Abstract
Lifestyle modification should be an important part of therapy when hypertension is first diagnosed, with or without starting antihypertensive medication. The objective of the present study was to determine the extent to which recently diagnosed hypertensive Canadians modify their lifestyles and to examine how lifestyle modification relates to antihypertensive medication use. The longitudinal National Population Health Survey in Canada was conducted between 1994 and 2002, including five interview cycles at two-year intervals. During this time, 1281 persons reported hypertension in one cycle but not in the previous cycle, and were considered to be new hypertensive patients. Information collected included body mass index, smoking, alcohol consumption, physical inactivity and medication use. The main lifestyle modification associated with newly diagnosed hypertensive patients was smoking cessation, with a 18.6% relative risk reduction (RRR). A smaller change was seen in decreasing physical inactivity (RRR 6.2%). Persons not taking antihypertensive medication were not more likely to make lifestyle improvements. Paradoxically, new hypertensive patients showed increased numbers in the obese category (RRR –9.6%). Weight gain was especially marked among antihypertensive medication users and largest in female beta-blocker users (RRR –36.6%). If confirmed, this needs to be considered when prescribing to overweight people. In general, a greater effort is required to manage hypertension by lifestyle risk modification with or without antihypertensive medication.
Keywords: Hypertension, Lifestyle drugs
Abstract
Les modifications aux habitudes de vie devraient constituer une partie importante du traitement au premier diagnostic d’hypertension, qu’on entreprenne ou non des modifications antihypertensives. La présente étude visait à déterminer la mesure selon laquelle les Canadiens hypertensifs récemment diagnostiqués modifiaient leur mode de vie et à examiner en quoi ces modifications sont reliées à l’utilisation d’antihypertensifs. L’Enquête nationale longitudinale sur la santé de la population du Canada a eu lieu entre 1994 et 2002, y compris cinq cycles d’entrevue à intervalles de deux ans. Pendant cette période, 1 281 personnes ont déclaré faire de l’hypertension pendant un cycle, mais pas au cycle précédent, et ont été considérés comme de nouveaux patients hypertendus. L’information colligée incluait l’indice de masse corporelle, le tabagisme, la consommation d’alcool, l’inactivité physique et l’utilisation de médicaments. Les principales modifications aux habitudes de vie associées aux patients hypertendus nouvellement diagnostiqués étaient le renoncement au tabac, avec une réduction du risque relatif (RRR) de 18,6 %. On observait un changement plus faible à l’égard de la diminution de l’inactivité physique (RRR 6,2 %). Les personnes qui ne prenaient pas d’antihypertensifs n’étaient pas plus susceptibles d’améliorer leurs habitudes de vie. Paradoxalement, les nouveaux patients hypertendus présentaient des chiffres plus élevés dans la catégorie obésité (RRR –9,6 %). La prise de poids était particulièrement marquée chez les utilisateurs d’antihypertensifs et la plus élevée chez les femmes qui prenaient des bêta-bloquants (RRR –36,6 %). Si ces observations sont confirmées, il faudra en tenir compte au moment de prescrire des médicaments aux personnes ayant une surcharge pondérale. En général, il faut faire plus d’efforts pour prendre en charge l’hypertension par des modifications aux risques reliés aux habitudes de vie avec ou sans prise d’antihypertensifs.
Although hypertension is an important and common cardiovascular disease risk factor (1), it is not always taken seriously and is often poorly controlled (2,3). One reason is the lack of symptoms, and people may not be aware of having high blood pressure (2). The Canadian Heart Health Survey (1985 to 1992) found that while 22% of adults 18 to 74 years of age had high blood pressure, 43% of hypertensive persons were unaware of their hypertension, 22% were aware but untreated, 21% were treated but not controlled, and only 13% were treated and controlled (2).
Much of the risk associated with hypertension can be prevented by establishing effective blood pressure control (4,5). Although there is increasing emphasis on treatment by medication, lifestyle modification is an important part of hypertension management (6–12). Blood pressure increases with weight, excess alcohol consumption and sodium intake, but decreases with physical activity (4,13). Hypertension management recommendations include that the body mass index (BMI) remain lower than 25 kg/m2, alcohol consumption be limited and physical activity be increased. Diet modification should aim at attaining an optimum weight, and reducing sodium and saturated fat intake, as well as increasing fresh fruit, legumes, vegetables and low-fat dairy products (13–16).
Despite the beneficial effects of preventing hypertension and reducing blood pressure, designing and implementing effective strategies that lead to sustained lifestyle modification is difficult (8,13,16,17). To optimize existing strategies, we need to evaluate whether people alter existing risk factors after they first learn of their hypertension. Thus, the objectives of the present study were to determine the extent to which people recently diagnosed with high blood pressure modify their lifestyles, and the relationship, if any, between taking antihypertensive medication and lifestyle risk factor modification.
METHODS
The longitudinal National Population Health Survey (NPHS) in Canada consisted of five interview cycles at two-year intervals between 1994 and 2002. Data were collected by personal interview in the first cycle and telephone interviews subsequently. Over the years of data collection, 6.3% of the original population either died or were institutionalized, while 21.4% were lost because of various types of nonresponse, resulting in a population of 9538 respondents who completed all five interviews and were 20 years of age or older in 1994. The NPHS data were collected as a statistical sample of the Canadian population, but because the data used in the present study represent a small select portion of this sample, weighting was considered to be inappropriate.
The information available included demographic variables, self-reported hypertension and risk factors for hypertension, such as BMI, smoking, physical inactivity and chronic disease. Excess alcohol use was considered to be more than nine drinks per week for women and more than 14 drinks for men, as per Canadian recommendations (18). Medication use was based on the question, “What is the exact name of the medication that you took in the past two days?”, and the respondent was asked to read the name off the label of the container.
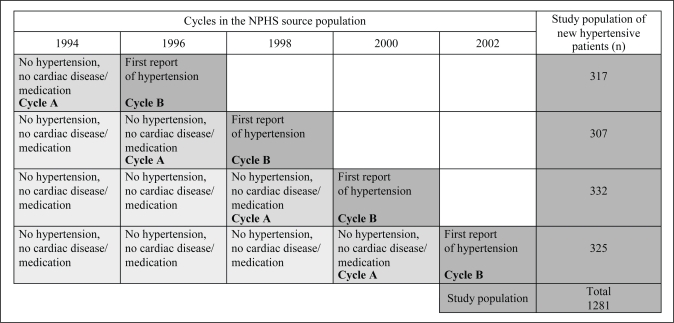
The newly diagnosed hypertensive study population consisted of respondents who had not reported diagnosis of, or treatment for, hypertension in any of the previous cycles, but then reported diagnosis with hypertension and/or received medication for hypertension in the next cycle (Figure 1). Persons with existing cardiac disease or who were receiving treatment for cardiac disease were excluded from the analysis. New hypertensive patients were identified in each interval between cycles and combined to form the newly hypertensive study population (Figure 1). The last cycle in which no hypertension could be identified was called cycle A, and the first cycle in which hypertension or its treatment was reported was called cycle B. Thus, 1281 new hypertensive patients were identified over the duration of the study.
Figure 1).
A respondent was judged to have no hypertension if there was no self-reported hypertension in the current and previous cycles, there was no reported antihypertensive medication use within two days before the interview in the current and previous cycles and there was no reported use of antihypertensive medications or diuretics within 30 days before the interview in the current and previous cycles. A respondent was judged to show evidence of hypertension if there was self-reported hypertension in cycle B, there was reported antihypertensive medication use within two days before the interview in cycle B, or there was reported use of antihypertensive medication or diuretics within 30 days before the interview in cycle B. NPHS National Population Health Survey
Analysis consisted of comparing cycle A with cycle B for changes in lifestyle factors for the 1281 new hypertensive patients. Data for each new hypertensive patient were treated as a matched pair when comparing before and after attributes, and McNemar’s test was used to determine statistical significance. Changes in proportion of lifestyle risk factors before and after hypertension were summarized by absolute risk reduction (ARR) and relative risk reduction (RRR). ARR was the difference in the proportions of persons with lifestyle risk factors before and after diagnosis of hypertension, and RRR was the proportion of ARR as a percentage of the presence of prehypertension risk factors.
RESULTS
The source population decreased from 6823 to 5586 patients over time (Table 1), because respondents with cardiac diseases and hypertension were removed as they were no longer at risk for new hypertension. Some differences in age distribution were seen between the source population and the 1281 newly diagnosed hypertensive study population. The new hypertensive patients showed few changes in lifestyle risk factors since the previous cycle (Table 2), with the greatest improvement occurring in smoking cessation (RRR 18.2%) and some improvement in physical activity (RRR 7.9%). Statistically significant changes in smoking cessation were seen in both sexes, and in older and younger age groups, but improvement in physical activity was seen mostly in the younger age group. Surprisingly, the proportions of obese persons (BMI greater than 30 kg/m2) tended to increase rather than decrease after the diagnosis of hypertension (Table 2).
TABLE 1.
Age and sex distribution of the newly diagnosed hypertensive and source populations
| 1994 | 1996 | 1998 | 2000 | 2002 | Total | |
|---|---|---|---|---|---|---|
| Source population, n (%) | ||||||
| Total | 6823 | 6498 | 6244 | 5928 | 5586 | – |
| Male sex | 3020 (44.3) | 2879 (44.3) | 2774 (44.4) | 2650 (44.7) | 2489 (44.6) | – |
| Female sex | 3803 (55.7) | 3619 (55.7) | 3470 (55.6) | 3278 (55.3) | 3097 (55.4) | – |
| Age <60 years | 5873 (86.1) | 5560 (85.6) | 5258 (84.2) | 4928 (83.1) | 4602 (82.4) | – |
| Age ≥60 years | 950 (13.9) | 938 (14.4) | 986 (15.8) | 1000 (16.9) | 984 (17.6) | – |
| Newly diagnosed hypertensive population, n (%) | ||||||
| Total | – | 317 | 307 | 332 | 325 | 1281 |
| Male sex | – | 136 (42.9) | 114 (37.1) | 131 (39.5) | 149 (45.9) | 530 (41.4) |
| Female sex | – | 181 (57.1) | 193 (62.9) | 201 (60.5) | 176 (54.2) | 751 (58.6) |
| Age <60 years | – | 211 (66.6) | 209 (68.1) | 212 (63.9) | 207 (63.7) | 839 (65.5) |
| Age ≥60 years | – | 106 (33.4) | 98 (31.9) | 120 (36.9) | 118 (36.3) | 442 (34.5) |
Note that the source population was the same from cycle to cycle except for the cumulative removal of existing hypertensive patients, while newly diagnosed hypertensive patients were different individuals from cycle to cycle and could therefore be added to form the study population
TABLE 2.
Proportion of study population with lifestyle risk factors before and after diagnosis of hypertension
| Presence of lifestyle risk factor
|
Presence of lifestyle risk factor
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before, n (%) | After, % | ARR, % | RRR, % | P | Before, n (%) | After, % | ARR, % | RRR, % | P | |
|
Overall | ||||||||||
| Smoking | 346 (27.0) | 22.1 | 4.9 | 18.2 | <0.001* | – | – | – | – | – |
| Excessive alcohol use | 77 (7.9) | 8.6 | –0.7 | –8.9 | 0.38 | – | – | – | – | – |
| Physical inactivity | 765 (60.9) | 56.1 | 4.8 | 7.9 | <0.01* | – | – | – | – | – |
| BMI ≥25 kg/m2 | 830 (66.0) | 68.2 | –2.2 | –3.3 | 0.04* | – | – | – | – | – |
| BMI ≥30 kg/m2 | 306 (24.3) | 27.1 | –2.8 | –11.5 | 0.02* | – | – | – | – | – |
|
By sex |
Men |
Women |
||||||||
| Smoking | 150 (28.4) | 23.2 | 5.2 | 18.3 | <0.001* | 196 (26.1) | 21.3 | 4.8 | 18.4 | <0.001* |
| Excessive alcohol use | 44 (10.8) | 11.9 | –1.1 | –10.2 | 0.23 | 33 (5.8) | 6.2 | –0.4 | –6.9 | 1.00 |
| Physical inactivity | 298 (58.3) | 52.9 | 5.4 | 9.3 | 0.05* | 467 (62.7) | 58.3 | 4.4 | 7.0 | 0.03* |
| BMI ≥25 kg/m2 | 385 (72.9) | 73.3 | –0.4 | –0.5 | 0.81 | 445 (60.9) | 64.5 | –3.6 | –5.9 | 0.01* |
| BMI ≥30 kg/m2 | 109 (20.6) | 22.7 | –2.1 | –10.2 | 0.12 | 197 (27.0) | 30.2 | –3.2 | –11.9 | 0.08 |
|
By age group |
Age <60 years |
Age ≥60 years |
||||||||
| Smoking | 271 (32.3) | 26.5 | 5.8 | 18.0 | <0.01* | 75 (17.0) | 13.8 | 3.2 | 18.8 | <0.01* |
| Excessive alcohol use | 62 (9.2) | 9.5 | –0.3 | –3.3 | 0.81 | 15 (4.9) | 6.8 | –1.9 | –38.8 | 0.11 |
| Physical inactivity | 507 (61.4) | 55.3 | 6.1 | 9.9 | <0.01* | 258 (60.0) | 57.8 | 2.2 | 3.7 | 0.50 |
| BMI ≥25 kg/m2 | 584 (70.6) | 73.5 | –2.9 | –4.1 | 0.02* | 246 (57.1) | 58.1 | –1.0 | –1.8 | 0.71 |
| BMI ≥30 kg/m2 | 221 (26.7) | 30.2 | –3.5 | –13.1 | <0.01* | 85 (19.7) | 21.2 | –1.5 | –7.6 | 1.00 |
Absolute risk reduction (ARR) is the absolute risk difference between before and after percentages, while the relative risk reduction (RRR) consists of the ARR as a percentage of the risk factor before hypertension diagnosis.
*Statistically significant at P≤0.05 as calculated by McNemar’s test. BMI Body mass index
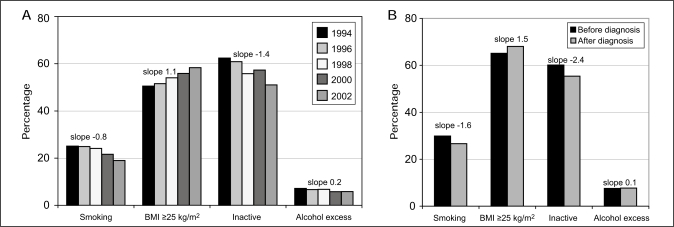
Age-standardized trends of the lifestyle risk factors (Figure 2) indicated that changes occurred not only in the hypertensive study population, but also in the source population. Thus, the proportions of smokers and physically inactive people decreased over the years, while the proportion of overweight people increased. The slopes entered above the clusters of bars show that, numerically, changes were greater for the newly diagnosed hypertensive population than for the source population, especially for smoking and physical inactivity. Of additional interest is that the newly diagnosed hypertensive population included more people who smoked and were overweight before being diagnosed with hypertension than the source population in any cycle. A more detailed look at differences between the source and hypertensive populations (Table 3) confirms these differences. For example, new hypertensive patients showed an increase in smoking cessation compared with the source population, with RRR in the hypertensive population ranging from 15.9% to 28.8% compared with 1.1% to 12.8% in the source population. Data in Table 3 also confirm that new hypertensive patients were more likely to be overweight in the cycle before diagnosis than source population patients at any time. In fact, the proportion of persons who were overweight before developing hypertension varied from 63% to 72%, while in the source population, the proportion varied from 46% to 52%.
Figure 2).
Trends in age-standardized rates of risk factors for source (A) and newly diagnosed hypertensive (B) populations. BMI Body mass index
TABLE 3.
Changes in lifestyle risk factors: comparing the source population with the study population
| Source population (%)
|
Study population (%)
|
Comparison of study and source populations
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proportion with lifestyle risk factor
|
ARR | RRR | Proportion with lifestyle risk factor
|
ARR | RRR | After* |
Before† |
|||||
| Before | After | Before | After | P CMH | Homogeneity | P CMH | Homogeneity | |||||
| Smoking | ||||||||||||
| 1994–96 | 27.7 | 27.4 | 0.3 | 1.1 | 27.0 | 22.7 | 4.3 | 15.9 | <0.005* | 0.56 | 0.20 | 0.92 |
| 1996–98 | 27.4 | 26.6 | 0.8 | 2.9 | 30.4 | 26.3 | 4.1 | 13.5 | 0.15 | 0.04* | <0.001 | 0.58 |
| 1998–00 | 26.5 | 23.7 | 2.8 | 10.6 | 25.7 | 18.3 | 7.4 | 28.8 | <0.001* | <0.001* | 0.18 | 0.93 |
| 2000–02 | 23.4 | 20.4 | 3.0 | 12.8 | 25.5 | 21.4 | 4.1 | 16.1 | 0.73 | <0.005* | 0.09 | 0.09 |
| Excessive alcohol use (>14 drinks/week for men, >9 drinks/week for women) | ||||||||||||
| 1994–96 | 7.4 | 6.9 | 0.5 | 6.8 | 8.2 | 7.1 | 1.1 | 13.4 | 0.86 | 0.63 | 0.29 | 0.28 |
| 1996–98 | 6.9 | 7.1 | –0.2 | –2.9 | 5.2 | 5.5 | –0.3 | –5.8 | 0.91 | 0.26 | 0.44 | 0.59 |
| 1998–00 | 7.2 | 6.1 | 1.1 | 15.3 | 5.5 | 6.8 | –1.3 | –23.6 | 0.06 | 0.86 | 0.44 | 0.35 |
| 2000–02 | 6.1 | 6.2 | –0.1 | –1.6 | 5.2 | 5.5 | –0.3 | –5.8 | 0.85 | 0.78 | 0.75 | 0.64 |
| Physical inactivity | ||||||||||||
| 1994–96 | 60.4 | 58.4 | 2.0 | 3.3 | 65.7 | 62.7 | 3.0 | 4.6 | 0.91 | 0.53 | 0.07 | 0.90 |
| 1996–98 | 57.8 | 53.9 | 3.9 | 6.7 | 65.2 | 55.0 | 10.2 | 15.6 | 0.34 | 0.57 | 0.02* | 0.26 |
| 1998–00 | 53.3 | 55.5 | –2.2 | –4.1 | 56.6 | 54.8 | 1.8 | 3.2 | 0.32 | 0.11 | 0.55 | 0.46 |
| 2000–02 | 54.9 | 49.2 | 5.7 | 10.4 | 57.3 | 56.7 | 0.6 | 1.0 | 0.05* | 0.26 | 0.53 | 0.65 |
| BMI ≥25 kg/m2 | ||||||||||||
| 1994–96 | 46.0 | 48.2 | –2.2 | –4.8 | 63.0 | 66.1 | –3.1 | –4.9 | <0.001* | 0.25 | <0.001 | 0.05* |
| 1996–98 | 48.1 | 50.7 | –2.6 | –5.4 | 60.7 | 60.4 | 0.3 | 0.5 | 0.42 | 0.80 | <0.001 | 0.04* |
| 1998–00 | 49.9 | 52.9 | –3.0 | –6.0 | 65.3 | 67.9 | –2.6 | –4.0 | 0.02* | 0.42 | <0.001 | 0.07 |
| 2000–02 | 51.9 | 54.0 | –2.1 | –4.0 | 72.2 | 72.5 | –0.3 | –0.4 | 0.06 | 0.70 | <0.001 | 0.18 |
Absolute risk reduction (ARR) is the absolute risk difference between before and after percentages, while the relative risk reduction (RRR) consists of the ARR as a percentage of the risk factor before hypertension diagnosis.
*The likelihood of the presence of the risk factor after hypertension was diagnosed, adjusted for age, sex and the same lifestyle factor in the previous year;
†The likelihood of the lifestyle factor in the cycle before hypertension was reported, adjusted for age and sex. CMH Cochran-Mantel-Haenszel
Examining the interaction between lifestyle alteration and use of antihypertensive medication (Table 4) indicates that persons not taking antihypertensive medications were not more likely to change lifestyle in response to their recently diagnosed hypertension. In fact, people who consumed antihypertensive medication were also more likely to quit smoking and more likely to increase their physical activity. However, persons taking antihypertensive medications were also more likely to become obese (RRR –12.7; Tables 4 and 5). When examining changes in the proportion of obese individuals among those taking antihypertensive medication, it was found that the weight gain occurred mostly among those taking beta-blockers and especially among women (Table 5).
TABLE 4.
Changes in lifestyle by antihypertensive medication use
| Presence of lifestyle risk factor
|
ARR, % | RRR, % | P | ||
|---|---|---|---|---|---|
| Before, n (%) | After, % | ||||
| Total | |||||
| Smoking | 346 (27.0) | 22.1 | 4.9 | 18.2 | <0.001* |
| Excessive alcohol use† | 77 (7.9) | 8.6 | –0.7 | –8.9 | 0.38 |
| Physical inactivity | 765 (60.9) | 56.1 | 4.8 | 7.9 | <0.01* |
| BMI ≥25 kg/m2 | 830 (66.0) | 68.2 | –2.2 | –3.3 | 0.04* |
| BMI ≥30 kg/m2 | 306 (24.3) | 27.1 | –2.8 | –11.5 | 0.02* |
| Using antihypertensive medication | |||||
| Smoking | 200 (26.0) | 19.6 | 6.4 | 24.6 | <0.001* |
| Excessive alcohol use† | 39 (6.8) | 7.5 | –0.7 | –10.3 | 0.65 |
| Physical inactivity | 483 (64.1) | 58.8 | 5.3 | 8.3 | <0.01* |
| BMI ≥25 kg/m2 | 482 (63.8) | 65.8 | –2.0 | –3.1 | 0.23 |
| BMI ≥30 kg/m2 | 179 (23.7) | 26.7 | –3.0 | –12.7 | 0.05* |
| Not using antihypertensive medication | |||||
| Smoking | 146 (28.5) | 25.8 | 2.7 | 9.5 | 0.03* |
| Excessive alcohol use† | 38 (9.5) | 10.2 | –0.7 | –7.4 | 0.43 |
| Physical inactivity | 282 (56.0) | 52.1 | 3.9 | 7.0 | 0.15 |
| BMI ≥25 kg/m2 | 348 (69.2) | 71.7 | –2.5 | –3.6 | 0.06 |
| BMI ≥30 kg/m2 | 127 (25.3) | 27.7 | –2.4 | –9.5 | 0.20 |
Absolute risk reduction (ARR) is the absolute risk difference between before and after percentages, while the relative risk reduction (RRR) consists of the ARR as a percentage of the risk factor before hypertension diagnosis.
*Statistically significant at P≤0.05 as calculated by McNemar’s test;
†Excessive alcohol use was considered to be >14 drinks per week for men and >9 drinks per week for women
TABLE 5.
Proportions of obese persons (body mass index greater than 30 kg/m2) before and after hypertension diagnosis by antihypertensive medication use
| All
|
Men
|
Women
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before, n (%) | After, % | ARR, % | RRR, % | P | Before, n (%) | After, % | ARR, % | RRR, % | P | Before, n (%) | After, % | ARR, % | RRR, % | P | ||
| Taking any antihypertensive medication | ||||||||||||||||
| Yes | 179 (23.7) | 26.7 | –3.0 | –12.7 | 0.05* | 70 (20.1) | 21.2 | –1.1 | –5.5 | 0.47 | 120 (25.2) | 28.2 | –3.0 | –11.9 | 0.06 | |
| No | 127 (25.3) | 27.7 | –2.4 | –9.5 | 0.20 | 51 (20.1) | 22.1 | –2.0 | –10.0 | 0.30 | 79 (26.6) | 28.3 | –1.7 | –6.4 | 0.42 | |
| Among those taking antihypertensive medication | ||||||||||||||||
| Beta-blockers | Yes | 42 (18.4) | 23.7 | –5.3 | –28.8 | <0.01* | 15 (14.4) | 16.4 | –2.0 | –13.9 | 0.32 | 27 (21.8) | 29.8 | –8.0 | –36.7 | 0.01* |
| No | 148 (24.8) | 25.8 | –1.0 | –4.0 | 0.46 | 55 (22.5) | 23.3 | –0.8 | –3.6 | 0.69 | 93 (26.4) | 27.6 | –1.2 | –4.5 | 0.53 | |
Absolute risk reduction (ARR) is the absolute risk difference between before and after percentages, while the relative risk reduction (RRR) consists of the ARR as a percentage of the risk factor before hypertension diagnosis.
*Statistically significant at P≤0.05 as calculated by McNemar’s test
DISCUSSION
Canadians and people in other western countries are at considerable risk of becoming hypertensive (6). While changes in lifestyle risk factors should be an important part of hypertension management, the present study showed that a diagnosis of hypertension did not lead to many lasting lifestyle changes. Smoking was an exception, because almost one in five smokers quit after learning that they had hypertension. However, lifestyle changes should be a first-line treatment in any cardiovascular disease, and this was not seen in the results of the present study. Within the study population, smoking cessation and the small improvement in physical activity seemed to largely occur in people who were also taking antihypertensive medication. The increased smoking cessation associated with antihypertensive medication use may reflect the values people place on their health and, thus, persons who value their health most may be more inclined to do both.
The NPHS data used for the present study have strengths and limitations. Strengths include the extensive information available for each respondent, such as the major risk factors for hypertension. All of the variables were measured at five points in time, so that the emergence of hypertension could be detected, and before and after comparisons could be made. The study design, based on the before and after measurements on the same person, allowed a matched-pair analysis, which makes optimal use of available cases while adjusting for many attributes, including unmeasured ones such as socioeconomic class and type A personality. Limitations include the self-reporting of conditions such as hypertension and other chronic diseases. Although multiple data points were available for each person, the interviews were performed at two-year intervals unrelated to the time of the hypertension diagnosis. Hypertension could have been newly diagnosed in the previous month or as many as 24 months previously, with lifestyle changes made by respondents in the larger time frame having a greater likelihood of reverting back to earlier habits. Still, the purpose of the present study was to obtain an indication of changes in lifestyle and medication use associated with recently hypertensive patients, and this was achieved.
A concern that needs to be addressed is the extent to which changes in the newly diagnosed hypertensive populations are just a part of the secular changes occurring in the source population. In fact, the source population also showed a decreasing trend in smoking and physical inactivity, unrelated to recent development of hypertension; however, changes in the newly diagnosed hypertensive population tended to be more marked than in the source population. Also of special interest was the higher proportion of overweight individuals among the new hypertensive patients even before hypertension was diagnosed, indicating once again that this is a lifestyle risk for developing hypertension.
Perhaps a surprising finding was the increase in obesity among newly diagnosed hypertensive patients. Part of this increase was in parallel with the source population, which also showed an increasing trend in the proportion of overweight people over the years. Nevertheless, the newly diagnosed hypertensive population already consisted of a larger proportion of overweight people, and instead of showing decreasing weight after diagnosis, more obese respondents were seen rather than fewer. Further analysis showed that this was particularly true among persons taking antihypertensive medication, in whom beta-blockers appeared to be responsible for much of the increase in obese persons. This increase in weight after taking beta-blockers is consistent with observations from clinical trials (19) showing that longer exposure to beta-blockers led to a greater increase in average weight (20). A case series study in an outpatient clinic (21) showed that patients taking beta-blockers experienced twice the weight gain of patients taking angiotensin-converting enzyme inhibitors. To our knowledge, increases in weight related to beta-blocker therapy have not been previously reported in population studies. It is possible that previously overweight people were pushed into the obese category, and that the actual weight gain was not necessarily large, but more research is needed to confirm these results. Potential mechanisms include an altered metabolism or decreased maximal physical capacity related to the blockade of the beta receptor. In overweight patients with hypertension for whom weight loss would be beneficial, and other considerations being the same, it may be wiser to use other classes of antihypertensive medication (20).
It is clear that more work needs to be done about promoting lifestyle changes. The present study shows that other than in smoking cessation, there is little improvement in the lifestyles of newly diagnosed patients. The fact that three-quarters of those diagnosed with hypertension were taking antihypertensive medication within two years of first diagnosis while little lifestyle modification was seen suggests an over-reliance on antihypertensive medication compared with lifestyle modification. People developing hypertension are already more likely to have more risk factors, and reducing such risk factors by lifestyle changes, while often difficult, is effective in reducing hypertension. In addition, this would avoid the potential, however small, of adverse drug effects, as well as the costs of the medications. Because few patients with hypertension recall receiving advice to modify their lifestyles (3), health care professionals need to be more aggressive in their counselling regarding lifestyle issues when treating newly diagnosed hypertensive patients. To achieve lasting lifestyle changes, it is likely that system changes are needed, such as the creation of multidisciplinary teams with expertise in counselling and the remuneration of time spent in lifestyle counselling (12,13,16). A disadvantage of the greater promotion and emphasis on blood pressure may be the ‘sick patient’ effect, in which people assume a sick role and show more absenteeism after the diagnosis of hypertension (22). Promotion will need to include a component indicating that hypertension in itself is not a condition that hampers one’s lifestyle – on the contrary, if controlled, it will allow a normal lifestyle for a longer period of time.
Footnotes
CONFLICTS OF INTEREST: No conflicts of interest are reported for Dr C Ineke Neutel. Dr Norm RC Campbell has received honoraria for speaking and/or travel grants from most companies that produce brand name antihypertensive drugs in Canada, and has received research funds for epidemiological research from Pfizer Canada, sanofiaventis, Bristol-Myers Squibb, Servier Canada and Merck Frosst Canada.
REFERENCES
- 1.Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–10. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 2.Joffres MR, Ghadirian P, Fodor JG, Petrasovits A, Chockalingam A, Hamet P. Awareness, treatment, and control of hypertension in Canada. Am J Hypertens. 1997;10:1097–102. doi: 10.1016/s0895-7061(97)00224-0. [DOI] [PubMed] [Google Scholar]
- 3.Petrella RJ, Campbell NR. Awareness and misconception of hypertension in Canada: Results of a national survey. Can J Cardiol. 2005;21:589–93. [PubMed] [Google Scholar]
- 4.Campbell NR, Burgess E, Taylor G, et al. Lifestyle changes to prevent and control hypertension: Do they work? A summary of the Canadian consensus conference. CMAJ. 1999;160:1341–3. [PMC free article] [PubMed] [Google Scholar]
- 5.Staessen JA, Wang JG, Thijs L. Cardiovascular prevention and blood pressure reduction: A quantitative overview updated until 1 March 2003. J Hypertens. 2003;21:1055–76. doi: 10.1097/00004872-200306000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Appel LJ, Champagne CM, Harsha DW, et al. Writing Group of the PREMIER Collaborative Research Group Effects of comprehensive lifestyle modification on blood pressure control: Main results of the PREMIER clinical trial. JAMA. 2003;289:2083–93. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 7.Unal B, Critchley JA, Fidan D, Capewell S. Life-years gained from modern cardiological treatments and population risk factor changes in England and Wales, 1981–2000. Am J Public Health. 2005;95:103–8. doi: 10.2105/AJPH.2003.029579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Appel LJ. Lifestyle modification as a means to prevent and treat high blood pressure. J Am Soc Nephrol. 2003;14:S99–S102. doi: 10.1097/01.asn.0000070141.69483.5a. [DOI] [PubMed] [Google Scholar]
- 9.Hemmelgarn BR, Zarnke KB, Campbell NR, et al. Canadian Hypertension Education Program, Evidence-Based Recommendations Task Force The 2004 Canadian Hypertension Education Program recommendations for the management of hypertension: Part I – blood pressure measurement, diagnosis and assessment of risk. Can J Cardiol. 2004;20:31–40. [PubMed] [Google Scholar]
- 10.Critchley JA, Capewell S. Substantial potential for reductions in coronary heart disease mortality in the UK through changes in risk factor levels. J Epidemiol Community Health. 2003;57:243–7. doi: 10.1136/jech.57.4.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hemmelgarn BR, McAllister FA, Myers MG, et al. Canadian Hypertension Education Program The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk. Can J Cardiol. 2005;21:645–56. [PubMed] [Google Scholar]
- 12.Padwal R, Campbell N, Touyz RM, Canadian Hypertension Education Program Applying the 2005 Canadian Hypertension Education Program recommendations: 3. Lifestyle modifications to prevent and treat hypertension. CMAJ. 2005;173:749–51. doi: 10.1503/cmaj.050186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan NA, McAlister FA, Lewanczuk RZ, et al. Canadian Hypertension Education Program The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: Part II – therapy. Can J Cardiol. 2005;21:657–72. [PubMed] [Google Scholar]
- 14.Franco V, Oparil S, Carretero OA. Hypertensive therapy: Part II. Circulation. 2004;109:3081–8. doi: 10.1161/01.CIR.0000132615.44103.B1. [DOI] [PubMed] [Google Scholar]
- 15.Choinière R, Lafontaine P, Edwards AC. Distribution of cardiovascular disease risk factors by socioeconomic status among Canadian adults. CMAJ. 2000;162:S13–24. [PMC free article] [PubMed] [Google Scholar]
- 16.Touyz RM, Campbell N, Logan A, Gledhill N, Petrella R, Padwal R, Canadian Hypertension Education Program The 2004 Canadian recommendations for the management of hypertension: Part III –lifestyle modifications to prevent and control hypertension. Can J Cardiol. 2004;20:55–9. [PubMed] [Google Scholar]
- 17.Assaf AR, Parker D, Lapane KL, Coccio E, Evangelou E, Carleton RA. Does the Y chromosome make a difference? Gender differences in attempts to change cardiovascular disease risk factors. J Womens Health (Larchmt) 2003;12:321–30. doi: 10.1089/154099903765448835. [DOI] [PubMed] [Google Scholar]
- 18.Khan NA, McAlister FA, Lewanczuk RZ, et al. Canadian Hypertension Education Program The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: Part II – therapy. Can J Cardiol. 2005;21:657–72. [PubMed] [Google Scholar]
- 19.Pischon T, Sharma AM. Use of beta-blockers in obesity hypertension: Potential role of weight gain. Obes Rev. 2001;2:275–80. doi: 10.1046/j.1467-789x.2001.00044.x. [DOI] [PubMed] [Google Scholar]
- 20.Mosenkis A, Townsend RR. Antihypertensive medications and weight gain. J Clin Hypertens (Greenwich) 2004;6:90. doi: 10.1111/j.1524-6175.2004.02847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dzien A, Dzien-Bischinger C, Hoppichler F, Lechleitner M. Antihypertensive medication with beta-blockers and ACE-inhibitors – effects on weight gain associated with ageing. Age Ageing. 2003;32:557–8. doi: 10.1093/ageing/afg082e. [DOI] [PubMed] [Google Scholar]
- 22.Haynes RB, Sackett DL, Taylor DW, Gibson ES, Johnson AL. Increased absenteeism from work after detection and labeling of hypertensive patients. N Engl J Med. 1978;299:741–4. doi: 10.1056/NEJM197810052991403. [DOI] [PubMed] [Google Scholar]