Abstract
Purpose
Recent studies have showed that epithelial-mesenchymal transition (EMT) is a key process of glomerular and tubulointerstitial pathology in many chronic kidney diseases. However, there are no data of EMT in humane autosomal dominant polycystic kidney disease (ADPKD).
Patients and Methods
ADPKD kidneys (N = 5) with end stage renal disease (ESRD) and control kidneys (N = 4) were analyzed immnunohistochemically. We evaluated α-SMA, E-cadherin, vimentin, TGF-β1 and Smad 2/3 expression in ADPKD and compared them with those in control kidney. These immunohistochemical findings were quantitatively analyzed by computer-assisted image analyzer and positive tubules (%).
Results
There were severe interstitial fibrosis and proliferation of α-SMA+ myofibroblasts in ADPKD. Cystic tubular epithelial cells in ADPKD lost epithelial marker (E-cadherin) and expressed mesenchymal markers (α-SMA, vimentin). There were significant increases of α-SMA (34.3 ± 11.7% vs 0.9 ± 1.5%), vimentin (19.9 ± 3.9% vs 3.3 ± 1.4%), TGF-β1 (5.42 ± 2.83% vs 0%) and Smad 2/3 (3.4 ± 1.7% vs 0.7 ± 0.6%) in ADPKD kidneys compared with control kidneys evidenced by computer-assisted image analyzer. When we analyze the positive tubules (%), the results were the same as computer-assisted image analyzer.
Conclusion
Our results showed that the end stage of ADPKD is associated with TGF-β, Smad 2/3 and markers of EMT. It suggests that TGF-β mediated EMT has a role in progression of ADPKD.
Keywords: Epithelial mesenchymal transition, antosomal dominant polycystic kidney disease
INTRODUCTION
Autosomal dominant polycystic kidney disease (ADPKD) is a common hereditary disease, caused by mutations of either PKD1 or PKD2. End stage renal failure (ESRD) is the most dreaded complication of ADPKD. Despite recent advances in understanding the molecular pathogenesis and cystogenesis of ADPKD, and the development of ESRD due to polycystic kidney has remained elusive.1-3
The interstitial fibrosis is associated uniquely with renal failure in ADPKD4 and may be the final common pathway, in many chronic kidney diseases leading to ESRD. Renal interstitial fibroblasts are heterogeneous population that is difficult to define in situ. Recent studies have showed that epithelial-mesenchymal transition (EMT) can occur in tubular epithelial cells, which are able to migrate to the interstitium and produce extracelluar matrix protein.5-7 A recent study showed that overlap of fibroblast-specific protein 1 (FSP1)+ and α-smooth muscle actin (α-SMA)+ cells is associated with progressive fibrogenesis in animal PKD model. Some FSP1+ fibroblasts are likely derived from tubular epithelium undergoing EMT.8 In gene profiling of ADPKD, total of 87 genes were specifically regulated; 26 of these 87 genes were typical for smooth muscle, suggesting EMT as a pathogenetic factor in ADPKD.9 However, there are no direct data of EMT in human ADPKD.
Transforming growth factor-β (TGF-β) is needed to balance interactions between cells and extracelluar matrix. Studies of TGF-β signaling in the kidney had focused on the molecular biology of fibrogenesis. In recent years, TGF-β mediated glomerular and tubular epithelial cell apoptosis and EMT have been proposed as putative primary pathomechanisms that may underlie progressive renal disease.10
There are only a few data available to support the hypothesis that EMT has a role in human ADPKD. Complex mechanisms induce the EMT. However, it is not certain which factors are associated with EMT in ADPKD. To evaluate this hypothesis in human ADPKD, therefore, we immunohistochemically studied the expression of several makers of EMT.
PATIENTS AND METHODS
Patients
Informed consent was obtained from all patients. Elective transplant removal of ADPKD kidney was performed on renal graft recipients at the Samsung Medical Center. Normal renal tissue was obtained from tumor nephrectomies; tumor infiltration was excluded by histology. Tissue samples were fixed in 4% paraformaldehyde for immunohistochemistry immediately after organ removal. ADPKD kidneys from 5 patients (male : female = 3 : 2, age 54 ± 7 years) who developed ESRD and control renal tissues from 4 patients (male : female = 2 : 2, age 58 ± 9 years) with renal cell carcinoma and normal renal function were analyzed by immnunohistochemistry.
Methods
A part of each kidney was fixed in 4% paraformaldehyde and was embedded in paraffin. Sections were cut 4 µm in thickness from paraffin blocks and processed for hematoxylin-eosin and indirect immunoperoxidase staining. After deparaffinization and rehydration, the sections were treated with proteinase K and boiled with citrate buffer in microwave for antigen retrieval. After washing, they were immersed in 3% H2O2 in methanol to inhibit endogenous peroxidase and flooded with 5% bovine albumin in PBS to inhibit nonspecific reactions. Anti-α-SMA (Dako, Glostrup, Denmark), anti-E-cadherin (Zymed Lab, San Fransisco, CA, USA), anti-vimentin (Dako, Glostrup, Denmark), anti-TGF-β1 (Santa Cruz Biotech, Santa Cruz, CA, USA), and anti-Smad 2/3 (Santa Cruz Biotech, Santa Cruz, CA, USA) were applied as primary antibodies. Following primary immunoreaction, labelling was performed using streptavidin-biotin immunoperoxidase method (Nichirei Bioscience, Tokyo, Japan), and a Vectastain ABC kit (Vector Laboratories, Burlingame, CA, USA). Tissues were visualized using diaminobenzidine (DAB) as a chromogene (brown).
Images were captured by Baumer digital camera with olympus BX51 microscopy. Image analysis was accomplished using the public domain software ImageJ (available at http://rsb.info.nih.gov/ij). Operations during analysis consisted of converting the images to 8-bit grey scale [256 scales of grey, ranging from 0 (black) to 255 (white)], plotting the distribution of grey values, thresholding and measuring total area of positive cells automatically. For manual counting of positive tubules, several randomly selected fields, totaling 0.25 mm2 from the center area of the well were used. Positive tubules (%) were the percent of positive tubules/total tubules (× 200).
All results were analyzed using SPSS 12.0 and expressed as mean ± standard deviation. Statistical significances (p < 0.05) were analyzed by using the Mann-Whitney test.
RESULTS
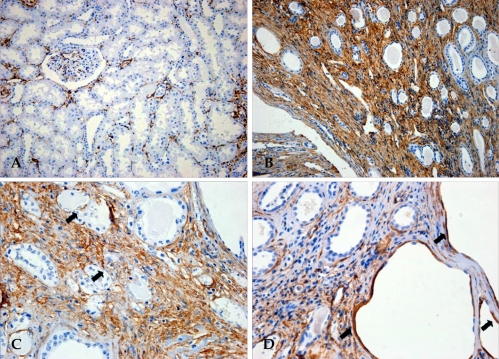
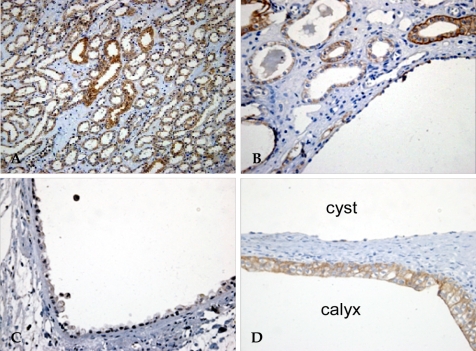
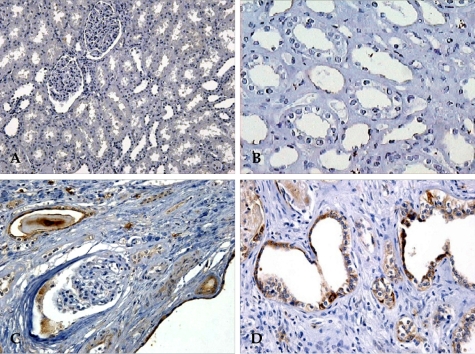
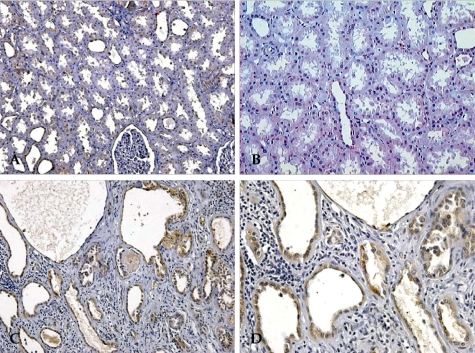
There were severe interstitial fibrosis and proliferation of α-SMA+ myofibroblasts in ADPKD compared to control kidneys. In ADPKD, tubular epithelial cells of dilated cysts were occasionally α-SMA+ (Fig. 1). E-cadherin is an epithelial cell marker. There were some portions with decreased expression in cystic epithelial cells of large renal cysts in ADPKD (Fig. 2). Vimentin is a mesenchymal cell marker, and it's vimentin expression was increased in the stromal and cystic epithelial cells in ADPKD kidneys (Fig. 3). TGF-β1 and Smad 2/3 were regulated upward in cystic epithelial cells (Figs. 4 and 5).
Fig. 1.
Immunohistochemical staining for α-SMA. α-SMA is a mesenchymal and myofibroblast marker. In normal kidneys, α-SMA was negative for tubular epithelial cells; there were a few positive myofibroblasts in the interstitium (A, × 200). In ADPKD kidneys, the stromal cells were diffusely positive (B, × 200), and occasional epithelial cells in the dilated cysts were positive (C and D, × 400, arrows). α-SMA, α-smooth muscle actin; ADPKD, autosomal dominant polycystic kidney disease.
Fig. 2.
Immunohistochemical staining for E-cadherin. E-cadherin is an epithelial cell marker. E-cadherin was widely expressed in distal tubular and collecting duct epithelial cells of normal kidneys (A, × 200). In ADPKD kidneys, the E-cadherin expression pattern was heterogeneous; there were portions in cystic epithelial cells of large renal cysts with decreased expression (B, × 200, C and D, × 400). ADPKD, autosomal dominant kidney disease.
Fig. 3.
Immunohistochemical staining for vimentin. Vimentin is a mesenchymal cell marker. Vimentin was positive in a few tubular epithelial cells of normal kidneys (A and B, × 200). In ADPKD kidneys, vimentin expression was increased in the stromal and cystic epithelial cells (C, × 200 and D, × 400). ADPKD, autosomal dominant kidney disease.
Fig. 4.
Immunohistochemical staining for TGF-β1. TGF-β1 was negative in the normal kidneys (A, × 200 and B, × 400). In ADPKD kidneys, TGF-β1 was upregulated in cystic epithelial cells (C and D, × 400). TGF-β1, transforming growth factor-β1; ADPKD, autosomal dominant kidney disease.
Fig. 5.
Immunohistochemical staining for Smad 2/3. Smad 2/3 showed sparse weakly positive cells in the normal kidneys (A, × 200 and B, × 400). The cystic epithelial cells showed moderately positive reactions in ADPKD kidneys (C and D, × 400). ADPKD, autosomal dominant kidney disease.
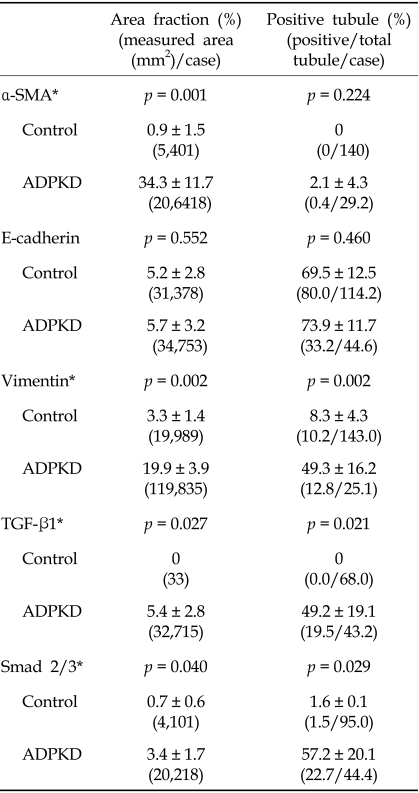
These immunohistochemical findings were quantitatively summarized by computer-assisted image analyzer and positive tubules (%) (Table 1). There were significant increases of α-SMA (34.3 ± 11.7 vs 0.9 ± 1.5), vimentin (19.9 ± 3.9 vs 3.3 ± 1.4), TGF-β1 (5.42 ± 2.83 vs 0) and Smad 2/3 (3.4 ± 1.7 vs 0.7 ± 0.6) in ADPKD kidneys than control kidneys, demonstrated by computer-assisted image analyzer. When we analyzed the positive tubules (%), the results were the same as computer-assisted image analyzer. Large cystic tubular cells in ADPKD showed many α-SMA+, vimentin++ and E-cadherin- (Table 2).
Table 1.
Immunohistochemical Results in Control and ADPKD by Morphometry Using a Color Image Analysis and Tubular Count
ADPKD, autosomal dominant polycystic kidney disease; α-SMA, α-smooth muscle actin; TGF-β1, transforming growth factor-β1.
Area fractions (%) are evaluated by color image analysis for 4 fields each specimen (× 200).
Positive tubules (%) are evaluated as percent of positive tubules/total tubules (× 200).
Data are shown as mean ± SD.
*p < 0.05.
Table 2.
Location of Phenotypic Markers in ADPKD
ADPKD, autosomal dominant polycystic kidney disease; TE, tubular epithelium; α-SMA, α-smooth muscle actin; TGF-β1, transforming growth factor-β1.
DISCUSSION
Human ADPKD is a heterogenic genetic disorder that progresses to ESRD. Progression to ESRD in ADPKD is associated with not only forming cysts, but also the accumulation of interstitial collagens, presumably because of proliferation of fibroblasts.4,11 As cysts arise from only a small percentage of nephrons, other downstream mechanisms are important in progression to ESRD in ADPKD. In our study, proliferation of α-SMA+ myofibroblasts and interstitial fibrosis were key features of ADPKD with ESRD. α-SMA is normally synthesized by vascular smooth muscle cells and myofibroblasts differ from fibroblasts in granulation tissue. The origin of contractile myofibroblasts has not been easy to characterize. The conventional view is that these myofibroblsts are originated by differentiation of resident renal fibroblast, or migration of pericytes, or tubular epithelia cells by EMT.
EMT and transdifferentiation are concepts which originally belong to embryology and oncology. Cell shifting between epithelial and mesenchymal phenotype, by turning on and off specific genes during development, is a well recognized mechanism that characterizes the embryonal plasticity.12 EMT can also play a key element in metastasis of tumors derived from epithelial tissues.13 Recently emerging evidences suggest that EMT can be an important role in several glomelulonephritis,14,15 peritoneal fibrosis of peritoneal dialysis,16 failing renal transplants17 and diabetic nephropathy.2 However, there are few data of EMT available in human ADPKD.
In a recent study by Okada et al.,8 many nonoverlapping as well as fewer overlapping populations of FSP1+ and α-SMA+ cells shared in the collagen expression were found to be associated with progressive fibrogenesis in pcy mice undergoing cystogenesis. Some FSP1+ fibroblasts are likely derived from tubular epithelium undergoing EMT, whereas α-SMA +, VIM-cells probably represent vascular smooth muscle cells or pericytes surviving vessel attenuation during the chaos of fibrogenesis. A recent study by Schieren et al.9 showed that total of 87 genes in gene profiling of ADPKD were specifically regulated; 26 of these 87 genes were typical for smooth muscle, suggesting EMT as a pathogenetic factor in ADPKD. They showed that smooth muscle actin and caldesmon were mainly expressed in the interstitium of ADPKD kidneys. In our study, tubular epithelial cells in ADPKD lost epithelial marker (E-cadherin) and expressed mesenchymal markers (α-SMA, vimentin). These finding suggest that EMT has an important role in progression in ADPKD.
Since the discovery of TGF-β as a key mediator of glomerular and tubulointerstitial fibrosis in many chronic kidney diseases over a decade ago, studies of TGF-β signaling had been focused on the cell proliferation and extracellular-matirx synthesis.18 In recent years, TGF-β signaling was found to play central role in renal fibrosis19 by EMT.20,21 In the present study, we showed that TGF-β-Smad signaling was regulated upward in ADPKD, thus suggesting that TGF-β-Smad signaling is associated with renal EMT and renal fibrosis in ADPKD. It is highly likely that cyst cell proliferation and fluid secretion initiated the renal cysts, that enlarged cyst then stretched tubular cells that would secrete the TGF-β, and that increased TGF-β mediated EMT and interstitial fibrosis. In future studies, therefore, we plan to suppress TGF-β and EMT to delay the clinical course to ESRD in ADPKD.
In summary, α-SMA+ myofibroblasts and interstitial fibrosis were key features of ADPKD with ESRD. Cystic tubular epithelial cells lost epithelial marker and expressed mesenchymal markers. TGF-β-Smad signaling was regulated upward in ADPKD, suggesting that TGF-β mediated EMT has a role in progression of ADPKD.
Footnotes
This study was supported by IN-SUNG Foundation for Medical Research.
References
- 1.Ong AC, Harris PC. Molecular pathogenesis of ADPKD: the polycystin complex gets complex. Kidney Int. 2005;67:1234–1247. doi: 10.1111/j.1523-1755.2005.00201.x. [DOI] [PubMed] [Google Scholar]
- 2.Simonson MS. Phenotypic transitions and fibrosis in diabetic nephropathy. Kidney Int. 2007;71:846–854. doi: 10.1038/sj.ki.5002180. [DOI] [PubMed] [Google Scholar]
- 3.Simons M, Walz G. Polycystic kidney disease: cell division without a c(l)ue? Kidney Int. 2006;70:854–864. doi: 10.1038/sj.ki.5001534. [DOI] [PubMed] [Google Scholar]
- 4.Zeier M, Fehrenbach P, Geberth S, Möhring K, Waldherr R, Ritz E. Renal histology in polycystic kidney disease with incipient and advanced renal failure. Kidney Int. 1992;42:1259–1265. doi: 10.1038/ki.1992.413. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y. Epithelial to mesenchymal transition in renal fibrogenesis: pathologic significance, molecular mechanism, and therapeutic intervention. J Am Soc Nephrol. 2004;15:1–12. doi: 10.1097/01.asn.0000106015.29070.e7. [DOI] [PubMed] [Google Scholar]
- 6.Iwano M, Plieth D, Danoff TM, Xue C, Okada H, Neilson EG. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest. 2002;110:341–350. doi: 10.1172/JCI15518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang J, Liu Y. Dissection of key events in tubular epithelial to myofibroblast transition and its implications in renal interstitial fibrosis. Am J Pathol. 2001;159:1465–1475. doi: 10.1016/S0002-9440(10)62533-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okada H, Ban S, Nagao S, Takahashi H, Suzuki H, Neilson EG. Progressive renal fibrosis in murine polycystic kidney disease: an immunohistochemical observation. Kidney Int. 2000;58:587–597. doi: 10.1046/j.1523-1755.2000.00205.x. [DOI] [PubMed] [Google Scholar]
- 9.Schieren G, Rumberger B, Klein M, Kreutz C, Wilpert J, Geyer M, et al. Gene profiling of polycystic kidneys. Nephrol Dial Transplant. 2006;21:1816–1824. doi: 10.1093/ndt/gfl071. [DOI] [PubMed] [Google Scholar]
- 10.Böttinger EP, Bitzer M. TGF-beta signaling in renal disease. J Am Soc Nephrol. 2002;13:2600–2610. doi: 10.1097/01.asn.0000033611.79556.ae. [DOI] [PubMed] [Google Scholar]
- 11.Wilson PD, Norman JT, Kuo NT, Burrow CR. Abnormalities in extracellular matrix regulation in autosomal dominant polycystic kidney disease. Contrib Nephrol. 1996;118:126–134. doi: 10.1159/000425085. [DOI] [PubMed] [Google Scholar]
- 12.Thiery JP, Sleeman JP. Complex networks orchestrate epithelial-mesenchymal transitions. Nat Rev Mol Cell Biol. 2006;7:131–142. doi: 10.1038/nrm1835. [DOI] [PubMed] [Google Scholar]
- 13.Thompson EW, Newgreen DF, Tarin D. Carcinoma invasion and metastasis: a role for epithelial-mesenchymal transition? Cancer Res. 2005;65:5991–5995. doi: 10.1158/0008-5472.CAN-05-0616. discussion 5995. [DOI] [PubMed] [Google Scholar]
- 14.Rastaldi MP, Ferrario F, Giardino L, Dell'Antonio G, Grillo C, Grillo P, et al. Epithelial-mesenchymal transition of tubular epithelial cells in human renal biopsies. Kidney Int. 2002;62:137–146. doi: 10.1046/j.1523-1755.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 15.Jinde K, Nikolic-Paterson DJ, Huang XR, Sakai H, Kurokawa K, Atkins RC, et al. Tubular phenotypic change in progressive tubulointerstitial fibrosis in human glomerulonephritis. Am J Kidney Dis. 2001;38:761–769. doi: 10.1053/ajkd.2001.27693. [DOI] [PubMed] [Google Scholar]
- 16.Yáñez-Mó M, Lara-Pezzi E, Selgas R, Ramírez-Huesca M, Domínguez-Jiménez C, Jiménez-Heffernan JA, et al. Peritoneal dialysis and epithelial-to-mesenchymal transition of mesothelial cells. N Engl J Med. 2003;348:403–413. doi: 10.1056/NEJMoa020809. [DOI] [PubMed] [Google Scholar]
- 17.Vongwiwatana A, Tasanarong A, Rayner DC, Melk A, Halloran PF. Epithelial to mesenchymal transition during late deterioration of human kidney transplants: the role of tubular cells in fibrogenesis. Am J Transplant. 2005;5:1367–1374. doi: 10.1111/j.1600-6143.2005.00843.x. [DOI] [PubMed] [Google Scholar]
- 18.Blobe GC, Schiemann WP, Lodish HF. Role of transforming growth factor beta in human disease. N Engl J Med. 2000;342:1350–1358. doi: 10.1056/NEJM200005043421807. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y. Renal fibrosis: new insights into the pathogenesis and therapeutics. Kidney Int. 2006;69:213–217. doi: 10.1038/sj.ki.5000054. [DOI] [PubMed] [Google Scholar]
- 20.Zavadil J, Böttinger EP. TGF-beta and epithelial-to-mesenchymal transitions. Oncogene. 2005;24:5764–5774. doi: 10.1038/sj.onc.1208927. [DOI] [PubMed] [Google Scholar]
- 21.Roberts AB, Tian F, Byfield SD, Stuelten C, Ooshima A, Saika S, et al. Smad3 is key to TGF-beta-mediated epithelial-to-mesenchymal transition, fibrosis, tumor suppression and metastasis. Cytokine Growth Factor Rev. 2006;17:19–27. doi: 10.1016/j.cytogfr.2005.09.008. [DOI] [PubMed] [Google Scholar]