Abstract
Objective
HIV prevention has been ongoing in Lusaka for many years. Recent reports suggest a possible decline in HIV sero-incidence in Zambia and some neighbouring countries. This study aimed to examine trends in HIV seroprevalence among pregnant and parturient women between 2002 and 2006.
Methods
We analysed HIV seroprevalence trends from two Lusaka sources: (i) antenatal data from a city-wide programme to prevent mother-to-child HIV transmission, and (ii) delivery data from two anonymous unlinked cord-blood surveillances performed in 2003 and again in 2005–2006, where specimens from > 97% of public-sector births in each period were obtained and analysed.
Findings
Between July 2002 and December 2006, the Lusaka district tested 243 302 antenatal women for HIV; 54 853 (22.5%) were HIV infected. Over this period, the HIV seroprevalence among antenatal attendees who were tested declined steadily from 24.5% in the third quarter of 2002 to 21.4% in the last quarter of 2006 (P < 0.001). The cord-blood surveillances were conducted between June and August 2003 and again between October 2005 and January 2006. Overall HIV seroprevalence declined from 25.7% in 2003 to 21.8% in 2005–2006 (P = 0.001). Among women ≤ 17 years of age, seroprevalence declined from 12.1% to 7.7% (P = 0.015).
Conclusion
HIV seroprevalence appears to be declining among antenatal and parturient women in Lusaka. The decline is most dramatic among women ≤ 17 years of age, suggesting a reduction in sero-incidence in this important age group.
Résumé
Objectif
La prévention de l’infection par le VIH est pratiquée à Lusaka depuis de nombreuses années. Les rapports récents laissent entrevoir un déclin de la séroincidence du VIH en Zambie et dans certains pays voisins. L’objectif de la présente étude est d’examiner les tendances de la séroprévalence du VIH chez les femmes enceintes et les parturientes entre 2002 et 2006.
Méthodes
Nous avons analysé les tendances de la séroprévalence du VIH à partir de deux sources d’informations provenant de Lusaka : (i) les données anténatales d’un programme couvrant la ville et visant à prévenir la transmission mère-enfant du VIH et (ii) des données d’accouchement fournies par deux surveillances à partir du sang du cordon, anonymes et non reliées, réalisées en 2003, puis une nouvelle fois sur la période 2005-2006, dans lesquelles on a prélevé et analysé des échantillons pour plus de 97 % des naissances intervenues dans le secteur public sur chacune des périodes précitées.
Résultats
Entre juillet 2002 et décembre 2006, le district de Lusaka a pratiqué plus de 243 302 dépistages du VIH chez des femmes enceintes, parmi lesquelles 54 853 (22,5 %) étaient infectées par ce virus. Sur cette période, la séroprévalence du VIH parmi les femmes enceintes testées a baissé constamment, passant de 24,5% au troisième trimestre 2002 à 21,4% au dernier trimestre 2006 (p < 0,001). Les surveillances à partir du sang du cordon ont été menées entre juin et août 2003 et entre octobre 2005 et janvier 2006. Globalement, la séroprévalence du VIH est tombée de 25,7 % en 2003 à 21,8 % en 2006-2006 (p = 0,01). Chez les femmes de 17 ans et moins, la séroprévalence est passée de 12,1 % à 7,7 % (p = 0,015).
Conclusion
La séroprévalence du VIH semble baisser chez les femmes enceintes et les parturientes de Lusaka. C’est chez les femmes de 17 ans et moins que cette baisse est la plus forte, ce qui suggère une diminution de la séroincidence dans cette importante tranche d’âge.
Resumen
Objetivo
Desde hace ya muchos años se aplican en Lusaka medidas de prevención de la infección por VIH. Algunos datos recientes parecen indicar que se ha producido una disminución de la seroincidencia de VIH en Zambia y en algunos países vecinos. El objetivo de este estudio fue examinar las tendencias de la seroprevalencia de VIH entre las mujeres embarazadas y parturientas entre 2002 y 2006.
Métodos
Analizamos las tendencias de la seroprevalencia de VIH en Lusaka a partir de dos fuentes: (i) datos prenatales de un programa de prevención de la transmisión del VIH de la madre al niño que abarcaba toda la ciudad, y (ii) datos sobre partos extraídos de dos sistemas anónimos independientes de vigilancia de la sangre de cordón umbilical aplicados en 2003 y de nuevo en 2005–2006, que permitieron obtener y analizar muestras en más del 97% de los nacimientos registrados en el sector público en cada periodo.
Resultados
Entre julio de 2002 y diciembre de 2006, el distrito de Lusaka analizó la serología VIH de 243 302 mujeres que recibieron atención prenatal; 54 853 (22,5%) estaban infectadas por el virus. A lo largo de ese periodo, la seroprevalencia de VIH entre las mujeres que recibieron atención prenatal y se sometieron a los análisis disminuyó de forma sostenida del 24,5% en el tercer trimestre de 2002 al 21,4% en el último trimestre de 2006 (p < 0,001). Las medidas de vigilancia de la sangre de cordón se aplicaron entre junio y agosto de 2003 y, nuevamente, entre octubre de 2005 y enero de 2006. La seroprevalencia global de VIH cayó del 25,7% en 2003 al 21,8% en 2005–2006 (p = 0,001). Entre las mujeres ≤ 17 años, la seroprevalencia disminuyó del 12,1% al 7,7% (p = 0,015).
Conclusión
La seroprevalencia de VIH parece estar disminuyendo entre las mujeres en fase prenatal y parturientas en Lusaka. La reducción es especialmente acusada entre las muchachas ≤ 17 años, lo que lleva a pensar en una reducción de la seroincidencia en ese importante grupo de edad.
ملخص
الغرض
تتواصل جەود الوقاية من فيروس الإيدز في لوزاكا منذ سنوات عديدة. وتشير التقارير الحديثة إلى إمكانية انخفاض معدل الوقوع المصلي لفيروس الإيدز في زامبيا وبعض البلدان المجاورة لەا. وقد استەدفت ەذە الدراسة الوقوف على اتجاەات الانتشار المصلي لفيروس الإيدز بين السيدات الحوامل والماخضات في الفترة من 2002 إلى 2006.
الطريقة
أجرى الباحثون تحليلاً لاتجاەات الانتشار المصلي لفيروس الإيدز من مصدرين في لوزاكا، ەما: (أ) معطيات سابقة للولادة مستمدة من برنامج لاتقاء سراية الفيروس من الأم إلى الطفل، منفَّذ على مستوى المدينة، (ب) معطيات أثناء الولادة مستمدة من دراستين منفصلتين غافلتين عن الأسماء، أجريتا في عام 2003 ثم في 2005-2006، لترصُّد دم الحبل السُّري، حيث تم أخذ وتحليل عينات من أكثر من 97% من الولادات التي تمت في مرافق القطاع العام في كل فترة من الفترتين.
الموجودات
قامت منطقة لوزاكا في الفترة من تموز/يوليو 2002 إلى كانون الأول/ديسمبر 2006 بتحري فيروس الإيدز لدى 302 243 امرأة قبل الولادة؛ وكان 853 54 منەن (نسبة 22.5%) مصابات بعدوى الفيروس. وتبين أيضاً خلال ەذە الفترة أن الانتشار المصلي للفيروس بين المترددات على العيادات قبل الولادة، اللاتي تم اختبارەن، قد انخفض بشكل منتظم من 24.5% في الربع الثالث من عام 2002 إلى 21.4% في الربع الأخير من عام 2006 (نسبة الاحتمال أقل من 0.001). وأُجريت دراسات ترصد دم الحبل السُّري في الفترة من حزيران/يونيو إلى آب/أغسطس 2003، ثم في الفترة من تشرين الأول/أكتوبر 2005 إلى كانون الثاني/يناير 2006. ولوحظ انخفاض عـام في الانتشـار المصلي لفيروس الإيـدز مـن 25.7% في عـام 2003 إلى 21.8% في الفترة 2005-2006 (نسبة الاحتمال = 0.001). وانخفض الانتشار المصلي بين السيـدات اللاتي ەن في عمـر 17 عاماً أو أقل، من 12.1% إلى 7.7% (نسبة الاحتمال = 0.015).
الاستنتاج
يبدو أن الانتشار المصلي لفيروس الإيدز آخذ في الانخفاض بين السيدات اللاتي ەن في عمر 17 عاماً أو أقل، مما يوحي بانخفاض في الوقوع المصلي للفيروس في ەذە الفئة العمرية المەمة.
Introduction
Lusaka is the largest city in Zambia and is among those places most heavily burdened by HIV.1,2 Public-sector antenatal and delivery care occurs in 24 government clinics that are spread throughout the city. Each year, there are approximately 45 000 births in this system. In late 2001, the Zambian government began implementing services to prevent mother-to-child HIV transmission (PMTCT) in Lusaka and expanded this to all facilities in just over 2 years.3 Using data available from all Lusaka public-sector obstetrical facilities, we examined trends in HIV seroprevalence among pregnant and parturient women between 2002 and 2006.
Methods
Data sources
We examined data from two sources. The first comprised routinely collected PMTCT data from the Lusaka Urban Health District. In 2002, nine clinics were offering PMTCT services. By January 2004, all clinics were covered. For this analysis, we used data collected between July 2002 and December 2006 from public-sector clinics offering PMTCT. Routine indicators collected at these facilities include: number of new antenatal attendees, number of women counselled for HIV testing, number of women tested for HIV, number of women with positive test results, and numbers of women and infants receiving antiretroviral prophylaxis for PMTCT. These indicators are collected in facility-based log books and aggregated periodically for government reporting. Age data are not routinely collected.
The second data source comes from two anonymous cord-blood surveillance exercises performed in Lusaka to evaluate the effectiveness of PMTCT services. Details of the surveillance methodology have been described elsewhere.4 Since maternal IgG (gamma globulin) anti-HIV antibodies cross the placenta freely throughout pregnancy, seropositivity of umbilical-cord blood indicates maternal HIV infection. The first surveillance was conducted for 12 weeks between 7 June 2003 and 31 August 2003. The second surveillance was conducted for 10 weeks between 12 October 2005 and 15 January 2006, with a hiatus between 12 November and 2 December 2005 during which time no specimens were collected. In each surveillance exercise, cord blood was obtained from discarded placentas of almost all liveborn infants (> 97% of births) in all Lusaka public-sector delivery facilities. Specimens were analysed for maternal HIV serostatus using a single rapid HIV antibody test (Determine HIV1/2; Abbott Laboratories, Abbott Park, IL, United States of America).
Ethical approval
Cord-blood surveillance activities received ethical approval from both the University of Zambia Research Ethics Committee and the University of Alabama at Birmingham Institutional Review Board for Human Use. The programmatic analysis of the Lusaka District PMTCT programme was deemed exempt from human subjects review by the same two committees.
Analysis
Programmatic data on HIV prevalence were aggregated over periods of 3 months to provide stability for individual period estimates. We used the Cochran-Armitage test to evaluate the trend in HIV prevalence over time and used logistic regression to produce predicted probabilities of maternal HIV-positive status over the course of the programme. Since HIV-prevalence rates may vary geographically, and not all sites had PMTCT services until the beginning of 2004, we also evaluated site-specific estimates by examining each site separately over time and by employing generalized linear mixed models with random coefficient analysis.5
For analysis of the cord-blood surveillances, we restricted the data to women who received their antenatal care in Lusaka to maximize comparability with the antenatal data. We used the χ² test to compare HIV prevalence rates (overall and stratified by age) between the two surveillance exercises. We used Wilson’s method6 to generate confidence intervals around prevalence estimates in both the programmatic data and the cord-blood surveillance. Analyses were performed with SAS 9.1 (SAS Institute, Cary, NC, USA) and S-Plus 6.1 (Insightful Corporation, Seattle, WA, USA.).
Results
Programmatic PMTCT data
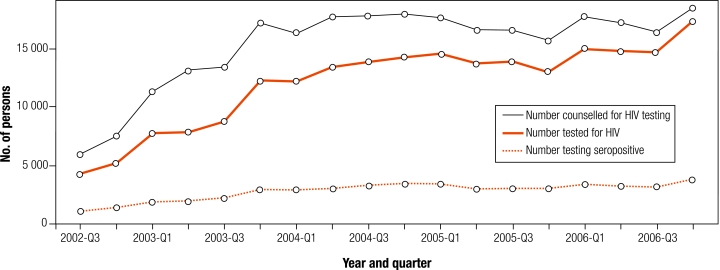
From July 2002 to December 2006, the proportion of women attending antenatal care clinics who accepted HIV testing increased steadily over the evaluation period (71% to 94%; P < 0.001; Fig. 1). During that same period, the absolute number of women testing positive for HIV also increased. However, as a proportion of those accepting testing, the number testing positive declined from approximately 24.5% (3rd quarter 2002) to 21.4% (4th quarter 2006; Cochran-Armitage trend test < 0.001). Yearly seroprevalences were 24.8% (2002); 24.0% (2003); 23.0% (2004); 22.3% (2005); and 21.6% (2006). In a site-specific analysis, we observed a decreasing seroprevalence in 21 of 24 sites (Table 1). These site-specific declines were statistically significant (P < 0.05) in 11 sites. In three sites, the trend was slightly positive, but did not achieve statistical significance.
Fig. 1.
Uptake of HIV testing among antenatal attendees and parturients in Lusaka, Zambiaa
a Uptake of HIV testing among women attending antenatal care in public sector facilities in Lusaka.
Table 1. HIV seroprevalence among women tested for HIV in antenatal care at 24 public sector clinics in Lusaka, Zambia.
| Clinic | Yeara |
Trendb | P-value | ||||
|---|---|---|---|---|---|---|---|
| 2003 | 2004 | 2005 | 2006 | ||||
| Bauleni | 22.2 | 21.5 | 19.7 | 18.5 | –2.18 | 0.03 | |
| Chianama | 25.5 | 23 | 20.3 | 16.6 | –4.13 | < 0.0001 | |
| Chainda | 22.1 | 20.2 | 19.8 | 17 | –2.51 | 0.012 | |
| Chawama | 22.2 | 20.5 | 23.1 | 22.6 | 1.65 | 0.099 | |
| Chazanga | 17 | 20.1 | 16.9 | 18.1 | –0.77 | 0.444 | |
| Chelstone | 25.1 | 20.2 | 19.3 | 22.1 | –2.32 | 0.020 | |
| Chilenje | 23.7 | 19.4 | 18 | 18.5 | –2.89 | 0.004 | |
| Chipata | 23.9 | 24.2 | 21.7 | 20.4 | –4.29 | < 0.0001 | |
| Civic Center | 28.3 | 26.3 | 25.8 | 26.9 | –0.70 | 0.483 | |
| George | 22.9 | 24.1 | 24.1 | 22.5 | –0.78 | 0.439 | |
| Kabwata | 24.5 | 23.8 | 24.5 | 22.3 | –1.44 | 0.151 | |
| Kalingalinga | 24.8 | 24.9 | 24.6 | 25.5 | 0.40 | 0.69 | |
| Kamwala | 27.7 | 25.8 | 23 | 23 | –5.29 | < 0.0001 | |
| Kanyama | 23 | 24.6 | 22.4 | 22.5 | –1.60 | 0.109 | |
| Kaunda Square | 25.3 | 23.2 | 22.6 | 18.1 | –3.38 | 0.001 | |
| Lilayi | 18.3 | 18 | 17.8 | 9.2 | –6.33 | < 0.0001 | |
| Makeni | 20.4 | 21.5 | 21.1 | 19.6 | –0.95 | 0.341 | |
| Mandevu | 27.1 | 24.9 | 22.3 | 23.5 | –3.19 | 0.001 | |
| Matero Main | 28 | 22.7 | 30.4 | 27.5 | –0.032 | 0.974 | |
| Matero Reference | 25.3 | 26.5 | 25.2 | 23.9 | –1.88 | 0.06 | |
| Mtendere | 22.6 | 21.6 | 21 | 20.3 | –2.08 | 0.037 | |
| Ngombe | 19.4 | 21 | 19.8 | 17.9 | –1.25 | 0.212 | |
| Railway | 24.7 | 21.7 | 23.4 | 25.1 | 0.882 | 0.378 | |
| State Lodge | 16.4 | 13 | 15.7 | 11.8 | –1.12 | 0.264 | |
a The year 2002 is omitted because only partial year data are available. b Trend statistic is Z score derived from Cochran-Armitage test of quarterly prevalence data between 3rd quarter of 2002 and 4th quarter of 2006. A negative trend indicates declining prevalence over time.
The generalized linear mixed models with random coefficients analysis estimated the average decline in the site-specific HIV prevalence rates of about 1% per year (0.988%, P < 0.001). This rate of decline is slightly greater than that estimated by the logistical model, which does not consider site variation in its estimate (Fig. 2).
Fig. 2.
Seroprevalence among antenatal attendees and parturients in Lusaka, Zambiaa
a The logistical regression line represents the most conservative estimate of seroprevalence decline. A generalized linear mixed model with random coefficient analysis fits a steeper curve, as does a simple connection of the two cord-blood surveillance estimates.
Cord-blood surveillance data
The first cord-blood survey occurred between 7 June 2003 and 31 August 2003. Over this period, 10 384 women gave birth to liveborn infants in public-sector facilities in Lusaka and 10 194 (98%) analysable specimens were obtained. Of these, 8787 (86%) received antenatal care in Lusaka, of which 2255 (25.7%) were seropositive. The second surveillance was conducted between 12 October 2005 and 12 November 2005 and then again between 3 December 2005 and 15 January 2006. Over the period of the 2005–2006 cord-blood surveillance, 7665 women gave birth to liveborn infants in public-sector facilities in Lusaka and 7438 (97%) analysable specimens were obtained. Of these, 6756 (88%) received antenatal care in Lusaka, of which 1473 (21.8%) were seropositive (Fig. 2).
In women ≤ 17 years of age, the HIV seroprevalence declined 37% between the two surveillance periods, from 12.1% (77/635) in 2003 to 7.7% (37/481) in 2005–2006 (P = 0.015). Similarly, HIV seroprevalence declined among women aged 20–24 from 25.8% (833/3234) to 20.3% (499/2455) (P < 0.001) and among women aged 25–29 from 31.8% (677/2126) to 27.8% (499/1794) (P = 0.006). The HIV seroprevalence did not change significantly in women aged 18–19, 30–34, or ≥ 35 years (Table 2).
Table 2. Age-stratified HIV prevalence among women delivering in all public-sector facilities using cord-blood surveillancesa.
| Age group (years) | 2003 |
2005–2006 |
Relative decrease (%) | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Seroprevalence | Seroprevalence (%) | 95% CI | Seroprevalence | Seroprevalence (%) | 95% CI | |||||
| ≤ 17 | 77/635 | 12.1 | 9.7–14.9 | 37/481 | 7.7 | 5.6–10.5 | 0.36 | 0.015 | ||
| 18–19 | 197/1235 | 16.0 | 14.0–18.1 | 132/924 | 14.3 | 12.1–16.7 | 0.11 | 0.29 | ||
| 20–24 | 833/3234 | 25.8 | 24.3–27.3 | 499/2455 | 20.3 | 18.8–22.0 | 0.21 | < 0.001 | ||
| 25–29 | 677/2126 | 31.8 | 29.9–33.9 | 499/1794 | 27.8 | 25.8–30.0 | 0.13 | 0.006 | ||
| 30–34 | 349/1055 | 33.1 | 30.2–36.0 | 232/798 | 29.1 | 26.0–32.4 | 0.12 | 0.066 | ||
| ≥ 35 | 122/497 | 24.5 | 21.0–28.5 | 74/304 | 24.3 | 19.9–29.5 | 0.01 | 0.948 | ||
| Unknown age | 2/5 | – | – | 1/2 | – | – | – | – | ||
| Total | 2257/8787 | 25.7 | 24.8–26.6 | 1 474/6758 | 21.8 | 20.8–22.8 | 0.15 | < 0.001 | ||
CI, confidence interval. a Exact dates were: 2003 surveillance (7 June 2003–31 August 2003); 2005–2006 surveillance (12 October 2005–12 November 2005 and 2 December 2005–15 January 2006).
Discussion
These data clearly indicate a decline in HIV seroprevalence among pregnant women in Lusaka between 2002 and 2006. The most notable decline occurred among the youngest women (≤ 17 years of age). HIV in this age group declined from 12.1% to 7.7% over a 28-month period. HIV prevalence among adolescents has been proposed as a reasonable surrogate for HIV incidence since this population can be presumed to have become sexually active recently. Use of HIV seroprevalence among adolescents to estimate incidence is particularly useful in settings where more accurate measures of HIV incidence (e.g. detuned antibody assays, pooled RNA testing) are not yet part of widespread surveillance activities.7 Other investigators in Zambia corroborate our findings with notable declines in the youngest age groups and in Lusaka in general.8,9
The primary strength of this analysis lies in the very high ascertainment of samples. The cord-blood surveillance exercises each achieved > 97% specimen ascertainment and, as such, are essentially census surveys of all public-sector births. The antenatal data represent increasing specimen ascertainment over time. When the programme began, not all antenatal sites were offering services yet and testing uptake was around 70%.3 However, testing rates have steadily increased and, since mid-2005, more than 90% of new antenatal attendees are being tested (N Chintu, unpublished). We also know from the cord-blood surveillances that women who refused testing in 2003 were more likely to be seropositive than those who accepted.4 In light of this, it is likely that the decline in seroprevalence represented by the regression line in Fig. 2 may actually under-represent the real decline.
Since these data derive from populations of pregnant women, we should be careful not to make broad generalizations about HIV trends among all adolescents or all women. However, we would anticipate that the HIV seroprevalence among pregnant adolescents would be higher than among adolescents in the general population. Michelo et al. have reported that HIV seroprevalence among urban-dwelling women in Zambia aged 15–19 years declined from 12.3% in 1995 to 7.7% in 2003.9 In addition, the results of the 2005 Zambian Sexual Behaviour Study indicate that the median age of sexual debut declined from 18.5 years to 16.5 years between 2003 and 2005.10
In the oldest age groups of women, the HIV seroprevalence declined only modestly or not at all. This may represent a cohort effect, where HIV-infected women become older between sampling periods and move from one age group to another, but also, we suspect that the slight decline in the older populations may be due to death of infected women.4 As highly active antiretroviral therapy becomes more widespread, and there are potentially fewer people dying from AIDS, we might expect over time that the overall HIV seroprevalence would increase in the older populations.11
With over 37 million adults infected worldwide, and 5.3 million new cases each year, the ultimate solution to the epidemic is to prevent new cases of HIV, especially among young people. Ecological data from Uganda suggest that prevention campaigns are working: condom usage and preventive sexual behaviour has increased simultaneously as the HIV prevalence among the antenatal population has continued to decline.12 As countries work hard to curb the HIV epidemics, these results from the youngest age groups in urban Zambia are encouraging, given the large investments in prevention of HIV. ■
Acknowledgements
We thank the clinicians in the Lusaka Urban District and University Teaching Hospital, whose hard work in the area of PMTCT has saved many thousands of babies and has also made this study possible. We also thank Dr Meade Morgan and Dr Ray Shiraishi of the United States CDC-Atlanta for their help in reviewing this paper for statistical soundness.
Footnotes
Funding: This work was initially supported by the Call-to-Action initiative of the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF) and later by a multicountry grant to EGPAF from the United States CDC (U62/CCU12354). Additional investigator salary support was provided by the National Institutes of Health (K01-TW05708; K01-TW06670; P30-AI027767) and the Elizabeth Glaser Pediatric AIDS Foundation (EGSA 19-02).
Competing interests: None declared.
References
- 1.Demographic and health surveys Measure DHS. Calverton, MD: Macro International Inc. Available from: http://www.measuredhs.com [accessed 21 May 2008].
- 2.Zambia Demographic and Health Survey 2001-2002 Central Statistical Office (Zambia) CBHZORCM, ed.. Lusaka and Maryland: Central Board of Health and ORC Macro; 2003.
- 3.Stringer EM, Sinkala M, Stringer JS, Mzyece E, Makuka I, Goldenberg RL, et al. Prevention of mother-to-child transmission of HIV in Africa: successes and challenges in scaling-up a nevirapine-based program in Lusaka, Zambia. AIDS. 2003;17:1377–82. doi: 10.1097/00002030-200306130-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stringer JS, Sinkala M, Maclean CC, Levy J, Kankasa C, Degroot A, et al. Effectiveness of a city-wide program to prevent mother-to-child HIV transmission in Lusaka, Zambia. AIDS. 2005;19:1309–15. doi: 10.1097/01.aids.0000180102.88511.7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.FitzMaurice Garrett M, Laird Nan M, Ware James H. Applied Longitudinal Analysis New Jersey: John Wiley & Sons; 2004. [Google Scholar]
- 6.Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat. 1998;52:119–26. doi: 10.2307/2685469. [DOI] [Google Scholar]
- 7.McDougal JS, Parekh BS, Peterson ML, Branson BM, Dobbs T, Ackers M, et al. Comparison of HIV type 1 incidence observed during longitudinal follow-up with incidence estimated by cross-sectional analysis using the BED capture enzyme immunoassay. AIDS Res Hum Retroviruses. 2006;22:945–52. doi: 10.1089/aid.2006.22.945. [DOI] [PubMed] [Google Scholar]
- 8.Sandoy IF, Kvale G, Michelo C, Fylkesnes K. Antenatal clinic-based HIV prevalence in Zambia: declining trends but sharp local contrasts in young women. Trop Med Int Health. 2006;11:917–28. doi: 10.1111/j.1365-3156.2006.01629.x. [DOI] [PubMed] [Google Scholar]
- 9.Michelo C, Sandoy IF, Dzekedzeke K, Siziya S, Fylkesnes K. Steep HIV prevalence declines among young people in selected Zambian communities: population-based observations (1995-2003). BMC Public Health. 2006;6:279. doi: 10.1186/1471-2458-6-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MEASURE Evaluation: Zambian Sexual Behavior Survey Zambia: Central Statistical Office, Ministry of Health; March 2005.
- 11.Stringer JS, Zulu I, Levy J, Stringer EM, Mwango A, Chi B, et al. Rapid scale-up of antiretroviral therapy at primary care sites in Zambia: feasibility and early outcomes. JAMA. 2006;296:782–93. doi: 10.1001/jama.296.7.782. [DOI] [PubMed] [Google Scholar]
- 12.Kirungi WL, Musinguzi J, Madraa E, Mulumba N, Callejja T, Ghys P, et al. Trends in antenatal HIV prevalence in urban Uganda associated with uptake of preventive sexual behaviour. Sex Transm Infect. 2006;82(Suppl 1):i36–41. doi: 10.1136/sti.2005.017111. [DOI] [PMC free article] [PubMed] [Google Scholar]