Abstract
Objective
To assess the influence of country of origin effects and of adjustment and selection processes by comparing noncommunicable disease mortality and life expectancy among migrants to Israel from the former Soviet Union (FSU) with noncommunicable disease mortality and life expectancy among Israelis and the population of the Russian Federation.
Methods
Data from 926 870 FSU-immigrants who migrated to Israel between 1990 and 2003 (study cohort) were analysed. Life expectancy was calculated for the study cohort, all Israelis, and the population of the Russian Federation. Age-standardized death rates were calculated for grouped causes of death. FSU immigrants were additionally compared with other Israelis and with inhabitants of the Russian Federation using cause-specific standardized mortality ratios (SMRs).
Findings
Life expectancy at age 15 years in 2000–2003 was 61.0 years for male and 67.0 years for female FSU immigrants to Israel. Age-standardized death rates for FSU immigrants in Israel were similar to those of other Israelis and much lower than those of inhabitants of the Russian Federation. Relative to Israelis, the study cohort had a higher SMR for neoplasms, and particularly for stomach cancer. Mortality from brain cancer was higher when immigrants were compared to the Russian Federation (SMR: 1.71, 95% confidence interval, CI: 1.50–1.94 for males; SMR: 1.77, 95% CI: 1.56–2.02 for females), whereas mortality from stomach cancer was lower among immigrants relative to the Russian Federation (SMR: 0.43, 95% CI: 0.40–0.47 for males; SMR: 0.56, 95% CI: 0.52–0.61 for females). Mortality from external causes was lower among immigrants relative to the population of the Russian Federation (SMR: 0.20, 95% CI: 0.19–0.21 for males; SMR: 0.35, 95% CI: 0.33–0.37 for females) but significantly higher relative to other Israelis (SMR: 1.41, 95% CI: 1.35–1.47 for males; SMR: 1.08, 95% CI: 1.02–1.15).
Conclusion
Noncommunicable disease mortality among FSU immigrants to Israel is lower than in the population of the Russian Federation. Mortality rates in FSU immigrants, particularly from circulatory diseases, have rapidly adjusted and have become similar to those of the destination country. However, immigrants from the FSU have considerably higher mortality than other Israelis from external causes and some noncommunicable diseases such as cancer. Mortality rates in these diaspora migrants show a mixed picture of rapid assimilation together with persistent country of origin effects, as well as the effects of adjustment hardships.
Résumé
Objectif
Evaluer l’influence du pays d’origine et des processus d’adaptation et de sélection en comparant la mortalité par maladies non transmissibles et l’espérance de vie chez les immigrés en Israël issus de l’ex-Union soviétique avec ces mêmes variables chez les Israéliens et les habitants de la Fédération de Russie.
Méthodes
Des données concernant 926 870 personnes émigrées de l’ex-Union soviétique en Israël entre 1990 et 2003 (étude de cohorte) ont été analysées. L’espérance de vie a été calculée pour la cohorte étudiée, l’ensemble des Israéliens et la population de la Fédération de Russie. Les taux de mortalité standardisés selon l’âge ont été déterminés par groupes de causes de décès. Les immigrés provenant de l’ex-Union soviétique ont en outre été comparés avec d’autres Israéliens et avec les habitants de la Fédération de Russie au moyen des taux de mortalité standardisés (TMS) selon la cause.
Résultats
Sur la période 2000-2003, l’espérance de vie à 15 ans pour les immigrés provenant de l’ex-Union soviétique était de 61,0 ans pour les hommes et de 67,0 ans pour les femmes. Les taux de mortalité standardisés selon l’âge pour ces immigrés étaient similaires à ceux des autres Israéliens et nettement inférieurs à ceux des habitants de la Fédération de Russie. Par rapport aux Israéliens, les membres de la cohorte étudiée présentaient un TMS plus élevé pour les néoplasmes, en particulier pour le cancer de l’estomac. La mortalité par cancer du cerveau était plus forte chez les immigrés que chez les habitants de la Fédération de Russie (TMS : 1,71 ; intervalle de confiance à 95%, IC : 1,50-1,94 pour les hommes ; TMS : 1,77, IC à 95% : 1,56-2,02 pour les femmes), alors que les termes de cette comparaison s’inversaient pour le cancer de l’estomac (TMS : 0,43, IC à 95% : 0,40-0,47 pour les hommes ; TMS : 0,56, IC à 95% : 0,52-0,61 pour les femmes). La mortalité par cause externe était plus faible parmi les immigrés que dans la population de la Fédération de Russie (TMS : 0,20 ; IC à 95% : 0,19-0,21 pour les hommes ; TMS : 0,35 ; IC à 95% : 0,33-0,37 pour les femmes), mais significativement plus forte que parmi les autres Israéliens (TMS : 1,41, IC à 95% : 1,35-1,47 pour les hommes ; TMS : 1,08, IC à 95% : 1,02-1,15 pour les femmes).
Conclusion
La mortalité par maladies non transmissibles des immigrés en Israël provenant de l’ex-Union soviétique est inférieure à celle des habitants de la Fédération de Russie. Les taux de mortalité chez ces immigrés, notamment par maladie circulatoire, se sont rapidement ajustés et sont devenus similaires à ceux du pays d’accueil. Cependant, les immigrés conservent des taux de mortalité par cause externe et pour certaines maladies non transmissibles, telles que le cancer, considérablement plus élevés que ceux des autres Israéliens. Les taux de mortalité parmi cette diaspora reflètent un mélange d’assimilation rapide et de persistance des effets du pays d’origine, ainsi que les effets des difficultés d’adaptation.
Resumen
Objetivo
Evaluar la influencia del país de origen y de los procesos de adaptación y selección comparando la mortalidad por enfermedades no transmisibles y la esperanza de vida entre los migrantes a Israel de la antigua Unión Soviética (AUS) y la mortalidad por enfermedades no transmisibles y la esperanza de vida entre los israelíes y en la población de la Federación de Rusia.
Métodos
Se analizaron los datos correspondientes a 926 870 personas de la AUS que migraron a Israel entre 1990 y 2003 (cohorte de estudio). Se calculó la esperanza de vida de la cohorte de estudio, todos israelíes, y de la población de la Federación de Rusia. Se calcularon también las tasas de mortalidad normalizadas por edad para grupos de causas de mortalidad. Además, los inmigrantes de la AUS fueron comparados con otros israelíes y con los habitantes de la Federación de Rusia utilizando las razones de mortalidad normalizadas (RMN) por causas específicas.
Resultados
La esperanza de vida a los 15 años en 2000–2003 era de 61,0 años para los hombres y 67,0 años para las mujeres entre los inmigrantes de Israel procedentes de la AUS. Las tasas de mortalidad normalizadas por edad para los inmigrantes de Israel procedentes de la AUS fueron similares a las de otros israelíes y mucho más bajas que las de la población de la Federación de Rusia. En comparación con los israelíes, la cohorte de estudio presentaba una RMN mayor para las neoplasias, en particular para el cáncer de estómago. La mortalidad por cáncer cerebral fue mayor entre los inmigrantes que en la Federación de Rusia (RMN: 1,71, intervalo de confianza, IC, del 95%: 1,50–1,94 para los hombres; RMN: 1,77, IC95%: 1,56–2,02 para las mujeres), mientras que la mortalidad por cáncer de estómago entre los inmigrantes fue menor que la de la población de la Federación de Rusia (RMN: 0,43, IC95%: 0,40–0,47 para los varones; RMN: 0,56, IC95%: 0,52–0,61 para las mujeres). La mortalidad por causas externas entre los inmigrantes fue menor que en la población de la Federación de Rusia (RMN: 0,20, IC95%: 0,19–0,21 para los hombres; RMN: 0,35, IC95%: 0,33–0,37 para las mujeres) pero significativamente mayor que entre los otros israelíes (RMN: 1,41, IC95%: 1,35–1,47 para los hombres; RMN: 1,08, IC95%: 1,02–1,15 para las mujeres).
Conclusión
La mortalidad por enfermedades no transmisibles entre los inmigrantes de Israel procedentes de la AUS es más baja que en la población de la Federación de Rusia. Las tasas de mortalidad entre esos inmigrantes, en particular por problemas del aparato circulatorio, han evolucionado rápidamente hasta hacerse similares a las del país de destino. Sin embargo, los inmigrantes de la AUS presentan una mortalidad considerablemente mayor que la de otros israelíes por causas externas y por algunas enfermedades no transmisibles como el cáncer. Las tasas de mortalidad entre esos migrantes de la diáspora muestran un panorama desigual de asimilación rápida y efectos persistentes del país de origen, así como los efectos de las dificultades asociadas a la adaptación.
ملخص
الغرض
استەدفت الدراسة تقييم تأثير البلد الأصلي وتأثير عمليات التكيُّف والاختيار، بالمقارنة بين معدل الوفيات الناجمة عن الأمراض غير السارية ومأمول الحياة لدى المەاجرين إلى إسرائيل من الاتحاد السوفيتي السابق، مع مثيلتەا لدى الإسرائيليِّـين ولدى سكان الاتحاد الروسي.
الطريقة
تم تحليل البيانات المأخوذة من 870 926 من المەاجرين من الاتحاد السوفيتي السابق إلى إسرائيل في المدة من 1990 إلى 2003 (مجموعة الدراسة). وتم حساب مأمول الحياة لمجموعة الدراسة، ولجميع الإسرائيليِّـين، ولسكان الاتحاد الروسي. وتم أيضاً حساب معدلات الوفيات بحسب العمر لمجموعة مصنفة من أسباب الوفاة. كما أُجريت مقارنة بين المەاجرين من الاتحاد السوفيتي السابق وبين غيرەم من الإسرائيليِّـين وسكان الاتحاد الروسي، وذلك باستخدام نسب الوفيات بحسب أسباب معينة.
النتائج
بلغ مأمول الحياة لدى المەاجرين من الاتحاد السوفيتي السابق إلى إسرائيل عند عمر 15 عاماً، في المدة 2000 – 2003، نحو 61 عاماً للذكور و67 عاماً للإناث. وكانت معدلات الوفيات بحسب العمر لدى المەاجرين من الاتحاد السوفيتي السابق إلى إسرائيل مماثلة للمعدلات لدى سائر الإسرائيليِّـين، وأقل كثيراً من مثيلتەا لدى سكان الاتحاد الروسي. وبالنسبة إلى الإسرائيليِّـين، لوحظ ارتفاع نسبة الوفيات الناجمة عن الأورام لدى مجموعة الدراسة، ولاسيَّما سرطان المعدة. كما لوحظ ارتفاع معدل الوفيات الناجمة عن سرطان الدماغ عند المقارنة بين المەاجرين وبين سكان الاتحاد الروسي (نسبة الوفيات بحسب سبب معين: 1.71، عند فاصلة ثقة 95%: 1.50 إلى 1.94 للذكور؛ وبلغت ەذە النسبة 1.77، عند فاصلة ثقة 95%: 1.56 إلى 2.02 للإناث)، في حين كانت الوفيات الناجمة عن سرطان المعدة أقل لدى المەاجرين بالمقارنة مع سكان الاتحاد الروسي (نسبة الوفيات بحسب سبب معين: 0.43) عند فاصلة ثقة 95%: 0.40 إلى 0.47 للذكور؛ وبلغت ەذە النسبة 0.56، عند فاصلة ثقة 95%: 0.52 إلى 0.61 للإناث). وكانت الوفيات الناجمة عن أسباب خارجية أقل لدى المەاجرين بالمقارنة مع سكان الاتحاد الروسي (نسبة الوفيات بحسب سبب معين 0.20، عند فاصلة ثقة 95%: 0.19 إلى 0.21 للذكور؛ وبلغت ەذە النسبة 0.35 عند فاصلة ثقة 95%: 0.33 إلى 0.37 للإناث)، ولكث كانت ەذە النسبة عالية بشكل يعتد بە بالمقارنة مع سائر الإسرائيليِّـين (نسبة الوفيات بحسب سبب معين 1.41، عند فاصلة ثقة 95%: 1.35 على 1.47 للذكور؛ وبلغت 1.08 عند فاصلة ثقة 95%: 1.02 إلى 1.15 للإناث).
الاستنتاج
تشير النتائج إلى أن الوفيات الناجمة عن الأمراض غير السارية لدى المەاجرين من الاتحاد السوفيتي السابق تعدَّلت سريعاً وأصبحت مماثلة لتلك الموجودة في بلد المقصد. ومع ذلك، يُلاحظ أن معدل الوفيات الناجمة عن أسباب خارجية وعن بعض الأمراض غير السارية، مثل السرطان، أعلى كثيراً لدى المەاجرين من الاتحاد السوفيتي السابق بالمقارنة مع سائر الإسرائيليِّـين. كما بينت معدلات الوفيات لدى ەؤلاء المەاجرين المشتتين وجود صورة مختلطة من الاندماج السريع مع تأثيرات مستديمة للبلد الأصلي، إضافةً إلى التأثيرات الناجمة عن صعوبة التكيُّف.
Introduction
Much research has been carried out on mortality rates among migrants all over the world. However, with the focus usually on refugees and those who migrate for economic reasons, studies often overlook a group comprising millions of people: diaspora migrants.
Several countries, including Finland, Germany, Greece, Hungary and Israel, have immigration policies that encourage migration on the basis of common ancestry. Such diaspora migrations were especially numerous following the fall of the Iron Curtain, a notable example being the arrival in Israel of about 1 million immigrants from the former Soviet Union (FSU) between 1989 and 2003.1 Most were Jews, and about one quarter were non-Jewish family members. The proportion of highly educated professionals among them was much higher than among the Israeli population, but so was the proportion of single-parent families and elderly people.1 Although these migrants have enjoyed generous conditions of reception, the new country’s health system, standards of medical care, lifestyles and environment have differed greatly from those in their country of origin. Such changes, in addition to a decline in social standing and the difficulties of integration, are factors that should have an effect on mortality rates.
Since the mid-1960s, mortality rates in the FSU and Russian Federation have been rising, and the differences between them and the rates in western European countries continue to widen.2,3 The Russian Federation has some of the highest standardized death rates from noncommunicable diseases of all industrialized countries. These differences have been attributed to large numbers of deaths from external causes (such as deliberate or accidental injuries) among young men, and also from circulatory diseases in middle-aged adults.2,4 There is evidence that unhealthy behaviours and lifestyle factors such as high levels of tobacco consumption5 and alcohol abuse – especially binge drinking6 – along with increased consumption of red meat, sugar and polyunsaturated fats,7 have increased the number of deaths from preventable and chronic diseases.8–10 An increasing prevalence of obesity in the FSU could also be contributing to increased mortality rates.11
Various authors have examined the effects of certain negative characteristics of the health-care system in the FSU on the number of avoidable deaths, with poor health promotion and inadequate access to advanced health care mentioned as relevant factors.8,12–14 Consequently, the arrival in Israel of migrants from the FSU was expected to cause a significant rise in Israel’s mortality rates.15 However, a study of mortality among Jews in Moscow from 1993 to 1995 showed that these men and women had lower mortality rates than did other ethnic groups within Russia, even when controlling for their relatively high educational level. These results led the study authors to argue that mortality among Jews in Moscow was similar to mortality among Jews in Israel.16 Indeed, an analysis of data up to 1994 showed that age-adjusted mortality rates, both overall and for cardiovascular diseases, were lower among FSU immigrants to Israel than among the Jewish population residing in Israel, including native-born residents and earlier immigrants.17 Mortality among immigrant groups is known to be affected by the stresses of acculturation and by socioeconomic challenges, both of which can cause a wide range of psychopathological symptoms, and also by pre-migration health conditions and behaviour.18,19 Although immigrants to Israel receive substantial financial, occupational and educational support and housing subsidies for the first few years after they arrive, they are nevertheless affected by psychological stress from having to cope with a new social and cultural environment or a downward shift in employment status.20
A study of Russian immigrants in Israel showed that a perceived lack of social support was significantly associated with psychological distress and that length of stay did not decrease stress levels.21 According to another study of the somatic manifestations of psychological distress, a longer length of time since migration was associated with more symptoms of somatization.22
In this study the authors investigate and describe the life expectancy and mortality profile of the large migrant population that arrived in Israel from the FSU in 1990–2003 and compare it with that of the general populations of the Russian Federation and of Israel.
Methods
The study cohort consisted of all 926 870 immigrants born in the FSU who arrived in Israel between 1 January 1990 and 31 December 2003. Of the members of this group, 75% were registered as Jews in Israel and 25% as non-Jewish family members. The data set was assembled at the Israel Central Bureau of Statistics (ICBS) from administrative records of immigration, official death records, as well as border-control records of departures from Israel, all of which were matched by the unique Israeli personal identification number. An SAS software program (Cary, NC, United States of America) was used to aggregate individual person-years at risk by age, sex, year of immigration, calendar year of death and by cause of death.
Data from the cohort were analysed with an end-of-follow-up date of 31 December 2003. Dates of death were available for all years, but causes were not available for 2002. Before 1998, causes were coded in accordance with the International classification of diseases and related health problems, ninth revision (ICD-9), and thereafter with the tenth revision (ICD-10).
For comparing FSU immigrant mortality with that of the host population, a data file was constructed at the ICBS for all Israelis excluding the FSU immigrant study cohort. This was considered necessary because the cohort represents about 15% of the total population of Israel. Mortality rates for non-cohort Israelis (“other Israelis”) apply to all other Israelis, Jews and Arabs alike, including 190 000 immigrants from areas of the world other than the FSU and 40 000 immigrants who arrived in Israel from the FSU before 1990.
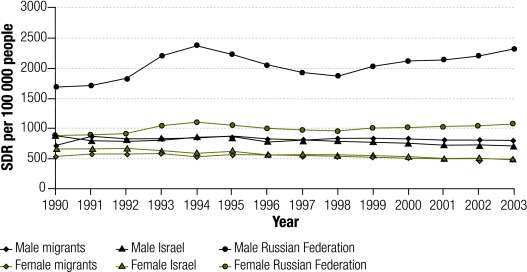
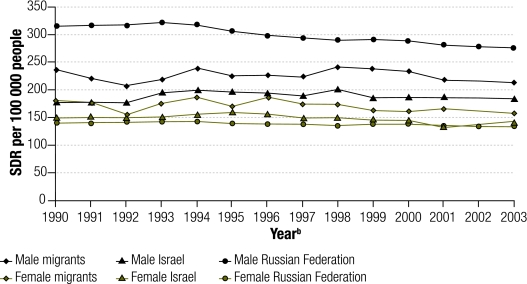
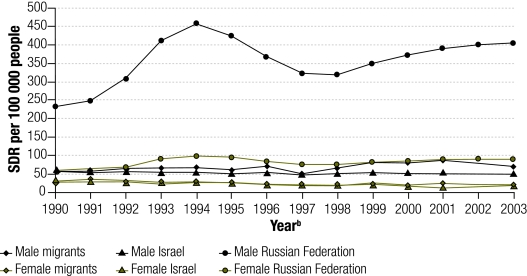
Using the European standard population as a reference, age-standardized death rates were calculated for men and women for all causes of death, all malignant neoplasms (ICD-9: 140-208; ICD-10: C00-C97), diseases of the circulatory system (ICD-9: 390-434, 436-459; ICD-10: I00-I09, I10-I13, I20-I25, I26-I51, I60-I69, I70, I71-I99), and for all external causes of mortality. The latter refer to deliberate and accidental injuries and poisoning, including deaths due to accidents, assaults or self harm (ICD-9: 800-999; ICD-10:V01-Y89). Age-standardized death rates were calculated for the study cohort and for other Israelis and are graphed in Fig. 1, Fig. 2, Fig. 3 and Fig. 4 alongside age-standardized cause-specific and sex-specific mortality rates for the Russian Federation derived from the European “health for all” database.23
Fig. 1.
SDRs for all causes of death in study of FSU immigrants to Israel, 1990–2003
FSU, former Soviet Union; SDR, standardized death rate.
Fig. 2.
SDRs for circulatory diseasesa in study of FSU migrants to Israel, 1990–2003
FSU, former Soviet Union; SDR, standardized death rate.
a International classification of diseases and related health problems, tenth revision: I00-I13, I20-I51, I60-I99.
b Cause-of-death data missing for Israeli residents in 2002.
Fig. 3.
SDRs for malignant neoplasmsa in study of FSU migrants to Israel, 1990–2003
FSU, former Soviet Union; SDR, standardized death rate.
a International classification of diseases and related health problems, tenth revision: C00-C97.
b Cause-of-death data missing for Israeli residents in 2002.
Fig. 4.
SDRs for external causes of deatha in study of FSU migrants to Israel, 1990–2003
FSU, former Soviet Union; SDR, standardized death rate.
a International classification of diseases and related health problems, tenth revision: V01-Y89.
b Cause-of-death data missing for Israeli residents in 2002.
Life expectancies at ages 15 and 65 years were calculated for three 4-year-periods: 1992–1995, 1996–1999 and 2000–2003. Data were pooled into periods to restrict random variation in mortality rates. Indirect standardization to mortality rates of the Russian Federation and the non-FSU immigrant Israeli population was performed for cohort members who died between 1990 and 2001 or in 2003 and who were aged 15 years or older at death. Mortality rates of the Russian Federation were used for the country of origin comparison since mortality data limited to the Jewish population of the FSU were not available. Mortality rates for the Russian Federation and the expected number of deaths in the FSU immigrant population were calculated on the basis of mortality and population data obtained from the WHO mortality database.24
Standardized mortality ratios (SMRs) and 95% confidence intervals (95% CI) were calculated for all causes of death, all malignant neoplasms and major tumour sites, diseases of the circulatory system (cardiovascular and cerebrovascular diseases separately) and all external causes of death.
Results
Table 1 shows the demographic characteristics of the cohort. Almost two-thirds of the immigrants had arrived from the Ukraine or the Russian Federation. Mean age at immigration was 33.5 years for men and 37.3 years for women.
Table 1. Cohort characteristics.
| Characteristic | Cohort (n = 926 870) |
|---|---|
| No. (%) | |
| Vital status | |
| Alive in Israel at end datea | 767 281 (82.8) |
| Deaths to end datea | 74 231 (8.0) |
| Left Israel before end datea | 85 358 (9.2) |
| Origin in the FSUb | |
| Ukraine | 302 175 (32.6) |
| Russian Federation | 294 745 (31.8) |
| Central Asian republicsc | 115 609 (12.5) |
| Belarus | 71 124 (7.7) |
| Caucasian republicsd | 57 992 (6.3) |
| Moldova | 47 042 (5.1) |
| Baltic republicse | 21 003 (2.3) |
| Unknown | 17 180 (1.9) |
| Sex | |
| Male | 431 774 (46.6) |
| Female | 495 096 (53.4) |
| Religion | |
| Jewish | 695 094 (75.0) |
| Non-Jewish | 231 776 (25.0) |
| Age at immigration | |
| 0–14 years | 182 622 (19.7) |
| 15–29 years | 226 568 (24.4) |
| 30–44 years | 209 616 (22.6) |
| 45–59 years | 140 889 (15.2) |
| 60–74 years | 128 975 (13.9) |
| ≥ 75 years | 38 199 (4.1) |
| Period of arrival | |
| 1990 | 184 030 (19.9) |
| 1991 | 147 048 (15.9) |
| 1992–1993 | 130 770 (14.1) |
| 1994–1995 | 132 031 (14.2) |
| 1996–1997 | 113 011 (12.2) |
| 1998–1999 | 109 642 (11.8) |
| 2000–2001 | 80 831 (8.7) |
| 2002–2003 | 29 507 (3.2) |
| Total | 926 870 (100.0) |
FSU, former Soviet Union. a End date, 31 December 2003. b In descending order of population. c Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, Uzbekistan. d Armenia, Azerbaijan, Georgia. e Estonia, Latvia, Lithuania.
Table 2 shows life expectancies at ages 15 and 65 years for the Russian Federation, immigrants to Israel from the FSU and other Israelis. In 1992–1995, male FSU immigrants to Israel had a 14.7-year advantage in life expectancy at age 15 over men in the Russian Federation, whereas women had an advantage of 6.3 years. At age 65 years, FSU immigrants had a much smaller advantage that was similar for men and women. Compared with other females in Israel, female FSU immigrants had slightly longer life expectancy at both 15 and 65 years of age. By 2000–2003, male FSU immigrants had a life expectancy equal to that of other Israelis at age 65 years, but their life expectancy at age 15 years had fallen behind that of other Israelis by 2.0 years.
Table 2. Life expectancy in the Russian Federation and in Israel at age 15 years (e15) and 65 years (e65): 1992–1995, 1996–1999 and 2000–2003.
| Life expectancy in years | Russian Federation |
Israel |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| FSU immigrants |
Other Israelis |
||||||||||
| Men | Women | Differencea | Men | Women | Differencea | Men | Women | Differencea | |||
| 1992–1995 | |||||||||||
| e15 | 45.9 | 58.8 | 12.8 | 60.6 | 65.1 | 4.5 | 61.2 | 64.9 | 3.7 | ||
| e65 | 11.0 | 15.1 | 4.1 | 16.2 | 18.4 | 2.1 | 15.8 | 17.8 | 2.0 | ||
| 1996–1999 | |||||||||||
| e15 | 47.2 | 59.3 | 12.1 | 60.7 | 66.1 | 5.4 | 62.0 | 65.6 | 3.7 | ||
| e65 | 11.3 | 15.2 | 3.9 | 16.5 | 19.0 | 2.5 | 16.4 | 18.4 | 2.0 | ||
| 2000–2003 | |||||||||||
| e15 | 45.3 | 58.4 | 13.1 | 61.0 | 67.0 | 6.1 | 63.0 | 66.8 | 3.8 | ||
| e65 | 10.9 | 15.1 | 4.2 | 17.2 | 19.8 | 2.6 | 17.3 | 19.4 | 2.0 | ||
| Change from 1992–1995 to 2000–2003 (in years) | |||||||||||
| e15 | –0.6 | –0.4 | +0.4 | +1.9 | +1.8 | +1.9 | |||||
| e65 | –0.1 | –0.1 | +1.0 | +1.5 | +1.5 | +1.6 | |||||
FSU, former Soviet Union. a Between men and women, in years.
Overall mortality among FSU immigrants was lower than for the Russian Federation and showed the same trend over time as life expectancy when compared to mortality among other Israelis. Mortality rates for female FSU immigrants converged to Israeli rates by the mid-1990s, whereas the age-standardized death rates of male immigrants from the late 1990s were lower than those of other Israelis (Fig. 1). Despite high rates of death from all circulatory diseases in the Russian Federation, mortality from these diseases in FSU immigrants of either sex was lower than among other Israelis in the early 1990s but had attained similar levels by the mid-1990s (Fig. 2). The biggest difference in death rates was seen for malignant neoplasms (Fig. 3). Although male FSU immigrants had lower rates of cancer mortality than men in the Russian Federation, they had significantly higher rates than the rest of the Israeli population. Female immigrants seemed to be worse off, with higher cancer mortality rates than noted for other Israeli and Russian women. Fig. 4 shows that age-standardized rates of death from external causes among male immigrants increased, while such rates among other Israelis stayed constant throughout the study period.
Applying indirect standardization to the 1990–2003 period as a whole, male FSU immigrants had slightly higher overall mortality than other Israelis, with an SMR of 1.05 (95% CI: 1.04–1.07), while the rate in women was slightly lower, with an SMR of 0.94 (95% CI: 0.93–0.95; Table 3). Compared with the Russian population, FSU immigrants to Israel of either sex had mortality rates that were lower by half: 0.406 (95% CI: 0.401–0.411) among men and 0.568 (95% CI: 0.562–0.574) among women.
Table 3. SMRs: FSU immigrants in Israel compared with the Russian Federation and Israel.
| Cause of death | ICD-10 | Men |
Women |
|||||
|---|---|---|---|---|---|---|---|---|
| Deaths | Russian Federation SMR (95% CI) | Israel SMR (95% CI) | Deaths | Russian Federation SMR (95% CI) | Israel SMR (95% CI) | |||
| All causes | 28 082 | 0.406 | 1.053 | 31 625 | 0.568 | 0.942 | ||
| (0.401–0.411) | (1.041–1.065) | (0.562–0.574) | (0.932–0.953) | |||||
| All malignant neoplasms | C00-D00 | 7 740 | 0.77 | 1.22 | 9 036 | 1.31 | 1.15 | |
| (0.75–0.79) | (1.20–1.25) | (1.28–1.34) | (1.13–1.17) | |||||
| Stomach | C16 | 717 | 0.43 | 1.85 | 599 | 0.56 | 1.86 | |
| (0.40–0.47) | (1.72–1.99) | (0.52–0.61) | (1.71–2.01) | |||||
| Colorectal | C18-C21 | 1 218 | 1.25 | 1.41 | 1 357 | 1.35 | 1.21 | |
| (1.18–1.32) | (1.33–1.49) | (1.28–1.43) | (1.15–1.28) | |||||
| Liver | C22 | 239 | 0.85 | 1.41 | 220 | 1.17 | 1.30 | |
| (0.75–0.96) | (1.24–1.60) | (1.02–1.32) | (1.14–1.48) | |||||
| Pancreas | C25 | 488 | 1.24 | 1.20 | 507 | 1.53 | 1.07 | |
| (1.13–1.35) | (1.10–1.31) | (1.40–1.67) | (0.99–1.17) | |||||
| Lung | C33-C34 | 1 590 | 0.51 | 1.21 | 555 | 1.14 | 0.75 | |
| (0.49–0.54) | (1.15–1.27) | (1.05–1.24) | (0.69–0.82) | |||||
| Prostate | C61 | 474 | 1.05 | 0.73 | NA | NA | NA | |
| (0.96–1.15) | (0.67–0.80) | |||||||
| Breast | C50 | NA | NA | 1 859 | 1.74 | 1.15 | ||
| (1.67–1.83) | (1.10–1.20) | |||||||
| Ovary | C56 | NA | NA | 503 | 1.33 | 1.22 | ||
| (1.22–1.45) | (1.12–1.34) | |||||||
| Brain | C70-C72 | 242 | 1.71 | 1.33 | 225 | 1.77 | 1.22 | |
| (1.50–1.94) | (1.17–1.51) | (1.56–2.02) | (1.07–1.40) | |||||
| Leukaemia | C91-C95 | 326 | 1.51 | 1.09 | 313 | 1.70 | 0.94 | |
| (1.36–1.68) | (0.98–1.21) | (1.52–1.90) | (0.85–1.05) | |||||
| Diseases of the circulatory system | I00-I13 | 9 370 | 0.266 | 0.986 | 11 385 | 0.305 | 0.900 | |
| I20-I51 | (0.261–0.271) | (0.965–1.005) | (0.300–0.310) | (0.881–0.913) | ||||
| I60-I99 | ||||||||
| Cardiovascular diseases | I00-I13 | 7 157 | 0.335 | 0.989 | 8 239 | 0.44 | 0.89 | |
| I20-I51 | (0.328–0.343) | (0.967–1.013) | (0.43–0.45) | (0.87–0.91) | ||||
| Cerebrovasc. diseases | I60-I69 | 1 925 | 0.165 | 0.961 | 2 883 | 0.184 | 0.951 | |
| (0.157–0.172) | (0.919–1.005) | (0.177–0.191) | (0.917–0.986) | |||||
| All external causes | V01-Y89 | 2 397 | 0.20 | 1.41 | 1 170 | 0.35 | 1.08 | |
| (0.19–0.21) | (1.35–1.47) | (0.33–0.37) | (1.02–1.15) | |||||
FSU, former Soviet Union; SMR, standardized mortality ratio; ICD-10, International classification of diseases and related health problems, tenth revision; NA, not applicable.
The pattern of mortality from malignant neoplasms differed by sex and comparison population. Whereas male FSU immigrants had lower rates of death from all cancers than men in the Russian Federation (0.77; 95% CI: 0.75–0.79), female FSU immigrants had higher rates than Russian women, with an SMR of 1.31 (95% CI: 1.28–1.34). In comparison with women in the Russian Federation, female FSU immigrants had SMRs in the range of 1.7 and higher for cancers of the breast and brain, as well as for leukaemias, with breast cancer accounting for 37% of the excess observed deaths from neoplasms. Male FSU immigrants to Israel had a lower rate of cancer deaths than Russians overall, but this difference was chiefly due to much smaller rates of death from lung and stomach cancer. In comparison with other Israelis, FSU immigrants had higher cancer mortality for all examined causes except for prostate cancer, leukaemia, and, in women only, cancer of the pancreas and lung.
Excess mortality from stomach cancer was especially noteworthy. Immigrants of both sexes had almost twice the risk of dying from stomach cancer as other Israelis, with an SMR of 1.86 (95% CI: 1.71–2.01) for women and 1.85 (95% CI: 1.72–1.99) for men, and the disease accounted for 24% of excess deaths from neoplasms. However, for both sexes stomach cancer mortality among FSU immigrants to Israel was approximately half of that among the people of the Russian Federation, and the SMR was among the lowest of all when compared to that in the country of origin.
Likewise, male FSU immigrants to Israel had half the lung cancer risk of Russians, but an SMR of 1.21 (95% CI: 1.15–1.27) compared with other Israelis. However, lung cancer mortality among female FSU immigrants was higher than in the country of origin (SMR: 1.14; 95% CI: 1.05–1.24) but substantially lower than among Israeli women (SMR: 0.75; 95% CI: 0.69–0.82). Mortality from liver cancer was much higher in male FSU immigrants than in other Israelis, with an SMR of 1.41 (95% CI: 1.24–1.60). However, male immigrants were less likely to die from liver cancer than were men in the Russian Federation (SMR: 0.85; 95% CI: 0.75–0.96).
Large differences between FSU immigrants and the general Russian population were found in mortality from noncommunicable diseases, such as cardiovascular and cerebrovascular diseases, favouring FSU immigrants. Differences between FSU immigrants and other Israelis were either insignificant or favoured the immigrants (Table 3). Mortality from external causes was much lower among FSU immigrants than for the Russian Federation (SMR: 0.20 for men, 0.35 for women). However, FSU immigrants of both sexes, and particularly men, had a significantly elevated risk of death from external causes compared with other Israelis resulting in an SMR of 1.41 (95% CI: 1.35-1.47) for male and 1.08 (95% CI: 1.02-1.15) for female immigrants.
Discussion
The results of this study show that mortality rates among FSU immigrants to Israel resemble those of the destination country more than those of the country of origin, mirroring the apparent relative advantages in mortality rates for Jews in Moscow relative to other Russians.16 Furthermore, the findings support the hypothesis that mortality patterns in the immigrant study population resemble those in the predominantly Jewish population of Israel. Similarly, in another study of diaspora migration, a cohort of Russian immigrants to Germany who were of German ethnic origin were found to have better mortality rates than those in their country of origin and which resembled those of native Germans.25,26
Mortality from diseases of the circulatory system is of particular interest given its substantial contribution to the growing gap in life expectancy between the Russian Federation and the rest of the developed world. The low SMR for circulatory diseases when FSU immigrants in Israel were compared to the Russian Federation is in line with findings from Shkolnikov et al.16 to the effect that male Jews in Moscow have lower mortality rates from heart disease and cerebrovascular diseases than other Russians. Moreover, our data support the finding that better educated Russians have lower death rates from circulatory diseases,27 since FSU immigrants are highly educated, with nearly 49% of them having over 13 years of schooling.28 The trend towards a decrease in age-standardized death rates from circulatory diseases in the study population, convergent with the pattern in Israeli rates, may be the result of assimilation effects, such as changes in diet, but are more than likely due to increased utilization of modern treatments.
Country-of-origin effects are most evident in cancer mortality data, although comparisons with the Russian Federation must be made with caution since weaknesses in the cause-of-death registration of neoplasms have been identified.29 When compared with all Russians, male FSU immigrants to Israel and male Jews in Moscow show lower mortality from cancer in general and particularly from lung and stomach cancer. Yet when cancer mortality rates among FSU immigrants to Israel are compared with mortality rates among other Israelis, the immigrants appear to have had a greater exposure to risk factors for cancer in the FSU and to have continued to have higher cancer mortality rates even after moving to Israel. The long latency period for most tumours would make risk-factor exposure relevant long after immigration had taken place. Health policy-makers should therefore be alerted to the increased risk of cancer in this particular immigrant population.
Lung cancer is the most frequently observed cancer among male FSU immigrants to Israel, and their lung cancer mortality rate lies between that of the Russian Federation and that of Israel. Since lung cancer rates are mainly determined by smoking prevalence, this result suggests that men in the FSU immigrant cohort are less likely to smoke than Russians but more likely to do so than other Israelis. Among women, the opposite effect was noted: rates of lung cancer mortality in the study cohort were higher than those in the Russian Federation but lower than those in Israel. This finding may be due to the predominantly urban origin of FSU immigrants, since female smoking in the Russian Federation is more common in urban areas, but this cannot be concluded from the data obtained.
Among female FSU immigrants, breast cancer is the most common malignancy. The high SMR when FSU immigrant rates are compared to those of the Russian Federation may be partly the result of genetic factors.30,31 In comparison with other Israelis, FSU immigrants have only slightly higher mortality from breast cancer. Reproductive factors, such as low fertility rates, may be playing a role, but firm conclusions cannot be drawn from the data. It has been suggested that cultural factors and the economic and emotional burdens of immigration are associated with less frequent gynaecological check-ups and mammography among FSU immigrants in Israel, which may lead to late diagnosis and increased mortality.32,33
For both sexes, mortality rates from stomach cancer among FSU immigrants lie between Russian and Israeli rates – substantially lower than the first and substantially higher than the latter. Dietary factors are likely to play a role in this respect, along with differences in the prevalence of Helicobacter pylori infection.34,35
Brain cancer is the only tumour type showing a greater relative risk for FSU immigrants to Israel than for both other Israelis and the population of the Russian Federation. An increased risk of brain tumours among Jews in general and among Jews in Israel in particular has been reported.36 The higher risk in FSU immigrants as compared to other Israelis may be triggered by the process of immigration itself. In the United States of America, an 82% higher risk of death from brain cancer was found among immigrants than among native-born residents.37 A study of immigrants to Canada showed a similar pattern: SMRs for all cancer sites were close to one; however, the SMR was significantly higher when male immigrants were compared to the Canadian-born population and even higher when they were compared to the population of their countries of origin.38 The stress of resettlement was suggested as a possible cause, along with exposure to chemicals in low-skilled occupations in industry and agriculture. However, since the aetiology of brain cancer is not well understood, these theories remain speculative.
The elevated SMR for external causes of death among men in the study cohort may be associated with patterns of risky behaviour, perhaps related to alcohol use, which were brought from the Russian Federation.39,40 On the other hand, difficulties in psychosocial adjustment might result in elevated deaths from violence, accidents and suicide. Studies of FSU immigrants in Israel have shown that levels of psychological distress are not attenuated over time.21 Loss of professional status was widespread among immigrants and may have annulled the usual protective effect of a higher educational level against distress. Rising age-standardized rates of mortality from external causes among FSU immigrants point to the need for social intervention programmes long after migration.
The growing gap between male and female FSU immigrants in Israel in life expectancy at age 15 years is in contrast with the small gap of 3.5 years observed in Moscow Jews in life expectancy at age 20, which is similar to the gap observed between males and females among Jews in Israel. Deaths from external causes may explain most of this growing gap in people below the age of 65 years. The very small differences found in life expectancy at age 65 years between FSU immigrants to Israel and other Israelis could be indicative of selective migration among older people, with the least healthy among the elderly possibly left behind.
These conclusions depend on the quality of the data from official death certificates. Both FSU immigrants to Israel and other Israelis were diagnosed and coded within the same system, making any bias between these two groups unlikely. The risk of differences in diagnostic and coding practices between Israel and the Russian Federation were minimized by focusing on broad categories of causes of death. Similarly, changes in classifications between ICD-9 and ICD-10 are unlikely to have affected the analysis.
Although post-1990 immigrants to Israel from places other than the FSU were included in the data set representing the host country, it is unlikely that their inclusion biased the results since they constitute only 2.7% of the total Israeli population. The choice of the Russian Federation as a reference was based on the fact that its data were better than the data available from any other state of the FSU. Mortality trends in the Ukraine, the other principal area of origin, are similar to those in the Russian Federation.41 Nevertheless, greater differences may exist between mortality trends in the Russian Federation and mortality trends in other areas of origin within the FSU or among immigrant populations from the Central Asian republics.
Similarly, the differences in mortality risk detected in this study have to be interpreted with caution, since socioeconomic characteristics and risk-factor exposure were not controlled for. Furthermore, in this initial analysis there was no control for length of stay in Israel and for possible differences between the immigrants by period of arrival.
The main methodological strengths of our study are the large size of the immigrant cohort, the long time over which the data were gathered and the completeness of follow-up, all of which are rare among migrant studies and made it possible to report findings on specific mortality groupings with a fair degree of confidence. One direct implication of this study is that the advantages and disadvantages in mortality shown by immigrants compared with other groups result from complex effects linked to their country of origin and to their destination. Such effects need to be disaggregated if they are to be understood.
This study has shown that mortality patterns among the FSU immigrant population differed from those in the country of origin and that the expectation, based on Russian mortality patterns, that the FSU immigrants would impose a heavy burden on the Israeli health system was misplaced. However, it is not possible to confirm whether the relatively low mortality rates in the cohort compared to the Russian Federation are due to the “healthy migrant effect” in diaspora migration. Many differences are presumably related to the lifestyle of the Jewish community in Russia; however, since there is no detailed information on the cause-specific mortality of the Jewish population of the FSU as a whole, it is not possible to construct pre-migration mortality profiles. Ethnicity-specific mortality analysis with risk factor assessment should be the subject of future research.
The data from this study show that the stresses of migration have significant health consequences, even in the presence of generous migrant reception policies, highly-educated immigrants and ethnic similarities between the host and the migrant population. These stresses seem to be especially acute for men, who may be less likely to seek aid than women and would benefit from outreach programmes. On the positive side, the study data document improvements in mortality from noncommunicable diseases that may result from the availability of modern treatment methods for cardiovascular diseases in the host country. Conversely, mortality from certain cancers is persistently large among FSU immigrants, because they do not take advantage of the more advanced treatment that is available in Israel. This finding indicates the need for enhanced screening programmes targeted at migrants and their specific vulnerabilities. ■
Acknowledgements
Data were assembled at the Israel Central Bureau of Statistics.
Footnotes
Funding: The study was funded by a grant from the German Research Foundation, Graduate College 793: epidemiology of communicable and chronic noncommunicable diseases and their interrelationships.
Competing interests: None declared.
References
- 1.ICBS, Israel Central Bureau of Statistics. Immigrants, by period of immigration, country of birth and last country of residence. 2003. Available from: http://www.cbs.gov.il/publications [accessed on 22 October 2008].
- 2.Men T, Brennan P, Boffetta P, Zaridze D. Russian mortality trends for 1991-2001: analysis by cause and region. BMJ. 2003;327:964. doi: 10.1136/bmj.327.7421.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leon DA, Chenet L, Shkolnikov VM, Zakharov S, Shapiro J, Rakhamanova G, et al. Huge variation in Russian mortality rates 1984-94: artifact, alcohol, or what? Lancet. 1997;350:383–8. doi: 10.1016/S0140-6736(97)03360-6. [DOI] [PubMed] [Google Scholar]
- 4.Notzon FC, Komarov YM, Ermakov SP, Sempos CT, Marks JS, Sempos EV. Causes of declining life expectancy in Russia. JAMA. 1998;279:793–800. doi: 10.1001/jama.279.10.793. [DOI] [PubMed] [Google Scholar]
- 5.McKee M, Bobak M, Rose R, Shkolnikov V, Chenet L, Leon D. Patterns of smoking in Russia. Tob Control. 1998;7:22–6. doi: 10.1136/tc.7.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bobak M, McKee M, Rose R, Marmot M. Alcohol consumption in a national sample of the Russian population. Addiction. 1999;94:857–66. doi: 10.1046/j.1360-0443.1999.9468579.x. [DOI] [PubMed] [Google Scholar]
- 7.Popkin B, Zohoori N, Kohlmeier L, Baturin A, Martinchik A, Deev A. Nutritional risk factors in the former Soviet Union. In: Bobadilla JL, Costello, CA, Mitchell F, eds. Premature death in the new independent states Washington, DC: National Academy Press; 1997. pp. 314-35. [Google Scholar]
- 8.Andreev EM, Nolte E, Shkolnikov VM, Varavikova E, McKee M. The evolving pattern of avoidable mortality in Russia. Int J Epidemiol. 2003;32:437–46. doi: 10.1093/ije/dyg085. [DOI] [PubMed] [Google Scholar]
- 9.Anderson BA, Silver BD. Patterns of cohort mortality in the Soviet population. Popul Dev Rev. 1989;15:471–501. doi: 10.2307/1972443. [DOI] [Google Scholar]
- 10.Bobak M, Marmot M. East-West mortality divide and its potential explanations: proposed research agenda. BMJ. 1996;312:421–5. doi: 10.1136/bmj.312.7028.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jahns L, Baturin A, Popkin BM. Obesity, diet and poverty: trends in the Russian transition to market economy. Eur J Clin Nutr. 2003;57:1295–302. doi: 10.1038/sj.ejcn.1601691. [DOI] [PubMed] [Google Scholar]
- 12.Shkolnikov V, Andreev E, Leon D, McKee M, Meslé F, Vallin J. Mortality reversal in Russia: the story so far. Hygiea Internationalis. 2004;4:29–80. doi: 10.3384/hygiea.1403-8668.044129. [DOI] [Google Scholar]
- 13.Remennick LI, Shtarkshall RA. Technology versus responsibility: immigrant physicians from the former Soviet Union reflect on Israeli health care. J Health Soc Behav. 1997;38:191–202. doi: 10.2307/2955366. [DOI] [PubMed] [Google Scholar]
- 14.World development report: from plan to market New York: Oxford University Press; 1996. [Google Scholar]
- 15.Rennert G. Implications of Russian immigration on mortality patterns in Israel. Int J Epidemiol. 1994;23:751–6. doi: 10.1093/ije/23.4.751. [DOI] [PubMed] [Google Scholar]
- 16.Shkolnikov VM, Andreev EM, Anson J, Meslé F. The peculiar pattern of mortality of Jews in Moscow, 1993-1995. Popul Stud (Camb) 2004;58:311–29. doi: 10.1080/0032472042000272366. [DOI] [PubMed] [Google Scholar]
- 17.Rotem N. Mortality among immigrants from former USSR 1990-1994: current briefings in statistics 8 Jerusalem: Central Bureau of Statistics; 1998. [Google Scholar]
- 18.Bhugra D, Jones P. Migration and mental illness Available from: http://apt.rcpsych.org/cgi [accessed on 22 October 2008].
- 19.Bhugra D. Migration, distress and cultural identity. Br Med Bull. 2004;69:129–41. doi: 10.1093/bmb/ldh007. [DOI] [PubMed] [Google Scholar]
- 20.Baider L, Ever-Hadani P, DeNour AK. Crossing new bridges: the process of adaptation and psychological distress of Russian immigrants in Israel. Psychiatry. 1996;59:175–83. doi: 10.1080/00332747.1996.11024758. [DOI] [PubMed] [Google Scholar]
- 21.Lerner Y, Kertes J, Zilber N. Immigrants from the former Soviet Union, 5 years post-immigration to Israel: adaptation and risk factors for psychological distress. Psychol Med. 2005;35:1805–14. doi: 10.1017/S0033291705005726. [DOI] [PubMed] [Google Scholar]
- 22.Ritsner M, Ponizovsky A, Kurs R, Modai I. Somatization in an immigrant population in Israel: a community survey of prevalence, risk factors, and help-seeking behavior. Am J Psychiatry. 2000;157:385–92. doi: 10.1176/appi.ajp.157.3.385. [DOI] [PubMed] [Google Scholar]
- 23.European health for all database. Geneva: World Health Organization; 2008. Available from: http://www.euro.who.int [accessed on 22 October 2008].
- 24.WHO Mortality database. Geneva: World Health Organization; 2008. Available from: http://www.who.int/whosis/mort [accessed on 22 October 2008].
- 25.Kyobutungi C, Ronellenfitsch U, Razum O, Becher H. Mortality from external causes among ethnic German immigrants from former Soviet Union countries, in Germany. Eur J Public Health. 2006;16:376–82. doi: 10.1093/eurpub/ckl013. [DOI] [PubMed] [Google Scholar]
- 26.Ronellenfitsch U, Kyobutungi C, Becher H, Razum O. All-cause and cardiovascular mortality among ethnic German immigrants from the former Soviet Union: a cohort study. BMC Public Health. 2006;6:16. doi: 10.1186/1471-2458-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shkolnikov VM, Leon DA, Adamets S, Andreev E, Deev A. Educational level and adult mortality in Russia: an analysis of routine data 1979–1994. Soc Sci Med. 1998;47:357–69. doi: 10.1016/S0277-9536(98)00096-3. [DOI] [PubMed] [Google Scholar]
- 28.Israel, Central Bureau of Statistics. Immigration to Israel, 2000-2001 [Publication No. 1291]. Jerusalem: CBS; 2007.
- 29.Shkolnikov VM, McKee M, Vallin J, Aksel E, Leon D, Chenet L, et al. Cancer mortality in Russia and Ukraine: validity, competing risks and cohort effects. Int J Epidemiol. 1999;28:19–29. doi: 10.1093/ije/28.1.19. [DOI] [PubMed] [Google Scholar]
- 30.Kelsey JL, Bernstein L. Epidemiology and prevention of breast cancer. Annu Rev Public Health. 1996;17:47–67. doi: 10.1146/annurev.pu.17.050196.000403. [DOI] [PubMed] [Google Scholar]
- 31.Rubinstein WS. Hereditary breast cancer in Jews. Fam Cancer. 2004;3:249–57. doi: 10.1007/s10689-004-9550-2. [DOI] [PubMed] [Google Scholar]
- 32.Remennick LI. Preventive behavior among recent immigrants: Russian-speaking women and cancer screening in Israel. Soc Sci Med. 1999;48:1669–84. doi: 10.1016/S0277-9536(99)00051-9. [DOI] [PubMed] [Google Scholar]
- 33.Remennick L. The challenge of early breast cancer detection among immigrant and minority women in multicultural societies. Breast J. 2006;12(Suppl 1):S103–10. doi: 10.1111/j.1075-122X.2006.00204.x. [DOI] [PubMed] [Google Scholar]
- 34.González CA, Pera G, Agudo A, Bueno-de-Mesquita HB, Ceroti M, Boeing H, et al. Fruit and vegetable intake and the risk of stomach and oesophagus adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Int J Cancer. 2006;118:2559–66. doi: 10.1002/ijc.21678. [DOI] [PubMed] [Google Scholar]
- 35.Palli D, Masala G, Del Giudice G, Plebani M, Basso D, Berti D, et al. CagA+ Helicobacter pylori infection and gastric cancer risk in the EPIC-EURGAST study. Int J Cancer. 2007;120:859–67. doi: 10.1002/ijc.22435. [DOI] [PubMed] [Google Scholar]
- 36.Inskip PD, Tarone RE, Hatch EE, Wilcosky TC, Fine HA, Black PM, et al. Sociodemographic indicators and risk of brain tumours. Int J Epidemiol. 2003;32:225–33. doi: 10.1093/ije/dyg051. [DOI] [PubMed] [Google Scholar]
- 37.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 2001;91:392–9. doi: 10.2105/AJPH.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Neutel CI, Quinn A, Brancker A. Brain tumour mortality in immigrants. Int J Epidemiol. 1989;18:60–6. doi: 10.1093/ije/18.1.60. [DOI] [PubMed] [Google Scholar]
- 39.Neumark YD, Lopez-Quintero C, Grinshpoon A, Levinson D. Alcohol drinking patterns and prevalence of alcohol-abuse and dependence in the Israel National Health Survey. Isr J Psychiatry Relat Sci. 2007;44:126–35. [PubMed] [Google Scholar]
- 40.Schiff M, Rahav G, Teichman M. Israel 2000: immigration and gender differences in alcohol consumption. Am J Addict. 2005;14:234–47. doi: 10.1080/10550490590949578. [DOI] [PubMed] [Google Scholar]
- 41.Meslé F. Mortality in central and eastern Europe: long-term trends and recent upturns. Demo Res (Max Planck Institute for Demographic Research, Germany) 2004:16 April.