Abstract
In 2005, the Member States of WHO adopted a resolution encouraging countries to develop health financing systems capable of achieving and/or maintaining universal coverage of health services – where all people have access to needed health services without the risk of severe financial consequences. In doing this, a major challenge for many countries will be to move away from out-of-pocket payments, which are often used as an important source of fund collection. Prepayment methods will need to be developed or expanded but, in addition to questions of revenue collection, specific attention will also have to be paid to pooling funds to spread risks and to enable their efficient and equitable use. Developing prepayment mechanisms may take time, depending on countries’ economic, social and political contexts. Specific rules for health financing policy will need to be developed and implementing organizations will need to be tailored to the level that countries can support and sustain. In this paper we propose a comprehensive framework focusing on health financing rules and organizations that can be used to support countries in developing their health financing systems in the search for universal coverage.
Résumé
En 2005, les Etats Membres de l’OMS ont adopté une résolution encourageant les pays à développer des systèmes de financement de la santé capables de mettre en place et/ou de maintenir une couverture universelle des services de santé permettant à toutes les personnes d’avoir accès aux services sanitaires dont elles ont besoin sans risquer des conséquences financières graves. Dans cette voie, l’une des difficultés majeures pour de nombreux pays réside dans l’abandon du système des débours directs par les ménages, qui sert fréquemment de source importante de financement. Il faut développer ou élargir des méthodes de prépaiement, tout en accordant une attention particulière non seulement aux questions de collecte des contributions, mais aussi à la mise en commun des fonds pour répartir les risques et permettre un usage efficace et équitable de ces fonds. La mise au point de mécanismes de prépaiement peut prendre du temps en fonction du contexte économique, social et politique qui règne dans les pays. Il faut aussi élaborer des règles spéciales pour les politiques de financement de la santé et adapter les organisations chargées de la mise en œuvre de ces politiques en fonction du niveau que les pays sont en mesure de supporter et de maintenir. Nous proposons dans cet article un cadre complet, régissant principalement les règles et les organisations de financement de la santé, utilisable pour aider les pays à développer des systèmes de financement de la santé orientés vers la réalisation de la couverture universelle.
Resumen
En 2005 los Estados Miembros de la OMS adoptaron una resolución en la que se alienta a los países a desarrollar sistemas de financiación sanitaria capaces de alcanzar o mantener la cobertura universal de servicios de salud: mecanismos para garantizar que toda la población tenga acceso a los servicios de salud necesarios sin arriesgarse a sufrir consecuencias financieras graves. En ese empeño, un reto importante para muchos países será el de renunciar a los pagos directos, empleados a menudo como una fuente importante de fondos. Habrá que desarrollar o expandir los métodos de prepago, pero, además de las cuestiones relativas a la recaudación de ingresos, se deberá prestar especial atención a la mancomunación de fondos para repartir los riesgos y utilizar dichos fondos de forma eficiente y equitativa. El desarrollo de mecanismos de prepago puede requerir tiempo, según el contexto económico, social y político de los países. Será necesario elaborar normas específicas para las políticas de financiación sanitaria y habrá que adaptar las organizaciones ejecutoras a niveles que los países puedan apoyar y mantener. En este artículo proponemos un marco integral centrado en las normas y organizaciones de financiación de la salud que pueden utilizarse para ayudar a los países a desarrollar sus sistemas de financiación sanitaria en pro de la cobertura universal.
ملخص
اعتمدت الدول الأعضاء في منظمة الصحة العالمية، عام 2005، قراراً يشجِّع البلدان على وضع نُظُم تمويل صحي تكون قادرة على تحقيق، أو الحفاظ على، تغطية شاملة بالخدمات الصحية بحيث يمكن لجميع السكان الوصول إلى الخدمات الصحية التي يحتاجونەا دون التعرُّض للمخاطر الناجمة عن العواقب المالية الوخيمة. ولدى عمل ذلك، سيمثِّل التحوُّل عن المدفوعات من جيوب المواطنين التي تستخدم عادة كمصدر مەم لجمع الأموال، واحداً من التحدِّيات الرئيسية وذلك للعديد من البلدان. وستكون ەناك حاجة لتطوير طرق الدفع المسبق أو توسيع نطاقە، إلا أنە، إلى جانب المسائل المتعلقة بجمع الإيرادات، سيكون من اللازم توجيە اەتمام خاص لتجميع الأموال، بغرض توزيع المخاطر، ولإمكان استخدام ەذە الإيرادات استخداماً يتسم بالكفاءة والإنصاف. وقد يستغرق وضع الآليات اللازمة للدفع المسبق بعض الوقت، وفقاً لظروف البلدان الاقتصادية والاجتماعية والسياسية. كما ستدعو الحاجة أيضاً إلى وضع قواعد محدَّدة لسياسات التمويل الصحي. وسيكون من اللازم كذلك تەيئة الجەات المنفذة وفقاً لمستوى الدعم الذي يمكن للبلدان تقديمە وضمان استمرارە. ويقترح الباحثون في ەذە الورقة وضع إطار شامل يركِّز على قواعد التمويل الصحي والەيئات التي يمكن استخدامەا لدعم البلدان في تطوير نظم التمويل الصحي لديەا، بحثاً عن التغطية الشاملة.
Introduction
Out-of-pocket payments create financial barriers that prevent millions of people each year from seeking and receiving needed health services1,2 In addition, many of those who do seek and pay for health services are confronted with financial catastrophe and impoverishment.3–5 People who do not use health services at all, or who suffer financial catastrophe are the extreme. Many others might forego only some services, or suffer less severe financial consequences imposed by user charges, but people everywhere, at all income levels, seek protection from the financial risks associated with ill health.
A question facing all countries is how their health financing systems can achieve or maintain universal coverage of health services. Recognizing this, in 2005 the Member States of WHO adopted a resolution encouraging countries to develop health financing systems aimed at providing universal coverage.6 This was defined as securing access for all to appropriate promotive, preventive, curative and rehabilitative services at an affordable cost. Thus, universal coverage incorporates two complementary dimensions in addition to financial risk protection: the extent of population coverage (e.g. who is covered) and the extent of health service coverage (e.g. what is covered).
In some countries it will take many years to achieve universal coverage according to the above-mentioned dimensions. This paper addresses a number of key questions that countries will need to address and considers how the responses can be tailored to the specific country context. In addition, it highlights the critical need to pay attention to the role of institutional arrangements and organizations in implementing universal coverage.
Shifting to prepayment
A first important observation is that many of the world’s 1.3 billion people on very low incomes still do not have access to effective and affordable drugs, surgeries and other interventions because of weaknesses in the health financing system.1
We investigated 116 recent household expenditure surveys from 89 countries, which allowed calculations of the consequences of paying for health services by those who do use them. Up to 13% of households face financial catastrophe in any given year because of the charges associated with using health services and up to 6% are pushed below the poverty line. Extrapolating the results globally suggests that around 44 million households suffer severe financial hardship and 25 million are pushed into poverty each year simply because they need to use, and pay for, health services.7 Households are considered to suffer financial catastrophe if they spend more than 40% of their disposable income – the income remaining after meeting basic food expenditure – on health services. They are often forced to reduce expenditure on other essential items such as housing, clothing and the education of children to pay for health services. Households are considered impoverished if health expenses push them below the poverty line.
Inability to access health services, catastrophic expenditure and impoverishment are strongly associated with the extent to which countries rely on out-of-pocket payments as a means of financing their health systems. These payments generally take the form of fees for services (levied by public and/or private sector providers), co-payments where insurance does not cover the full cost of care, or direct expenditure for self-treatment often for pharmaceuticals. A major challenge, therefore, to the achievement of universal coverage is finding ways to move away from out-of-pocket payments towards some form of prepayment. Solutions are complex, and countries’ economic, social and political contexts differ, moderating the nature and speed of development of prepayment mechanisms.8
Policy norms in health financing
Health financing policy, however, cannot afford to focus just on how to raise revenues.9 It requires concomitant attention to be focused on three health financing functions and related specific policy norms:10–13 (i) revenue collection, whereby financial contributions should be collected in sufficient quantities, equitably and efficiently; (ii) pooling of contributions so that costs of accessing health services are shared and not met only by individuals at the time they fall ill, thus ensuring financial accessibility; and (iii) purchasing and/or provision, with contributions being used to purchase or to provide appropriate and effective health interventions in the most efficient and equitable way. Efficiency includes considering the type of services to fund and who should provide them. In addition, and also anticipating the need for cost-containment measures, the identification of an appropriate mix of provider payment methods is warranted.
Active consideration of the policy norms discussed above should steer the development of a universal coverage policy. Some form of legislation or regulation is generally needed to consolidate these norms. For example, revenue collection legislation will usually specify the funds to be raised from taxes or from health insurance contributions, if any vulnerable population groups are exempt and whether contributions vary by income. In pooling, norms establishing the extent of solidarity are described showing who can benefit from the pooled funds and when. The definition of a detailed health services benefit package may be a response to the norm defined for purchasing, while ways of paying providers will usually require some form of legal agreement.
Key questions
Do political will and stewardship exist?
Before a reform towards universal coverage can be initiated, governments need to have the political will and the capacity to exercise good stewardship. Most will also need to consider the extent of diverse preferences within their society. An important case of stewardship is from the Republic of Korea, where it has been suggested that universal coverage implementation benefited from the strong leadership of President Park Jung-Hee in 1977.14 Thailand is an example of political stewardship that was helped by population support. A network of civic groups pushed for the introduction of a universal coverage policy. After the elections of January 2001, a policy was introduced that rapidly ensured coverage of the entire population, although this was but the last step of a process that had begun in 1975 with the establishment of free health services for low-income people.15 Some sub-Saharan African countries are also moving towards universal coverage including Zambia whose president declared the abolition of user fees in rural health facilities in April 2006.16 Prepayment of health services is being enhanced there due to an increase in government funding supported by external donors. Other countries use an alternative path. For example, Ghana has passed a health insurance law17 and Lesotho has explored the feasibility of social health insurance reform.18 Kenya’s National Hospital Insurance Fund has been examining ways of extending coverage to the informal sector,19 requiring strong political will and stewardship.
Tax-based or social health insurance?
Often the initial discussions revolve around these two broad choices that, in fact, have a number of common features. Prepayments are compulsory and are generally set according to income. All people make payments (through taxes or through contributions) whether they are sick or not, although people on very low incomes or other vulnerable groups might be exempt. People of low risk are not allowed to opt out although they might be able to take out insurance coverage for services that are not included in the tax or social health insurance funded packages. All people who are sick can draw from the pooled funds, thereby spreading the financial risks of ill health.
In both types of systems, there are substantial differences across countries in the institutional and organizational arrangements used to ensure funds are raised, pooled and used to purchase or provide services. It is the combination of institutional arrangements and legislation relating to revenue collection, pooling and purchasing/provision that determine how equitable and efficient a system is, rather than the name that is used to describe it. In fact, we have been unable to find evidence that implementation of universal coverage either via tax-based funding or social health insurance is more important to the final outcome.7,20
How can we pay?
At the outset, it is important to note that many of the low-income countries in the world are unlikely to be able to finance universal coverage from domestic sources in the short to medium term. In 2003, 48 of 59 low-income countries spent less than US$ 30 per capita on health. This includes the expenditure derived from external assistance. In 12 of these countries, total health expenditure was less than US$ 10 per capita. Even a very basic set of services for prevention and treatment would cost in excess of US$ 34 per year using year 2000 prices.21
In most countries with low levels of spending, the bulk of government health expenditure is derived from taxes of various types. Tax-financed domestic financing would have to remain prominent, even if they chose to develop a universal health insurance scheme. In the feasibility analysis of social health insurance in Kenya and Lesotho, for example, maintaining government subsidies was seen as imperative, given that contributions from the formal sector were not able to fully cross-subsidize the informal sector and the poor.18,22 External donor funding will also be needed to supplement the resources that can be raised domestically. Indeed, if universal coverage is to be achieved, there still needs to be substantial increases in external funding, with improved predictability.
How long will reform take?
International evidence shows that most reforms towards universal coverage have been gradual. Social health insurance systems, for example, usually start by covering formal sector employees and slowly expand to other population groups - often starting with dependents of the employees. In most European countries that have achieved universal coverage, the transition took place over many decades, often taking more than 50 years.23,24 More recently, in Costa Rica, the Republic of Korea and Thailand, reform took between 20 and 30 years.
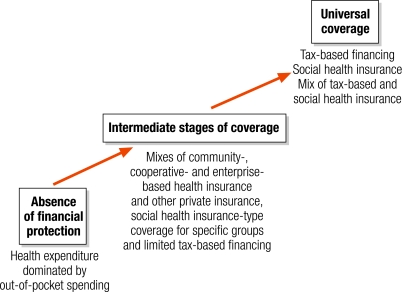
During the transition process, population coverage often remains incomplete and sometimes may even become more unequal, with the poorest groups the least likely to be protected and often the last to benefit from extended coverage. It is here that existing community, cooperative and enterprise-based health insurance, as well as other forms of private health insurance, might have a role to play, protecting as many people as possible.25 Such forms of protection will co-exist with compulsory health insurance coverage for particular population groups and with other forms of tax-based funding for particular types of health interventions (e.g. prevention and promotion) or for particular population groups (e.g. self-employed people and those on very low incomes). Eventually, however, the various forms of health insurance and tax-based funding need to be combined, though this last step can be difficult to achieve if some population groups have better coverage during the transition than others. Fig. 1 illustrates some of the key health financing options at different stages of the evolution towards universal coverage. Detailed standard paths and timelines for universal coverage are difficult to implement, however.
Fig. 1.
Key health financing options at different stages of the evolution towards universal coverage26
Factors to consider
Countries at various stages of economic development and in different social and political contexts have diverse problems and require tailored solutions. Health financing options will be shaped according to what countries can sustain. Economic constraints linked to the general state and structure of the economy as well as the size and skill distribution of the labour force will be important to consider, the latter also influencing a country’s ability to administer the process, e.g. managing the financing system capable of delivering universal coverage requires capacities in accountancy, actuarial analysis, banking and information processing. The whole process of health financing reform will also need to be monitored and guided, a task that falls naturally on the government. This imposes costs associated with the task of monitoring the process and enforcement of legislation for health financing policy.27
Broad policy norms and values, which may be also relevant beyond health financing, will also codetermine the nature of the implementing organizations and their required tasks. First, it may be stipulated that communities at village or district level would need to be given a voice in health financing. This may then explain the establishment of community-based health insurance schemes in a voluntary setting or the existence of district level mutual health insurance funds in a compulsory framework. Second, the extent of private sector involvement in the three health financing functions must be decided and appropriate legislation developed. In India, for example, it is mandatory for formal insurance companies to expand their activities to the rural and social sectors in the country so that the private sector also offers insurance coverage to parts of the low-income population.28
Third, the degree of solidarity that can be achieved in health financing is an important factor. An effective system of financial protection for the population as a whole requires a significant amount of cross-subsidization, both from rich to poor and from people at low risk of illness (e.g. the young) to people with higher risks (e.g. the elderly). Cross-subsidization must be greater the broader the extent of income inequality in a country and each country needs to define the appropriate level of solidarity for its setting. This will have an important impact on the type of organizations that are developed and their tasks. Smaller, geographically based insurance pools allow for more local autonomy but involve less risk pooling across the country as a whole. More extensive pooling arrangements may be established along with an increased acceptance of risk sharing across society’s population groups. Finally, health financing policy towards universal coverage is not isolated from the politics, pressure groups and lobbies at country level. Governments have an important role to play in interacting with stakeholders and guiding the overall public interest as health financing systems develop.29 Nevertheless, it is also this political pressure from civil society that may stimulate governments to manifest political will and to exercise good stewardship.
Towards a comprehensive framework
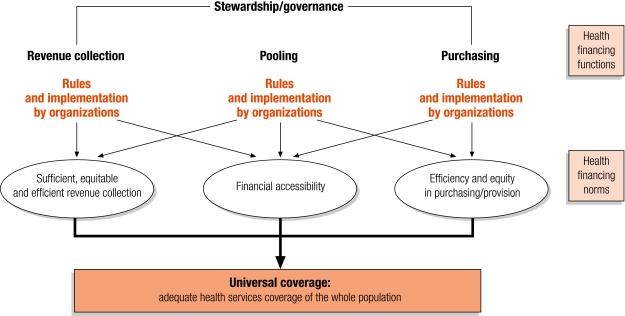
Achievement of the goal of universal coverage is contingent on the underlying institutional design of the three health financing functions (collection, pooling and purchasing/provision). We propose to integrate the concept of institutional design into a conceptual framework for assessing health financing system reform towards universal coverage. As conceptualized by North,27 institutions can be understood as “the rules of the game” that guide human and organizational interaction. These rules are the specification of the three health financing functions, as found in legislation and regulations; they are expected to reflect the specific and broad policy norms and values referred to earlier in this paper.
However, the existence of appropriate rules will not be sufficient to ensure high performance of the health financing system and the attainment or maintenance of universal coverage. Equally important is the way these rules are implemented by organizations, i.e. how these rules are carried out and put in practice. Organizations involved in the health financing functions of revenue collection, pooling and purchasing as well as stewardship may include political bodies (e.g. ministry of health, regulatory agencies), economic bodies (e.g. private health insurance, cooperatives), social bodies (e.g. social health insurance agencies, faith-based organizations) and educational bodies (e.g. training centres).27
It should be clear that rules and organizations are very much interconnected. In fact, the established rules can restrain or induce people and organizations to do certain things. In other words, rules set incentives and disincentives and as such influence behaviour of organizations and individuals and ultimately the outcomes of organizational activities. In many instances, the prevailing rules in a health financing system may not represent the most efficient institutional design to achieve or maintain universal coverage. Hence, when countries seek to move towards universal coverage, there are many explicit institutional design choices to be taken, far beyond the question of whether a predominantly tax-based system, social health insurance or a mixed system is preferred. Table 1 illustrates some of the possible rules and organizations that may specify a country’s health financing functions and norms in revenue collection, pooling and purchasing.
Table 1. Example of rules and organizations that may influence a country’s health financing functions.
| Type of rule | Legislation and other regulatory provisions of rules | Organizations |
|---|---|---|
| Revenue collection | ||
| Taxation rules | Income tax rates range from 15–40%. | MoF or revenue collection authority |
| SHI contribution rules | 6% contribution rates to be shared 50/50 by employer/employee; informal sector workers with an annual household income of more than US$ 1200 pay a flat amount of US$ 40. | For payroll deductions: SHI fund and MoF; for informal sector: NGOs, district authorities, microfinance institutions |
| Membership/registration rules | All formal sector employees and civil servants are mandatory members of the SHI scheme; informal sector workers can join voluntarily in a group of more than 20 workers in the same professional area. | SHI fund/registration department; NGOs involved in outreach activities |
| MoH schedule of user fees | The noninsured pay the established user fees at public and private health facilities. | Public and private health service providers |
| Pooling | ||
| Pooling across MOH and SHI fund | 1% of SHI income is transferred to the MoH to subsidize services rendered to the non-insured. | MoH, MoF, SHI fund |
| Risk equalization rules among SHI funds | Additional resources are provided to SHI funds with high health risk by those SHI funds with low health risks, based on a specific risk adjustment formula. | Risk equalization agency |
| Pooling within the SHI scheme | Contribution rates are income-related and not risk-related; access is based on need. | SHI fund |
| Purchasing | ||
| SHI rules on purchasing | The SHI can purchase from both public and private facilities; the SHI must contract all facilities that meet the accreditation standards. | SHI fund/contracts department, health providers associations or health providers, accreditation agency |
| SHI rules on type and rate of provider remuneration | The SHI remunerates providers on the basis of a case-payment, with pre-defined rates that vary according to the facility level. | SHI fund/remuneration department, health providers |
| MoH rules on type and rate of provider remuneration | MoH allocates global budgets to sub-national levels based on rational criteria (population characteristics, epidemiological profile, poverty rates within that sub-national unit). | MoH, subnational MoH units such as health districts, MoF |
| Rule on MoH benefit package | MoH provides an essential health services package with services at the primary, secondary and tertiary levels. | MoH |
| Rule on benefit package definition of MoH | Services are included based on cost-effectiveness, analysis results and considerations of equity of the disease burden; the benefit package is reviewed every 2 years. | MoH or a national benefit package committee |
MoF, Ministry of Finance; MoH, Ministry of Health; SHI, social health insurance; NGO, nongovernmental organization.
Ultimately, it is the combination of specific rules in revenue collection, pooling and purchasing as well as the effectiveness of organizations in implementation that will determine the efficiency and equity of a health financing system. However, before the rules and organizational arrangements can be optimized, it is necessary to assess and understand the existing situation. WHO is developing a framework for doing this, building on North’s concept of institutions and rules and some of the applications that have already been made in the area of health and social protection.30,31 Fig. 2 outlines the fundamentals of this framework; it focuses on the rules and organizational arrangements currently in force, either explicitly or implicitly, and assesses how they contribute or detract from the achievement of universal coverage. This forms the basis of plans to modify rules and organizations or to introduce new ones. An example of this framework’s application can be found in Mathauer et al.32.
Fig. 2.
Basic components of the framework to guide health financing system reform
Conclusion
The Member States of WHO have endorsed universal coverage as an important goal for the development of health financing systems but, in order to achieve this long-term solution, flexible short-term responses are needed. There is no universal formula. Indeed, for many countries, it will take some years to achieve universal coverage and the path is complex. The responses each country takes will be determined partly by their own histories and the way their health financing systems have developed to date, as well as by social preferences relating to concepts of solidarity.
It is clear that formulating and implementing health policy towards universal coverage will require a multitude of interrelated decisions. The proposed framework links the overall policy goal of universal coverage to the nuts and bolts of health financing policy, the rules and organizational arrangements. It can help countries to undertake the detailed institutional-organizational analysis required to assess the need for different kinds of change. This assessment should consider fund collection, pooling and purchasing/provision separately and should also consider the links between the three functions. This will enable a clear assessment of what rules need to be modified or developed and where organizational capacity should be strengthened. ■
Footnotes
Competing interests: None declared.
References
- 1.Preker A, Langenbrunner J, Jakab M. Rich-poor differences in health care financing. In: Dror D, Preker A, eds. Social re-insurance - a new approach to sustainable community health care financing Washington, DC: The World Bank; 2002. [Google Scholar]
- 2.Hjortsberg C. Why do the sick not utilise health care? The case of Zambia. Health Econ. 2003;12:755–70. doi: 10.1002/hec.839. [DOI] [PubMed] [Google Scholar]
- 3.Xu K, Evans D, Kawabata K, Zeramdini R, Klavus J, Murray C. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–7. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 4.Xu K, Evans D, Carrin G, Aguilar A. Designing health financing systems to reduce catastrophic health expenditure [technical briefs for policy-makers no. 2]. Geneva: WHO; 2005. [Google Scholar]
- 5.Wagstaff A, Van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993-1998. Health Econ. 2003;12:921–34. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 6.Sustainable health financing, universal coverage and social health insurance [A58/33]. Geneva: WHO; 2005.
- 7.Xu K, Evans DB, Carrin G, Aguilar AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff. 2007;26:972–83. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 8.Mills A. Strategies to achieve universal coverage: are there lessons from middle income countries [A literature review commissioned by the Health Systems Knowledge Network, Commission on the Social Determinants of Health]. Geneva: WHO;2007. [Google Scholar]
- 9.The world health report 2000: health systems: improving performance Geneva: WHO;2000. [PubMed]
- 10.Kutzin J. A descriptive framework for country-level analysis of health care financing arrangements. Health Policy. 2001;56:171–204. doi: 10.1016/S0168-8510(00)00149-4. [DOI] [PubMed] [Google Scholar]
- 11.Savedoff W, Carrin G. Developing health financing policies. In: Murray C, Evans D, eds. Health system performance assessment: debates, methods and empiricism Geneva: WHO; 2003. [Google Scholar]
- 12.Carrin G, James C. Key performance indicators for the implementation of social health insurance. Appl Health Econ Health Policy. 2005;4:15–22. doi: 10.2165/00148365-200504010-00004. [DOI] [PubMed] [Google Scholar]
- 13.Schieber G, Baeza C, Kress D, Maier M. Health financing systems in the 21st century. In: Jamison D, Breman J, Measham A, Alleyne G, Claeson M, Evans D et al., eds. Disease control priorities in developing countries 2nd edn. New York: Oxford University Press; 2006. pp. 225-42. [Google Scholar]
- 14.Yang B, Holst J. Implementation of health insurance in developing countries: Experience from selected Asian countries. In: Holst J, Brandrup-Lukanow A, eds. Extending social protection in health Eschborn, Germany: Deutsche Gesellschaft für Technische Zusammenarbeit (GTZ); 2007. pp. 158-67. [Google Scholar]
- 15.Social health insurance: selected case studies from Asia and the Pacific New Delhi & Manila: WHO/SEARO & WHO/WPRO;2005.
- 16.Guidelines on removal of user fees in public health facilities in Zambia Lusaka: Ministry of Health; 2006.
- 17.National health insurance scheme (NHIS) law [Act 650]. Accra: Government of Ghana; 2003. Available from: http://www.parliament.gh/files/imce/National_Health_Insurance_Act__2003.pdf [accessed on 26 September 2008].
- 18.Mathauer I, Doetinchem O, Kirigia J, Carrin G. Feasibility assessment and financial projection results for a social health insurance scheme in Lesotho. Geneva: WHO; 2007. [Google Scholar]
- 19.Mathauer I, Schmidt J-O, Wenyaa M. Extending social health insurance to the informal sector in Kenya. An assessment of factors affecting demand. Int J Health Plann Manage. 2008;23:51–68. doi: 10.1002/hpm.914. [DOI] [PubMed] [Google Scholar]
- 20.Carrin G, Zeramdini R, Musgrove P, Poullier JP, Valentine N, Xu K. The impact of the degree of risk-sharing in health financing on health system attainment. In: Preker A, Carrin G, eds. Health financing for poor people Washington, DC: The World Bank; 2004. [Google Scholar]
- 21.Macroeconomics and health: investing in health for economic development [report of the Commission on Macroeconomics and Health]. Geneva: WHO; 2001.
- 22.Carrin G, James C, Doetinchem O, Adelhardt M, Eriki P, Kirigia J, et al. Health financing reform in Kenya-assessing the social health insurance proposal. S Afr Med J. 2007;97:130–5. [PubMed] [Google Scholar]
- 23.Barnighausen T, Sauerborn R. One hundred and eighteen years of the German health insurance system: are there any lessons for middle- and low-income countries? Soc Sci Med. 2002;54:1559–87. doi: 10.1016/S0277-9536(01)00137-X. [DOI] [PubMed] [Google Scholar]
- 24.Carrin G, James C. Social health insurance: key factors affecting the transition towards universal coverage. Int Soc Secur Rev. 2005;58:45–64. doi: 10.1111/j.1468-246X.2005.00209.x. [DOI] [Google Scholar]
- 25.Jacobs B, Bigdeli M, van Pelt M, Ir P, Salze C, Criel B. Bridging community-based health insurance and social protection for health care - a step in the direction of universal coverage? Trop Med Int Health. 2008;13:140–3. doi: 10.1111/j.1365-3156.2007.01983.x. [DOI] [PubMed] [Google Scholar]
- 26.Carrin G, James C, Evans D. Achieving universal health coverage: developing the health financing system [technical briefs for policy-makers]. Geneva: WHO; 2005. [Google Scholar]
- 27.North DC. Institutions, institutional change and economic performance Cambridge: Cambridge University Press; 1990. [Google Scholar]
- 28.Ahuja R, Guha-Khasnobis B. Micro-insurance in India: trends and strategies for further extension [working paper no.162]. New Delhi: Indian Council for Research on International Economic Relations; 2005.
- 29.Saltman RB, Ferroussier-Davis O. The concept of stewardship in health policy. Bull World Health Organ. 2000;78:732–9. [PMC free article] [PubMed] [Google Scholar]
- 30.Mathauer I. Institutional analysis toolkit for nutrition programs: institutional assessment, institutional design, institutional capacity strengthening Washington, DC, The World Bank; 2001. [Google Scholar]
- 31.Mathauer I. Institutional analysis toolkit for safety net interventions [social protection discussion series, no. 0418]. Washington, DC: The World Bank; 2004. [Google Scholar]
- 32.Mathauer I, Cavagnero E, Vivas G. Evaluación institucional del sistema de financiamiento de salud nicaragüense Geneva & Washington, DC: WHO & PAHO; 2008. [Google Scholar]