Abstract
BACKGROUND:
While health service use appears to be positively correlated with resource availability, no study has explored the interactions among health service supply, cardiovascular disease burden and health service use. The objective of the present study was to examine the relationship among cardiovascular evaluation and management intensity, physician supply and cardiovascular disease burden in the Canadian population.
METHODS:
The present cross-sectional, population-based study consisted of adult residents in Ontario in 2001. Cardiac evaluation and management intensity, the main outcome measure, was measured at the individual level, and consisted of receiving one or more of the following services: noninvasive cardiac testing, coronary angiography and statin use (the latter among individuals 65 years of age and older). Mortality was the secondary outcome measure. Cardiovascular disease burden, and cardiologist and primary care physician supply were measured at the regional (ie, county) level. Analyses were adjusted for age and sex using Poisson regression, accounting for regional clustering.
RESULTS:
Regional per capita cardiologist supply varied more than twofold across regions, but was inversely related to the regional cardiovascular disease burden (r=−0.34, P=0.01). Primary care physician supply was relatively evenly distributed across regions. Residents in areas with more cardiologists were more likely to receive some form of cardiac intervention (RR=1.074, 95% CI 1.066 to 1.082 per additional cardiologist per 100,000). Those in areas with more primary care physicians were also more likely to receive noninvasive cardiac testing (RR=1.056, 95% CI 1.051 to 1.061 per six additional primary care physicians per 100,000). However, the intensity of provision of cardiac health services was unrelated to regional cardiovascular disease burden and was not associated with improved survival.
CONCLUSIONS:
The mismatch between physician supply and cardiac disease burden may explain why cardiovascular health service use is neither concordant with the cardiovascular disease burden nor associated with mortality in the population. These results underscore the importance of physician service maldistribution and supply-sensitive care on the appropriateness of cardiac health service use.
Keywords: Canada, Cardiovascular disease, Noninvasive diagnostic testing, Physician supply, Regional variations
Abstract
HISTORIQUE :
L’utilisation des services de santé semble être directement proportionnelle à la disponibilité des ressources, mais aucune étude n’a porté sur l’interaction entre la disponibilité des services de santé, le fardeau des maladies cardiovasculaires et l’utilisation des services de santé. La présente étude visait à examiner le lien entre l’évaluation cardiovasculaire et l’intensité de la prise en charge, la disponibilité de médecins et le fardeau des maladies cardiovasculaires au sein de la population canadienne.
MÉTHODOLOGIE :
La présente étude transversale en population se composait de citoyens adultes de l’Ontario en 2001. Chez chaque patient, les auteurs ont mesuré l’évaluation cardiaque et l’intensité de la prise en charge comme principale mesure d’issue, composée d’au moins l’un des services suivants : test cardiaque non effractif, coronarographie et utilisation de statine (seulement chez les patients de 65 ans et plus). La mortalité était la mesure d’issue secondaire. Les auteurs ont mesuré le fardeau des maladies cardiovasculaires et la disponibilité de cardiologues et de médecins de premier recours à l’échelle régionale (par comté). Ils ont rajusté les analyses selon l’âge et le sexe au moyen de la régression de Poisson, compte tenu de la concentration régionale.
RÉSULTATS :
La disponibilité régionale de cardiologues per capita variait de plus du simple au double entre les régions, mais était inversement proportionnelle au fardeau des maladies cardiovasculaires (r=−0,34, P=0,01). La disponibilité de médecins de premier recours était relativement uniforme entre les régions. Les résidents des régions comptant plus de cardiologues étaient plus susceptibles de recevoir une forme d’intervention cardiaque (RR=1,074, 95 % IC 1,066 à 1,082 par cardiologue supplémentaire pour une population de 100 000 habitants). Ceux des régions comptant plus de médecins de premier recours étaient également plus susceptibles de subir des tests cardiaques non effractifs (RR=1,056, 95 % IC 1,051 à 1,061 par tranche de six médecins de premier recours pour une population de 100 000 habitants). Cependant, l’intensité de la prestation de services de santé cardiaque n’était ni reliée au fardeau régional des maladies cardiovasculaires ni à un meilleur taux de survie.
CONCLUSIONS :
Le décalage entre la disponibilité de médecins et le fardeau des maladies cardiaques peut expliquer que l’utilisation des services de santé cardiovasculaire ne concorde pas avec le fardeau des maladies cardiovasculaires et la mortalité au sein de la population. Ces résultats soulignent l’importance d’une mauvaise distribution des services des médecins et des soins selon les ressources sur l’adéquation de l’utilisation des services de santé cardiaque.
Among most industrialized countries, policy makers and system planners assume that medical service intensity will be delivered in accordance with the medical needs of the population (1–3). In some jurisdictions, ‘needs-based’ funding models have been developed and implemented to help guide health service resource allocation to regions with the greatest medical disease burden. For example, Ontario policy makers and health care system planners used acute coronary syndrome hospitalization data to estimate volume requirements of coronary angiography, percutaneous coronary intervention (PCI) and coronary artery bypass surgery capacity across regions (4). Similarly, in the United Kingdom, policy makers implemented needs-based funding models to estimate the cardiovascular resource requirements across regions, as well as for general national health services funding (1).
Notwithstanding the existence of such funding models, available evidence in Canada, like elsewhere, has demonstrated marked regional variations in the use of cardiovascular health services in magnitudes that exceed those expected from variations in cardiovascular disease burden and illness severity alone (5–7). While onsite procedural hospital capacity remains an important determinant of coronary invasive service use (8,9), available evidence has demonstrated marked variations in the use of noninvasive and medical services in Canada and the United States (7,10,11). Given the importance of physician decision making as a determinant of cardiovascular specialty service use (12), one may reasonably hypothesize that variations in physician supply play a more important determining factor in accounting for inter-regional cardiovascular referral and management disparities than differences in cardiovascular disease burden (7,13,14). Moreover, a mismatch between physician supply and cardiovascular disease burden may also have downstream repercussions on health outcome disparities, should a disproportionate intensity of cardiovascular services be allocated to lower- rather than higher-risk communities.
The objective of the present study was to examine the relationship between physician supply, health service use and cardiovascular disease burden across Ontario. Canada is an ideal country to examine, given that its publicly funded universal health care system is designed to ensure that all citizens have equal access to necessary medical services without out-of-pocket payments or user fees (15). Consequently, the alignment between service supply, service use and disease burden should, in theory, be greater than that observed elsewhere, especially among those countries whose health care systems have parallel private funding options in place. Nonetheless, we hypothesized that cardiovascular health service intensity would correlate poorly with cardiovascular disease burden as a result of a service maldistribution of cardiology specialty providers in the population.
METHODS
System context and study population
The present retrospective, population-based study comprised the Ontario adult population 20 years of age and older. Ontario is the largest province in Canada, consisting of 11.9 million people, and is subdivided into 17,824 census dissemination areas (DAs) and 50 counties. The median population size per DA is 415 adults (20 years of age and older), and ranges from five to 8365 adults; the corresponding population per county ranges from 9462 to 1.98 million adults. In Ontario, the use of tertiary cardiovascular services (ie, coronary angiography, PCI and coronary artery bypass surgery) is regionalized, but such service requirements are projected to reflect existing variations in cardiovascular disease burden across communities (4).
Data sources
Patient records were linked across multiple health administrative databases using a unique encrypted study number to protect patient confidentiality. Information regarding noninvasive testing and physician visits was obtained through medical claims data from the Ontario Health Insurance Plan (OHIP). OHIP captures all outpatient claims throughout Ontario, but does not capture services provided in alternative payment plans (5% of total claims for Ontario). The Registered Persons Database was used to identify information related to the patient residence (postal codes) and mortality during the 2001 calendar year. Cardiac hospitalizations and coronary angiography were identified using hospital discharge abstracts from the Canadian Institutes for Health Information database. Provider specialty was obtained from the Institute for Clinical Evaluative Sciences Physician Database (IPDB) (16). The IPDB contains information on physician demographics, specialty training and practice location. The quality of data in the IPDB was validated against the Ontario Physician Human Resource Data Centre database, which verifies this information through periodic telephone interviews with physicians. Drug prescription data were obtained from the Ontario Drug Benefit Program database. The postal code conversion file was used to link postal codes to DAs, and official 2001 census data were used to ascertain the DA population (17). The study received ethics approval at Sunnybrook and Women’s College Health Sciences Centre (Toronto, Ontario).
Physician supply
Physicians self-designated themselves as primary care providers (ie, general or family practitioners) or cardiologists in the IPDB survey. The specialty assignment of ‘cardiology’ was based on ‘functional specialty’, which reflects what the physician actually does in her/his practice. Functional specialty was validated by physician self-report. Consequently, internists who spend most of their time providing cardiac care would be classified as ‘cardiologists’ for study purposes. For each county, in-area head counts of primary care and cardiology physicians were converted to full-time equivalents using a Health Canada formula (16,18). These were adjusted for population travel across county boundaries based on claims for cardiac evaluation and management visits using previously published methods (19). Rates of physician supply were adjusted for age and sex, and were expressed per 100,000 county residents.
Cardiac disease burden
Cardiac disease burden was estimated using age- and sex-specific county-level rates of cardiac hospitalizations for acute myocardial infarction (International Classification of Diseases, 9th revision [ICD-9], code 410), unstable angina (ICD-9 codes 411 and 413) and congestive heart failure (ICD-9 code 428) using the most responsible diagnosis from hospital discharge abstracts in 2000 (the year preceding the assessment of noninvasive testing). Hospitalizations were geographically attributed to the patient’s county of residence based on postal code data. Hospitalization data provides a surrogate for the ‘expressed’ health service needs and disease burden prevalence of a population, and have been used as markers of population need in other studies (9,11,20,21). As a further assessment of validity, county-specific cardiac hospitalization rates in 2000 were found to be positively correlated with the prevalence of county-specific, self-reported cardiovascular risk factors (ie, defined by the presence of smoking, hypertension, diabetes and heart disease), as obtained from the 1996 Ontario Health Survey (www.apheo.ca/indicators) (r=0.59, P<0.0001).
Cardiac health service intensity
Cardiac evaluation and management intensity served as our main outcome variable; it was defined as the use of noninvasive services, invasive services or medical therapy (3-hydroxy-3-methyl-glutaryl coenzyme A reductase inhibitors [statins]), and was measured at the individual patient level. The use of noninvasive tests (echocardiography, graded exercise treadmill testing [hereafter termed ‘stress testing’] and nuclear perfusion imaging) was identified using the professional component (ie, diagnostic interpretation) of physician claims data between January 1, 2001, and December 31, 2001. Multiple tests per day on the same patient for any diagnostic service were excluded. Codes for echocardiography included one- or two-dimensional studies with or without Doppler examination (G561, G562, G567, G568, G571, G572, G575). Stress tests were identified by G319, while perfusion imaging tests included exercise or dipyridamole myocardial perfusion imaging with or without single photon emission computed tomography, using either sestamibi or thallium as its radiotracer (J607, J608, J609, J666, J807, J808, J809, J866). Such codes have previously been used to examine noninvasive cardiac testing in Ontario (11). Given that perfusion imaging tests may be conducted over one or more consecutive days, a two-day window was applied on either side of the date of a nuclear imaging claim to avoid duplicate counting. A similar two-day window was applied to stress testing to differentiate isolated stress tests from those with concomitant perfusion. The use of invasive testing (ie, coronary angiography) was derived using OHIP procedure codes (11).
The use of statins (among patients 65 years of age and older) served as our indicator of medical therapy for three reasons. First, statins represent evidence-based pharmacotherapy associated with irrefutable survival benefits among patients with cardiovascular diseases (22). Second, their indications are predicated on estimates of cardiovascular risk rather than symptoms per se, which should, in theory, positively correlate with cardiovascular disease burden (see below) if used appropriately (23). Third, they are well-tolerated and among the most frequently prescribed cardiovascular drugs in Canada (24).
Mortality
Mortality in 2001 served as a secondary outcome measure, and was measured using individual-level data.
Statistical analyses
Rates of noninvasive and invasive testing, physician visits and cardiac admissions were computed as the number of tests or prescriptions divided by the corresponding population. All rates were directly standardized according to the age and sex distribution of the Ontario adult population. Regional (ie, county) variation was expressed using the interquartile ratio (IQR) and the coefficient of variation. Univariate associations between per capita rates of physician supply, noninvasive and invasive testing, statin use and cardiac hospitalizations were expressed using the coefficient of determination, unweighted for county population.
To examine the relationship between individual cardiac evaluation and management intensity, the regional supply of primary care providers and cardiologists, and the regional cardiac disease burden, an overdispersed multilevel Poisson regression model was used, with an offset to incorporate the stratum-specific population (25). Separate models were run for echocardiography, stress or perfusion imaging, coronary angiography and statin use (patients 65 years of age and older). The unit of analysis was the five-year age, sex, DA stratum for computational efficiency; the average stratum size was 15 people. Because population-based rates of invasive and noninvasive testing were low, most strata had one or no events. The dependent variable was the stratum-specific count of tests or prescriptions during 2001. Independent variables included age group and sex (and their interactions), regional per capita supply of generalists and cardiologists, as well as regional age- and sex-specific cardiac admission rates for acute myocardial infarction, chronic heart failure or angina. In the models, cardiologist and primary care supply, as well as cardiac disease burden, were scaled to assess the effect of similar increments in supply, specifically, one-half the interquartile range for their respective specialties (one cardiologist and six primary care physicians per 100,000). Point estimates and 95% CI for RR were obtained by exponentiating the corresponding regression parameters. Similar models were used to study mortality. Variance overdispersion was incorporated in the estimates of all standard errors to account for nesting of individuals within age- and sex-adjusted DA strata, as well as multiple tests to the same individual (25). All tests were performed at the 5% level of significance and were two-sided.
RESULTS
Baseline characteristics
Table 1 summarizes descriptive statistics and variations in the rates across counties for physician supply, cardiac management and hospitalization rates throughout Ontario. Intercounty variations were greater for cardiologist (IQR=1.9) than for primary care physician (IQR=1.2) supply. The IQR ranged from 1.2 to 1.6 for cardiac evaluation and management intensity, and was similar for both noninvasive and invasive tests, but lowest for statin use. Intercounty variations in cardiac disease burden ranged from 1.4 to 1.7, and were slightly higher than for cardiac evaluation and management intensity.
TABLE 1.
Baseline summary characteristics for county-specific, age- and sex-adjusted rates of physician supply, noninvasive and invasive cardiac testing, cardiac hospitalization and statin use in Ontario
| Characteristic | Total, n* | Q1 | Median | Q3 | Interquartile ratio | Extremal ratio | CV |
|---|---|---|---|---|---|---|---|
| Physician supply per 100,000 in 2001 | |||||||
| Primary care provider | 8257 | 61.9 | 68.2 | 75.1 | 1.2 | 2.1 | 15.7 |
| Cardiologist | 434 | 1.9 | 3.1 | 3.7 | 1.9 | 10.7 | 41.6 |
| Evaluation and management intensity per 1000 in 2001 | |||||||
| Echocardiography | 286,679 | 22.1 | 27.5 | 34.2 | 1.5 | 5.4 | 30.8 |
| Stress or perfusion imaging | 284,525 | 25.4 | 30.6 | 36.1 | 1.4 | 7.6 | 29.5 |
| Any noninvasive testing | 571,204 | 48.4 | 55.7 | 70.2 | 1.5 | 6.4 | 28.8 |
| Coronary angiography | 46,647 | 4.3 | 5.2 | 6.8 | 1.6 | 3.1 | 30.3 |
| Any invasive or noninvasive test | 617,851 | 53.6 | 63.9 | 75.6 | 1.4 | 5.9 | 27.8 |
| Statin use (in adults ≥65 years of age) | 368,317 | 205.5 | 223.6 | 243.7 | 1.2 | 1.8 | 12.4 |
| Any management or evaluation (in adults ≥65 years of age) | 592,324 | 327.6 | 360.4 | 406.9 | 1.2 | 2.6 | 16.4 |
| Cardiac hospitalization per 1000 in 2000 | |||||||
| Acute myocardial infarction hospitalization | 24,350 | 2.7 | 3.0 | 3.6 | 1.4 | 3.0 | 25.7 |
| Angina hospitalization | 25,599 | 2.8 | 3.7 | 4.8 | 1.7 | 6.7 | 35.3 |
| Congestive heart failure hospitalization | 21,503 | 2.3 | 3.0 | 3.4 | 1.4 | 3.0 | 25.6 |
| Any cardiac hospitalization | 71,421 | 7.9 | 9.9 | 11.3 | 1.4 | 2.9 | 25.7 |
Noninvasive cardiac testing and physician visits reflect population rates for the year 2001, while cardiac hospitalizations correspond to population rates for 2000.
*Not adjusted for population size. CV Coefficient of variation (SD/mean); Q1, Q3 First, third quartiles
Correlations between age- and sex-adjusted physician supply, cardiac evaluation and management and cardiac hospitalization rates
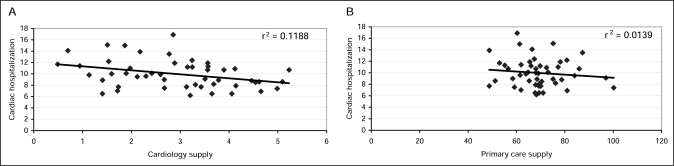
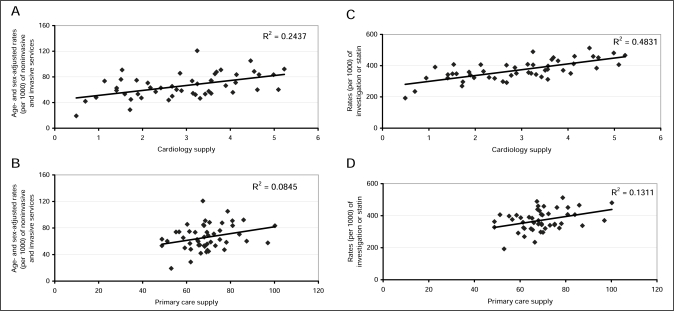
Univariate analyses showed that cardiac hospitalizations were inversely correlated with cardiology supply (r=−0.34, P=0.01) but unrelated to supply of primary care supply (Figure 1). Regional intensity of cardiac testing and combined testing and statin use were strongly correlated with cardiology supply (R2=0.24 and R2=0.48, respectively) (Figures 2A and 2B) and weakly associated with primary care supply (R2=0.08 and R2=0.13, respectively) (Figures 2C and 2D) across regions. In contrast, cardiac testing and statin intensity were not related to the prevalence of cardiovascular disease across jurisdictions (r2=0.008).
Figure 1).
The relationship between age- and sex- adjusted cardiovascular disease burden (ie, cardiac hospitalization per 100,000) and physician supply (per 100,000). A The relationship between the rates of cardiac hospitalization in 2000 and cardiology supply in 2001. B The relationship between the rates of cardiac hospitalizations in 2000 and primary care supply
Figure 2).
The relationships between regional age- and sex-adjusted rates of cardiac investigations (per 1000) and physician supply (per 100,000). A The relationship between the rates of cardiac investigations (echocardiography, imaging and nonimaging stress tests and coronary angiography) and cardiology supply in 2001. B The relationship between the rates of cardiac investigations and primary care supply in 2001. C The relationship between combined regional cardiac testing and statin intensity and cardiology supply in 2001 among patients 65 years and older. D The relationship between combined regional cardiac testing and statin intensity and primary care supply in 2001 among patients 65 years and older
Predictors of cardiac evaluation and management
Table 2 reports the relationship between cardiac evaluation and management intensity, physician supply and cardiac disease burden from multivariate Poisson regression models. Cardiologist supply was significantly associated with all outcomes (P<0.001), and remained among the strongest determinant of an individual’s cardiac testing and statin use after accounting for age, sex and regional cardiac burden. Adjusted RR for any form of cardiac investigation was 1.074 (95% CI 1.066 to 1.082), and ranged from 1.03 (95% CI 1.02 to 1.04) for coronary angiography to 1.16 (95% CI 1.15 to 1.17) for echocardiography per cardiologist per 100,000 population. Primary care physician supply was significantly associated with an individual’s noninvasive testing (RR=1.056, 95% CI 1.051 to 1.061 per six primary care physicians per capita), but not with invasive testing or statin use. In contrast, cardiac hospitalizations were weakly associated with cardiovascular evaluation and management, where significant.
TABLE 2.
The relationship between regional physician supply, cardiac hospitalization rates, cardiac evaluation and management intensity in multivariate analyses in Ontario
| Outcome and predictors | Adjusted RR | 95% CI | P |
|---|---|---|---|
| Echocardiography | |||
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.07 | 1.07–1.08 | <0.001 |
| Cardiology supply (per 100,000 adult population) | 1.16 | 1.15–1.17 | <0.001 |
| Acute myocardial infarction hospitalizations (per 200 adult population) | 1.00 | 0.98–1.01 | 0.685 |
| Angina hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.01 | 0.003 |
| Congestive heart failure hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.01 | 0.008 |
| Stress or perfusion imaging | |||
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.04 | 1.04–1.05 | <0.001 |
| Cardiology supply (per 100,000 adult population) | 1.05 | 1.05–1.06 | <0.001 |
| Acute myocardial infarction hospitalizations (per 200 adult population) | 1.02 | 1.01–1.04 | 0.005 |
| Angina hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.272 |
| Congestive heart failure hospitalizations (per 1000 adult population) | 0.99 | 0.99–1.00 | <0.001 |
| Any noninvasive test | |||
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.06 | 1.05–1.06 | <0.001 |
| Cardiology supply (per 100,000 adult population) | 1.10 | 1.10–1.11 | <0.001 |
| Acute myocardial infarction hospitalizations (per 200 adult population) | 1.01 | 1.00–1.02 | 0.065 |
| Angina hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.220 |
| Congestive heart failure hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.076 |
| Coronary angiography | |||
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.00 | 0.99–1.00 | 0.217 |
| Cardiology supply (per 100,000 adult population) | 1.03 | 1.02–1.04 | <0.001 |
| Acute myocardial infarction hospitalizations (per 200 adult population) | 0.98 | 0.95–1.00 | 0.066 |
| Angina hospitalizations (per 1000 adult population) | 1.01 | 1.01–1.02 | <0.001 |
| Congestive heart failure hospitalizations (per 1000 adult population) | 0.99 | 0.98–0.99 | <0.001 |
| Any cardiac investigation | |||
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.05 | 1.05–1.06 | <0.001 |
| Cardiology supply (per 100,000 adult population) | 1.10 | 1.09–1.10 | <0.001 |
| Acute myocardial infarction hospitalizations (per 200 adult population) | 1.01 | 1.00–1.02 | 0.120 |
| Angina hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.026 |
| Congestive heart failure hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.004 |
| Statin use | |||
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.00 | 1.00–1.01 | 0.071 |
| Cardiology supply (per 100,000 adult population) | 1.06 | 1.06–1.07 | <0.001 |
| Acute myocardial infarction hospitalizations (per 200 adult population) | 1.01 | 1.00–1.02 | 0.004 |
| Angina hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | >0.99 |
| Congestive heart failure hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.223 |
| Any cardiac investigation or statin use* | |||
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.02 | 1.01–1.02 | <0.001 |
| Cardiology supply (per 100,000 adult population) | 1.07 | 1.07–1.08 | <0.001 |
| Acute myocardial infarction hospitalizations (per 200 adult population) | 1.01 | 1.00–1.02 | 0.107 |
| Angina hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.810 |
| Congestive heart failure hospitalizations (per 1000 adult population) | 1.00 | 1.00–1.00 | 0.075 |
Multivariate analyses were also adjusted for age, sex and an age-sex interaction. Physician supply and noninvasive testing rates refer to the year 2001. Cardiac hospitalizations correspond to admissions for angina, acute myocardial infarction or congestive heart failure during 2000.
*Among patients 65 years of age and older
Predictors of mortality
While strongly associated with cardiac disease burden, as expected, physician supply, cardiac testing and statin intensity were not significant predictors of individual mortality (Table 3).
TABLE 3.
The relationship between regional physician supply, cardiac hospitalization rates, cardiac evaluation, management intensity and mortality in multivariate analyses in Ontario
| Predictor | Adjusted RR | 95% CI | P |
|---|---|---|---|
| Primary care supply (per 6 primary care physicians per 100,000 adult population) | 1.00 | 0.99–1.01 | 0.97 |
| Cardiology supply (per 100,000 adult population) | 0.99 | 0.97–1.00 | 0.12 |
| Echocardiography (per 100 adult population) | 1.00 | 0.99–1.01 | 0.50 |
| Stress or perfusion imaging (per 100 adult population) | 1.00 | 0.98–1.01 | 0.84 |
| Angiography (per 100 adult population) | 1.03 | 1.00–1.06 | 0.07 |
| Statin use (per 100 patients ≥65 years of age) | 1.00 | 1.00–1.01 | 0.43 |
| Cardiac hospitalizations (per 100 adult population) | 1.04 | 1.03–1.06 | <0.001 |
Multivariate analyses were also adjusted for age, sex and an age-sex interaction. Physician supply and noninvasive testing rates refer to years 2001. Cardiac hospitalizations correspond to admissions for angina, acute myocardial infarction or congestive heart failure during the year 2000. The model for statin use was conducted separately, and applied to patients 65 years of age and older. There was no significant relationship between evaluation and management intensity (ie, any invasive test, noninvasive test or statin) and mortality among patients ages 65 years and older (Adjusted RR 1.00, 95% CI 1.00–1.00, P=0.77)
DISCUSSION
Our study demonstrated significant regional variations in cardiology supply throughout Ontario that correlated inversely with cardiac disease burden, but nevertheless remained among the strongest determinants of an individual’s cardiovascular evaluation and management intensity after accounting for all baseline factors.
If one assumes that cardiovascular disease burden appropriately reflects the expressed health service medical needs across populations, our study was the first to demonstrate poor concordance between the supply of cardiovascular service providers and cardiovascular population needs. Such findings are consistent with other studies (26,27), which have demonstrated a maldistribution between physician supply and health service needs across Canada. Moreover, previous work by our group (28) has also demonstrated a mismatch between cardiovascular tertiary hospital services and population needs, as estimated using neighbourhood socioeconomic status as a surrogate of cardiovascular disease burden and illness severity.
Our study demonstrated at best only a modest correlation between health service use and cardiovascular disease burden. For example, the relationship between pre-existing cardiovascular hospitalizations and cardiovascular service intensity was notably weaker than the associations between cardiology supply and testing intensity. The strong positive relationship between angina hospitalizations and coronary angiography, however, was one exception, and might have been attributable to the evolution of clinical trial evidence favouring modest outcome benefits associated with early invasive coronary management among patients hospitalized with acute coronary syndromes (29). The lack of a relationship between health service intensity and cardiac disease burden may explain why cardiovascular management and treatment intensity bore little relationship with mortality.
Our results reaffirm the importance of supply factors on physician decision-making behaviours in Canada (8), like elsewhere (9,13,14), and underscore the fact that supply may overshadow medical needs as a determinant of health service use in the population (5,30,31).
The extent to which physician decision making reflected appropriate or inappropriate evaluation and management behaviour cannot be ascertained from the present study. In Ontario, cardiovascular providers often own and operate noninvasive diagnostic services, such as echocardiography and stress test laboratories. Patients may receive noninvasive diagnostic services through direct referrals from primary care providers or through a consulting cardiologist who uses his/her own facility (or others’) to conduct further evaluation when necessary. Although fee-for-service systems provide potential financial incentives to those who ‘self-refer’ patients to their own diagnostic laboratories for evaluation, the indications for tests may not necessarily be inappropriate. Indeed, available evidence has demonstrated that inappropriate indications comprise a low prevalence of the total case volumes referred for cardiac evaluation (32). In short, geographical variations in the use of supply-sensitive care may largely be attributable to differences in referral propensity among discretionary rather than inappropriate or appropriate indications (12).
Our study was not designed to explore the underlying reasons for the health service mismatch between physician service supply and cardiovascular disease burden. Nonetheless, two hypotheses exist. First, physicians’ personal and social values favour practice locations in urban and/or medical service supply-intensive regions, regardless of population needs – an effect that may partially be overcome through explicit recruitment and retention strategies (33). Second, population health service demands may be driven by perceptions more than by true medical needs (34).
Canada’s universal health care system prohibits parallel private funding streams. One may reasonably hypothesize that the additional market-driven forces that exist in other first-payer private health care systems (eg, United States) may further erode the alignment between service supply and population needs, especially given that disease burden correlates inversely with the socioeconomic affluence of a community (35). Therefore, the poor alignment between service supply and medical needs observed in our study is likely conservative compared with other international jurisdictions.
The integration of ‘needs-based’ modelling into health system policy decision making is becoming more frequent in many industrialized nations worldwide (1,4,36–38). Our study illustrates the significance of physician supply factors and underscores the importance of alignment between physician supply and population need when projecting future cardiovascular resources. Conversely, resource allocation processes, which do not take into account physician supply, may result in suboptimal resource use in the population. In the absence of appropriate supply-need resource alignment, policy makers may require the implementation of referral networks between high- and low-supply regions to mitigate physician shortfalls and unmet cardiovascular needs. Other strategies may include information technology (eg, telemedicine), which may allow for more remote access to provider and procedural services (39,40). However, others may argue that service maldistribution may not necessitate specific reallocation initiatives – that it will equilibrate passively through increases in physician supply. Nonetheless, available evidence has suggested otherwise (41).
Our study has several limitations. First, census DAs reflect geopolitical boundaries and were not designed to demarcate health service areas, which provide a more relevant regional unit of analysis by optimally aligning resource supply and use (42). Nonetheless, these methodological limitations would have biased our results toward the null. Second, cardiac disease burden, by design, was measured using regional- rather than individual-level cardiac-specific hospitalizations to estimate the ‘expressed’ population cardiac need. While cardiac health service intensity was measured at the individual level, more rigorous risk adjustment might have altered our results. However, the predominant variations in population clinical status are correlated with age, sex and regional burden of cardiac disease. Moreover, county-specific cardiac hospitalization rates correlated well with self-reported cardiovascular risk factors using previous population health survey data. While better risk adjustment may explain the relationship between supply and use, it is unlikely to explain the mismatch between individual use and population disease burden (43). In addition, our data were five years old at the time of writing, and cardiac service supply and population needs might have changed in the interim. Moreover, the regional allocation and delivery of cardiac services in Ontario may continue to evolve through the development and implementation of Local Health Integration Networks over the next several years. Nonetheless, future alignment between service capacity and population needs remains speculative. Finally, our data were limited to Ontario. However, Ontario has the largest population size of any province in Canada, consisting of over 10,000,000 people, including 10,000 physicians. Moreover, the relationship between health service supply and use has been demonstrated to exist throughout many jurisdictions outside of Ontario, both within Canada and beyond. Accordingly, we have no reason to believe that our results would not be adaptable to other Canadian jurisdictions.
CONCLUSIONS
Physician supply maldistribution may explain the poor concordance between cardiovascular service use and cardiovascular disease burden in Ontario. Such results underscore the potential importance of physician service maldistribution and supply-sensitive care on the appropriateness of cardiac health service use in Canada and elsewhere.
Footnotes
FUNDING: Dr Alter is a Career Scientist with the Heart and Stroke Foundation of Ontario. This work was supported, in part, by a grant by the Heart and Stroke Foundation of Canada. The Institute for Clinical Evaluative Sciences is supported, in part, by a grant from the Ontario Ministry of Health. The results, conclusions and opinions are those of the authors, and no endorsement by the Ministry or the Institute is intended or should be inferred.
REFERENCES
- 1.Martin RM, Hemingway H, Gunnell D, Karsch KR, Baumbach A, Frankel S. Population need for coronary revascularisation: Are national targets for England credible? Heart. 2002;88:627–33. doi: 10.1136/heart.88.6.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pink GH, Montgomery C, Aird C, Vimr MA, Morgan CD. Developing guidelines for allocating catheterization laboratory resources: Lessons from an Ontario Consensus Panel. Consensus Panel on Cardiac Catheterization Laboratory Services in Ontario and the Steering Committee of the Cardiac Care Network of Ontario. Can J Cardiol. 2000;16:49–57. [PubMed] [Google Scholar]
- 3.Stolk EA, Poley MJ. Criteria for determining a basic health services package. Recent developments in The Netherlands. Eur J Health Econ. 2005;6:2–7. doi: 10.1007/s10198-004-0271-0. [DOI] [PubMed] [Google Scholar]
- 4.The Cardiac Care Network of Ontario. Consensus Panel on Target Setting – final report and recommendations. Mar, 2004.
- 5.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–87. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 6.Pilote L, Merrett P, Karp I, et al. Cardiac procedures after an acute myocardial infarction across nine Canadian provinces. Can J Cardiol. 2004;20:491–500. [PubMed] [Google Scholar]
- 7.Wennberg DE, Birkmeyer JD, editors. The Dartmouth atlas of cardiovascular health care. Centre for the Evaluative Clinical Sciences, Dartmouth Medical School. 1999:11–40. [PubMed] [Google Scholar]
- 8.Alter DA, Naylor CD, Austin PC, Tu JV. Long-term MI outcomes at hospitals with or without on-site revascularization. JAMA. 2001;285:2101–8. doi: 10.1001/jama.285.16.2101. [DOI] [PubMed] [Google Scholar]
- 9.Wennberg D, Dickens J, Jr, Soule D, et al. The relationship between the supply of cardiac catheterization laboratories, cardiologists and the use of invasive cardiac procedures in northern New England. J Health Serv Res Policy. 1997;2:75–80. doi: 10.1177/135581969700200204. [DOI] [PubMed] [Google Scholar]
- 10.Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:374–9. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alter DA, Stukel TA, Newman A. Proliferation of cardiac technology in Canada: A challenge to the sustainability of Medicare. Circulation. 2006;113:380–7. doi: 10.1161/CIRCULATIONAHA.105.560466. [DOI] [PubMed] [Google Scholar]
- 12.Guadagnoli E, Landrum MB, Normand SL, et al. Impact of underuse, overuse, and discretionary use on geographic variation in the use of coronary angiography after acute myocardial infarction. Med Care. 2001;39:446–58. doi: 10.1097/00005650-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Davis P, Gribben B, Scott A, Lay-Yee R. The “supply hypothesis” and medical practice variation in primary care: Testing economic and clinical models of inter-practitioner variation. Soc Sci Med. 2000;50:407–18. doi: 10.1016/s0277-9536(99)00299-3. [DOI] [PubMed] [Google Scholar]
- 14.Wennberg JE, Barnes BA, Zubkoff M. Professional uncertainty and the problem of supplier-induced demand. Soc Sci Med. 1982;16:811–24. doi: 10.1016/0277-9536(82)90234-9. [DOI] [PubMed] [Google Scholar]
- 15.Canada Health Act. 1984: Section 10.
- 16.Chan BTB, Schultz SE.Supply and utilization of general practitioner and family physician services in Ontario. Institute for Clinical Evaluative SciencesAugust2005
- 17.Wilkins R. Use of postal codes and addresses in the analysis of health data. Health Rep. 1993;5:157–77. [PubMed] [Google Scholar]
- 18.Ontario Case Costing Initiative. 2005 < www.occp.com> (Version current at January 24, 2008)
- 19.Goodman DC, Fisher ES, Bubolz TA, Mohr JE, Poage JF, Wennberg JE.Benchmarking the US physician workforce. An alternative to needs-based or demand-based planning JAMA 19962761811–7.(Erratum in 1997;277:966) [DOI] [PubMed] [Google Scholar]
- 20.Rockett IR, Putnam SL, Jia H, Chang CF, Smith GS. Unmet substance abuse treatment need, health services utilization, and cost: A population-based emergency department study. Ann Emerg Med. 2005;45:118–27. doi: 10.1016/j.annemergmed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Cornell SJ, Chilcott JB, Brennan A. Is it feasible to plan secondary care services for coronary heart disease rationally? A quantified modelling approach for a UK Health Authority. J Epidemiol Community Health. 2001;55:521–7. doi: 10.1136/jech.55.7.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allen Maycock CA, Muhlestein JB, Horne BD, et al. Intermountain Heart Collaborative Study Statin therapy is associated with reduced mortality across all age groups of individuals with significant coronary disease, including very elderly patients. J Am Coll Cardiol. 2002;40:1777–85. doi: 10.1016/s0735-1097(02)02477-4. [DOI] [PubMed] [Google Scholar]
- 23.Manuel DG, Tanuseputro P, Mustard CA, et al. The 2003 Canadian recommendations for dyslipidemia management: Revisions are needed CMAJ 20051721027–31.(Erratum in 2005;173:133) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.2005/06 Report card for the Ontario drug benefit program. <www.health.gov.on.ca/english/public/pub/ministry_reports/odb_report05/odb_rep_05_06.pdf > (Version current at February 19, 2008).
- 25.McCullagh P, Nelder JA. Generalized Linear Models. 2nd edn. New York: CRC Press; 1989. [Google Scholar]
- 26.Coyte PC, Catz M, Stricker M. Distribution of physicians in Ontario. Where are there too few or too many family physicians and general practitioners? Can Fam Physician. 1997;43:677–83. 733. [PMC free article] [PubMed] [Google Scholar]
- 27.Krishnan V. A macro approach to the explanation of physician distribution in Canada. J Health Soc Policy. 1997;9:45–61. doi: 10.1300/j045v09n01_04. [DOI] [PubMed] [Google Scholar]
- 28.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999;341:1359–67. doi: 10.1056/NEJM199910283411806. [DOI] [PubMed] [Google Scholar]
- 29.Mehta SR, Cannon CP, Fox KA, et al. Routine vs selective invasive strategies in patients with acute coronary syndromes: A collaborative meta-analysis of randomized trials. JAMA. 2005;293:2908–17. doi: 10.1001/jama.293.23.2908. [DOI] [PubMed] [Google Scholar]
- 30.Lucas FL, Wennberg DE, Malenka DJ. Variation in the use of echocardiography. Eff Clin Pract. 1999;2:71–5. [PubMed] [Google Scholar]
- 31.Khaykin Y, Austin PC, Tu JV, Alter DA. Utilisation of coronary angiography after acute myocardial infarction in Ontario over time: Have referral patterns changed? Heart. 2002;88:460–6. doi: 10.1136/heart.88.5.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGlynn EA, Naylor CD, Anderson GM, et al. Comparison of the appropriateness of coronary angiography and coronary artery bypass graft surgery between Canada and New York State. JAMA. 1994;272:934–40. [PubMed] [Google Scholar]
- 33.Rabinowitz HK. Recruitment, retention, and follow-up of graduates of a program to increase the number of family physicians in rural and underserved areas. N Engl J Med. 1993;328:934–9. doi: 10.1056/NEJM199304013281307. [DOI] [PubMed] [Google Scholar]
- 34.Alter DA, Iron K, Austin PC, Naylor CD, SESAMI Study Group Socioeconomic status, service patterns, and perceptions of care among survivors of acute myocardial infarction in Canada. JAMA. 2004;291:1100–7. doi: 10.1001/jama.291.9.1100. [DOI] [PubMed] [Google Scholar]
- 35.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 36.Sheldon TA, Smith GD, Bevan G. Weighting in the dark: Resource allocation in the new NHS. BMJ. 1993;306:835–9. doi: 10.1136/bmj.306.6881.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Birch S, Chambers S. To each according to need: A community-based approach to allocating health care resources. CMAJ. 1993;149:607–12. [PMC free article] [PubMed] [Google Scholar]
- 38.Ontario Joint Policy and Planning Committee . Hospital funding report using 2002/2003 Data. Reference document RD10–8. Toronto: JPPC; Dec, 2004. [Google Scholar]
- 39.Gilman G, Lutzi CA, Daniels BK, Springer RF, Fye WB. The architecture of a mobile outreach echocardiography service. J Am Soc Echocardiogr. 2006;19:1526–8. doi: 10.1016/j.echo.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 40.Gruen RL, Weeramanthri TS, Bailie RS. Outreach and improved access to specialist services for indigenous people in remote Australia: The requirements for sustainability. J Epidemiol Community Health. 2002;56:517–21. doi: 10.1136/jech.56.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barnett JR. Where have all the doctors gone? (2). Intraurban trends: Changes in the geographic distribution of general practitioners in Auckland, 1980-7. N Z Med J. 1991;104:337–9. [PubMed] [Google Scholar]
- 42.Kay BJ. Describing health service areas: A methodological note on a summary indicator. Health Policy. 1985;5:133–41. doi: 10.1016/0168-8510(85)90027-2. [DOI] [PubMed] [Google Scholar]
- 43.Alter DA, Austin PC, Naylor CD, Tu JV. Factoring socioeconomic status into cardiac performance profiling for hospitals: Does it matter? Med Care. 2002;40:60–7. doi: 10.1097/00005650-200201000-00008. [DOI] [PubMed] [Google Scholar]