Abstract
Background
Elderly patients with bipolar disorder have been found to have higher mortality than those with major depressive disorder. The authors compare medical burden in elderly patients with bipolar disorder with that in those with major depressive disorder.
Methods
Fifty-four patients with bipolar I or II disorder who were 60 years of age and older were equated 1-to-2 to 108 patients with nonpsychotic, major depressive disorder according to age, sex, race, and lifetime duration of mood disorder illness. Variables examined included the following: Cumulative Illness Rating Scale for Geriatrics (CIRS-G) total scores, body mass index (BMI), and CIRS-G subscale scores.
Results
Compared with patients with major depressive disorder, patients with bipolar disorder had similar levels of general medical comorbidity on the CIRS-G total score and number of systems affected but higher BMI. After controlling for multiple comparisons, the endocrine/metabolic and respiratory subscale scores on the CIRS-G were higher for patients with bipolar disorder.
Conclusion
Although overall medical burden appears comparable in elderly patients with bipolar and those with major depressive disorder, patients with bipolar disorder have higher BMI and greater burden of endocrine/metabolic and respiratory disease.
Keywords: bipolar disorder, major depressive disorder, medical comorbidity, aged
Patients with bipolar disorder and their healthcare providers tend to view their psychiatric care as the most important aspect of medical care.1,2 This view has led to a relative underrecognition and inattention to many of the physical diseases these patients have. Our research group has shown even young and middle-aged patients with bipolar disorder have substantial medical burden.3 The accumulation of medical illness and poor medical care may explain the increased mortality rate among older bipolar patients. Specifically, in a survival analysis, Shulman et al.4 found that over a six-year period 50%of elderly manic patients had died compared with only 20% of an age- and sex-matched group of unipolar depressed patients.
Therefore, we decided to examine the relative medical burden in older adults with bipolar disorder compared with that in those with major depressive disorder. We wanted to determine how the profile of disease burden varied between the two groups, because some, but not all, reports have shown worse medical outcomes for patients with bipolar disorder than for mixed-age adults with major depressive disorder.5-7 On the basis of our previous work, our primary hypotheses were that medical illness burden, as measured with the Cumulative Illness Rating Scale for Geriatrics (CIRS-G), would be greater for and that body mass index (BMI) would be higher in the patients with bipolar disorder than in those with major depressive disorder. Our secondary hypothesis was that there would be an increased burden of endocrine/metabolic and cardiovascular disease in the patients with bipolar disorder, given reports that obesity,8,9 diabetes mellitus,9-11 dyslipidemia,9,12,13 and hypertension9,14 are associated with the disorder. To date, we are not aware of any report comparing medical burden on a systems level between the two diagnostic groups with the CIRS-G or comparing BMI.
METHODS
Subjects
As previously described,8 the Bipolar Disorder Center for Pennsylvanians Study is a multicenter, randomized, controlled study involving subjects with bipolar I and II disorders not otherwise specified or schizoaffective disorder bipolar subtype. This study was designed to test the efficacy of an Enhanced Clinical Intervention, a psychoeducational intervention. All subjects received a standardized, well-accepted drug regimen and were randomized to receive Enhanced Clinical Intervention or usual supportive care. The present analysis included 54 subjects, age 60 years and older, with bipolar I (N=39) and II (N=15) disorders confirmed through a research diagnostic interview using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.15 They were consecutively recruited from academic and community-based practices between November 2003 and July 2005 into the Bipolar Disorder Center for Pennsylvanians Study at the site in Pittsburgh, Pennsylvania. Special efforts were made to recruit African Americans. Fifty-nine subjects were screened for study participation, of whom five were excluded for various reasons: unstable medical illness (N=1), death (N=1), inconvenience of study procedures (N=2), and psychiatric illness secondary to general medical condition (N=1). Subjects were not required to be acutely ill to enroll in the study; most subjects enrolled the study euthymic or with mild depressive symptoms. Roughly 80% of subjects were referred by mental health providers for research participation.
Comparators were 108 elderly patients with nonpsychotic, major depressive disorder equated 2-to-1 with bipolar subjects according to age, sex, race, and lifetime duration of mood disorder illness. We matched on lifetime duration of mood disorder illness to control for the negative health behaviors associated with depressive illness.16 Comparators were selected from completed and ongoing intervention studies of depression conducted within the Advanced Center for Intervention and Services Research for Late-Life Mood Disorders (ACISR/LLMD) at the University of Pittsburgh School of Medicine.17,18 Diagnosis was confirmed with the Schedule for Affective Disorders and Schizophrenia Lifetime Version19 in 63 of the comparators18 and with the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, in the remaining 4317 and 220 comparators. To enroll in any one of these studies, subjects were required to have a Hamilton Rating Scale for Depression score (17-item)21 of ≥15. Age equation was aimed to be within three years; 90% of subjects were equated within five years, and all subjects were equated within six years. Duration of illness was equated within 10 years for 75% of subjects; an additional 15% of subjects were equated within 20 years, and an additional 5% were equated within 30 years. Four outliers, with >30 years’ duration of bipolar illness, could not be equated within 30 years; for example, an elderly individual with a 75-year history of bipolar disorder was equated with an individual with a 19-year history of depression. Because subjects and comparators were recruited through the Advanced Center for Intervention and Services Research for Late-Life Mood Disorders, similar exclusions for medical comorbidity were present; specifically, the only medical exclusion was for unstable medical illness or mood disorder due to general medical condition. Furthermore, similar practices were used for recruiting both bipolar and depressed subjects; hence, the participants were recruited from the same base population of western Pennsylvania. Roughly 3% of depressed subjects were excluded due to unstable medical illness. Approximately 40% of subjects were referred by mental health providers for research participation.
The Institutional Review Board at the University of Pittsburgh reviewed and approved all the procedures described in these protocols, and all subjects provided written informed consent before participating in the study.
Measures
All measures were taken from the baseline assessment in each of the studies. Height and weight were measured in light clothing. Trained physician assistants or nurse practitioners completed the CIRS-G21 based on medical history collected from each subject and review of their medical records, including primary care provider notes, inpatient hospitalization records, test results, and pharmacy records.
The CIRS-G is an instrument originally developed to assess the chronic medical burden in adult22 and geriatric21 populations. Studies have confirmed criterion validity,23 concurrent validity,21 interrater reliability,24 and construct validity.25 However, evidence supporting its predictive validity is limited. Rating the CIRS-G based on chart review has shown good reliability and offers some practical advantages.24 The CIRS-G is structured in 13 organ systems (we excluded the psychiatric system); it rates the severity of disease for each system according to operationalized criteria on a 5-point Likert-type scale (ranging from 0=no impairment to 4=extremely severe), providing a useful way of summarizing overall medical burden across specific organ systems. Few of our patients received a score of 4 because unstable or life-threatening medical condition was an exclusion criterion across the studies. The CIRS-G records both current active medical problems and history of medical problems, which are no longer active; hence, CIRS-G scores tend to gradually increase over time and not to fluctuate substantially.21 We report the total score (the sum of ratings across the 13 categories), the number of organ systems affected, and the score for each organ system.
Statistical Analyses
Subjects were described using means and SDs. Groups were compared with χ2 statistics for categorical measures, group t-tests on continuous measures, and ordinal logistic regression for the CIRS-G items. Given the exploratory nature of examining the CIRS-G individual items, we used the Bonferroni method (p <0.004 was considered significant) to correct for multiple comparisons in testing the secondary hypothesis.
RESULTS
The diagnostic and demographic characteristics of the study groups are listed in Table 1. By design, the two groups were balanced according to age, sex, race, and lifetime duration of illness. Subjects with bipolar disorder had more education and were more likely to be currently married than subjects with major depressive disorder. Subjects with major depressive disorder were on higher numbers of nonpsychotropic medications than subjects with bipolar disorders. At the time of baseline evaluation, 21 bipolar disorder patients (39%) were treated with lithium, 10 (19%) were treated with anticonvulsants (divalproex or carbamazepine), and 13 (24%) were treated with second-generation antipsychotic drugs (olanzapine, quetiapine, risperidone, or ziprasidone). Patients with major depressive disorder already had discontinued use of psychotropic medications (at the time of baseline assessment). However, 4 subjects (4%) were still taking donepezil, 1 (1%) was taking desipramine, 1 (1%) was taking olanzapine, and 1 (1%) was taking modafinil. Information on prior medication exposure was not systematically recorded in the depressed group. There was a higher percentage of smokers in the bipolar group (N=9, 17%) than in the depressed group (N=11, 11%); however, this information was missing for 12 subjects in the depressed group.
TABLE 1.
Demographic and Clinical Characteristics of Older Subjects With Bipolar Disorder (N = 54) or Major Depressive Disorder (N = 108)
| Bipolar (N = 54) | Depressed (N = 108) | χ 2 or t | df | p | |
|---|---|---|---|---|---|
| Men age (SD), years | 69.5 (7.6) | 70.5 (6.6) | 0.86 | 160 | 0.39 |
| Men, no. (%) | 37 (20) | 37 (40) | 0.00 | 1 | 1.00 |
| White, no. (%) | 89 (48) | 92 (99) | 0.33 | 1 | 0.57 |
| Mean duration from first onset (SD), years | 33.7 (15.2) | 30.3 (15.0) | 1.35 | 160 | 0.18 |
| Less than high school education, no. (%) | 2 (4) | 17 (16) | 13.45 | 4 | 0.01 |
| High school education, no. (%) | 15 (28) | 44 (41) | |||
| Some college, no. (%) | 11 (20) | 22 (20) | |||
| College, no. (%) | 14 (26) | 12 (11) | |||
| Graduate, no. (%) | 12 (22) | 13 (12) | |||
| Never married, no. (%) | 2 (4) | 34 (31) | 25.03 | 3 | 0.0001 |
| Married, no. (%) | 26 (48) | 20 (19) | |||
| Separated/divorced, no. (%) | 17 (31) | 42 (39) | |||
| Widowed, no. (%) | 9 (17) | 12 (11) | |||
| Mean no. of nonpsychotropic medications (SD); median | 4.9 (3.2); 4 | 7.6 (6.5); 6 | 2.54 | 160 | 0.012a |
| Current smoker, no. (%) | 9 (17) | 11 (11)b | 4.49 | 1 | 0.04 |
Square root transformation before statistical comparison.
Ninety-six patients.
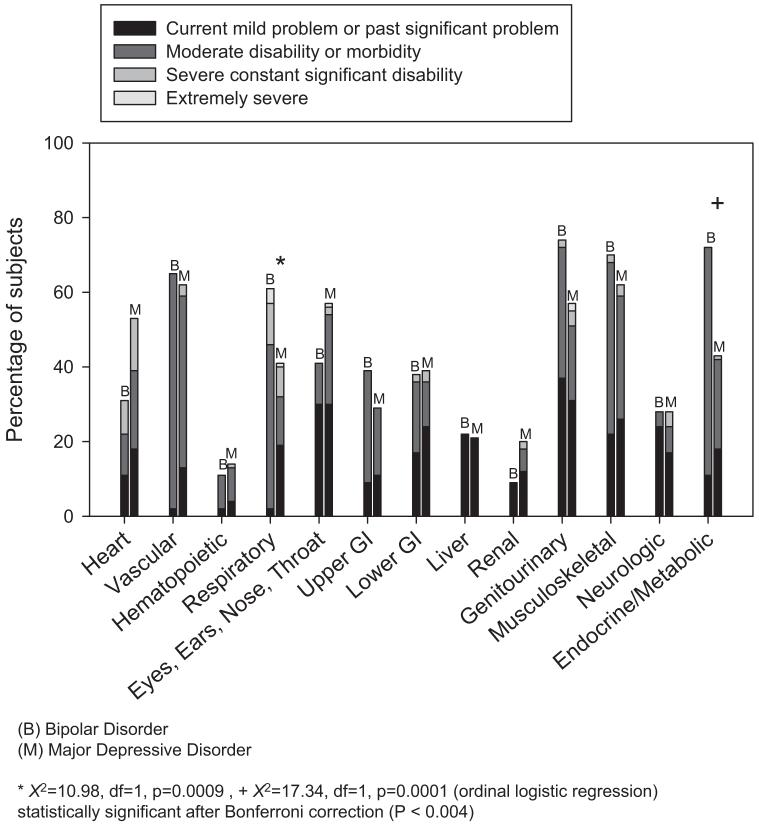
CIRS-G total scores were comparable between the two groups (Figure 1). Mean (SD) CIRS-G total scores for subjects with bipolar disorder compared with depressed subjects were 9.6 (3.9) versus 8.6 (4.4) (t = 1.40, df=160, p=0.16), respectively. Subjects with bipolar disorder had a higher mean BMI (29.8 [5.5]) than subjects with major depressive disorder (27.9 [5.1]) (t=2.18, df=147, p=0.04). Both groups were heavier than the national average for adults (overweight, 34%; obese, 30%)26: 30% of bipolar patients were overweight, and 49% were obese; 41% of depressed patients were overweight, and 29% were obese.
FIGURE 1.
Comulative Illness Rating Scale: Geriatric Subscale Scores in Subjects with Bipolar Disorder Versus Major Depressive Disorder
Mean (SD) number of systems affected in the bipolar versus depressed subjects was 5.6 (2.0) versus 5.2 (2.2) (t=1.08, df = 160, p=0.28), respectively. Subjects with bipolar disorder had significantly higher mean scores on ratings of the endocrine/metabolic system than depressed subjects: 1.33 (0.89) versus 0.69 (0.87), respectively (ordinal logistic regression; χ2=17.34, df=1, p=0.0001), indicating increased severity of endocrine/metabolic disorders in this bipolar group. In addition, subjects with bipolar disorder had significantly higher mean scores on ratings of the respiratory system than subjects with depression: 1.39 (1.22) versus 0.73 (1.04) (χ2=10.98, df = 1, p=0.0009), respectively. All other body system scores were similar between bipolar and depressed groups. In the bipolar group, the endocrine/metabolic abnormalities included hypothyroidism (N=12, 22%), diabetes mellitus (N=7, 13%; Type 2: N=5, 9%; Type 1: N=2, 4%), thyroid nodule (N=4, 7%), and breast lesion (N=3, 6%). Respiratory abnormalities included asthma (N=3, 6%), chronic obstructive pulmonary disease (N=2, 4%), bronchitis (N=1, 2%), and pulmonary nodule (N=1, 2%). In relation to smoking status, 53% patients with bipolar disorder who were current nonsmokers scored ≥2 on the CIRS-G respiratory subscale, while 15% of the depressed subjects who were current nonsmokers scored ≥2 on this subscale. Of the current smokers, 89% of bipolar subjects scored ≥2 on the CIRS-G respiratory subscale, while 64% of the depressed subjects scored ≥2 on this subscale.
DISCUSSION
Although older adult subjects with bipolar disorder and major depressive disorder have comparable overall burden of physical illness, subjects with bipolar disorder had significantly higher BMI and a greater burden of endocrine/metabolic and respiratory illness. Endocrine/metabolic illness burden mainly consisted of hypothyroidism and diabetes mellitus. Almost all bipolar subjects were treated with lithium, anticonvulsants, or atypical antipsychotic drugs that are well known to increase the risk for hypothyroidism, weight gain, and diabetes.27 However, the iatrogenic effects of these medications may not fully explain the greater illness burden in the case of diabetes, because biologic factors have been implicated as well.28,29 Despite the increased endocrine/metabolic illness burden in the bipolar group, we did not find a difference in the extent of cardiovascular disease between the two groups as we had hypothesized. We found that both groups had high levels of cardiovascular illness. Respiratory illness burden mainly consisted of asthma and chronic obstructive pulmonary disease. The underlying cause of the increased prevalence of respiratory burden in the bipolar group, given the limits of the data collected, was difficult to ascertain. In general, the high prevalence of tobacco use in patients with bipolar disorder may lead to increased prevalence of respiratory illnesses in current or former smokers.30 That patients with bipolar disorder were generally taking fewer nonpsychotropic medications compared with depressed patients may suggest that patients with bipolar disorder receive more limited attention to general medical conditions.
Limitations of this analysis need to be acknowledged. First, the patients described in this analysis may not generalize to patients seen outside of a university-based research clinic and may underestimate medical comorbidity in bipolar and depressed patients because unstable medical illness was excluded across the studies. Second, because the standardized mortality ratio for all deaths appears higher in bipolar patients (2.5 for bipolar males and 2.7 for bipolar females) compared with patients with major depressive disorder (2.0 for both sexes), these results may apply only to subjects who achieve older age.7 In addition, because the bipolar group was more likely to consist of “survivors,” the medical comorbidity in patients with bipolar disorder could be underestimated in relation to patients with depression. Third, complete information on psychotropic medication exposure in the depressed group was not available. That patients in the depressed group had increased illness severity at baseline was likely related to their receiving treatment with fewer psychotropic medications: that is, patients with bipolar disorder were less symptomatic because they were receiving psychotropic treatment. Fourth, although the CIRS-G as a whole has been found to be valid and reliable,25 the validity and reliability of examining the CIRS-G individual subscales is not well established. Last, while we attempted to fully describe each subject’s medical status, information on medical status may have been missed. Information on smoking history was not available, which would have been helpful in understanding the higher level of respiratory illness burden in the bipolar subjects than in the depressed subjects who were current nonsmokers.
Despite the limitations noted, we believe that this analysis further highlights the importance of integrating general medical care into psychiatric care of patients with bipolar disorder. Patients with bipolar disorder may receive less medical attention than depressed patients, emphasizing a need to enhance clinician attention to the general medical needs of bipolar patients.31 Further, the nature of bipolar disorder may often preclude effective primary medical care. Hence, for patients with bipolar disorder, the integration of general medical care with mental healthcare may be more effectively accomplished in the mental healthcare setting than in the primary care setting.32 Conversely, for patients with major depressive disorder, physical illnesses are recognized in primary care; hence, these patients may benefit from receiving high-quality, mental health treatment in primary care.33
To put our findings into context, Fortin et al.34 examined the extent of multimorbidity in primary care patients in the Saguenay region (Quebec) of Canada. They found that mean CIRS-G total scores were 13.1 (confidence interval: 11.9-14.2) among men 65 years of age and older and 12.9 (confidence interval: 12.2-13.7) among women 65 years of age and older, which included the psychiatric subscale. Had we included the psychiatric subscale in the CIRS-G total scores, all of our ratings would have been 3 points higher. By limiting our sample to subjects 65 years of age and older and including the psychiatric subscale, mean total scores (SD) in the bipolar group (N=32) would have been 13.3 (4.0).
Our findings argue for advances in treatment of bipolar disorder to go together with increased integration of psychiatric and general medical care. Interventions focused on weight loss are critical, given the prevalence of obesity in elderly patients with mood disorders in general and bipolar disorder in particular.35 Modest weight loss (5%-10%) can have beneficial effects on blood glucose and plasma lipid levels and blood pressure.36 Targeted smoking cessation programs for middle-aged and older adult patients with bipolar disorder may reduce respiratory illness burden in later life. In addition, randomized, controlled trials of pharmacotherapy for older adults with bipolar disorder are needed to better understand the potential iatrogenic effects of bipolar pharmacotherapy on the elderly.
Acknowledgments
The authors thank the staff of the Clinical Trials Management Unit of the Intervention Research Center and the Advanced Center for Intervention and Services Research for Late-Life Mood Disorders (Pittsburgh, PA) for their care of the patients in this study. The authors thank Elizabeth Weber, C.R.N.P., Rajeev Malhotra, M.D., and Mark Miller, M.D., for collecting, organizing, and interpreting the data presented in this report. This work was supported in part by Public Health Service grants P30 MH52247, P30 MH71944, T32 MH19986, K23 MH 073772, K23 MH 67710, K01 MH01684, K24 MH069430, and R01 MH072947 and grant ME-02385 from the Commonwealth Center of Excellence for Bipolar Disorder, Pennsylvania Department of Health. This work was also supported by the VA, Veterans Health Administration, Health Services Research and Development Service (IIR 02-283; MPR02269 to AM K [PI]). AGG has participated in scientific advisory board meetings for Shire Pharmaceuticals. He is a “minor” (less than $10,000) stockholder of Eli Lilly & Company. RAD is a minor stockholder of Eli Lilly & Company and Sanofi-Aventis. CFR has received research support from Forest Pharmaceuticals and GlaxoSmith-Kline. EF has participated in scientific advisory board meetings for Servier Amerique. She has received research support from Forest Pharmaceuticals and the Pittsburgh Foundation. She has received royalties from the Guilford Press. She has served as a consultant to Pfizer, Eli Lilly & Company, Novartis, and Lundbeck. DJK has served on the advisory board of Eli Lilly & Company, Forest Pharmaceuticals, Pfizer, and Solvay/Wyeth Pharmaceuticals. He has served as a consultant for Servier Amerique. BHM received grant support from Forest Pharmaceuticals, Janssen, and Pfizer. He has served as a consultant to AstraZeneca, Fox Learning System, Lundbeck, and Pfizer. He has given lectures supported by AstraZeneca, Eisai, Forest Pharmaceuticals, and Pfizer. He is a minor stockholder of Akzo-Nobel, Alkermes, AstraZeneca, Biogen, Celsion, Elan, Eli Lilly & Company, Forest, General Electric, Immune Response, and Pfizer. He has received honoraria from AstraZeneca, Eisai, Forest Pharmaceuticals, Lundbeck, and Pfizer.
References
- 1.Kupfer DJ. The increasing medical burden in bipolar disorder. JAMA. 2005;293:2528–2530. doi: 10.1001/jama.293.20.2528. [DOI] [PubMed] [Google Scholar]
- 2.Cradock-O’Leary J, et al. Use of general medical services by VA patients with psychiatric disorders. Psychiatr Serv. 2002;53:874–878. doi: 10.1176/appi.ps.53.7.874. [DOI] [PubMed] [Google Scholar]
- 3.Kilbourne AM. The burden of general medical conditions in patients with bipolar disorder. Curr Psychiatry Rep. 2005;7:471–477. doi: 10.1007/s11920-005-0069-5. [DOI] [PubMed] [Google Scholar]
- 4.Shulman KI, et al. Mania compared with unipolar depression in old age. Am J Psychiatry. 1992;149:341–345. doi: 10.1176/ajp.149.3.341. [DOI] [PubMed] [Google Scholar]
- 5.Angst F, et al. Mortality of patients with mood disorders: follow-up over 34-38 years. J Affect Disord. 2002;68:167–181. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- 6.Winokur G, et al. Further distinctions between manic-depressive illness (bipolar disorder) and primary depressive disorder (unipolar depression) [see comment] Am J Psychiatry. 1993;150:1176–1181. doi: 10.1176/ajp.150.8.1176. [DOI] [PubMed] [Google Scholar]
- 7.Osby U, et al. Excess mortality in bipolar and unipolar Disorder in Sweden. Arch Gen Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- 8.Fagiolini A, et al. Metabolic syndrome in bipolar disorder: findings from the Bipolar Disorder Center for Pennsylvanians. Bipolar Disorders. 2005;7:424–430. doi: 10.1111/j.1399-5618.2005.00234.x. [DOI] [PubMed] [Google Scholar]
- 9.Beyer J, et al. Medical comorbidity in a bipolar outpatient clinical population. Neuropsychopharmacology. 2005;30:401–404. doi: 10.1038/sj.npp.1300608. [DOI] [PubMed] [Google Scholar]
- 10.Cassidy F, Ahearn E, Carroll BJ. Elevated frequency of diabetes mellitus in hospitalized manic-depressive patients. Am J Psychiatry. 1999;156:1417–1420. doi: 10.1176/ajp.156.9.1417. [DOI] [PubMed] [Google Scholar]
- 11.Regenold WT, et al. Increased prevalence of type 2 diabetes mellitus among psychiatric inpatients with bipolar I affective and schizoaffective disorders independent of psychotropic drug use. J Affect Disord. 2003;73:301–302. doi: 10.1016/s0165-0327(01)00456-6. erratum appears in. [DOI] [PubMed] [Google Scholar]; J Affect Disord. 2002;70:19–26. doi: 10.1016/s0165-0327(01)00456-6. [DOI] [PubMed] [Google Scholar]
- 12.Atmaca M, et al. Serum leptin and cholesterol levels in patients with bipolar disorder. Neuropsychobiology. 2002;46:176–179. doi: 10.1159/000067809. [DOI] [PubMed] [Google Scholar]
- 13.Horrobin DF, Bennett CN. Depression and bipolar disorder: relationships to impaired fatty acid and phospholipid metabolism and to diabetes, cardiovascular disease, immunological abnormalities, cancer, ageing and osteoporosis. Possible candidate genes. Prostaglandins Leukot Essent Fatty Acids. 1999;60:217–234. doi: 10.1054/plef.1999.0037. [DOI] [PubMed] [Google Scholar]
- 14.Yates WR, Wallace R. Cardiovascular risk factors in affective disorder. J Affect Disord. 1987;12:129–134. doi: 10.1016/0165-0327(87)90004-8. [DOI] [PubMed] [Google Scholar]
- 15.First MB, et al. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- 16.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds CF, III, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354:1130–1138. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- 18.Reynolds CF, 3rd, et al. Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: a randomized controlled trial in patients older than 59 years [see comment] JAMA. 1999;281:39–45. doi: 10.1001/jama.281.1.39. [DOI] [PubMed] [Google Scholar]
- 19.Spitzer RL. Schedule for Affective Disorders and Schizophrenia-Lifetime Version (SADS-L) New York State Psychiatric Institute; New York: 1978. [Google Scholar]
- 20.Whyte EM, et al. Geriatric depression treatment in nonresponders to selective serotonin reuptake inhibitors. J Clin Psychiatry. 2004;65:1634–1641. doi: 10.4088/jcp.v65n1208. [DOI] [PubMed] [Google Scholar]
- 21.Miller MD, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- 22.Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968;16:622–626. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 23.Conwell Y, et al. Validation of a measure of physical illness burden at autopsy: the Cumulative Illness Rating Scale. JAm Geriatr Soc. 1993;41:38–41. doi: 10.1111/j.1532-5415.1993.tb05945.x. [DOI] [PubMed] [Google Scholar]
- 24.Hudon C, Fortin M. Cumulative Illness Rating Scale was a reliable and valid index in a family practice context. J Clin Epidemiol. 2005;58:603–608. doi: 10.1016/j.jclinepi.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 25.de Groot V, et al. How to measure comorbidity. A critical review of available methods. J Clin Epidemiol. 2003;56:221–229. doi: 10.1016/s0895-4356(02)00585-1. [DOI] [PubMed] [Google Scholar]
- 26.Flegal KM, et al. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 27.Young RC, et al. Pharmacotherapy of bipolar disorder in old age. Am J Geriatr Psychiatry. 2004;12:342–357. doi: 10.1176/appi.ajgp.12.4.342. [DOI] [PubMed] [Google Scholar]
- 28.Evans DL, et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 29.McIntyre RS, et al. Bipolar disorder and diabetes mellitus: epidemiology, etiology, and treatment implications. Ann Clin Psychiatry. 2005;17:83–93. doi: 10.1080/10401230590932380. [DOI] [PubMed] [Google Scholar]
- 30.Waxmonsky JA, et al. Prevalence and correlates of tobacco use in bipolar disorder: data from the first 2000 participants in the Systematic Treatment Enhancement Program [see comment] Gen Hosp Psychiatry. 2005;27:321–328. doi: 10.1016/j.genhosppsych.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 31.Horvitz-Lennon M, Kilbourne AM, Pincus HA. From silos to bridges: meeting the general health care needs of people with mental illness. Health Aff. 2006;25:659–669. doi: 10.1377/hlthaff.25.3.659. [DOI] [PubMed] [Google Scholar]
- 32.Das AK, et al. Screening for bipolar disorder in a primary care practice. JAMA. 2005;293:956–963. doi: 10.1001/jama.293.8.956. [DOI] [PubMed] [Google Scholar]
- 33.Bruce ML, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 34.Fortin M, et al. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3:223–228. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adams KF, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 36.Van Gaal LF, Wauters MA, De Leeuw IH. The beneficial effects of modest weight loss on cardiovascular risk factors. Int J Obes Relat Metab Disord. 1997;21(Supplementsuppl 1):S5–S9. [PubMed] [Google Scholar]