Abstract
Purpose
We describe the epidemiological and clinical characteristics and the efficacy of a delayed initiation to therapy in an oropharyngeal tularemia outbreak in Duzce, Turkey.
Materials and Methods
Between March and June 2000, 22 patients with tularemia were diagnosed by microagglutination tests.
Results
Oropharyngeal and ulceroglandular forms of the disease were discovered. Most of the cases were oropharyngeal (19 cases). The most common symptoms were sore throat (95.4%) and fever (90.9%). Lymphadenopathy (95.4%) and pharyngeal hyperemia (81.8%) were usually observed signs. The lymphadenopathies were localized especially in the left cervical region (66.7%), a finding that has not been previously reported in the literature. The time between the onset of the symptoms and diagnosis was 40.7 ± 22.8 (10 - 90) days. The patients were treated with streptomycin plus doxycycline and ciprofloxacin. The patients' recoveries took up to 120 days.
Conclusion
This report describes the first outbreak of tularemia in northwest Turkey. Tularemia may occur in any region where appropriate epidemiological conditions are found and should be kept in mind for differential diagnosis in oropharyngeal symptoms. Late initiation of therapy may delay complete recovery. In this outbreak, cervical lymph nodes predominantly localized on the 1eft side were found, which had not been previously reported.
Keywords: Outbreak, tularemia, waterborne, oropharyngeal, left cervical lymph nodes
INTRODUCTION
There are many reservoirs of F. tularencis in many parts of the world, including ticks and rodents, which may be associated with unusual increases in population density of these animal hosts.1-5 Depending on the mode of transmission, tularemia presents various clinical forms, such as ulceroglandular, glandular, oculoglandular, oropharyngeal, pneumonic, and typhoidal tularemia forms. As an intracellular pathogen, F. tularensis, causes granulomatosus and suppurative lesions especially in the affected regional lymph nodes and various organs.5-8 Diagnosis of tularemia mainly depends on serological tests such as microagglutination, enzyme immune assay (EIA), immunochromatography, and PCR.4,9,10 Without antimicrobial treatment, tularemia can be acute and fulminant or protracted and debilitating. Streptomycin, gentamicin, tetracycline, and fluoroqinolone antibiotics are effective, and early initiation of these agents is important in the effective treatment.5,8,11,12
Tularemia has been reported in different parts of Turkey since 1936.13 The present paper reports the clinical characteristics of 22 patients who were diagnosed with tularemia between March and June 2000 from Duzce (north-western Turkey). The aim of the study was to draw attention to the fact that tularemia may be found where there are differential diagnosis of patients with oropharyngeal symptoms and lymphadenopathy.
MATERIALS AND METHODS
A total of 22 patients were diagnosed with tularemia between March and June 2000, in the Department of Clinical Microbiology and Infectious Diseases, Abant Izzet Baysal University School of Medicine (Duzce, Turkey). All patients came from two neighbouring villages that were situated in a forest region of Duzce-Akcakoca, in north-western Turkey.
By using a clinical history protocol, the following data were collected for all patients: symptoms, physical signs, and results of laboratory tests. All patients with suspected tularemia were physically examined. Detailed information about their occupation, the site of infection, day of onset, insect bites, contact with animals, working in poultry houses, clinical symptoms, and so on was obtained using an applied questionnaire. The sanitary conditions the water sources of these villages were examined.
The microagglutination tests for the tularemia diagnosis were performed in Uludag University, School of Medicine. The diagnosis was considered positive when the patient had an F. tularensis microagglutination titer of ≥ 1 : 40 or when seroconversion was present.10,13 Before the diagnosis of tularemia, 15 patients had been using betalactam antibiotics and four patients had been using gentamicin in addition to beta-lactams, which was prescribed by their local practitioner. After the confirmation of tularemia, tetracycline plus streptomycin was used for 15 patients, and one patient was administered ciprofloxacin and another streptomycin. Therapeutic failure was defined by the presence of one of the following findings: persistence or recurrence of fever, increase in the size or appearance of new lymphadenopathies, and persistence of the constitutional syndrome with the elevation of the levels of the proteins that are associated with the acute phase of infection.6,14 Disappearance of all signs and symptoms except for stationary lymphadenomegaly was accepted as a cure.
Fisher's Chi-square test was used for statistical analysis.
RESULTS
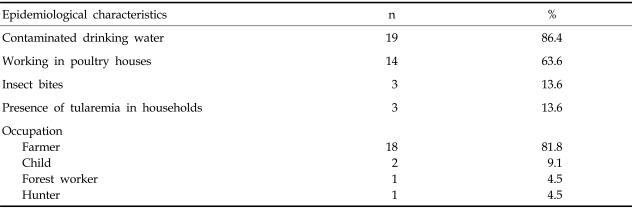
A total of 22 patients (11 females, and 11 males) were diagnosed with tularemia. The mean age (Mean ± SD) of the patients was 34.9 ± 17.2 (11 - 70) years. None of the patients had a previous clinical history of tularemia. Three patients (13.6%) had a clinical history or signs of tick bites. For 19 patients (86.4%) the water sources were not suitable as drinking water. The most important epidemiological finding was that poultry farm work was the most common livelihood in this region, and increased rodent activity around poultry houses and villages had been reported by residents during the previous year. Furthermore, people living in the two villages were using water that was not treated with any disinfection or chlorination procedures. The water springs were contaminated with rattus and other wild rodent excrements. One rattus carcass was found in one of the village wells. The epidemiologic characteristics of the patients with tularemia are shown in Table 1.
Table 1.
Epidemiologic Characteristics of the Patients with Tularemia
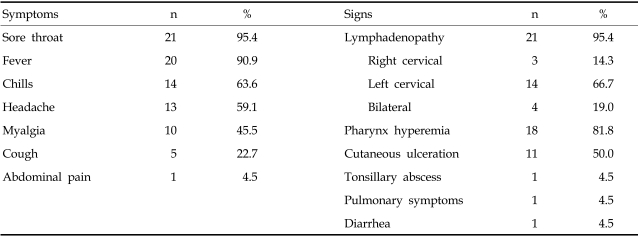
The time between the onset of the symptoms and diagnosis was 40.7 ± 22.8 (10 - 90) days. The most frequent symptoms were sore throat (95.4%) and fever (90.9%). Lymphadenopathy (95.4%) and pharyngeal hyperemia (81.8%) were the most frequent signs. The lymphadenopathies were localized in the cervical region, especially in the left cervical area (66.7%). Three patients had a clinical history of tick bites, ulcero-nodular lesions 0.5 cm in diameter on the left forearm, and cervical lymphadenopathy. The oropharyngeal form was the most frequent with 19 cases, and the Ulceroglandular form was observed in 3 cases. The symptoms and signs of the patients are presented in Table 2.
Table 2.
Symptoms and Signs in Patients (n = 22)
The results from the patients' laboratory tests were normal, except for an increase in the levels of tests in ESR: 56 ± 16 mm/hour and leukocytosis in blood: 11, 8 × 109/L ± 2, 1 × 109/L were observed. Serological diagnosis was put on the basis of the following findings; the antibody titer against F. tularencis was found to be over 1/160 in 10 and 1/80 in 6 patients' sera. A four-fold rise of the antibody titer was determined in 6 cases. Brucella agglutination tests and anti-EBV IgM antibody with EIA were found negative.
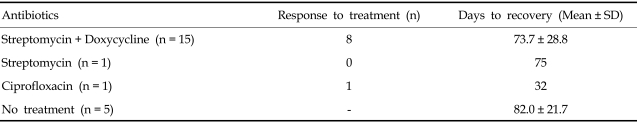
The patients were treated with intramuscularly administered streptomycin at a dosage of either 1g every 24 hours or 500 mg every 12 hours for 10 - 14 days, plus doxycycline (100 mg orally every 12 hours for 2 weeks) and, in the case of one patient, with ciprofloxacin (500 mg iv every 12 hours for 14 days). No treatment was used for the 5 patients who had been treated before for differential diagnosis. All of the patients recovered within 120 days. The antibiotics used for the treatment of tularemia, responses to treatments, and recovery times are shown in Table 3.
Table 3.
Treatment Characteristics of the Patients (n = 22)
DISCUSSION
Tularemia is transmitted to humans through various modes, including the direct handling of infectious carcasses, ingestion of contaminated food or water, arthropod bites, or inhalation of infectious dusts or aerosols. However, the principal port of entry is through the skin.2,3,5 F. tularensis has been isolated in wells that contained dead rodents and carcasses.4,5
No previous epidemic had been reported in this region of Turkey. Residents reported increased rodent activity around poultry houses and villages the previous year. The increases in rodent activity were probably due to insufficient wasting of hen carcasses in poultry houses. The present outbreak was considered waterborne because the water springs of these villages were contaminated with rattus and other wild rodent excrements. Reintjes R et al.5 reported that, in rural areas, farmers were the most affected in the Kosova outbreak, which occurred in March 2000. In addition, rodents were found to be responsible for contaminating water supplies and food storage. The increases in local rodent populations were related to food storage areas that had been left unprotected and crops that had been left unharvested.
In this outbreak, the principal form of tularemia was the oropharyngeal form (19 cases), and the probable port of entry of the organisms was the oropharyngeal route. Clinical signs and symptoms that support the oropharyngeal route theory are as follows: 21 patients had a sore throat, 18 had pharyngeal hyperemia, and 21 had cervical lymphadenopathy.
In the Southwest-central states of the US, 1,026 cases were analyzed between 1981 - 1987. The most frequent symptoms were fever (96%), lymphadenopathy (77%), and cutaneous ulcers (65%).15 Christenson B et al.16 evaluated 344 tularemia patients in a northern part of central Sweden, and the most frequent symptoms there were fever (94%), lymphadenopathy (87%), chills (83%), muscle pain (55%), and sore throat (22%). Helvacı et al.17 reported 205 patients with tularemia in Turkey, and lymphadenopathy (85%) was found to be the most frequent sign. Reintjes R et al.5 reported several hundred cases with a clinical picture of fever, pharyngitis, and cervical lymphadenitis, together with serologic confirmation.
In the present outbreak, the oropharyngeal form was found to be very high (86.4%). In contrast to reports in the literature,1 most of the cases reported from Turkey and Kosova were in the oropharyngeal form. The clinical form in two neighbouring countries may be related to a common biotype of F. tularencis and a similar port entry.
In Japan, Ohara et al.18 had observed swelling of axillary, cubital, and brachial lymph nodes predominantly on the left side in 1,355 cases between the years 1924 - 1987, and the authors explained that this situation may be due to the fact that right-handed persons held the captured animal firmly with the left hand while cooking. In this outbreak, lymphadenopathies predominantly were localized in the cervical region, especially on the left side (66.7%). This situation may be related to the localization of oropharyngeal ulcers, but we can make no further comment about this. Oropharyngeal tularemia may be easily confused with other diseases that affect the cervical lymph nodes, such as streptococcus angina, tuberculosis, infectious mononucleosis, and lymphoma.6 This may lead to late diagnosis and inadequate treatment, as it was the case with the present epidemic. The delay was due to the novelty of this illness to the region. Tularemia should be considered in differential diagnoses where cervical lymphadenopathy is involved.
The recommended agents for the treatment of tularemia include aminoglycosides (streptomycin and gentamicin) and tetracyclines.8,12 It was demonstrated that ten strains of F. tularensis had in vitro susceptibility to ciprofloxacin, norfloxacin, ofloxacin, and pefloxacin.19 The fluoroquinolones were found to be an excellent alternative. When therapy is not initiated within a few days of illness, defervescence may be delayed, and suppuration may progress in spite of effective treatment.1,19 In the present outbreak, ciprofloxacin was used for only one patient, and a good result was obtained with this drug. Fifteen of the patients used a treatment of streptomycin plus doxycycline. No treatment was used for five patients who had been using various antibiotics, such as gentamicin, and whose disease had a mild clinical course. There were no significant differences between the different treatment protocols. The therapeutic failure that was observed in 8 patients may be related to the delay in the initiation of antibiotic therapy and the presence of fluctuating lymphadenopathies. The prognosis of the patients was good, and no patient died.
What follows is a summary of findings: this is the first reported outbreak of oropharyngeal tularemia in our region. It appears that Tularemia was acquired through contact with water that was contaminated by rodents. An increase in the number of rodents may be related to the waste from poultry houses. The Oropharyngeal form of the disease was the most frequent, as it was in other outbreaks reported from Turkey and Kosova. In this outbreak, one of the interesting findings that had not been previously reported was the repeated cases of cervical lymphadenopathies on the left.
ACKNOWLEDGEMENTS
We thank the Head of Clinical Microbiology and Infectious Diseases, University of Uludag, School of Medicine for studying the microagglutination test of sera.
References
- 1.Jacobs RF. Fauci AS, Braunwald F, Isselbach RJ, Wilson JD, Martin JB, Kasper DL, et al. Harrison's principles of internal medicine. New York: McGraw-Hill; 1998. Tularemia; pp. 971–975. [Google Scholar]
- 2.Maranan MC, Schiff D, Johnson DC, Abrahams C, Wylam M, Gerber SI. Pneumonic tularemia in a patient with chronic granulomatous disease. Clin Infect Dis. 1997;25:630–633. doi: 10.1086/513777. [DOI] [PubMed] [Google Scholar]
- 3.Byrd RP, Jr, Vasquez J, Roy TM. Respiratory manifestation of tick-borne diseases in the Southeastern United States. South Med J. 1997;90:1–4. doi: 10.1097/00007611-199701000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Berdal BP, Mehl R, Haaheim H, Løksa M, Grunow R, Buran S, et al. Field detection of Francisella tularensis. Scand J Infect Dis. 2000;32:287–291. doi: 10.1080/00365540050165938. [DOI] [PubMed] [Google Scholar]
- 5.Reintjes R, Dedushaj I, Gjini A, Jorgensen TR, Cotter B, Lieftucht A, et al. Tularemia outbreak investigation in Kosovo: case control and environmental studies. Emerg Infect Dis. 2002;8:69–73. doi: 10.3201/eid0801.010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tärnvik A, Sandström G, Sjöstedt A. Infrequent manifestations of tularaemia in Sweden. Scand J Infect Dis. 1997;29:443–446. doi: 10.3109/00365549709011851. [DOI] [PubMed] [Google Scholar]
- 7.Penn RL. Francisella tularensis (Tularemia) In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett's principles and practice of infectious diseases. 4th ed. New York: Churchill Ligingstone; 1995. pp. 2060–2068. [Google Scholar]
- 8.Syrjälä H, Kujala P, Myllylä V, Salminen A. Airborne transmission of tularemia in farmers. Scand J Infect Dis. 1985;17:371–375. doi: 10.3109/13813458509058777. [DOI] [PubMed] [Google Scholar]
- 9.de la Puente-Redondo VA, del Blanco NG, Gutiérrez-Martín CB, García-Peña FJ, Rodríguez Ferri EF. Comparison of different PCR approaches for typing of Francisella tularensis strains. J Clin Microbiol. 2000;38:1016–1022. doi: 10.1128/jcm.38.3.1016-1022.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sato T, Fujita H, Ohara Y, Homma M. Microagglutination test for early specific serodiagnosis of tularemia. J Clin Microbiol. 1990;28:2372–2374. doi: 10.1128/jcm.28.10.2372-2374.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Enderlin G, Morales L, Jacobs RF, Cross JT. Streptomycin and alternative agents for the treatment of tularemia: review of the literature. Clin Infect Dis. 1994;19:42–47. doi: 10.1093/clinids/19.1.42. [DOI] [PubMed] [Google Scholar]
- 12.Baker CN, Hollis DG, Thornsberry C. Antimicrobial susceptibility testing of Francisella tularensis with a modified Mueller-Hinton broth. J Clin Microbiol. 1985;22:212–215. doi: 10.1128/jcm.22.2.212-215.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akdiş AC, Kiliçturgay K, Helvaci S, Mistik R, Oral B. Immunological evaluation of erythema nodosum in tularaemia. Br J Dermatol. 1993;129:275–279. doi: 10.1111/j.1365-2133.1993.tb11846.x. [DOI] [PubMed] [Google Scholar]
- 14.Pérez-Castrillón JL, Bachiller-Luque P, Martín-Luquero M, Mena-Marbín FJ, Herreros V. Tularemia epidemic in northwestern Spain: clinical description and therapeutic response. Clin Infect Dis. 2001;33:573–576. doi: 10.1086/322601. [DOI] [PubMed] [Google Scholar]
- 15.Taylor JP, Istre GR, McChesney TC, Satalowich FT, Parker RL, McFarland LM. Epidemiologic characteristics of human tularemia in the southwest-central states, 1981-1987. Am J Epidemiol. 1999;133:1032–1038. doi: 10.1093/oxfordjournals.aje.a115812. [DOI] [PubMed] [Google Scholar]
- 16.Christenson B. An outbreak of tularemia in the northern part of central Sweden. Scand J Infect Dis. 1984;16:285–290. doi: 10.3109/00365548409070402. [DOI] [PubMed] [Google Scholar]
- 17.Helvaci S, Gedikoğlu S, Akalin H, Oral HB. Tularemia in Bursa, Turkey: 205 cases in ten years. Eur J Epidemiol. 2000;16:271–276. doi: 10.1023/a:1007610724801. [DOI] [PubMed] [Google Scholar]
- 18.Ohara Y, Sato T, Fujita H, Ueno T, Homma M. Clinical manifestations of tularemia in Japan-analysis of 1,355 cases observed between 1924 and 1987. Infection. 1991;19:14–17. doi: 10.1007/BF01643750. [DOI] [PubMed] [Google Scholar]
- 19.Syrjälä H, Schildt R, Räisäinen S. In vitro susceptibility of Francisella tularensis to fluoroquinolones and treatment of tularemia with norfloxacin and ciprofloxacin. Eur J Clin Microbiol Infect Dis. 1991;10:68–70. doi: 10.1007/BF01964409. [DOI] [PubMed] [Google Scholar]