In the present study, we initially reported that the percentages of CD4+ and CD8+ effector memory T cells (TEM cells) were increased in PB and BM of AA. The elevated TEM cells with the potent effector capacity may relate to t he abnormal immune status in the pathogenesis of AA.
T-cell mediated suppression of hematopoiesis is considered the pivotal mechanism responsible for bone marrow failure in aplastic anemia (AA).1 In patients with AA, oligoclonal T cells in marrow were detected to show mature memory/effector phenotypes,2 implicating memory T cells might participate in the pathophysiological process of AA. Based on the ability to express chemokine receptor CCR7 and the phosphatase CD45RA, CD4+ and CD8+, T cells can be divided into naïve T cells (CD45RA+CCR7+), central memory T cells (TCM cells, CD45RA−CCR7+), and effector memory T cells (TEM cells, CD45RA−CCR7−). For CD8+ T cells, TEM cells also contain terminally differentiated CD45RA+CCR7−TEM cells (terminal TEM cells).3,4 Perturbation in the homeostasis of memory T cells has been reported in several T-cell mediated autoimmune diseases.5–7 In the present study, we initially investigated the distribution and function of naïve T cells, TCM cells, and TEM cells in patients with AA.
The study was approved by the Ethics Committee of Qilu Hospital, Shandong University, and informed consent was obtained from each participant. Forty-five newly-diagnosed untreated patients with AA (23 males and 22 females, mean age 36 years, range 18–69) were enrolled in this study. Criteria for the diagnosis and severity classification of AA were as previously reported.8,9 Out of 45 patients, 27 patients were diagnosed with severe AA (SAA) and 18 patients with moderate AA (MAA). No patient with AA had received any treatment or transfusion before enrollment. Thirty gender- and age-matched healthy volunteers served as controls (16 males, 14 females, mean age 41 years, range 21–67).
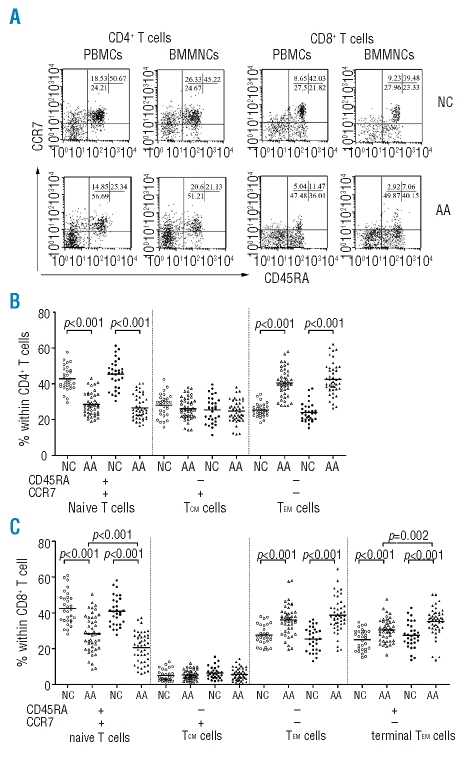
Freshly isolated peripheral blood mononuclear cells (PBMCs) and bone marrow mononuclear cells (BMMNCs) were stained with FITC-conjugated anti-CD45RA, PE-conjugated anti-CCR7, and PE-Cy5-conjugated anti-CD4 or PE-Cy5-conjugated anti-CD8 (BD Biosciences, San Diego, CA, USA) to measure percentages of naïve T cells, TCM cells and TEM cells in CD4+ and CD8+ T cells in both PBMCs and BMMNCs. For the important pathogenic role of T cell-produced IFN-γ in AA, intracellular cytokine IFN-γ production by different T-cell subsets was detected to assess their function. PBMCs and BMMNCs were simulated with 25 ng/mL PMA and 1 umol/L ionomycin in the presence of 2 ug/mL monesin (Sigma, St Louis, MO, USA) for 5h. After staining with PE-conjugated anti-CCR7 and PE-Cy5-conjugated anti-CD4 or PE-Cy5-conjugated anti-CD8, cells were fixed and permabilized and then stained with FITC-conjugated anti-IFN-γ (BD Biosciences). Stained cells were analyzed on a FACSCalibur flow cytometer using a build-in CellQuest software (BD Biosciences, San Diego, CA, USA). Statistical analyses were performed using SPSS 11.5 for Windows (SPSS Inc., Chicago, IL, USA). Differences between two groups were analyzed by Student’s t test. In the CD4+ T-cell population, significantly decreased percentages of CD45RA+CCR7+ naïve T cells were observed in PBMCs and BMMNCs of AA patients compared with controls (Figure 1A and B). In contrast, the percentages of CD45RA−CCR7− TEM cells in PBMCs and BMMNCs were higher in AA patients than in controls (Figure 1B). As far as CD8+ T-cell population was concerned, patients with AA still had decreased percentages of CD45RA+CCR7+ naïve T cells in PBMCs and BMMNCs compared with controls (Figure 1A and C). Meanwhile, both CD45RA−CCR7− TEM cells and CD45RA+CCR7− terminal TEM cells were increased in PBMCs and BMMNCs of patients with AA compared with controls (Figure 1C). There was no significant difference between patients with AA and controls in the percentages of CD4+ and CD8+ CD45RA−CCR7+ TCM cells from PBMCs or BMMNCs (Figure 1C). In CD4+ and CD8+ T-cell population of PBMCs and BMMNCs, no significant difference in percentages of naïve and memory T-cell subsets was detected between SAA and MAA, suggesting that the distribution of CD4+ and CD8+ T-cell subsets might not correlate with the severity of disease.
Figure 1.
Naïve and memory T-cell subsets in PBMCs and BMMNCs of patients with AA (AA, n=45) and normal controls (NC, n=30). (A) Representative flow cytometric analysis from a patient with AA and a normal control. Naïve and memory subsets were identified by the expressions of CD45RA and CCR7 after gating on CD4+ or CD8+ T cells in PBMCs and BMMNCs. (B) Percentages of naïve T cells, TCM cells and TEM cells in CD4+ T cells. (C) Percentages of naïve T cells, TCM cells, TEM cells and terminal TEM cells in CD8+ T cells. The open symbols (in B and C) represent percentages from PBMCs and solid symbols from BMMNCs. Horizontal lines indicate mean percentages.
Percentages of T-cell subsets in PBMCs were also compared with those in BMMNCs. There were no significant differences in T-cell subsets in CD4+ T cells between PBMCs and BMMNCs in either patients with AA or controls (Figure 1B). Concerning the CD8+ T-cell population, significantly increased CD45RA+CCR7− terminal TEM cells and decreased CD45RA+CCR7+ naïve T cells were observed in BMMNCs compared with PBMCs in AA patients, but no difference was detected in controls (Figure 1C).
Chemokine receptor CCR7 is essential for lymphocyte migration to secondary lymphoid organs. Compared with naïve T cells and TCM cells, TEM cells lack CCR7 expression and fail to migrate to lymph nodes, but TEM cells have acquired potential to rapidly enter inflamed tissues, secrete large amounts of cytokines and display immediate effector function.3,4 Our finding of higher percentages of CD4+ and CD8+ TEM cells in peripheral blood (PB) and bone marrow (BM) of patients with AA suggests TEM cells expand in AA and are recruited to BM.
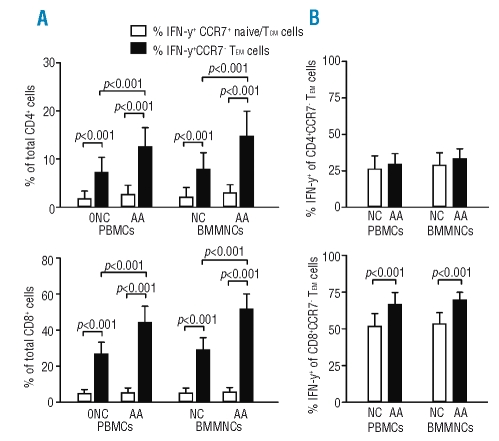
In humans, the TEM pool contains Th1, Th2 and CTL.3,10 In the present study, CD4+ and CD8+ CCR7− TEM cells from both PBMCs and BMMNCs, compared with CCR7+ naïve/TCM cells, produced significantly more IFN-γ in patients with AA as well as in controls (Figure 2A), which is consistent with previous studies, indicating that CCR7−TEM cells have more potent effector capacity. Among total CD4+ or CD8+ T cells, the percentages of IFN-γ-producing CD4+or CD8+ CCR7− TEM cells were significantly higher from PBMCs and BMMNCs in patients with AA than that in controls (Figure 2A). Interestingly, the percentages of IFN-γ producers in CD4+CCR7− TEM cells from PBMCs or BMMNCs did not differ between patients with AA and normal controls; whereas the production of IFN-γ in CD8+CCD7− TEM cells from both PBMCs and BMMNCs was significantly higher in patients with AA than normal controls (Figure 2B), suggesting that CD8+ TEM cells have increased effector capacity in AA. We presume increased TEM cells, particularly in marrow of AA, react as effector cells and participate in immune-mediated suppression of hematopoiesis in AA.
Figure 2.
IFN-γ production by stimulated CCR7+ naïve/TCM cells and CCR7− TEM cells in patients with AA (AA, n=26) and normal controls (NC, n=18). (A) Percentages of IFN-γ-producing CD4+ or CD8+ CCR7− TEM cells and CCR7+ naïve/TCM cells among total CD4+ or CD8+ T cells from PBMCs and BMMNCs. (B) Percentages of IFN-γproducing cells in CD4+ or CD8+CCR7− TEM cells from PBMCs and BMMNCs. Columns represent mean ± SD values.
In summary, the present study initially revealed that percentages of CD4+ and CD8+ TEM cells were increased in PB and BM of AA, and CD8+ terminal TEM cells were preferentially increased in BM of AA. The elevated TEM cells with the potent effector capacity may relate to the abnormal immune status in the pathogenesis of AA. Further studies regarding the influence of disease activity on TEM cells are required and might provide more insights into the pathophysiological significance of this T-cell subset in AA.
References
- 1.Young NS, Calado RT, Scheinberg P. Current concepts in the pathophysiology and treatment of aplastic anemia. Blood. 2006;108:2509–19. doi: 10.1182/blood-2006-03-010777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zeng W, Maciejewski JP, Chen G, Young NS. Limited heterogeneity of T cell receptor BV usage in aplastic anemia. J Clin Invest. 2001;108:765–73. doi: 10.1172/JCI12687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sallusto F, Lenig D, Förster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401:708–12. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 4.Sallusto F, Geginat J, Lanzavecchia A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu Rev Immunol. 2004;22:745–63. doi: 10.1146/annurev.immunol.22.012703.104702. [DOI] [PubMed] [Google Scholar]
- 5.Abdulahad WH, van der Geld YM, Stegeman CA, Kallenberg CG. Persistent expansion of CD4+ effector memory T cells in Wegener’s granulomatosis. Kidney Int. 2006;70:938–47. doi: 10.1038/sj.ki.5001670. [DOI] [PubMed] [Google Scholar]
- 6.Rus H, Pardo CA, Hu L, Darrah E, Cudrici C, Niculescu T, et al. The voltage-gated potassium channel Kv1.3 is highly expressed on inflammatory infiltrates in multiple sclerosis brain. Proc Natl Acad Sci USA. 2005;102:11094–9. doi: 10.1073/pnas.0501770102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gattorno M, Prigione I, Morandi F, Gregorio A, Chiesa S, Ferlito F, et al. Phenotypic and functional characterisation of CCR7+ and CCR7− CD4+ memory T cells homing to the joints in juvenile idiopathic arthritis. Arthritis Res Ther. 2005;7:R256–67. doi: 10.1186/ar1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaufman DW, Kelly JP, Jurgelon JM, Anderson T, Issaragrisil S, Wiholm BE, et al. Drugs in the aetiology of agranulocytosis and aplastic anaemia. Eur J Haematol Suppl. 1996;60:23–30. doi: 10.1111/j.1600-0609.1996.tb01641.x. [DOI] [PubMed] [Google Scholar]
- 9.Camitta BM, Rappeport JM, Parkman R, Nathan DG. Selection of patients for bone marrow transplantation in severe aplastic anemia. Blood. 1975;45:355–63. [PubMed] [Google Scholar]
- 10.Messi M, Giacchetto I, Nagata K, Lanzavecchia A, Natoli G, Sallusto F. Memory and flexibility of cytokine gene expression as separable properties of human T(H)1 and T(H)2 lymphocytes. Nat Immunol. 2003;4:78–86. doi: 10.1038/ni872. [DOI] [PubMed] [Google Scholar]