Abstract
Objective
Male circumcision reduces the risk of HIV acquisition by approximately 60%. Male circumcision services are now being introduced in selected populations in sub-Saharan Africa and further interventions are being planned. A serious concern is whether male circumcision can be provided safely to large numbers of adult males in developing countries.
Methods
This prospective study was conducted in the Bungoma district, Kenya, where male circumcision is universally practised. Young males intending to undergo traditional or clinical circumcision were identified by a two-stage cluster sampling method. During the July–August 2004 circumcision season, 1007 males were interviewed 30–89 days post- circumcision. Twenty-four men were directly observed during and 3, 8, 30 and 90 days post-circumcision, and 298 men underwent clinical exams 45–89 days post-procedure. Twenty-one traditional and 20 clinical practitioners were interviewed to assess their experience and training. Inventories of health facilities were taken to assess the condition of instruments and supplies necessary for performing safe circumcisions.
Findings
Of 443 males circumcised traditionally, 156 (35.2%) experienced an adverse event compared with 99 of 559 (17.7%) circumcised clinically (odds ratio: 2.53; 95% confidence interval: 1.89–3.38). Bleeding and infection were the most common adverse effects, with excessive pain, lacerations, torsion and erectile dysfunction also observed. Participants were aged 5 to 21 years and half were sexually active before circumcision. Practitioners lacked knowledge and training. Proper instruments and supplies were lacking at most health facilities.
Conclusion
Extensive training and resources will be necessary in sub-Saharan Africa before male circumcision can be aggressively promoted for HIV prevention. Two-thirds of African men are circumcised, most by traditional or unqualified practitioners in informal settings. Safety of circumcision in communities where it is already widely practised must not be ignored.
Résumé
Objectif
La circoncision masculine réduit le risque d’acquisition du VIH d’environ 60 %. Des services de circoncision masculine sont en cours d’introduction dans certaines populations d’Afrique sub-saharienne et d’autres interventions de ce type sont prévues. Pourrait-on pratiquer sans risque cette intervention sur un grand nombre d’hommes adultes des pays en développement : cette question préoccupe fortement les responsables sanitaires.
Méthodes
Cette étude prospective a été menée dans le district de Bungoma, au Kenya, où la circoncision masculine est universellement pratiquée. Les jeunes hommes s’apprêtant à subir une circoncision traditionnelle ou médicale ont été identifiés par sondage en grappes à deux degrés. Pendant la saison de la circoncision juillet-août 2004, 1007 hommes ont été interrogés 30 à 89 jours après leur circoncision. Vingt-quatre ont fait l’objet d’une observation directe les 3, 8, 30 et 90e jours après l’opération et 298 ont subi des examens cliniques 45 à 89 jours après. Vingt-et-un praticiens traditionnels et 20 praticiens cliniques ont été interrogés pour évaluer leur expérience et leur formation. On a dressé des inventaires dans les établissements de soins pour évaluer la disponibilité des instruments et des fournitures nécessaires pour effectuer sans risque les circoncisions.
Résultats
Parmi les 443 hommes ayant subi une circoncision traditionnelle, 156 (35,2 %) avaient souffert d’effets indésirables contre 99 des 559 (17,7 %) hommes circoncis médicalement (odds ratio : 2,53; intervalle de confiance à 95 % : 1,89-3,38). Les saignements et les infections faisaient partie des effets indésirables les plus courants, mais on relevait également des douleurs excessives, des lacérations, des torsions et des troubles de la fonction érectile. Les participants étaient âgés de 5 à 21 ans et la moitié d’entre eux étaient sexuellement actifs avant l’opération. Les connaissances et la formation des praticiens étaient souvent insuffisantes. La plupart des établissements de soins manquaient d’instruments et de fournitures appropriés.
Conclusion
Avant d’entamer, en Afrique sub-saharienne, une promotion énergique de la circoncision masculine pour prévenir l’infection par le VIH, il faut fournir des moyens importants en formation et en ressources. Deux tiers des Africains sont circoncis, la plupart l’ayant été par des praticiens traditionnels ou non qualifiés, dans le cadre de structures informelles. La sécurité de la circoncision dans les communautés où elle est déjà largement pratiquée ne doit pas être ignorée.
Resumen
Objetivo
La circuncisión masculina reduce el riesgo de contagio del VIH en un 60% aproximadamente. Se están implantando servicios de circuncisión masculina en poblaciones seleccionadas del África subsahariana, al tiempo que se planifican nuevas intervenciones. Un motivo serio de preocupación es la duda sobre si es posible practicar la circuncisión masculina en condiciones seguras a un gran número de varones adultos en los países en desarrollo.
Métodos
Este estudio prospectivo se llevó a cabo en el distrito de Bungoma, Kenya, donde la circuncisión masculina es una práctica generalizada. Mediante un método de muestreo por conglomerados en dos etapas se seleccionó a hombres jóvenes que deseaban someterse a circuncisión, tradicional o médica. Durante los meses de julio y agosto de 2004, 1007 varones fueron entrevistados a los 30-89 días de la intervención. Veinticuatro hombres fueron objeto de observación durante la circuncisión y a los 3, 8, 30 y 90 días de la misma, y 298 fueron sometidos a exploración clínica pasados 45-89 días tras la intervención. Se entrevistó asimismo a 21 prácticos tradicionales y 20 profesionales médicos para evaluar su experiencia y grado de adiestramiento, y se hicieron inventarios de los establecimientos de salud para determinar el estado del instrumental y los suministros necesarios para realizar las circuncisiones de forma segura.
Resultados
De 443 hombres circuncidados por el método tradicional, 156 (35,2%) sufrieron eventos adversos, frente a 99 de los 559 (17,7%) sometidos a circuncisión médica (razón de posibilidades (OR): 2,53; intervalo de confianza del 95%: 1,89-3,38). Hemorragias e infecciones fueron los efectos adversos más comunes, pero se observaron también casos de desgarro, torsión y disfunción eréctil. Los participantes tenían entre 5 y 21 años, y la mitad de ellos eran sexualmente activos antes de la circuncisión. Prácticos y profesionales carecían de los conocimientos y preparación necesarios, y la mayoría de los centros de salud no disponían del instrumental y los suministros adecuados.
Conclusión
Habrá que desplegar un gran esfuerzo de capacitación y abundantes recursos en el África subsahariana antes de poder pasar a fomentar resueltamente la circuncisión masculina como medio de prevención de la infección por VIH. Dos de cada tres hombres africanos han sido circuncidados, la mayoría por prácticos tradicionales o no preparados y en entornos informales. El tema de la seguridad de la circuncisión no debe ser ignorado en las comunidades donde es ya ampliamente practicada.
ملخص
الەدف
يقلّص ختان الذكور مخاطر اكتساب العدوى بفيروس الإيدز بنحو 60%. ويتم الآن إدخال خدمات ختان الذكور بين مجموعات منتقاة من سكان المناطق الواقعة جنوب الصحراء الأفريقية، كما يجري التخطيط للمزيد من المداخلات. وەنالك مخاوف حقيقية بشأن إمكانية إجراء الختان المأمون للذكور لعدد كبير من الذكور البالغين في البلدان النامية.
الطريقة
أُجريت ەذە الدراسة الاستطلاعية في منطقة بنغوما، في كينيا، حيث يُمارس ختان الذكور ممارسة واسعة الانتشار. وتم تحديد صغار الذكور الذين يودون إجراء الختان الشعبي أو السريري من خلال طريقة (اعتيان المجموعة) على مرحلتَيْن. ومن موسم الختان في شەري تموز/يوليو وآب/أغسطس 2004، أُجريت لقاءات مع 1007 من الذكور بعد انقضاء 30 – 89 يوماً على الختان. وأُجريت ملاحظة مباشرة لأربعة وعشرين رجلاً أثناء وبعد
الختان بـ 3، و8، و30، و90 يوماً. كما أُجريت اختبارات سريرية لنحو 298 رجلاً بعد الختان بما يتـراوح بين 45 و89 يوماً. وأُجريت لقاءات مع 21 ممارساً للطب الشعبي و20 ممارساً للطب السريري لتقيـيم خبراتەم ومستوى تدريبەم. وأُجري جرد للمرافق الصحية لتقيـيم حالة الإمدادات والمعدات اللازمة لإجراء الختان المأمون.
الموجودات
وُجد أن من بين 443 ذكراً أجروا ختاناً تقليدياً، تعرَّض 156 (35.2%) لأحداث ضائرة، بالمقارنة بتعرُّض 99 من 559 (17.7%) أجروا ختاناً سريرياً لأحداث ضائرة (نسبة الأرجحية: 2.53؛ بفاصل ثقة 95% إذْ تـراوحت نسبة الأرجحية بين 1.89 و3.38). وثبت أن العدوى والنزف ەما أكثر الآثار الضائرة شيوعاً، كما لوحظ وجود ألم مفرط، وتەتك، ولوي، وخلل النعوظ وتـراوحت أعمار المشاركين بين 5 و21 عاماً، وكان نصفەم ناشطين جنسياً قبل الختان. ويفتقر الممارسون إلى التدريب والمعارف اللازمين، كما تفتقر معظم المرافق الصحية إلى المعدات والإمدادات الملائمة.
الاستنتاج
ينبغي توفير التدريب والموارد المكثفة في الأماكن الواقعة جنوب الصحراء الأفريقية قبل التـرويج العنيف لفعالية ختان الذكور في الوقاية من فيروس الإيدز. فثلثا الرجال الأفارقة. يتم ختانەم في الغالب من قِبَل ممارسين للطب الشعبي أو غير مؤەلين وفي أماكن غير رسمية. ومن ثـَمَّ يجب ألا نتجاەل مأمونية الختان في المجتمعات التي يُمارس فيەا الختان بالفعل على نطاق واسع.
Introduction
Over 35 observational studies and three randomized controlled trials from sub-Saharan Africa have shown that male circumcision reduces the risk of HIV incidence by approximately 60%.1–5 The biological mechanism for reduction in HIV infections in circumcised men is thought primarily to be through reduction of HIV target cells (e.g. Langerhans’ cells, CD+ T-cells and macrophages), which are plentiful on the inner, mucosal surface of the foreskin and through formation of a thick layer of squamous epithelial cells that form a barrier to HIV uptake in the underlying target cells.6–8 One model of the potential impact of circumcision interventions in sub-Saharan Africa has estimated that 5.7 million new infections could be averted over 20 years9 and another has shown that, with just 50% uptake over 10 years, the HIV prevalence in men in Nyanza Province, Kenya, would decline from 18% to 8%.10 Gray et al. have shown provision of male circumcision services could drive the reproductive rate of the epidemic to below replacement.5 Male circumcision interventions in high HIV prevalence areas would be at least as cost-effective as any of the other evidence-based HIV prevention tools currently available.10,11
A joint statement by WHO and the Joint United Nations Programme on HIV/AIDS (UNAIDS) recommended that “countries with high prevalence, generalized heterosexual HIV epidemics that currently have low rates of male circumcision consider urgently scaling up access to male circumcision services”.12 In view of the compelling evidence supporting male circumcision as an effective HIV prevention measure, as well as the declaration of the international health agencies and the support of governments and donor agencies, male circumcision services are now being introduced in selected populations in sub-Saharan Africa and further male circumcision interventions are being planned. A serious concern, however, is whether male circumcision can be provided to large numbers of adult males safely. While the beneficial effects of male circumcision are now widely recognized, those benefits must be weighed against the potential harms.
Male circumcision is a relatively simple, quick and safe procedure when performed in a clinical setting under aseptic conditions by a trained practitioner with proper instrumentation. However such conditions do not always prevail. There are few reliable data on complication rates from male circumcision in clinical settings in developing countries. The data that do exist suggest that circumcisions done at infancy or during childhood result in fewer adverse events. In Jamaica, 205 neonates were circumcised using the Plastibell device and complications were recorded in 2.4% of cases.13 In the United Republic of Tanzania, the rate of complications using the Plastibell was 2.0%.14 In Nigeria just five of 1563 (0.3%) circumcisions resulted in complications,15 and in the Comoros there were seven cases of haemorrhage and 18 cases of infection (2.4%) among 1019 boys circumcised at ages 3–8 years.16 However, a study of 270 neonates in Nigeria found two amputations of the glans penis and reported an overall complication rate of 20.2%.17 Reported rates of adverse events in adolescents and adults tend to be higher than in infants. In Turkey, the complication rate was 3.8% among 600 boys.18 A study of 249 consecutive circumcisions of adolescents and young adults in three major hospitals in Kenya and Nigeria found 28 (11.2%) complications, predominantly wound infection (2.8%) but also severe haemorrhage (1.2%), retention of urine (1.2%) and swelling (1.2%).19 That circumcision can be performed safely on young adults in clinical settings in Africa has been shown in Kisumu, Kenya, and in Orange Farm, South Africa, where the rates of adverse events were 1.7% and 3.6%, respectively, and most of these were mild.3,20 However, these were in the highly monitored and well-equipped contexts of clinical trials.
Accounts of serious complications from circumcisions performed in traditional settings in Africa are legend. For example, according to an article in a South African newspaper, there were more than 250 deaths following ritual circumcision between 1995 and 2003.21 Numerous other accounts of complications from traditional circumcision are available, but the rate of adverse events cannot be calculated because none of the reports include a denominator.22–24 In traditional circumcisions, one blade may be used for several initiates, leading to speculation that cases of sepsis and HIV transmissions occur.22,25 Additional complications also arise as a consequence of practices associated with traditional circumcision rituals. For example, deaths or serious complications have resulted from dehydration and exposure to cold or heat as boys are kept in outdoor camps sometimes for weeks after the surgery.21,22
Prior to implementing male circumcision as a public health measure against the spread of HIV, the feasibility, safety and costs of the procedure within target countries should be evaluated to understand what measures need to be taken to ensure access to safe, affordable voluntary circumcision services. The aims of this study were to assess variation and safety of male circumcision practices, as well as resource and training needs related to the procedure, in a community that has been practising circumcision traditionally for many generations. While traditional circumcision is the norm in the study community, many parents and young men are turning to medicalized circumcision. These circumstances provided the ideal opportunity to assess both traditional and medicalized circumcision practices and outcomes.
Methods
This prospective study was conducted in the Bungoma district, Western Province, Kenya. The residents of Bungoma district number approximately 997 000 and belong predominantly to the Bukusu ethnic group, which has practised male circumcision (but not female circumcision) for as long as there are historical records. Male circumcision is virtually universal and obligatory with most young Bukusu men undergoing the procedure in their village by a traditional surgeon, but increasingly families are turning to “western-style” medical practitioners for reasons of cost, healing in time for school, reduction of infections and modernization, among others.24
Sampling adverse events in young men
Participants for this study were recruited by a two-stage cluster sampling method. Two of the seven divisions inhabited primarily by Babukusu were selected randomly and, within those two divisions, 75 households were chosen randomly within each of the 15 total locations (the administrative unit loosely corresponding to a village) in the two divisions. The average number of households in a location was 315 (range: 313–429). Each household was assigned a sequential number and 75 numbers were chosen using a random numbers table. The aim was to achieve an initial sample of 1125 subjects to achieve a sample size of approximately 1000 young men undergoing circumcision that season. In April–June 2004, male and female research assistants speaking either the Bukusu dialect of Luluyia, English or Kiswahili enquired at each household if there was a boy present who would be circumcised during the July–August 2004 circumcision season. All boys who indicated that they were scheduled to be circumcised that season were eligible for inclusion in this study. A total of 1103 boys residing in the 1125 households were identified; of these 1099 were recontacted by end of August, and of those 1007 (91.6%) were circumcised. All were interviewed after the circumcision procedure to determine reported complication rates and levels of satisfaction with the procedure. All participants were asked questions regarding demographics, the date and nature of the procedure, their satisfaction, reported complications, knowledge of any peers who had experienced complications and sexual history before and after the circumcision.
For the purposes of this study, circumcisions performed in a hospital, health centre, dispensary or private office by anyone considered by the participant to be a clinician or “daktari” were categorized as “medical circumcisions”. All others were performed in villages or within household compounds and were categorized as “traditional”.
The first 24 circumcision procedures identified (12 traditional and 12 medicalized) were directly observed. These direct observations provided information about the methods used, the amount of bleeding and apparent pain involved, various adverse events, the instruments used, the suturing technique, if applicable, the bandaging used, and the condition of the subject. Each of these participants was then visited approximately 3, 8 and 30 days post-procedure and those observed to have a complication were seen approximately 90 days post-operation to observe the final outcome. In nine cases in which the progress of the wound was a concern, the subject had another visit at approximately 12 days post-operation.
Adverse events were recorded based on the protocol used in the randomized controlled trial in Kisumu, Kenya.4,23 The type of anaesthesia used, if any, was recorded as was the type of suturing, if any; the type of dressing; whether the suture line was intact; presence or absence of a haematoma; current pain or discomfort on a seven point scale; present level of bleeding, if any; presence of infection (none or erythema < 1 cm, erythema > 1 cm at the incision line, purulent discharge, cellulites or wound necrosis), cosmetic outcome (e.g. torsion, unusual scarring); and history of erections since circumcision. The sensitivity of different points of the penis was tested using a thread lightly rubbed against the thigh (as a control) and the penis with the participant blinded.
Sampling practitioners
Forty-one circumcisers – 21 traditional and 20 clinical – were interviewed to assess their experience with the procedure, their level of training, their experience with dealing with complications, and the amount they charge for the procedure. Those interviewed were a convenience sample of men who had performed circumcisions during the August 2004 circumcision season. Traditional circumcisers were identified by village leaders and by young men who underwent circumcision. All the providers contacted consented to be interviewed. Interviews lasted approximately one hour and were conducted in Luluyia, Kiswahili or English, depending on the preference of the circumciser.
Inventories of health facilities
Inventories of three hospitals, one health centre and 14 private clinics were taken to assess the presence and condition of the instruments and supplies necessary for performing safe circumcisions. Only those instruments considered to be in working order were included in the inventories. Twenty traditional circumcisers, identified by parents and by boys who underwent the procedure, were also asked to show the instruments and supplies they had on hand to perform circumcisions.
Data analysis
Data from the 1007 interviews were entered into a Microsoft ACCESS database (Microsoft Corporation, Seattle, WA, United States of America) and converted to SPSS (SPSS Inc., Chicago, IL, USA). Descriptive summaries of sociodemographic characteristics and adverse events were based on frequencies and proportions. Associations between these variables and method of circumcision are summarized using odds ratios adjusted using logistic regression for age, rural versus urban residence, and number of days since circumcision. The study protocol was approved by the Moi University Institutional Research and Ethics Committee.
Results
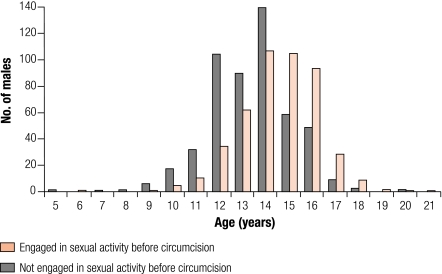
Of the 1099 boys contacted by the end of the circumcision season (late August), 1007 had undergone circumcision. Table 1 shows the results from the interviews of 445 young men circumcised traditionally and 562 circumcised medically. Interviews were held a mean of 60 days (range: 30–89) post-circumcision. Those circumcised medically were younger and were less likely to reside in a rural area. There was no difference in education level between the two groups. Those circumcised traditionally were 2.53 times more likely to report an adverse event than those circumcised medically. The proportion of males circumcised traditionally and reporting adverse events was a shocking 35.2%. The adverse-event rate among those circumcised medically was significantly lower (17.7%) but nevertheless very high compared with rates observed in developed countries and in clinical settings in Kenya and Nigeria.25 The median age at sexual debut was between 14 and 15 years (Fig. 1). Approximately half the young men were sexually active before they were circumcised, more in those circumcised traditionally (63.1%) than those circumcised medically (35.5%).
Table 1. Differences between males circumcised traditionally versus medically, July–August 2004, in Bungoma district, Kenya.
| Characteristics | Traditional |
Medical |
OR | 95% CI | P-value | |||
|---|---|---|---|---|---|---|---|---|
| (n) | (%) | (n) | (%) | |||||
| Age | ||||||||
| ≤ 15 | 291 | 66.3 | 506 | 90.4 | 0.21 | 0.15–0.30 | < 0.001 | |
| ≥ 16 | 148 | 33.7 | 54 | 9.6 | ||||
| Residence | ||||||||
| Rural | 388 | 87.2 | 430 | 76.5 | 2.08 | 1.49–2.94 | < 0.001 | |
| Urban | 57 | 12.8 | 132 | 23.5 | ||||
| Schooling | ||||||||
| Primary | 442 | 99.3 | 554 | 98.9 | 1.59 | 0.40–6.25 | 0.510 | |
| Secondary | 3 | 0.7 | 6 | 1.1 | ||||
| Complications | ||||||||
| Yes | 156 | 35.2 | 99 | 17.7 | 2.53 | 1.89–3.38 | < 0.001 | |
| No | 287 | 64.8 | 460 | 82.3 | ||||
| Fully healed | ||||||||
| Yes | 299 | 75.9 | 397 | 81.2 | 0.73 | 0.53–1.01 | 0.056 | |
| No | 95 | 24.1 | 92 | 18.8 | ||||
| Sought care at hospital | ||||||||
| Yes | 59 | 23.1 | 83 | 31.1 | 0.67 | 0.45–0.99 | 0.042 | |
| No | 196 | 76.9 | 184 | 68.9 | ||||
| Pain with erection | ||||||||
| Yes | 90 | 20.9 | 103 | 19.3 | 1.10 | 0.80–1.51 | 0.548 | |
| No | 341 | 79.1 | 430 | 80.7 | ||||
| Had sex before circumcision | ||||||||
| Yes | 280 | 63.1 | 199 | 35.5 | 3.11 | 2.40–4.02 | 0.001 | |
| No | 164 | 36.9 | 362 | 64.5 | ||||
| Had sex since circumcision | ||||||||
| Yes | 28 | 6.3 | 17 | 3.0 | 2.16 | 1.17–4.00 | 0.014 | |
| No | 413 | 93.7 | 542 | 97.0 | ||||
| Would choose different method | ||||||||
| Yes | 70 | 15.9 | 80 | 14.4 | 1.13 | 0.79–1.59 | 0.507 | |
| No | 371 | 84.1 | 477 | 85.6 | ||||
CI, confidence interval; OR, odds ratio.
Fig. 1.
The age of 1007 males who had engaged or not engaged in sexual activity before being circumciseda
a Median age at first intercourse was 14 years.
The subjects were asked to describe any adverse events that they experienced. The most common complications reported were excessive bleeding, infections and excessive pain, with bleeding the most common. Other common adverse events reported were pain upon urination, incomplete circumcision requiring recircumcision, and lacerations of the glans, the scrotum and the thighs. Many boys who were circumcised traditionally reported that they were unable to stop the bleeding after the procedure, and a parent either took them to hospital or, more frequently, called a health professional or “travelling nurse” to come to the compound to arrest the bleeding and provide bandaging. Infections were equally common among subjects circumcised medically and traditionally, although those circumcised traditionally were less likely to go to a health facility for post-operative care (odds ratio, OR: 0.67; 95% confidence interval, CI: 0.45–0.99). Those circumcised traditionally were more likely to report receiving antibiotics from local practitioners, some of whom are qualified clinical officers or nurses, but many of whom are “travelling nurses” with few or no qualifications. These informal practitioners often sold injections to address infections and bandaged the wound after applying gravacine (a talcum powder with penicillin). Whether it prevented infections we cannot be sure, but it tended to cake in the wound, delay healing and result in thick scarring and, in a few cases, permanent discolouration.
In 24% of the traditional cases and 19% of the medical cases, the wound had still not healed when participants were observed at 60 days after the operation. This was borderline significantly different (P = 0.056) and is in sharp contrast to the randomized control trial of male circumcision in Kisumu, Kenya, in which all but 64 (4%) of the subjects were fully healed by their 30 day post-operative visit.23 Since many of these young men are sexually active, such a long period for healing could expose them to elevated risk for HIV infection through an open wound. For example, 4.5% of the young men had already engaged in sex since their procedure – twice as many circumcised traditionally (6.3%) as those circumcised medically (3.0%) (adjusted OR: 2.16; 95% CI: 1.17–4.00).
Twenty-four circumcisions – 12 medical and 12 traditional – were observed directly. The mean age of boys circumcised medically was 13.6 years; those circumcised traditionally were slightly older, averaging 14.6 years. The outcomes of the procedures can be found in Table 2. Only one of 12 medical procedures and two of 12 traditional procedures resulted in no complications. The adverse events recorded ranged in severity from mild (e.g. mild infection or wound disruption) to very serious or life-threatening. Surprisingly, medical circumcisions did not result in appreciably fewer adverse events than traditional ones, and the severity of the adverse events was about the same for both methods.
Table 2. Practices and adverse events directly observed from medical and traditional circumcisions performed in Bungoma district, Kenya, July–August, 2004.
| Description of event | Medical
(N = 12) |
Traditional
(N = 12) |
|||
|---|---|---|---|---|---|
| (n) | (%) | (n) | (%) | ||
| Use of general anaesthesia | 2 | 17 | 0 | 0 | |
| Use of local anaesthesia | 10 | 83 | 0 | 0 | |
| Sutures used | 9 | 75 | 0 | 0 | |
| Sutures widely spaced with oedema | 5 | 56 | n/a | n/a | |
| Sutures broken | 5 | 56 | n/a | n/a | |
| Infection requiring antibiotics | 6 | 50 | 5 | 42 | |
| Wound not healed at 30 days | 12 | 100 | 12 | 100 | |
| Torsion | 2 | 17 | 0 | 0 | |
| Profuse bleeding requiring IV fluids | 1 | 8 | 0 | 0 | |
| Incomplete foreskin removed | 2 | 17 | 5 | 42 | |
| Required recircumcision | 2 | 17 | 4 | 33 | |
| Wound > 3 cm corona to cut line | 3 | 25 | 4 | 33 | |
| Jagged cut line/skin not uniform | 2 | 17 | 3 | 25 | |
| Haematoma requiring surgery | 1 | 8 | 0 | 0 | |
| No sensitivity corona to cut line | 4 | 33 | 3 | 25 | |
| Loss of erectile function at 3 months | 0 | 0 | 3 | 25 | |
| Required hospitalization | 1 | 8 | 0 | 0 | |
| Permanent adverse sequelaea | 3 | 25 | 4 | 33 | |
| No adverse event | 1 | 8 | 2 | 16 | |
n/a, not applicable. a Any event directly related to circumcision that results in a disability likely to last for years or a lifetime, including torsion, mutilation of the glans, excessive scarring causing loss of penile sensitivity, and erectile dysfunction.
After conducting the interviews with approximately two-thirds of the subjects and after directly following 24 cases, it was apparent that complications were occurring at very high rates. However, it was unknown whether the subjects were providing accurate reports of the adverse events nor could it be assessed whether the reported adverse events resulted in permanent sequelae. Therefore the remaining 298 of the 1007 consenting subjects who had not yet been interviewed were directly examined and interviewed two months (range: 45–89 days) after the procedure. The results of the observations are shown in Table 3.
Table 3. Results of penile examinations of 298 males circumcised by traditional and medical practitioners in Bungoma district, Kenya, 45–89 days post circumcision.
| Results | Traditional |
Medical |
Adjusted ORa | 95% CI | P-value | |||
|---|---|---|---|---|---|---|---|---|
| (n) | (%) | (n) | (%) | |||||
| Fully healed | ||||||||
| Yes | 136 | 78.6 | 112 | 89.6 | 0.43 | 0.22–0.84 | 0.014 | |
| No | 37 | 21.4 | 13 | 10.4 | ||||
| Crust still present | ||||||||
| Yes | 20 | 11.6 | 8 | 6.4 | 1.91 | 0.81–4.49 | 0.137 | |
| No | 153 | 88.4 | 117 | 93.6 | ||||
| Wound still open | ||||||||
| Yes | 3 | 1.7 | 2 | 1.6 | 1.09 | 0.18–6.59 | 0.929 | |
| No | 170 | 98.3 | 123 | 98.4 | ||||
| Excessive foreskin remaining | ||||||||
| Yes | 20 | 11.6 | 3 | 2.4 | 5.32 | 1.54–18.31 | 0.008 | |
| No | 153 | 88.4 | 122 | 97.6 | ||||
| Signs of infection | ||||||||
| Yes | 0 | 0 | 1 | 0.8 | – | – | – | |
| No | 173 | 100 | 124 | 99.2 | ||||
| Swelling | ||||||||
| Yes | 24 | 13.9 | 6 | 4.8 | 3.20 | 1.27–8.07 | 0.014 | |
| No | 149 | 86.1 | 119 | 95.2 | ||||
| Lacerations | ||||||||
| Yes | 29 | 16.9 | 12 | 9.6 | 1.91 | 0.93–3.91 | 0.077 | |
| No | 143 | 83.1 | 113 | 90.4 | ||||
| Keloid scarring | ||||||||
| Yes | 30 | 17.4 | 12 | 9.6 | 1.99 | 0.98–4.06 | 0.059 | |
| No | 142 | 82.6 | 113 | 90.4 | ||||
CI, confidence interval; OR, odds ratio. a Odds ratios are adjusted for age, rural versus urban residence, and number of days since circumcision.
The data from the direct observations were consistent with the reports from the subjects themselves. Those in the group who were traditionally circumcised were much more likely not to have healed, to have significant swelling, to have lacerations and keloid scarring, and to have a culturally unacceptable amount of foreskin remaining. Nevertheless, compared to developed country settings, delayed healing, swellings and lacerations were also prevalent among those circumcised medically.
Interviews with circumcisers
The level of education of the medical practitioners was 15.4 years whereas that of the traditional circumcisers was 6.8 years. The traditional circumcisers had performed more circumcisions over the previous 2 years than medical circumcisers. None of the traditional circumcisers (versus three of the medical circumcisers) had performed fewer than 10 circumcisions, while 9 (versus 5) had performed more than 100. When practitioners were asked if they felt that they were adequately trained to perform circumcisions, only one – a medical practitioner working as a nurse in a government health facility – responded “no”. Nevertheless, when we asked if they would like further training, about half in each group felt that they could profit from additional training. Several traditional circumcisers in particular stated that they would like more information on penile anatomy, with attention to where nerves and arteries are located, and they desired training on how to best arrest bleeding.
Cost of circumcision
The average cost charged by a traditional practitioner was about 345 Kenyan shillings (KS), ranging between 100 and 500 (70 KS/$1 US). Additional charges may include chicken, sheep, food and medical dressings. Medical practitioners charged a mean of 564 KS with a range of 350–2000 KS. Antibiotics, dressing, tetanus shots and added visits may have resulted in additional costs. Thus, the cost of the procedure at the hands of a traditional circumciser is less than if done by a medical practitioner. However, the amount charged by the practitioner for the procedure may not reflect the ultimate cost by the time the wound is fully healed. If there is a complication, which as we have seen there is in 25% of cases, then the cost may be significantly higher. Since there are twice as many complications arising from traditional circumcisions, the total cost to the family is likely to be higher in these cases than in cases done by medical practitioners. Moreover, it is important to emphasize that, with traditional circumcision, the charges for the procedure and any ensuing treatment are often a small part of the total cost to the family. As a traditional rite of passage, circumcision is an event that entails costly celebrations and rituals. The total cost varies but may reach into the tens of thousands of shillings.24 A circumcision performed by a clinician, on the other hand, may be a one-time procedure costing 350–2000 KS.
The adverse-event rates from procedures done in the private facilities (22.5%) were twice the rates in the public facilities (11%). Although practitioners in public facilities have nursing or more advanced qualifications, these rates are unacceptable and indicate that practitioners require further training.
The results from inventories of circumcision instruments and supplies indicate that both public and private health facilities lack some of the essential items for performance of safe circumcisions. The public health facilities, which included the district hospital and three health centres, were fairly well provisioned with the exception of autoclaves and proper sutures. On the other hand, private facilities were less well equipped. Fifty per cent of the public health centres had working autoclaves compared to 21% of the private facilities. Some facilities used pressure cookers or boiling, instead of autoclaves, to sterilize the equipment. Approximately half of the private and public facilities did not have sutures available. This sometimes resulted in circumcision performed without stitching: this was seen in four of the 12 medical cases that were observed directly. Others may have used the larger suture material, which tends to result in ruptures and crimping of tissue causing unnecessary swellings.
Discussion
This study found that the prevalence of adverse events from traditional and medical circumcisions in Bungoma district, Kenya, is an order of magnitude higher than clinical circumcisions performed on infants in developed countries and much higher than previously reported from African medical settings.14,19 The overall rate of adverse events was approximately 25%, with 35% of those circumcised traditionally experiencing at least one complication and 18% of those circumcised medically experiencing an adverse event. This is compared to a rate of 1.7% complications in the clinical setting of a randomized controlled trial of male circumcision in Kisumu, Kenya,20 and a 3.8% rate in the setting of private practitioners performing circumcisions for participants in the randomized control trial of male circumcision in Orange Farm, South Africa.3 While most of the adverse events we observed were resolved by 90 days post-operation, an unacceptable proportion did not, and the long periods of healing, inactivity and additional costs to families imposed unnecessary suffering and financial costs on young men and their families. Moreover, we estimate that approximately 6% of procedures resulted in permanent adverse sequelae. This study was conducted during and immediately after the 2004 circumcision season and conditions have not changed remarkably since that time (Egesah, personal observation).
High rates of complications impose costs on boys, parents, health facilities and civil society. The long periods necessary for proper healing take time away from school or from productive activities, such as helping in food production. The burden to parents and relatives for additional medical attention in this mostly rural, high-poverty district can be financially crippling. The necessity for health facilities to address complications during the prolonged circumcision season diverts scarce resources from other essential services.
Despite having gone through it themselves, there appeared to be a lack of knowledge on the part of fathers and older men about wound care or detection of complications. The prevailing approach to complications seemed to be to wait and see and hope for the best. This is likely in part because boys are expected to have difficulties just as the older men experienced difficulties themselves. Education of parents, guardians and the initiates themselves as to proper post-operative wound care and recognition of when medical assistance should be sought could reduce the frequency and severity of adverse events significantly.
Approximately half the young men in this study were sexually active before they were circumcised at the median age of 16 years. In communities such as Bungoma where circumcision is widely practised, educational programmes might be developed to encourage parents and young men to seek circumcision at earlier ages, before onset of sexual activity. This may avert more HIV infections and have the added advantage of reducing adverse events. However, male circumcision before the age of 18 requires guardian consent and informed assent on the part of the minor.
It became clear from both the observations of the circumcision outcomes and the interviews with medical and traditional practitioners that further training of practitioners in medical settings is required. Only medical officers have formal in-theatre supervised training in surgical circumcision. Clinical officers may observe circumcisions in training college but seldom actually perform the procedure under supervision, and nurses get no formal instruction in male circumcision. As circumcision becomes widely promoted for HIV prevention and general health, the demand for safe clinical services will become more widespread. Routine formal training in proper circumcision techniques should be integrated into the curricula of training colleges and made part of the required supervised practica for clinical officers and nurses. Roughly half of the medical practitioners whom we interviewed expressed a need for further training. Training should include pre-operative assessment, assessment of instruments, supplies and facilities, sterilization techniques, patient informed consent, proper patient preparation, surgical procedures, pain management, post-operative care, counselling about wound care, recognition and treatment of adverse events, and referral to tertiary centres. Male circumcision should not be considered a stand-alone medical procedure for HIV prevention, but rather be incorporated into a full complement of HIV prevention and reproductive health services, including, but not limited to, counselling about safe sex, diagnosis and treatment of sexually transmitted infections, HIV testing, and referral to HIV treatment and care. Therefore, training should include education about these additional HIV prevention methods. Consideration should be given to a certification process for practitioners who undergo approved training programmes. This might undermine the ability of unqualified practitioners to set up makeshift clinics and attract unsuspecting clients to low-quality services. Certification could include a requirement to provide services within an affordable range, and the public could be informed about which clinics and providers have been certified.
Even the best trained and most experienced clinician will have difficulty in keeping adverse events to a minimum if they do not have the correct surgical instruments or expendable supplies at hand. Many of the adverse events we observed were attributable to lack of instruments in good working order or to use of the wrong suture material. For example, the high frequency of jagged wound edges and of residual foreskin was due to dull scissors or lack of scalpel. Frequent infections may have been caused by lack of functional sterilization equipment. Poor post-operative wound care was in many cases due to insufficient fresh dressing material. If a practitioner is doing many circumcisions in a day and does not have several sets of instruments or adequate sterilization equipment, he or she may be using the same instruments on several patients. This is a widespread concern among parents and boys regarding the practices of traditional circumcisers, but it is also relevant to medical practitioners with limited resources. The higher adverse-event rates in private clinics (22.5%) versus in public, governmental clinics (11%) are likely due to the better instrumentation and consumable supplies available to those in public hospitals and health centres.
Because medical practitioners compete for clients in part on the basis of the fees they charge, the costs of the surgical instruments and expendable supplies are a significant concern. Private practitioners especially may be less likely to have instruments in working order, because the cost of replacement is beyond their means. They may not tie all the bleeders or may space the stitches widely because using an additional packet of suture material would push the cost of the procedure beyond what they can charge the patient. Practitioners are at risk of compromising safety and quality of service in the interests of keeping their costs down. The quality and safety of services might be improved by providing practitioners with up-to-date instruments and sufficient expendable supplies. An alternative approach could be to supplement the cost, perhaps by distributing through pharmacies and vendors at-cost kits containing essential expendables (e.g. antiseptic, suture, suture needle, disposable syringe, lidocaine, vaseline gauze, and bandages). Improving the quality and lowering the costs of male circumcision services could not only avert complications but also reduce healing times and thus reduce risk of HIV infection in those who resume sexual activity soon after circumcision.
There are several limitations to our study. Only 24 of the 1007 circumcisions were directly observed, making it difficult to attribute reported adverse events to specific causes. However, the lead investigators and the project clinical officer had observed or performed hundreds of procedures outside this study and they were thoroughly familiar with the etiology of various adverse outcomes. A sub-sample of 298 of the 1007 participants (30%) underwent penile examinations in conjunction with their interviews. The true adverse-event rates may have been higher in the absence of our study, since the research team could not observe complications without intervening to assist the participant. Interventions included redressing the wound in about 20 cases, giving a course of antibiotic (two cases) and taking a participant to the district hospital. We believe that this later case would very likely have died without our intervention.
Much attention is now focused on making safe, affordable male circumcision services available for HIV prevention in areas with high HIV seroprevalence and low male circumcision prevalence.12 The results of this study reinforce the observations that extensive training and resources will be necessary to build the capacity of health facilities in sub-Saharan Africa before safe circumcision services can be aggressively promoted for HIV prevention. However, our results showing 35% of traditional circumcisions resulting in adverse events, many of them serious and permanent, should also serve as an alarm to ministries of health and the international health community that focus cannot only be on areas where circumcision prevalence is low. Roughly two-thirds of males in Africa are circumcised, the majority by traditional circumcisers or practitioners in the informal sector.26 The levels of morbidity and mortality from circumcisions documented as occurring in this study community are unacceptable. Studies such as this are needed in additional communities. However, there is sufficient anecdotal evidence to indicate that Bungoma is not unique, especially in east and southern Africa where male circumcision is performed predominantly on adolescents and young adults unlike in west Africa where most boys are circumcised as infants.17,21,27 As the international public health community focuses attention and resources on providing male circumcision services in high HIV prevalence, low male circumcision prevalence communities, it must address the safety of circumcisions in populations where it is already widely practised. If the practices in these communities continue to be largely ignored, the gains to be achieved by promotion and provision of circumcision for HIV prevention may well be undermined by further accounts of unnecessary suffering and morbidity occurring in circumcising communities. ■
Footnotes
Funding: Support was provided by the Global Bureau of Health/HIV-AIDS, US Agency for International Development (USAID) and the AIDSMark Project of PSI.
Competing interests: None declared.
References
- 1.Bailey RC, Plummer FA, Moses S. Male circumcision and HIV prevention: current knowledge and future research directions. Lancet Infect Dis. 2001;1:223–31. doi: 10.1016/S1473-3099(01)00117-7. [DOI] [PubMed] [Google Scholar]
- 2.Weiss HA, Quigley MA, Hayes RJ. Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis. AIDS. 2000;14:2361–70. doi: 10.1097/00002030-200010200-00018. [DOI] [PubMed] [Google Scholar]
- 3.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 5.Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised controlled trial. Lancet. 2007;369:657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 6.Patterson BK, Landay A, Siegel JN, Flener Z, Pessis D, Chaviano A, et al. Susceptibility to humanimmunodeficiency virus-1 infection of human foreskin and cervical tissue grown in explant culture. Am J Pathol. 2002;161:867–73. doi: 10.1016/S0002-9440(10)64247-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCoombe SG, Short RV. Potential HIV-1 target cells in the human penis. AIDS. 2006;20:1491–5. doi: 10.1097/01.aids.0000237364.11123.98. [DOI] [PubMed] [Google Scholar]
- 8.Donoval BA, Landay AL, Moses S, Agot K, Ndinya-Achola JO, Nyagaya EA, et al. HIV-1 target cells in foreskins of African men with varying histories of sexually transmitted infections. Am J Clin Pathol. 2006;125:386–91. [PubMed] [Google Scholar]
- 9.Williams BG, Lloyd-Smith JO, Gouws E, Hankins C, Getz WM, Hargrove J, et al. The potential impact of male circumcision on HIV in Sub-Saharan Africa. PLoS Med. 2006;3:e262. doi: 10.1371/journal.pmed.0030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nagelkerke NJ, Moses S, de Vlas SJ, Bailey RC. Modelling the public health impact of male circumcision for HIV prevention in high prevalence areas in Africa. BMC Infect Dis. 2007;7:16. doi: 10.1186/1471-2334-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahn JG, Marseille E, Auvert B. Cost-effectiveness of male circumcision for HIV prevention in a South African setting. PLoS Med. 2006;3:e517. doi: 10.1371/journal.pmed.0030517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO and UNAIDS announce recommendations from expert meeting on male circumcision for HIV prevention UNAIDS & WHO; 2007. Available from: http://data.unaids.org/pub/PressRelease/2007/20070328_pr_mc_recommendations_en.pdf [accessed on 24 July 2008].
- 13.Duncan ND, Dundas SE, Brown B, Pinnock-Ramsaran C, Badal G. Newborn circumcision using the Plastibell device: an audit of practice. West Indian Med J. 2004;53:23–6. [PubMed] [Google Scholar]
- 14.Manji KP. Circumcision of the young infant in a developing country using the Plastibell. Ann Trop Paediatr. 2000;20:101–4. doi: 10.1080/02724936.2000.11748116. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed A, Mbibi NH, Dawam D, Kalayi GD. Complications of traditional male circumcision. Ann Trop Paediatr. 1999;19:113–7. doi: 10.1080/02724939992743. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed A. Circumcision practice in Anjouan. Trop Doct. 2000;30:52–3. doi: 10.1177/004947550003000130. [DOI] [PubMed] [Google Scholar]
- 17.Okeke LI, Asinobi AA, Ikuerowo OS. Epidemiology of complications of male circumcision in Ibadan, Nigeria. BMC Urol. 2006;60:21. doi: 10.1186/1471-2490-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozdemir E. Significantly increased complication risks with mass circumcision. BJU Int. 1997;80:136–9. doi: 10.1046/j.1464-410X.1997.00218.x. [DOI] [PubMed] [Google Scholar]
- 19.Magoha GA. Circumcision in various Nigerian and Kenyan hospitals. East Afr Med J. 1999;76:583–6. [PubMed] [Google Scholar]
- 20.Mayatula V, Mavundla TR. A review on male circumcision procedures among South African blacks. Curationis. 1997;20:16–20. [PubMed] [Google Scholar]
- 21.Crowley IP, Kesner KM. Ritual circumcision (Umkhwetha) amongst the Xhosa of the Ciskei. Br J Urol. 1990;66:318–21. doi: 10.1111/j.1464-410x.1990.tb14936.x. [DOI] [PubMed] [Google Scholar]
- 22.Myers RA, Omorodion FI, Isenalumhe AE, Akenzua GI. Circumcision: its nature and practice among some ethnic groups in southern Nigeria. Soc Sci Med. 1985;21:581–8. doi: 10.1016/0277-9536(85)90043-7. [DOI] [PubMed] [Google Scholar]
- 23.Naude JH. Reconstructive urology in the tropical and developing world: a personal perspective. BJU Int. 2002;89(Suppl 1):31–6. doi: 10.1046/j.1465-5101.2001.naude.136.x. [DOI] [PubMed] [Google Scholar]
- 24.Krieger JN, Bailey RC, Opeya JC, Ayieko BO, Opiyo FA, Agot K, et al. Adult male circumcision: results of a standardized procedure in Kisumu District, Kenya. BJU Int. 2005;96:1109–13. doi: 10.1111/j.1464-410X.2005.05810.x. [DOI] [PubMed] [Google Scholar]
- 25.Egesah O. Male circumcision among the Bukusu in Bungoma, Kenya: culture, religion and economics [dissertation]. Eldoret: Moi University; 2008. [Google Scholar]
- 26.Male circumcision: global trends and determinants of prevalence, safety and acceptability WHO and UNAIDS; 2007 Available from: http://www.who.int/hiv/pub/malecircumcision/globaltrends/en/index.html [accessed on 12 August 2008].
- 27.Sidley P. Botched circumcisions lead to arrest for murder. BMJ. 1996;313:647. doi: 10.1136/bmj.313.7058.647a. [DOI] [PubMed] [Google Scholar]