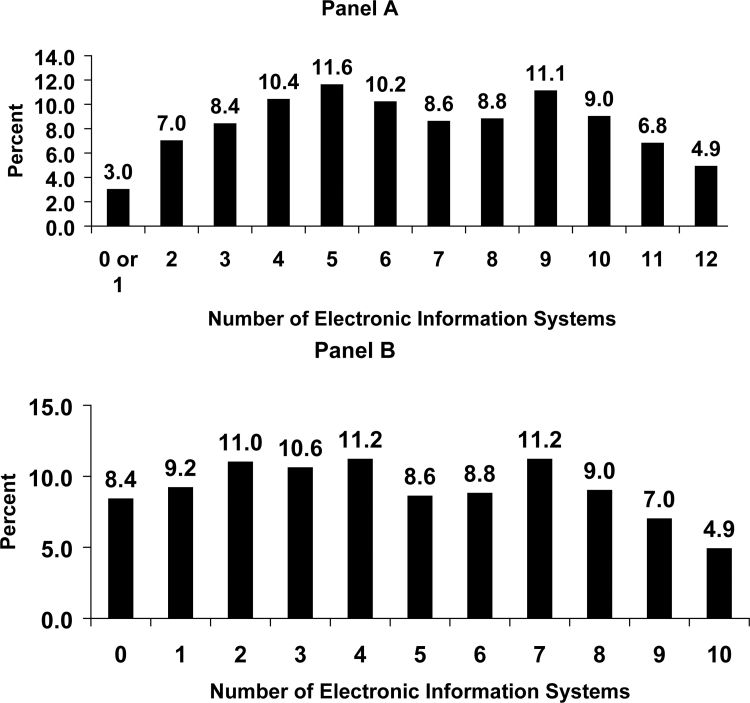
There was considerable variability in the total number of electronic information systems used by NH (▶). Although Panel A suggests that only a small proportion of facilities had 2 or fewer systems, only 10%, Panel B, which considers the 10 functional areas other than MDS and billing, shows that nearly 30% of facilities had two or fewer systems in place. Regardless of whether MDS and billing are considered, <5% of U.S. NH used electronic information systems for all 12 of the functional areas that were assessed in the 2004 NNHS.
Figure 2.
Distribution of electronic information systems in nursing homes: United States, 2004. Distribution in panel A includes MDS and billing; distribution in panel B excludes these functions.
Compared to for-profit NH, not-for-profit facilities used electronic information systems more often for laboratory (45.4% vs. 38.9%, p < 0.05) and human resources/personnel information (65.8% vs. 54.3%, p < 0.001) and less often for dietary information (46.4% vs. 54.3%, p < 0.05). Facility ownership was unrelated to electronic information system use in other areas. Those NH belonging to a chain had greater use of electronic information systems than freestanding facilities for admissions/discharge/transfer (82.7% vs. 76.0%, p < 0.01), dietary (57.2% vs. 44.2%, p < 0.0001), billing (97.4% vs. 93.0%, p < 0.001), and daily personal care by nursing assistants (16.9% vs. 11.9%, p = 0.02; data not shown).
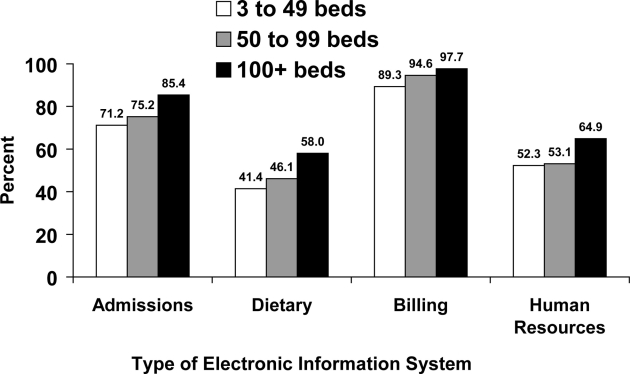
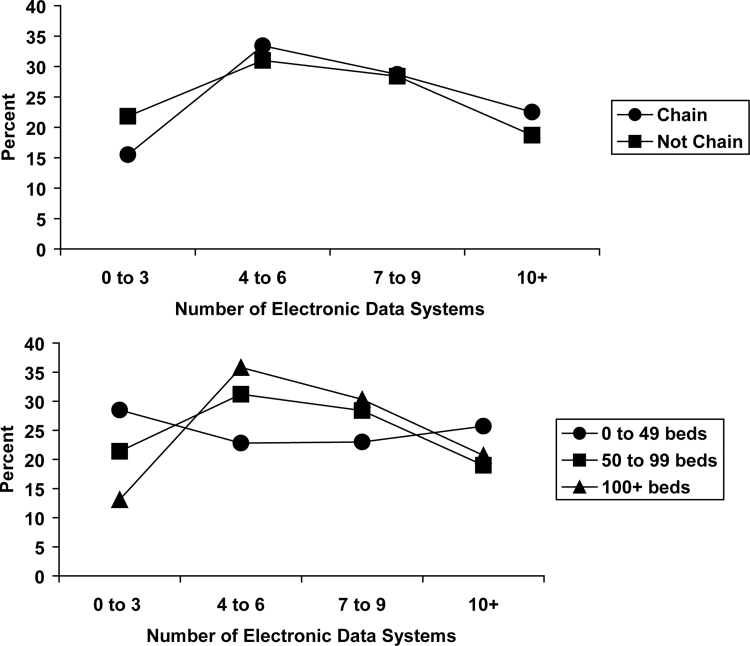
▶ shows that facility size was related in a stepwise manner to electronic information systems use for admissions (p < 0.0001), dietary (p < 0.0001), billing (p = 0.0001), and human resources (p = 0.0003). Larger facilities were more likely to have electronic systems supporting these functions. Utilization of electronic information systems differed by NH bed size (p < 0.0001, ▶) and by NH membership in a chain (p < 0.05). Larger facilities and those that were part of a chain tended to have a greater number of electronic information systems. Facility ownership category was not associated with the number of systems utilized.
Figure 3.
Use of selected electronic information systems in nursing homes, by bed size, United States, 2004.
Figure 4.
Number of electronic information systems by chain membership and bed size, United States, 2004.
▶ presents relevant comparisons from the authors' best knowledge of national estimates of EHR utilization in various health care settings. 15,16,17,18 The EHR adoption in NH compares favorably to those in physician offices and possibly to those in hospitals. Nearly all nursing homes (96%) had detailed electronic patient assessment information in 2004 via the MDS. A smaller proportion (43%; EHR A) had electronic systems that included both the MDS and nurses' and physicians' notes. About 20% (EHR B) had even more complete EHR functions, including physician orders, medication orders, and laboratory information.
Table 2.
Table 2 National Estimates of Electronic Medical Records in Different Health Care Sectors
| Percent with EMR/EHR or Function by Sector |
||||
|---|---|---|---|---|
| Survey | Definition of EMR/EHR or Function Studied | Hospitals | Physicians (Ambulatory Care) | Nursing Homes |
| 2005 15 | Electronic documentation of patient characteristics—could include clinical notes or only demographics | 59% | ||
| 2003 16 | Computerized physician order entry (CPOE) | 5% | ||
| 2005 NAMCS 17 | Full or partial electronic medical record ∗ | 25% | ||
| Full EMR† | 9% | |||
| 2007/08 18 | Basic EHR‡ | 13% | ||
| Fully functional EHR§ | 4% | |||
| 2004 NNHS | The MDS—patient assessment information | 96% | ||
| EHR A: Patient medical records—includes MDS, nurses' notes, and physician notes | 43% | |||
| EHR B: Patient medical records, physician orders, medication orders/drug dispensing, laboratory/procedures information | 20% | |||
| EHR C: Same components as EHR B (above) plus medication administration information | 17% | |||
∗ Answered yes to question “Do you use full or partial (part paper, part electronic) electronic medical records?” OR had all 4 components of a full EMR.
† Had all 4 of these computerized functions: orders for prescriptions, orders for tests, test results, physician notes.
‡ Had all these electronic functions: patient demographics, patient problem lists, medication lists, clinical notes, orders for prescriptions, viewing laboratory results, viewing imaging results.
§ All of the functions of basic EHR plus various clinical decision support tools (e.g., out of range test levels highlighted).
EMR = electronic medical record; EHR = electronic health record.
Discussion
Significance
This report provides one of the first nationally representative assessments of electronic information system utilization in U.S. nursing homes. It provides quantitative data regarding functional use of electronic information systems in 12 areas, offers new insight into use of these systems for both clinical and nonclinical functions, and provides a baseline for benchmarking future comparative work.
Previous work suggested that NH lagged behind other health care sectors in adopting electronic information systems. A report prepared for the National Commission for Quality Long-Term Care concluded that “long-term care has adopted information technology solutions even more slowly than the rest of health care.” 19 That conclusion, which carried over to the Commission's Final Report, and similar reports 20 are based on a 2006 report describing estimates first assembled in 2004. That report compared estimates by a small number of experts regarding information technology adoption in NH, hospitals, and physician offices. 1 In contrast, our results, derived from a nationally representative direct sampling of NH, indicate considerably higher adoption rates, are consistent with reports from single states and smaller surveys, and compare favorably to adoption rates of selected electronic information systems in physician offices and in hospitals.
Several of the current results contrast markedly with the frequently cited 2006 report. 1 The latter report estimated that 77% of NH used electronic information systems for billing, whereas our survey indicates that 95.3% of NH did so in 2004. The 2006 report estimated that 1% of NH had “computerized physician order entry”; the NNHS survey assessed use of electronic information systems for “physician orders”, and indicated that 48.5% of U.S. NH did so. Finally, the 2006 report estimated that 1% of NH had “electronic health records (e.g., demographics, problem list, medication list, allergies, advance directives),” whereas our data indicate that 42.8% of U.S. NH used electronic information systems for “patient medical records,” which were defined to include “nursing notes, physician notes, and MDS forms.”
There are major differences in methodology between the current and the 2006 reports. The 2006 report was a market analysis consisting of qualitative work in Denver and Boston and interviews with key informants, followed by estimates made by an expert panel consisting of 12 individuals. In contrast, the NNHS collected quantitative data from primary sources through a multistage sampling process that involved a nationally representative sample of 1,174 NH and interviews with NH administrators. These data derive from a survey conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention, and are applicable to the approximately 16,000 NH in the U.S. in 2004.
Estimates of electronic information systems use in NH from more narrowly focused surveys lend additional weight to the conclusion that actual use in NH is more prevalent than the experts have estimated. For example, a 2007 survey of mostly for-profit, national, multi-facility chains distinguished between electronic information systems for “medical records” (owned by nearly 50%) and presumably more comprehensive “electronic health records/electronic medical records” (owned by approximately 20%). 10 By either description, use is closer to the 43% figure for “patient medical records” reported in the NNHS than to the 1% use of “electronic health records” estimated by the experts. It should be noted that results from the multi-facility chains survey are reported at the corporate, rather than individual facility level, and that the response rate was only 19%. Offering further evidence of accelerating EHR adoption in nursing homes, a 2007 survey (with a 78% response rate) of Medicare-certified Minnesota nursing homes found 89% of respondents reported using electronic information systems for “census management,” 41% use them for “documentation of clinical notes,” and 31% reported that they have an “electronic health record.” 7
A review of EHR adoption rates in hospitals and physician offices (through 2005) has been published. 21 For comparison to adoption rates for nursing homes from the 2004 NNHS, we used adoption rates from the national surveys of hospitals and physician offices judged best by those reviewers and included one additional national survey of physician offices published in 2008. 17,18 Estimates of adoption rates in physician offices for EHR with somewhat less complete functions in the two different studies were 13% and 25%, whereas estimates for more complete EHR from the same two studies were 4% and 9%. The best available estimate of EHR in hospitals is a report that 59% (in 2005) had “electronic documentation of patient characteristics,” which previous reviewers noted could include clinical notes or just demographics. 15 Those systems, which we labeled “EHR B” in NH, appear similar to the “basic EHR,” which a recent national study found to be adopted by 13% of physician offices. 18 These estimates, taken together and compared to our summary of published national estimates for EHR in physicians' offices and hospitals (▶), indicate that NH adoption of electronic information systems for clinical records, variously described, is not nearly as behind the rest of the industry as previously suggested.
Although use of electronic information systems in NH patient care functions is considerably greater than previously thought, it is important to point out that in 2004 there remained considerable room for improvement. To the extent that electronic information systems could assist NH in maximizing CQI associated with how nursing assistants perform their daily personal care functions—arguably the feature of NH care of greatest concern to consumers—it is noteworthy that of the 12 functional areas assessed in the NNHS, electronic information systems were used the least to support this one (17.6%). Although frontline workers provide the majority of direct care in NH, they are rarely included in the care planning or CQI activities. 22 And yet, it has been shown that inclusion of certified nursing assistants (CNAs) in care documentation, care planning, and CQI is related to better quality of care. 23 The potential role of electronic information systems in helping to empower CNAs to engage in more efficient and higher quality care delivery and CQI in NH cannot be overemphasized. This question is ripe for further investigation in a well-designed study of the impact of electronic information systems in direct resident care.
Given the importance of Medicare and Medicaid reimbursement for U.S. NH, it was not surprising that there was nearly universal (>95%) use of electronic information systems for billing because Medicare mandates electronic submission of Medicare claims with very few exceptions. 24 Supplementary analyses showed that 10% of smaller facilities (those with fewer than 50 beds) did not use electronic information systems for billing, a contrast to the 4% figure in facilities with >200 beds. Small providers can obtain an exemption from the Medicare electronic billing mandate, but eligibility is based on staffing levels rather than bed size. Nonetheless, the observed relationship between bed size and use of electronic information systems for billing is consistent with the idea that smaller facilities may seek waivers to become exempt from mandatory electronic claim submission.
Federal requirements also mandate collection of MDS data by Medicare and Medicaid certified facilities; electronic submission of those data has been mandatory since 1998. Our data showed that >96% of U.S. NH use electronic information systems for MDS data. It is possible that facilities that reported not using these systems for MDS were not certified by the Centers for Medicare and Medicaid Services, and might have been those admitting only private pay residents. However, this question could not be directly addressed with our data because variables describing Medicare and Medicaid certification, although collected in the NNHS, are not included in the public use dataset. Nonetheless, only about 2% of NH nationwide were certified by neither Medicare nor Medicaid in 1999, according to the most recent reliable information. 25 Allowing for some growth in the private pay nursing home sector over time, that figure is reasonably close to the proportion of the 2004 sample that reported not using electronic information systems to support MDS. Our findings clearly point out the role of federal policy in driving some features of electronic information systems utilization in U.S. NH.
Differences in use of electronic information systems between facilities that were and were not members of a chain may reflect the tendency among chains for more standardized procedures and a more corporate business approach to operations, and a tendency to invest in electronic information systems for areas where such investment may yield higher efficiency and cost-effectiveness. Facilities that are members of a chain may also have access to more resources and a greater need to centralize data, both factors that would enhance the likelihood of adopting these technologies. It may also be the case that standalone NH have a different perception of return on investment associated with electronic information systems, and their independent decision-making ability permits more latitude to avoid investments in areas that they perceive to be of limited value.
Our data showed that as the size of a facility increased, so too did the use of electronic information systems. This finding is somewhat intuitive to the extent that larger facilities have more residents and staff, and may therefore benefit more from technological supports. Larger facilities also may have more resources available to invest in electronic information systems. In contrast, we observed that for-profit and not-for-profit facilities differed little in their use of these systems. However, it should be noted that not-for-profits tended to be smaller and less frequently members of a chain. Accordingly, we re-ran analyses separately according to ownership and noted that bed size and chain membership were largely unrelated to electronic information systems use in not-for-profits, whereas the strength of these observations was enhanced among for-profit facilities, particularly for dietary and human resources. Thus, the observations associated with bed size and chain membership on electronic information systems use for the overall sample seem to be driven to a large extent by the impact of these factors among for-profit facilities. This is important because for-profit NH account for approximately 61% of NH nationwide, and therefore represent a considerable portion of the market.
Our data show that when MDS and billing are not considered, nearly 30% of U.S. NH have 2 or fewer systems in place, and 8.4% have none at all. Although it is appealing to consider adoption of electronic information systems in larger numbers of functional areas to be a reasonable target for U.S. NH, questions remain as to whether adoption of these systems in all areas is feasible or if it would result in measurable improvements in efficiency or quality of care. Considerations involving return on investment may be particularly pressing for smaller facilities or facilities that are not part of larger organizations, such as continuing care retirement communities.
One way that electronic information systems could lead to improvements in quality of care would be for these systems to provide better support for transitions across care settings. However, it has been pointed out that interoperability issues create considerable challenges to integration of care across settings, including NH. 13 As these broader issues are addressed, it may be the case that short-term benefits of electronic information systems may be in the area of immediate, front-line care, including work by nursing assistants.
Study Limitations
This report has several limitations that should be considered. First, the NNHS is cross-sectional, a design feature that prevents research designed to study longitudinal associations between use of electronic information systems and relevant outcomes. However, the NNHS provides the first nationally representative data on electronic information systems use in U.S. NH, making this data source extremely valuable for benchmarking future changes in their use in this care setting; these data also offer marked improvements over previous estimates of electronic information systems use in NH. Future studies could be designed to examine longitudinal questions that aim to evaluate the impact of these systems on diverse outcomes in the NH setting.
Second, lack of clear definitions of specific functions could lead to inaccurate estimates of the use of these functions as they were intended to be measured in the NNHS. However, it is unlikely that differences in interpretation of these functions would lead to errors of such a large magnitude that they would render our results invalid. For example, if an administrator misunderstood the question regarding whether electronic information systems were used to document daily personal care by nursing assistants, it is unlikely that this error would result in a change in the point estimate that would be so dramatic as to change the inference from this report, which is that electronic information system use for nursing assistants was the lowest of all the functions assessed in the survey. Further, the impact of ambiguous terminology will be minimized in the future because of recent standardization efforts. 4
Conclusion
In 2004, NH use of electronic information systems for functions other than MDS and billing was highly variable, but considerably higher than previous estimates. Facility characteristics are strongly associated with the extent of electronic information systems use in U.S. NH.
References
- 1.Poon EG, Jha AK, Christino M, et al. Assessing the level of healthcare information technology adoption in the United States: a snapshot BMC Med Inform Decis Mak 2006;6:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hedstrom K. The values of IT in elderly care Inform Technol People 2007;20:72-84. [Google Scholar]
- 3.Anderson J. Social, ethical, legal barriers to E-Health Int J Med Inform 2007;76:480-483. [DOI] [PubMed] [Google Scholar]
- 4. The National Alliance for Health Information Technology Report to the Office of the National Coordinator for Health Information Technology on Defining Key Information Technology TermsApril 28, 2008http://www.nahit.org/docs/hittermsfinalreport_051508.pdf 2007. Accessed June 23, 2008.
- 5.Chan S. Factors associated with use of electronic information systems for drug dispensing and medication administration records in long term care J Am Med Dir Assoc 2008;9:414-421. [DOI] [PubMed] [Google Scholar]
- 6.Health Management Strategies, Inc. Health Information Technology: Are Long Term Care Providers Ready?Prepared for the California HealthCare Foundation, April 2007http://www.chcf.org/documents/chronicdisease/HITNursingHomeReadiness.pdf 2008. Accessed July 21, 2008.
- 7.Stratis Health (Kristina Milinkovich) Nursing Homes Health IT. Survey conducted for the Minnesota QIO. presented at the LTC HIT Summit, June 9, 2008http://www.ahima.org/meetings/ltc/documents/ResearchInitiativesPanel_000.pdf 2008. Accessed August 7, 2008.
- 8.Tena-Nelson R. Health Information Technology in Long Term Care: Survey Findings 2006Presented at the LTC HIT Summit, June 9, 2006http://www.ahima.org/meetings/ltc/documents/Tena-Nelson_HITSummit_CCLC20060609.ppt 2008. Accessed August 7, 2008.
- 9. LTC-HIT: A Snap-Shot of the Use of Health Information Technology in Long-term CareA White Paper completed by the AHCA HIT Committee, December 2006http://www.ahcancal.org/facility_operations/hit/Documents/HITWhitePaper.pdf 2008. Accessed June 20, 2008.
- 10. Information Technology in Long Term Care—State of the Industry, Multi-Facility Research Report, Maestro Strategies on behalf of AHCA and NCAL, April 2007http://www.ahcancal.org/facility_operations/hit/Documents/InformationTechnologyinLongTermCare.pdf 2008. Accessed June 20, 2008.
- 11.Kaushal R, Bates DW, Poon EG, Jha AK, Blumenthal D, Harvard Interfaculty Program for Health Systems Improvement NHIN Working Group Functional gaps in attaining a national health information network Health Affairs 2005;24:1281-1289. [DOI] [PubMed] [Google Scholar]
- 12.Kramer A, Bennett R, Fish R, et al. Case Studies of Electronic Health Records in Post-Acute and Long-Term Carehttp://aspe.hhs.gov/daltcp/reports/ehrpaltc.pdf 2005. Accessed January 8, 2009.
- 13.Bennett RE, Tuttle M, May K, Harvell J, Coleman EA. Health Information Exchange in Post-Acute and Long Term Care: Case Study Findingshttp://aspe.hhs.gov/daltcp/reports/2007/HIEcase.pdf 2005. Accessed August 7, 2008.
- 14.Available at: http://www.cdc.gov/nchs/about/major/nnhsd/nnhsdesc.htm. Accessed April 17, 2007.
- 15.Laschober M, Maxfield M, Lee M, et al. Hospital Responses to Public Reporting of Quality Data to CMS: 2005 survey of Hospitals(Washington: Mathmatica, 12 October 2005)http://www.mathematica-mpr.com/publications/PDFs/hospitalresponse.pdf 2005. Accessed August 4, 2008.
- 16.Cutler DM, Feldman NE, Horwitz JR. U.S. Adoption of Computerized Physician Order Entry Systems Health Affairs 2005;24:1634-1663Available at: http://content.healthaffairs.org/cgi/reprint/24/6/1654. Accessed August 4, 2008. [DOI] [PubMed] [Google Scholar]
- 17. National Ambulatory Medical Care Surveyhttp://www.cdc.gov/nchs/products/pubs/pubd/hestats/electronic/electronic.htm 2005. Accessed July 8, 2008.
- 18.DesRoches C, Campbell E, Rao S, et al. Electronic health records in ambulatory care: a national survey of physicians N Engl J Med 2008;359:50-60. [DOI] [PubMed] [Google Scholar]
- 19.Martin RD, Brantley D, Dangler D. Report to the National Commission for Quality Long-Term Care: Essential but Not Sufficient-Information Technology in Long-Term Care as an Enabler of Consumer Independence and Quality Improvementhttp://www.qualitylongtermcarecommission.org/pdf/BearingPoint_Report_for_NCQLTC.pdf 2008. Accessed January 8, 2009.
- 20.Certification Commission for Healthcare Information Technology Expansion of CCHIT Certification to Professional Specialties, Care Settings, or Patient Populations: Environmental Scan Data Report and Draft Expansion Roadmaphttp://www.ahima.org/infocenter/whitepapers/documents/Public_Comment_Expanding_CCHIT_Certification_Roadmap_20070202.pdf#page%3DI 2008. Accessed January 8, 2009.
- 21.Jha A, Ferris T, Donelan D, et al. How common are electronic health records in the United States?. A summary of the evidence. Health Affairs 2006;11:496-507. [DOI] [PubMed] [Google Scholar]
- 22.Stone RI, Reinhard SC, Bowers B, et al. Evaluation of the Wellspring Model for improving nursing home qualityThe Commonwealth Fund; 2002. August.
- 23.Harahan MF, Stone RI. The Long-Term Care Workforce: Can the Crisis be Fixed? Report prepared for the National Commission for Quality Long-Term Care 2007. Washington, DC, January.
- 24.Available at: http://www.adminastar.com/Providers/EDI/files/CR2966090507.pdf. Accessed August 7, 2008.
- 25.Jones A. The National Nursing Home Survey: 1999 Summary. National Center for Health Statistics Vital Health Stat 2002;13(152):3Available at: http://www.cdc.gov/nchs/data/series/sr_13/sr13_152.pdf. Accessed August 4, 2008. [PubMed] [Google Scholar]