As mentioned above, the combination of antithymocyte globulin of horse origin and cyclosporine A is the standard treatment for aplastic anemia in patients not eligible for bone marrow transplantation. The authors hypothesized that the addition of sirolimus to standard horse antithymocyte globulin and cyclosporine A would improve response rates in severe aplastic anemia, due to its complementary and synergistic properties to cyclosporine A. Despite a theoretical rationale for its use, unfortunately sirolimus did not improve the response rate. See related perspective article on page 310.
Keywords: aplastic anemia, antithymocyte globulin, cyclosporine, sirolimus, immunosuppression, pancytopenia
Abstract
Background
We hypothesized that the addition of sirolimus to standard horse antithymocyte globulin (h-ATG) and cyclosporine (CsA) would improve response rates in severe aplastic anemia, due to its complementary and synergistic properties to cyclosporine A.
Design and Methods
To test this hypothesis, we conducted a prospective randomized study comparing hATG/CsA/sirolimus to standard h-ATG/CsA. A total of 77 patients were treated from June 2003 to November 2005; 35 received h-ATG/CsA/sirolimus and 42 h-ATG/CsA. The two groups were well matched demographically and in blood counts prior to therapy. The primary end-point was hematologic response rate at 3 months, defined as no longer meeting the criteria for severe aplastic anemia. The study was powered to show a superior hematologic response rate of h-ATG/CsA/sirolimus compared to standard h-ATG/CsA.
Results
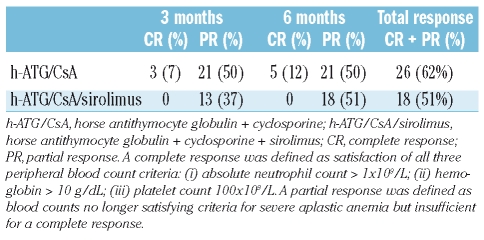
The overall response rate at 3 months was 37% for h-ATG/CsA/sirolimus and 50% for h-ATG/CsA and at 6 months 51% for h-ATG/CsA/sirolimus and 62% for h-ATG/CsA. After a planned interim analysis of 30 evaluable patients in each arm, accrual to the h-ATG/CsA/sirolimus arm was closed, as the conditional power for rejecting the null hypothesis was less than 1%. The rate of relapse, clonal evolution, and survival (secondary outcomes) did not differ significantly between patients treated with the two different regimens.
Conclusions
Despite a theoretical rationale for its use, sirolimus did not improve the response rate in patients with severe aplastic anemia when compared to standard h-ATG/CsA
Introduction
Severe aplastic anemia (SAA) is a life-threatening bone marrow failure disorder characterized by pancytopenia and a hypocellular bone marrow. Allogeneic bone marrow transplantation and immunosuppressive treatment with antithymocyte globulin (ATG) and cyclosporine (CsA) have dramatically changed the course of this illness, with the 10-year survival rate of patients undergoing either treatment now being about 70%.1 Since most patients are not suitable candidates for hematopoietic stem cell transplantation due to advanced age, lack of a histocompatible sibling (or suitable unrelated donor), presence of comorbidities, inaccessibility to transplantation (most frequent in developing countries), or patient’s choice, our efforts have stressed intensification of immunosuppressive therapy in order to improve response rates and survival, and to decrease the rate of relapse and clonal evolution in SAA.
In our experience and that of others, from one quarter to one third of patients with SAA do not show hematologic improvement after treatment with the standard combination of horse ATG (h-ATG) and CsA, about one third of responders relapse, continued CsA is often required in order to maintain adequate blood counts, clonal evolution occurs in 10-15% of cases, and long-term survival is closely correlated to hematologic recovery following treatment.2–6 Thus, although advances in response rates and survival with combined immunosuppression are encouraging, many patients with SAA are not adequately treated with a single course of standard h-ATG + CsA (h-ATG/CsA) due to unresponsiveness to ATG, relapse and/or clonal evolution. Novel immunosuppressive regimens to circumvent these problems are needed. As the addition of CsA to ATG had marked effects on response rates and survival,7 intensification of immunosuppression with agents that complement or are synergistic to h-ATG/CsA is rational. However, efforts to improve h-ATG/CsA with additional immunosuppressive or immunomodulatory agents have been frustrating. The addition of a third drug, such as high dose corticosteroids, androgens, or mycophenolate mofetil to the standard h-ATG/CsA regimen has not resulted in better response rates or a decrease in relapse and clonal evolution;4,8–10 and the use of cyclophosphamide is controversial because of infectious complications.11
Sirolimus is a macrocyclic antibiotic that blocks the multifunctional serine-threonine kinase, mammalian target of rapamycin (mTOR),12 which mediates both the activation of a co-stimulatory pathway during the G0 and G1 transition and signal transduction cascades following cytokine reception during the G1 phase of T-cell activation.13 The synergism of the combination of CsA/sirolimus has been established in vitro, experimentally and in the clinical setting, mainly in solid organ transplantation.14–17 Sirolimus received FDA approval in 1999 as an adjunct to prevent acute renal allograft rejection. Although CsA blocks T-cell activation by binding to calcineurin and inhibiting calcium-stimulated serine/threonine phosphatase activity, auto-reactive T cells may escape inhibition through calcium-independent (or CsA-resistant) pathways.18 Sirolimus has been shown to block CsA-resistant18 and calcium-independent pathways late in the progression of the T-cell cycle, in contrast to the calcineurin inhibitors (CsA and FK506) which act earlier and only on calcium-dependent pathways.19
We, therefore, postulated that the distinct complementary and synergistic mechanisms of action of sirolimus and CsA would result in further block of activated autoreactive T cells in SAA and lead to improved response rates (and survival) and less relapse. To test this hypothesis, we conducted a prospective randomized study investigating the two different immunosuppressive regimens in patients with SAA who were treatment-naïve. One group received h-ATG/CsA in addition to sirolimus for 6 months (h-ATG/CsA/sirolimus), and the second group received standard h-ATG/CsA for 6 months, followed by a slow taper of CsA with a 25% dose reduction every 3 months, for the subsequent 18 months. The goals of this trial were to determine the effectiveness of sirolimus in patients with SAA as well as the role of a cyclosporine taper in preventing relapses in patients treated with standard h-ATG/CsA.
Design and Methods
Patients
All patients with SAA were treated at the Warren Grant Magnuson Clinical Center or Mark O. Hatfield Clinical Research Center at the National Institutes of Health in Bethesda, MD, USA. The study had a two-arm randomized design comparing the new combined regimen of h-ATG/CsA/sirolimus versus standard h-ATG/CsA. Treatment was assigned by the pharmacy using a block randomization scheme with the assignment probability remaining fixed over the course of the trial; construction of the randomization schedule was based on a table of random numbers. All patients (or legal guardians) signed informed consent according to approved protocols by the Institutional Review Board of the National, Heart, Lung, and Blood Institute. This trial was registered at clinicaltrials.gov as NCT00061360.
Eligibility criteria
All patients older than 2 years of age with SAA were eligible for the study. For protocol entry purposes, SAA was defined as bone marrow cellularity of less than 30% and severe pancytopenia with at least two of the following peripheral blood count criteria: (i) absolute neutrophil count less than 0.5×109/L; (ii) absolute reticulocyte count less than 60×109/L; and (iii) platelet count less than 20×109/L.20 Exclusion criteria were: creatinine greater than 2.5 mg/dL, underlying carcinoma, a diagnosis of Fanconi anemia, prior history of immunosuppressive therapy with ATG, seropositivity for human immunodeficiency virus, evidence of a clonal disorder on bone marrow cytogenetics, pregnancy, significant comorbidities such that imminent death was likely, and inability to understand the investigational nature of the study. Bone marrow biopsy and aspiration, including cytogenetics, were performed before enrollment. For children and young adults (under 40 years of age), chromosomes were assayed after in vitro exposure of lymphocytes to diepoxybutane and to mitomycin C to exclude Fanconi anemia. All patients were tested for paroxysmal nocturnal hemoglobinuria by a flow cytometric assay. The presence of a paroxysmal nocturnal hemoglobinuria clone was defined as the absence of glycosylphosphatidylinositol (GPI)-anchored proteins on more than 1% of neutrophils or red cells and the size of the clone was defined by the highest level of GPI-negative red blood cells or GPI-negative neutrophils.
Immunosuppressive regimens
An ATG skin test was performed to assess allergic hypersensitivity. Intravenous h-ATG (ATGAM, Pharmacia & Upjohn Company, Kalamazoo, Mich, USA) was administered at a dose of 40 mg/kg/day for 4 days. Serum sickness prophylaxis with oral prednisone 1 mg/kg/day was given prior to the first dose of h-ATG and continued for 10 days and then tapered over the subsequent 7 days. CsA at 10 mg/kg/day by mouth (15 mg/kg/day for children under 12 years old) in divided doses every 12 h was started on day 1 and continued for at least 6 months. Dosing was adjusted to maintain CsA levels between 200–400 ng/mL. Oral sirolimus 2 mg/day in adults and 1 mg/m2/day in children (< 40 kg) was given on day 1 of ATG and continued for 6 months; the dose was adjusted to maintain sirolimus levels between 5–15 ng/mL. Among responders in the standard h-ATG/CsA arm, CsA was tapered after 6 months with a 25% reduction in dose every 3 months for 18 more months, totaling 2 years of oral CsA. In the h-ATG/CsA/sirolimus arm, both the CsA and the sirolimus were discontinued at 6 months.
As prophylaxis against Pneumocystis carinii pneumonia, all patients received aerosolized pentamidine for at least 6 months. In the h-ATG/CsA/sirolimus arm, valacyclovir at a daily dose of 500 mg for at least 8 weeks was added for Herpes simplex virus prophylaxis after 12 patients had been randomized to this regimen. Granulocyte colony-stimulating factor and prophylactic antimicrobials were not administered routinely with any of the immunosuppressive regimens.
End-points
The primary end-point was hematologic response rate at 3 months, with response being defined as no longer meeting criteria for SAA.20 Secondary end-points included relapse, 6-month response rate, clonal evolution to myelodysplasia or acute leukemia, and overall survival. A complete response was defined as satisfaction of all three peripheral blood count criteria: (i) absolute neutrophil count greater than 1×109/L; (ii) hemoglobin greater than 10 g/dL; and (iii) platelet count greater than 100×109/L. A partial response was defined as blood counts no longer satisfying criteria for SAA but insufficient for a complete response. Patients who relapsed by definition required reinstitution or augmentation of the dose of CsA or administration of another course of ATG.2 Patients underwent bone marrow biopsy at 3, 6, and 12 months, and then yearly. Evolution to myelodysplasia was defined as the appearance of a new clonal disorder on cytogenetics or characteristic morphological changes on bone marrow.
Statistical methods
The study was designed to accrue 60 patients per arm for a total of 120 patients. This sample size was calculated based on the primary end-point, the 3-month response rate, and the assumption that this rate for the h-ATG/CSA arm was 60%.20 At a 5% significance level and with 80% power in a two-sided test, 60 patients per treatment arm were required to detect a 25% difference (60% for the ATG/CsA arm and 85% for the ATG/CsA/sirolimus arm) for the 3-month response rate. The response rates between the two treatment arms were calculated and compared using the two-sample t test. Patients’ characteristics were described using summary statistics including means, proportions, standard errors and 95% confidence intervals. p values for comparing these patients’ characteristics between the two treatment groups were calculated using t tests. Survival analyses based on the Kaplan-Meier method and Cox proportional hazard models were used to draw inferences about the distributions of the overall survival of patients in the two treatment groups. Cumulative event distributions were analyzed using the Kaplan-Meier method and Cox proportional hazard models for time-to-relapse among patients who responded to the first immunosuppressive treatments and time-to-evolution for all the patients. Log-rank p values based on the Cox proportional hazard models were used to compare the survival and cumulative event curves between patients in the two treatment groups. For analyses of time-to-relapse and time-to-evolution distributions, patients who died or underwent stem cell transplantation before relapse or evolution were counted as censored. One patient in the h-ATG/CsA/sirolimus arm died in a traffic accident and was counted as censored for the purpose of statistical analyses. One interim analysis was planned when 30 patients per treatment arm (half of the overall sample size) were evaluable for 3-month responses. The study was monitored to ensure that treatment-related mortality did not substantially exceed an anticipated rate.
Results
Seventy-seven consecutive patients with SAA ages 4–78 years received an initial course of immunosuppressive therapy between June 2003 and October 2005. The patients’ characteristics are shown in Table 1 and a summary of the serious adverse events (requiring hospitalization) and noteworthy adverse events is given in Table 2. There were no significant differences in patients’ characteristics or adverse events between the two arms, except for an anticipated higher rate of hypercholesterolemia and hypertriglyceridemia in the sirolimus-treated group. The study accrued 64% of the target number of patients. The Institutional Review Board and the Data and Safety Monitoring Board closed accrual into the h-ATG/CsA/sirolimus arm after an interim analysis showed that the conditional power for rejecting the null hypothesis was less than 1%, and thus it would be extremely unlikely to be able to reject the null hypothesis with the remaining accrual. Three more patients were allowed to enroll into the standard h-ATG/CsA arm, which accounts for the slight inequality in numbers of patients between the two groups.
Table 1.
Patients’ characteristics.
Table 2.
Adverse events.
Response to treatment and relapse
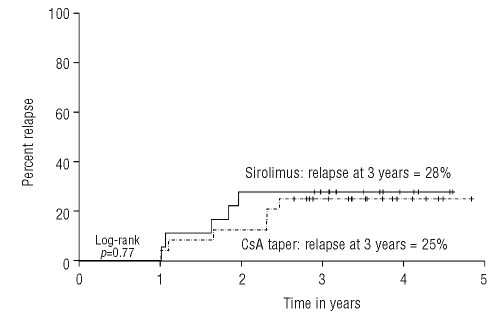
The overall response rate was 37% (13/35) at 3 months and 51% (18/35) at 6 months in the h-ATG/CsA/sirolimus group; and 57% (24/42) at 3 months and 62% (26/42) at 6 months in the h-ATG/CsA group (Table 3). Only two patients responded between 3 and 6 months in the h-ATG/CsA groups and five in the h-ATG/CsA/sirolimus group. The cumulative incidence of relapse at 3 years was 27% for the entire cohort, with no difference noted between the two arms (Figure 1). Eleven patients relapsed: five were in the h-ATG/CsA/sirolimus arm and six were in the h-ATG/CsA arm, of whom four had completed the CsA taper and two who relapsed during tapering. Of the relapsed patients, one died from complications of hematopoietic stem cell transplantation, eight were successfully treated with re-introduction of CsA or a repeat course of immunosuppressive therapy, one successfully underwent a matched related hematopoietic stem cell transplantation, and one has recently received a repeat course of immunosuppressive therapy. One patient in the h-ATG/CsA/sirolimus arm had a borderline response and received a second course of immunosuppressive therapy.
Table 3.
Response to the immunosuppressive regimens.
Figure 1.
Cumulative incidence of relapse in the groups treated with different immunosuppressive regimens. The h-ATG/CsA/sirolimus group (solid line) had a relapse rate of 28% by 3 years and the h-ATG/CsA taper group 25% (dotted line).
Survival and clonal evolution
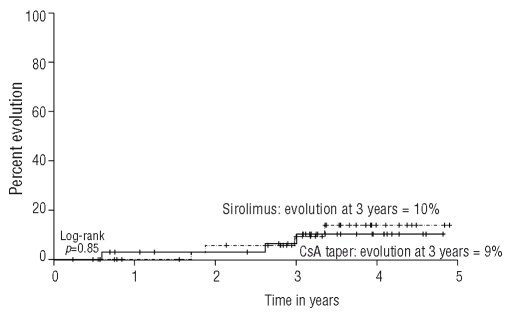
Seven patients showed evidence of clonal evolution; three were in the h-ATG/CsA/sirolimus group (one loss of chromosome 18, one deletion 13q, and one t(6,14)) and four in the h-ATG/CsA group (three to monosomy 7 and one with complex cytogenetics; Figure 2). Of the three patients who evolved to monosomy 7, one has died, one developed leukemia, and one is receiving only supportive care; the patients with deletion 13q and t(6,14) have responded to immunosuppressive therapy and remain in remission; the patient with loss of chromosome 18 underwent a hematopoietic stem cell transplant from a matched sibling; and the patient with complex cytogenetics is receiving supportive care.
Figure 2.
Cumulative incidence of disease evolution among the patients treated with each of the two immunosuppressive regimens. The evolution rate for the h-ATG/CsA/sirolimus arm (dotted line) was not different from that in the h-ATG/CsA taper arm (solid line).
Four patients who were refractory and one who relapsed in the h-ATG/CsA/sirolimus arm underwent hematopoietic stem cell transplantation (three from a matched related sibling and two from an unrelated donor), and five who were refractory and one who relapsed in the h-ATG/CsA arm underwent transplantation (four from a matched related sibling and two from an unrelated donor). Of the seven patients who received a graft from a matched sibling, six are alive, and of the four whose graft was from an unrelated donor, three are alive. After a median follow-up of 42 months, the median survival had not been reached in either arm (Figure 3). In total, eight patients died; five were in the h-ATG/CsA arm and three in the h-ATG/CsA/sirolimus arm. Three succumbed to infectious complications (two fungal and one catheter-related infection), two died from transplant-related complications (one was transplanted from a matched sibling donor and the other from an unrelated donor), one died of heart failure, one died in a car accident, and one expired at home of unknown causes. Overall, there were no significant differences in primary or secondary outcomes between the two arms.
Figure 3.
Overall survival for patients in the h-ATG/CsA/sirolimus (solid line) and h-ATG/CsA taper arm (dotted line). Patients who underwent hematopoietic stem cell transplantation were censored at the time of transplantation.
Discussion
Despite a strong theoretical rationale for its use, our study shows that the addition of sirolimus to standard h-ATG/CsA provided no significant benefit in outcome in SAA. Results using standard h-ATG/CsA were in accordance with our historical data, including a hematologic response rate of about 60%.2 These results were surprising, as sirolimus has been shown to be effective in treatment or prevention in several models of autoimmune disease including collagen-induced arthritis, streptococcal cell-wall induced arthritis, systemic lupus erythematosus, and experimental autoimmune uveoretinitis,21–25 and strong synergism has been shown in the suppression of lymphocyte proliferation against autoantigens in an experimental model of autoimmune uveore-tinitis.25 In clinical trials, the benefit of the combination of CsA-sirolimus has also been impressive: large prospective multicenter trials in solid organ transplantation using randomized and blinded designs showed that the addition of sirolimus to CsA/prednisone regimens reduced the incidence of acute rejection and graft failure;17,26 and in severe chronic plaque psoriasis, the combination of CsA-sirolimus was shown to be superior to either drug alone in a double-blind study.27 The use of sirolimus has also enabled cyclosporine withdrawal in the renal post-transplant setting as well as in the development of corticosteroid-sparing immunosuppressive regimens in islet cell transplantation in patients with type 1 diabetes mellitus, resulting in decreased toxicities from both CsA and corticosteroids.28,29
It is unclear why sirolimus did not yield an improvement in outcomes in SAA compared to those achieved by standard h-ATG/CsA in our study. CsA-resistant pathways have been reported in T cells (which are sensitive to sirolimus),18 but we infer from our negative clinical results that they do not appear to have a significant role in the pathogenesis of SAA. Sirolimus may have had a myelosuppressive effect that was difficult to discern in our population of patients, but no greater risk of infectious complications (other than Herpes simplex) was observed in this group compared to in the group given only h-ATG/CsA. It is possible that further immunomodulation beyond h-ATG/CsA cannot result in better response rates, if success in a minority of patients is limited by their stem cell number or a non-immune pathophysiology. Such a distinction cannot be readily determined in either the research laboratory or in clinical practice. However, hematologic responses in 30–70%30,31 of cases following second treatment with ATG make plausible the inference that some patients who initially failed to benefit from ATG treatment have been inadequately immunosuppressed.
Our study was not able to define the effect of sirolimus on relapse due to the small number of responders in this group, but the relapse rate did not seem to differ from that observed in h-ATG/CsA-treated patients. In addition, the effect of CsA-tapering could not be determined in this study among those who received standard immunosuppressive therapy, since accrual was halted after 42 patients had been treated. However, CsA-tapering is a component of our subsequent prospective studies, which will provide insight into its effect in preventing relapse. Despite a lower response rate in the h-ATG/CsA/sirolimus arm, no difference in survival between the two groups was observed, consequent to the improved outcomes among non-responders to immunosuppressive treatment in recent years due to better supportive care and more effective salvage therapies.32
Achieving a robust response to immunosuppressive therapy remains a primary goal in the management of SAA, as it correlates to better long-term survival and transfusion-independence.2 Unfortunately, the results of recent efforts, adding mycophenolate mofetil8 and in the current study sirolimus to standard h-ATG/CsA have been disappointing, as response rates have remained at about 60% since the addition of CsA to h-ATG about 20 years ago.7 Whether intensification by adding immunosuppressive agents to standard h-ATG and CsA will result in higher response rates remains uncertain but increasingly unlikely. Future investigational regimens that focus on increasing initial lymphocytotoxicity may prove better alternatives.
Acknowledgments
we would like to acknowledge Vu Haphuong for carefully conducting the laboratory data entry.
Footnotes
Funding: this research was supported by the Intramural Research Program of the NIH, National Heart, Lung and Blood Institute.
Authorship and Disclosures
PS is the principal investigator and participated in the primary conception of the study, writing the protocol, performing the research, data collection and analysis, and drafted the manuscript; COW did all the statistical analyses and participated in interim discussions; ON participated in the data collection; PS and CB collected all information on adverse events; EMS was involved in the patients’ care and execution of the study; NSY participated in the primary conception of the study, protocol development, data analysis, interim analysis and discussions, and writing of the manuscript.
The authors reported no potential conflicts of interest.
References
- 1.Locasciulli A, Oneto R, Bacigalupo A, Socie G, Korthof ET, Bekassy A, et al. Outcomes of patients with acquired aplastic anemia given first line bone marrow transplantation or immunosuppressive treatment in the last decade: a report from the European Group for Blood and Marrow Transplantation. Haematologica. 2007;92:11–8. doi: 10.3324/haematol.10075. [DOI] [PubMed] [Google Scholar]
- 2.Rosenfeld S, Follman D, Nu¤ez O, Young NS. Antithymocyte globulin and cyclosporine for severe aplastic anemia. Association between hematologic response and long-term outcome. JAMA. 2003;289:1130–5. doi: 10.1001/jama.289.9.1130. [DOI] [PubMed] [Google Scholar]
- 3.Bacigalupo A, Bruno B, Saracco P, Di Bona E, Locasciulli A, Locatelli F, et al. Antilymphocyte globulin, cyclosporine, prednisolone, and granulocyte colony-stimulating factor for severe aplastic anemia: an update of the GITMO/EBMT study on 100 patients. European Group for Blood and Marrow Transplantation (EBMT) Working Party on Severe Aplastic Anemia and the Gruppo Italiano Trapianti di Midollo Osseo (GITMO) Blood. 2000;95:1931–4. [PubMed] [Google Scholar]
- 4.Kojima S, Hibi S, Kosaka Y, Yamamoto M, Tsuchida M, Mugishima H, et al. Immunosuppressive therapy using antithymocyte globulin, cyclosporine, and danazol with or without human granulocyte colony-stimulating factor in children with acquired aplastic anemia. Blood. 2000;96:2049–54. [PubMed] [Google Scholar]
- 5.Fuhrer M, Rampf U, Baumann I, Faldum A, Niemeyer C, Janka-Schaub G, et al. Immunosuppressive therapy for aplastic anemia in children: a more severe disease predicts better survival. Blood. 2005;106:2102–4. doi: 10.1182/blood-2005-03-0874. [DOI] [PubMed] [Google Scholar]
- 6.Frickhofen N, Heimpel H, Kaltwasser JP, Schrezenmaier H. Anti-thymocyte globulin with or without cyclosporin A: 11-year follow-up of a randomized trial comparing treatments of aplastic anemia. Blood. 2003;101:1236–42. doi: 10.1182/blood-2002-04-1134. [DOI] [PubMed] [Google Scholar]
- 7.Frickhofen N, Kaltwasser JP, Schrezenmeier H, Raghavachar A, Vogt HG, Herrmann F, et al. Treatment of aplastic anemia with antilymphocyte globulin and methylprednisolone with or without cyclosporine. The German Aplastic Anemia Study Group. N Engl J Med. 1991;324:1297–304. doi: 10.1056/NEJM199105093241901. [DOI] [PubMed] [Google Scholar]
- 8.Scheinberg P, Nunez O, Wu C, Young NS. Treatment of severe aplastic anaemia with combined immunosuppression: anti-thymocyte globulin, ciclosporin and mycophenolate mofetil. Br J Haematol. 2006;133:606–11. doi: 10.1111/j.1365-2141.2006.06085.x. [DOI] [PubMed] [Google Scholar]
- 9.Jeng MR, Naidu PE, Rieman MD, Rodriguez-Galindo C, Nottage KA, Thornton DT, et al. Granulocyte-macrophage colony stimulating factor and immunosuppression in the treatment of pediatric acquired severe aplastic anemia. Pediatr Blood Cancer. 2005;45:170–5. doi: 10.1002/pbc.20278. [DOI] [PubMed] [Google Scholar]
- 10.Gluckman E, Rokicka-Milewska R, Hann I, Nikiforakis E, Tavakoli F, Cohen-Scali S, et al. Results and follow-up of a phase III randomized study of recombinant human-granulocyte stimulating factor as support for immunosuppressive therapy in patients with severe aplastic anaemia. Br J Haematol. 2002;119:1075–82. doi: 10.1046/j.1365-2141.2002.03947.x. [DOI] [PubMed] [Google Scholar]
- 11.Tisdale JF, Dunn DE, Geller NL, Plante M, Nunez O, Dunbar CE, et al. High-dose cyclophosphamide in severe aplastic anemia: a randomized trial. Lancet. 2000;356:1554–9. doi: 10.1016/S0140-6736(00)03126-3. [DOI] [PubMed] [Google Scholar]
- 12.Chung J, Kuo CJ, Crabtree GR, Blenis J. Rapamycin-FKBP specifically blocks growth-dependent activation of and signaling by the 70 kd S6 protein kinases. Cell. 1992;69:1227–36. doi: 10.1016/0092-8674(92)90643-q. [DOI] [PubMed] [Google Scholar]
- 13.Abraham RT, Wiederrecht GJ. Immunopharmacology of rapamycin. Annu Rev Immunol. 1996;14:483–510. doi: 10.1146/annurev.immunol.14.1.483. [DOI] [PubMed] [Google Scholar]
- 14.Kahan BD, Gibbons S, Tejpal N, Chou TC, Stepkowski S. Synergistic effect of the rapamycin-cyclosporine combination: median effect analysis of in vitro immune performances by human T lymphocytes in PHA, CD3, and MLR proliferative and cytotoxicity assays. Transplant Proc. 1991;23:1090–1. [PubMed] [Google Scholar]
- 15.Stepkowski SM, Kahan BD. Rapamycin and cyclosporine synergistically prolong heart and kidney allograft survival. Transplant Proc. 1991;23:3262–4. [PubMed] [Google Scholar]
- 16.MacDonald AS. A worldwide, phase III, randomized, controlled, safety and efficacy study of a sirolimus/cyclosporine regimen for prevention of acute rejection in recipients of primary mismatched renal allografts. Transplantation. 2001;71:271–80. doi: 10.1097/00007890-200101270-00019. [DOI] [PubMed] [Google Scholar]
- 17.Kahan BD. Efficacy of sirolimus compared with azathioprine for reduction of acute renal allograft rejection: a randomised multicentre study. The Rapamune US Study Group. Lancet. 2000;356:194–202. doi: 10.1016/s0140-6736(00)02480-6. [DOI] [PubMed] [Google Scholar]
- 18.Ghosh P, Buchholz MA, Yano S, Taub D, Longo DL. Effect of rapamycin on the cyclosporin A-resistant CD28-mediated costimulatory pathway. Blood. 2002;99:4517–24. doi: 10.1182/blood-2001-11-0062. [DOI] [PubMed] [Google Scholar]
- 19.Kay JE, Kromwel L, Doe SE, Denyer M. Inhibition of T and B lymphocyte proliferation by rapamycin. Immunology. 1991;72:544–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenfeld SJ, Kimball J, Vining D, Young NS. Intensive immunosuppression with antithymocyte globulin and cyclosporine as treatment for severe acquired aplastic anemia. Blood. 1995;85:3058–65. [PubMed] [Google Scholar]
- 21.Carlson RP, Baeder WL, Caccese RG, Warner LM, Sehgal SN. Effects of orally administered rapamycin in animal models of arthritis and other autoimmune diseases. Ann NY Acad Sci. 1993;685:86–113. doi: 10.1111/j.1749-6632.1993.tb35855.x. [DOI] [PubMed] [Google Scholar]
- 22.Warner LM, Adams LM, Sehgal SN. Rapamycin prolongs survival and arrests pathophysiologic changes in murine systemic lupus erythematosus. Arthritis Rheum. 1994;37:289–97. doi: 10.1002/art.1780370219. [DOI] [PubMed] [Google Scholar]
- 23.Roberge FG, Xu D, Chan CC, de Smet MD, Nussenblatt RB, Chen H. Treatment of autoimmune uveoretinitis in the rat with rapamycin, an inhibitor of lymphocyte growth factor signal transduction. Curr Eye Res. 1993;12:197–203. doi: 10.3109/02713689308999487. [DOI] [PubMed] [Google Scholar]
- 24.Yocum DE. Cyclosporine, FK-506, rapamycin, and other immunomodulators. Rheum Dis Clin North Am. 1996;22:133–54. doi: 10.1016/s0889-857x(05)70266-0. [DOI] [PubMed] [Google Scholar]
- 25.Martin DF, DeBarge LR, Nussenblatt RB, Chan CC, Roberge FG. Synergistic effect of rapamycin and cyclosporin A in the treatment of experimental autoimmune uveoretinitis. J Immunol. 1995;154:922–7. [PubMed] [Google Scholar]
- 26.MacDonald AS. A worldwide, phase III, randomized, controlled, safety and efficacy study of a sirolimus/cyclosporine regimen for prevention of acute rejection in recipients of primary mismatched renal allografts. Transplantation. 2001;71:271–80. doi: 10.1097/00007890-200101270-00019. [DOI] [PubMed] [Google Scholar]
- 27.Reitamo S, Spuls P, Sassolas B, Lahfa M, Claudy A, Griffiths CE. Efficacy of sirolimus (rapamycin) administered concomitantly with a subtherapeutic dose of cyclosporin in the treatment of severe psoriasis: a randomized controlled trial. Br J Dermatol. 2001;145:438–45. doi: 10.1046/j.1365-2133.2001.04376.x. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E, Warnock GL, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med. 2000;343:230–8. doi: 10.1056/NEJM200007273430401. [DOI] [PubMed] [Google Scholar]
- 29.Johnson RW, Kreis H, Oberbauer R, Brattstrom C, Claesson K, Eris J. Sirolimus allows early cyclosporine withdrawal in renal transplantation resulting in improved renal function and lower blood pressure. Transplantation. 2001;72:777–86. doi: 10.1097/00007890-200109150-00007. [DOI] [PubMed] [Google Scholar]
- 30.Di Bona E, Rodeghiero F, Bruno B, Gabbas A, Foa P, Locasciulli A, et al. Rabbit antithymocyte globulin (r-ATG) plus cyclosporine and granulocyte colony stimulating factor is an effective treatment for aplastic anaemia patients unresponsive to a first course of intensive immunosuppressive therapy. Br J Haematol. 1999;107:330–4. doi: 10.1046/j.1365-2141.1999.01693.x. [DOI] [PubMed] [Google Scholar]
- 31.Scheinberg P, Nunez O, Young NS. Retreatment with rabbit anti-thymocyte globulin and ciclosporin for patients with relapsed or refractory severe aplastic anaemia. Br J Haematol. 2006;133:622–7. doi: 10.1111/j.1365-2141.2006.06098.x. [DOI] [PubMed] [Google Scholar]
- 32.Scheinberg P, Wu CO, Nunez O, Young NS. Marked improvement in short- and long-term survival in severe aplastic anemia patients treated with immunosuppression in the past 18 years. ASH Annual Meeting Abstracts. 2007;110:506. [Abstract] [Google Scholar]