Abstract
Background
Reducing hospitalizations and emergency room visits is important to improve patient outcomes. This observational study examined the association between adherence to antipsychotics and risk of hospitalizations and emergency room (ER) visits among patients with bipolar disorder.
Methods
Claims data from commercial healthcare plans (Pharmetrics; January 2000 to December 2006) for patients with bipolar disorder receiving an antipsychotic prescription were examined. Adherence was analyzed over a 12-month follow-up period after the receipt of first prescription of an antipsychotic. Adherence to antipsychotics was measured by the medication possession ratio (MPR). The MPR was calculated as the number of days that an antipsychotic medication was filled as compared with the total number of days during the follow-up period. Logistic stepwise regressions examined the association between achievement of various adherence goals and patient outcomes (hospitalization or ER visit for mental health or any reason).
Results
In total, 7,769 patients with bipolar disorder were included. The mean MPR was 0.417, with 61.7% of individuals having an MPR < 0.50, and 78.7% an MPR < 0.75. As adherence improved, the risk of hospitalization or ER visit declined. A significant reduction in the risk of hospitalization (odds ratio (OR) 0.85, 95% confidence interval (CI) 0.75 to 0.98) or an ER visit (OR 0.84, 95% CI 0.74 to 0.96) for any cause was associated with an MPR ≥ 0.75. An MPR ≥ 0.80 was associated with a significant reduction in the risk of a mental health-related hospitalization (OR 0.82, 95% CI 0.70 to 0.95), while an MPR ≥ 0.90 was associated with a significant reduction in risk of a mental health-related ER visit (OR 0.71, 95% CI 0.54 to 0.91).
Conclusion
Patients with lower antipsychotic adherence were at greater risk of hospitalizations and ER visits. Thus, any efforts to increase adherence, even in small increments, can be helpful in decreasing these risks.
Introduction
As the sixth leading cause of disability worldwide [1], bipolar disorder affects approximately 5.7 million American adults, or about 2.6% of the US population aged 18 and older, annually [2]. A recent study of records from the annual National Hospital Discharge Survey (NHDS) reported that the population-adjusted rates of hospital discharges with a primary diagnosis of bipolar disorder grew significantly between 1996 and 2004 among all age groups [3], with the adult rate rising markedly, by 56%. While bipolar disorder has a spectrum of expression, the classic form of the illness, in which a person experiences recurrent episodes of mania and depression, is bipolar I disorder [4].
The direct costs of bipolar disorder are substantial and include inpatient hospitalization, outpatient general and specialist visits, nursing home, intermediate, and domiciliary care, medication, substance abuse treatment, and costs of supported living [5]. To date, two US cost-of-illness studies, one prevalence-based and the other incidence-based, have been conducted specifically on bipolar disorder [5,6]. The prevalence-based study estimated the direct, annual costs of the disease to be $7.6 billion (in 1991 US dollars) [5], while the incidence-based study reported the lifetime, direct costs for cases of bipolar disorder diagnosed in 1998 to be $13 billion [6]. When considering the costs of medical care, a study that assessed health care claims from a database of 1.66 million people insured through more than 900 employers determined bipolar disorder to be the most expensive behavioral health diagnosis [7]. Moreover, it has been shown to be the most expensive mental health condition among employees of six large US corporations [8]. In a recent analysis, direct, per-patient costs were $3,000 (in 2004 US dollars) higher for patients with bipolar disorder than for patients with non-bipolar depression (p < 0.001), with the primary differences observed for psychiatric medication ($1,641 vs $507) and psychiatric hospitalization ($1,187 vs $241) [9]. Other research has also shown that inpatient care is a key driver of medical costs for patients with mental illness and, in particular, bipolar disorder [5,10].
As the costs of bipolar disorder are very high, both to the patient and the health care community, finding ways to decrease unnecessary financial and personal costs is important. Though, bipolar disorder poses significant treatment challenges due to the severity and varied nature of the illness, patients can be stabilized and managed with proper treatment [11,12]. In most cases, bipolar disorder can be better controlled and outcomes are improved if the patients are adherent to their medication regimen [13-16]. However, medication adherence is a critical problem among bipolar disorder patients. Adherence to mood stabilizers and valproates, commonly used pharmacotherapy in bipolar disorder, is about 20 to 60% [13,15,17,18]. Adherence to atypical antipsychotics, recently approved for bipolar disorders, is relatively less studied; although one study did report that nearly half (48.1%) of patients taking antipsychotics to treat bipolar disorder are partially adherent or non-adherent with their medications [19].
The objective of our study is to evaluate various levels of adherence to antipsychotics among bipolar disorder patients and examine if increasing antipsychotic adherence can help to diminish the risk of hospitalization or emergency room (ER) visits. In this study, we examined the impact of different degrees of antipsychotic medication adherence on the risk of hospitalization or ER visits among individuals diagnosed with bipolar disorder.
Methods
Data collection and study population
This retrospective cohort study evaluated claims data from the Pharmetrics database (Watertown, MA, USA) covering the period 1 January 2000 to 31 December 2006. The fully de-identified and Health Insurance Portability and Accountability Act (HIPAA) compliant database contains information on patient demographics and hospitalizations, outpatient service utilization, and outpatient pharmacy data from over 75 different managed care organizations and more than 55 million individuals.
Data were obtained from patients aged between 18 and 64 years with bipolar disorder (identified by paid claims with the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), codes 296.4× to 296.8×) who had received an antipsychotic prescription. The first date of a paid claim for an antipsychotic was defined as the index prescription. All patients included in the study were required to have at least 6 months of continuous enrollment in the same health care plan prior to and 12 months after the date of the index prescription. Given the duration of the preindex and postindex periods, as well as the data collection period, the index date was required to be between 1 July 2000 and 1 January 2006.
Patients with a diagnosis of dementia (ICD-9-CM, code 290.xx) or schizophrenia (ICD-9-CM, code 295.xx) were excluded from the analysis in order to reduce the probability of including patients who were misdiagnosed.
Measures of adherence and outcomes
The medication possession ratio (MPR) was utilized as a measure of adherence, and was calculated as the number of unique days an antipsychotic medication was prescribed in the postindex period divided by the number of days in the same period [20-22]. Therefore, an MPR of 1 indicates that the patient was prescribed an antipsychotic over the complete 12 months following initiation, and that these prescriptions were filled 100% of the time.
The main outcome measures in this analysis were the probability of hospitalization or ER visit for any cause. Additional outcome measures examined the probability of hospitalization or an ER visit with an accompanying mental health diagnosis (ICD-9-CM, codes 290.xx to 319.xx).
Statistical analysis
A series of stepwise logistic multivariate analyses were conducted to assess the relationship between patient outcomes and progressive increases in MPRs (categorized into adherence thresholds of 0.25, 0.50, 0.70, 0.75, 0.80, 0.90, and 0.95) with adjustment for the effect of a wide range of confounding factors. Thus, the analysis controlled for patient demographic characteristics; type of bipolar disorder; patient general health status (including Charlson Comorbidity Index score [23,24], total number of diagnoses, and total number of outpatient prescription medications received in the postindex period); psychiatric prescriptions and specific comorbidities diagnosed in the preindex period (panic disorder, obsessive compulsive disorder and generalized anxiety disorder, attention-deficit hyperactivity, depression, substance abuse, obesity, cardiovascular disease, diabetes, hypertension, and high cholesterol).
MPR and all other variables that reached a threshold of 90% significance were included in the stepwise logistic regressions. By estimating a series of regressions with various MPR thresholds, the multivariate analyses allowed for an examination of how changes in the MPR affect patient outcomes, without artificially compelling a linear relationship between MPR and outcomes, or arbitrarily determining that any particular MPR threshold is appropriate. All analyses were conducted using SAS, version 9.1 (SAS, Cary, NC, USA). Statistical significance was accepted at p ≤ 0.05.
Results
Patient characteristics
Table 1 presents the demographic and clinical characteristics of the 7,769 patients with bipolar disorder included in the study.
Table 1.
Demographic and clinical characteristics of patients with bipolar disorder (n = 7,769)
| Variable | ||
| Mean | SD | |
| Patient characteristics | ||
| Age, years | 39.71 | 12.74 |
| General health, preindex period: | ||
| Charlson Comorbidity Index score | 0.38 | 0.99 |
| Diagnoses, n | 8.20 | 6.19 |
| Prescriptions, n | 6.40 | 5.38 |
| n | % | |
| Sex: | ||
| Female | 4,985 | 64.17 |
| Male | 2,784 | 35.83 |
| Region: | ||
| Midwest | 2,161 | 27.82 |
| Northeast | 2,299 | 29.59 |
| South | 2,262 | 29.12 |
| West | 1,047 | 13.48 |
| Insurance type: | ||
| Commercial | 7,334 | 94.40 |
| Other | 435 | 5.60 |
| Bipolar disorder type: | ||
| Depressed | 1,362 | 17.53 |
| Manic | 923 | 11.88 |
| Mixed | 1,424 | 18.33 |
| Other | 4,060 | 52.26 |
| General health, preindex period: | ||
| Hospitalized | 2,165 | 27.87 |
| Comorbidities, preindex period: | ||
| Panic disorder | 356 | 4.58 |
| Obsessive compulsive disorder | 218 | 2.81 |
| Generalized anxiety disorder | 584 | 7.52 |
| Substance abuse | 1,625 | 20.92 |
| Obesity | 268 | 3.45 |
| Depression | 2,775 | 35.72 |
| Cardiovascular disease | 198 | 2.55 |
| Diabetes | 452 | 5.82 |
| Hypertension | 1,101 | 14.17 |
| High cholesterol | 425 | 5.47 |
| Attention-deficit/hyperactivity | 390 | 5.02 |
| Compliance: | ||
| MPR ≥ 0.25 | 4,540 | 58.44 |
| MPR ≥ 0.50 | 2,776 | 35.73 |
| MPR ≥ 0.75 | 1,509 | 19.42 |
| MPR ≥ 0.80 | 1,229 | 15.82 |
| MPR ≥ 0.90 | 651 | 8.38 |
| MPR ≥ 0.95 | 333 | 4.29 |
MPR, medication possession ratio.
The mean MPR for this cohort was 0.417 (41.7%), with 61.9% having an MPR ≤ 0.50 and 78.7% having an MPR ≤ 0.75. Among the patients included in this cohort, the mean age was 40 years; 64% were female, and the majority were commercially insured (94.4%), with a diagnosis of bipolar type other (52.3%). An examination of the general health status of this population in the 6 months prior to antipsychotic medication initiation revealed that 27.9% had been hospitalized, and that patients had received a mean of 6.2 distinct diagnoses and 5.4 outpatient prescriptions. Depression (35.7%), substance abuse (20.9%), and hypertension (14.2%) were the most common comorbid conditions among patients in the 6 months before antipsychotic medication initiation.
An evaluation of antipsychotic medication use in the 12 months following initiation of antipsychotic treatment showed that the vast majority of individuals were prescribed atypical antipsychotics (Table 2). Notably, 95% of patients were prescribed at least one atypical antipsychotic in the postindex period, while only 10% were prescribed a typical antipsychotic over the same time period. Of the atypical antipsychotic medications used, patients were most likely to be prescribed quetiapine (43.5%), olanzapine (32.2%), or risperidone (26.8%). Of the typical antipsychotic medications, prochlorperazine (6.7%) and haloperidol (1.5%) were the most frequently prescribed medications.
Table 2.
Antipsychotic medication use among patients with bipolar disorder
| Use of drug | Days prescribed | |||
| Medication | n | % | Mean | SD |
| Atypicals: | ||||
| Aripiprazole | 1,354 | 17.43 | 125.71 | 120.88 |
| Clozapine | 6 | 0.08 | 140.67 | 176.62 |
| Olanzapine | 2,502 | 32.20 | 120.76 | 121.26 |
| Fluoxetine/Olanzapine | 316 | 4.07 | 114.78 | 139.2 |
| Quetiapine | 3,376 | 43.45 | 156.85 | 141.55 |
| Risperidone | 2,084 | 26.82 | 124.04 | 124.49 |
| Ziprasidone | 532 | 6.85 | 117.93 | 115.47 |
| Any atypical | 7,378 | 94.97 | 175.08 | 158.77 |
| Typicals: | ||||
| Chlorpromazine | 37 | 0.48 | 99.68 | 134.54 |
| Droperidol | 1 | 0.01 | 1 | |
| Fluphenazine | 12 | 0.15 | 87.25 | 84.06 |
| Haloperidol | 114 | 1.47 | 82.68 | 101.78 |
| Loxapine | 13 | 0.17 | 188.46 | 192.04 |
| Mesoridazine | 0 | 0 | ||
| Molindone | 1 | 0.01 | 60 | |
| Perphenazine | 63 | 0.81 | 127.24 | 128.42 |
| Pimozide | 1 | 0.01 | 30 | |
| Piperacetazine | 0 | 0 | ||
| Prochlorperazine | 518 | 6.67 | 14.96 | 30.975 |
| Promazine | 0 | 0 | ||
| Thioridazine | 16 | 0.21 | 79 | 73.50 |
| Thiothixene | 28 | 0.36 | 162.07 | 164.60 |
| Trifluoperazine | 10 | 0.13 | 268.5 | 226.81 |
| Triflupromazine | 0 | 0 | ||
| Any typical | 779 | 10.03 | 5.27 | 35.01 |
Adherence (medication possession ratio) and hospitalization risk
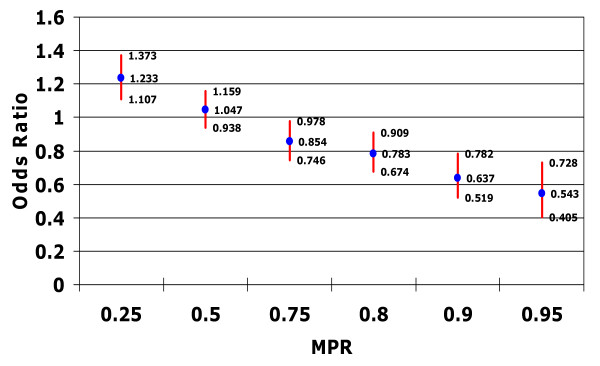
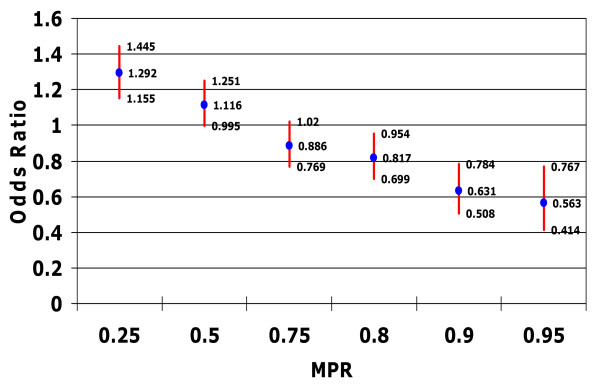
The associations between patient adherence, as measured by MPR, and the probability of hospitalization for any cause or with an accompanying mental health diagnosis are presented in Figures 1 and 2.
Figure 1.
Relationship between medication possession ratio and risk of hospitalization for any cause. Controlling for confounding factors such as patient demographic characteristics; type of bipolar disorder; patient general health status (including Charlson Comorbidity Index score, total number of diagnoses, and total number of outpatient prescription medications received in the postindex period) psychiatric prescriptions; and specific comorbidities diagnosed in the preindex period.
Figure 2.
Relationship between medication possession ratio and risk of hospitalization with mental health diagnosis. Controlling for confounding factors such as patient demographic characteristics; type of bipolar disorder; patient general health status (including Charlson Comorbidity Index score, total number of diagnoses, and total number of outpatient prescription medications received in the postindex period) psychiatric prescriptions; and specific comorbidities diagnosed in the preindex period.
Patients with an MPR threshold of 0.25 had significantly higher odds of hospitalization for any cause compared with patients with an MPR < 0.25 (odds ratio (OR) 1.23, 95% confidence interval (CI) 1.11 to 1.37) as well as significantly higher odds of a mental health-related hospitalization (OR 1.29, 95% CI 1.16 to 1.45). In contrast, patients who reached an MPR threshold of 0.75 had significantly lower odds of hospitalization for any cause (OR 0.85, 95% CI 0.75 to 0.91), and those who reached an MPR threshold of at least 0.80 demonstrated a significant reduction in the odds of a mental health-related hospitalization (OR 0.82, 95% CI 0.70 to 0.95).
Thus, as patients achieved a higher MPR threshold, the risk of hospitalization declined (Figures 1 and 2). Patients who achieved an MPR threshold of at least 0.75 had an approximate 15% reduction in the odds of being hospitalized (p < 0.05), while those who achieved an MPR threshold of 0.90 or 0.95 had a 36% (p < 0.05) or 46% (p < 0.05) reduction in the odds of hospitalization, respectively.
Adherence (medication possession ratio) and risk of emergency room visits
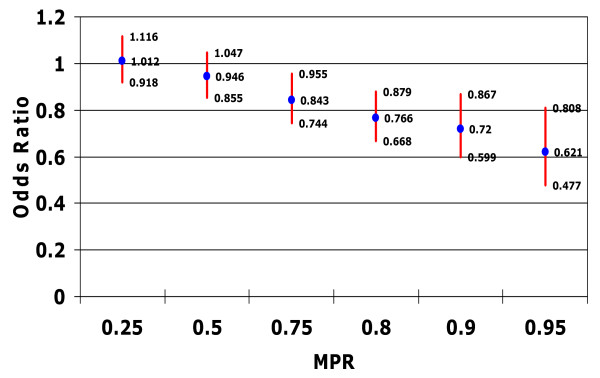
Figure 3 illustrates the association between patient adherence and the odds of an ER visit for any cause. At MPR thresholds of 0.25 or 0.50, the relationship between patient medication adherence and lower odds of ER visits for any cause did not reach significance. However, an MPR threshold of at least 0.75 was associated with significant reductions in the odds of an ER visit for any cause (OR 0.84, 95% CI 0.74 to 0.96). Thus, higher adherence thresholds (MPR > 0.75) resulted in a reduction in the risk of an ER visit for any cause, with an MPR of at least 0.75 associated with a 16% lower risk of visiting the ER (p < 0.05) (Figure 3). Moreover, patients with an MPR of at least 0.95 had 38% lower odds of visiting the ER (p < 0.05).
Figure 3.
Relationship between medication possession ratio and risk of emergency room visit for any cause. Controlling for confounding factors such as patient demographic characteristics; type of bipolar disorder; patient general health status (including Charlson Comorbidity Index score, total number of diagnoses, and total number of outpatient prescription medications received in the postindex period) psychiatric prescriptions; and specific comorbidities diagnosed in the preindex period.
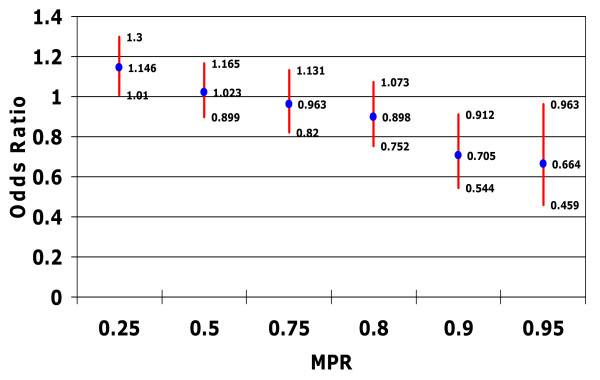
Evaluation of the association between medication adherence and ER visits with an accompanying mental health-related diagnosis revealed that, as MPR thresholds increase, the odds of a mental health-related ER visit reduced (Figure 4). Contrary to the results for ER visits for any cause, a significant reduction in the odds of an ER visit for mental health reasons was not observed until patients reached a threshold of at least 0.90 (OR 0.71, 95% CI 0.54 to 0.91).
Figure 4.
Relationship between medication possession ratio and risk of emergency room visit with mental health diagnosis. Controlling for confounding factors such as patient demographic characteristics; type of bipolar disorder; patient general health status (including Charlson Comorbidity Index score, total number of diagnoses, and total number of outpatient prescription medications received in the postindex period) psychiatric prescriptions; and specific comorbidities diagnosed in the preindex period.
As a test of the robustness of the results reported here, the relationship between medication adherence, and the risk of hospitalization or an ER visit with an accompanying diagnosis of bipolar disorder was also examined. The observed results were generally consistent with the results from the analyses of the risk of mental health-related hospitalizations or ER visits (data not shown).
Discussion
In this retrospective claims-based study, more than half of the 7,769 patients with bipolar disorder took their antipsychotic medication less than half of the time (61.9% had an MPR of less than 0.50), with the vast majority (78.7%) taking their medication less than 75% of the time. These observations are consistent with previous research indicating low levels of adherence to antipsychotics [19] and mood stabilizers [25] among patients with bipolar disorder. Alongside these findings, higher levels of adherence to antipsychotic medication were found to be associated with better patient outcomes, both in terms of hospitalizations and visits to the ER.
An examination of hospitalization outcomes revealed that, as patients achieved a higher MPR threshold, the odds of hospitalization for any cause as well as mental health-related hospitalizations, decreased. For instance, patients who achieved an MPR threshold of at least 0.75 had an approximate 15% reduction in the odds of being hospitalized for any cause (p < 0.05), while those who achieved an MPR threshold of 0.90 or 0.95 had a 36% or 46% (both p < 0.05) reduction in the odds of hospitalization, respectively.
While no previous study of individuals with bipolar disorder has reported on the relationship between adherence to antipsychotic medication and patient outcomes, previous research among patients with schizophrenia has shown partial or non-adherence to antipsychotic medication to be associated with higher rates of hospitalization [26]. In addition, several studies among patients with bipolar disorder have found a link between non-adherence to prescribed medication and hospitalization. An analysis of factors leading to hospitalization among elderly patients with bipolar mania found lack of adherence with prescribed psychiatric medication (for example, mood stabilizers) to be a major factor [14]. A study of adherence and outcomes among patients with bipolar disorder who were receiving antipsychotics, lithium, and antidepressants reported hospitalization rates of 73% for those classified as irregular medication users compared with 31% for regular users [15]. Similarly, an examination of adherence to mood stabilizers among individuals with mood disorders found hospital admission rates of non-adherent patients to be 81.2%, compared with a rate of only 9.7% among adherent individuals [16], while another study found non-adherence to mood-stabilizing medication to be a cause of relapse among patients with bipolar disorder [27]. Although these earlier studies did not primarily focus upon antipsychotic medications, the consistency of the findings indicates the importance of compliance to any treatment protocol.
Patients with an MPR of at least 0.75 had 16% lower odds of visiting the ER (p < 0.05), while those with an MPR of at least 95% had 38% lower odds of visiting the ER (p < 0.05). As observed with ER visits for any cause, an examination of the association between medication adherence and ER visits with an accompanying mental health-related diagnosis revealed that, as MPR thresholds increase, the odds of an ER visit decline. However, unlike the results for ER visits for any cause, a significant reduction in the odds of an ER visit for mental health reasons was not achieved until patients reached a threshold of at least 0.90 (OR 0.71, 95% CI 0.54 to 0.91). In comparison, an earlier study of the relationship between adherence to traditional mood-stabilizing therapy (lithium, valproate, carbamazepine, lamotrigine, oxcarbazepine) and health care utilization among patients with bipolar disorder, found adherence below 80% to be associated with a significantly greater risk of mental health-related ER visits (OR 1.98, 95% CI 1.38 to 2.84) [28]. This difference in results may indicate that the adherence threshold is higher for antipsychotic medications than for traditional mood-stabilizing therapy, although further research is needed before reaching a definitive conclusion.
One advantage of this study is that it allowed for an examination of effects on patient outcomes with various adherence thresholds. This study is in contrast to previous studies that defined adherence based upon a specific MPR threshold without necessarily explaining the choice of such a threshold [29-31]. Furthermore, it has been argued that 'the use of arbitrary categories of good and poor compliance (often set at 80%) usually was unsupported by research documenting the appropriateness of the cutoff for a specific medication class or disease' [32].
The findings presented here should be interpreted within the context of the limitations of the study design. This analysis was conducted using an administrative claims database, and included only patients with medical and outpatient prescription benefit coverage. The results, therefore, may not generalize well to other populations. Additionally, the use of diagnostic codes may be less rigorous than formal diagnostic assessments for identifying patients. Although analyses were adjusted for differences in bipolar disorder type, general health, and comorbidities, it was not possible to control for disease severity. The utilization of medical claims data precluded the inclusion of patient assessments and thus outcome measures related to quality of life, caregiver burden, or any of the other indirect costs associated with bipolar disorder were not included in this study. This investigation examined adherence to antipsychotic medications alone and did not account for prescribed changes in treatment protocol. Therefore, patients switched by their physicians from an antipsychotic to a different type of drug during the study period would have been viewed as non-adherent, even if they were fully compliant with their prescribed therapy. Finally, this study focused on both atypical and conventional antipsychotics, without controlling for class or exact type of medication. However, the results were largely driven by atypical antipsychotic medications, as demonstrated by 95% of the patient population receiving this class of therapy.
Conclusion
In summary, the results of this analysis indicate that, among patients with bipolar disorder, greater levels of adherence to therapy with antipsychotic medications are associated with better patient outcomes. Specifically, higher adherence thresholds were associated with lower chances of hospitalization and ER events. In view of the current evidence of poor adherence to long-term medication therapy [33-36], the findings of this study are encouraging as they show that the efforts to improve adherence, even in smaller increments, may improve patient outcomes.
Competing interests
MH is employed by AstraZeneca and ML received financial compensation from AstraZeneca for this project.
Authors' contributions
MH made substantial contributions to the conception and design of the study, acquisition of the data, interpretation of the data, and drafting of the manuscript. MJL made substantial contributions to the analysis of the data, interpretation of the data and drafting of the manuscript.
Acknowledgments
Acknowledgements
The authors would like to acknowledge the editorial assistance of Eleanor Bull (PAREXEL MMS). Financial support for this assistance was provided by AstraZeneca Pharmaceuticals LP.
Contributor Information
Maureen J Lage, Email: lagemj@hlthmetrics.com.
Mariam K Hassan, Email: mariam.hassan@astrazeneca.com.
References
- Murray CJ, Lopez AD, eds . The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020 (Global Burden of disease and Injury Series, Vol 1) Cambridge, MA, USA: Harvard University Press; 1996. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blader JC, Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996–2004. Biol Psychiatry. 2007;62:107–114. doi: 10.1016/j.biopsych.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt RJ, Henter I. An economic evaluation of manic depressive illness – 1991. Soc Psychiatry Psychiatr Epidemiol. 1995;30:213–219. doi: 10.1007/BF00789056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begley CE, Annegers JF, Swann AC, Lewis C, Coan S, Schnapp WB, Bryant-Comstock L. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics. 2001;19:483–495. doi: 10.2165/00019053-200119050-00004. [DOI] [PubMed] [Google Scholar]
- Peele PB, Xu Y, Kupfer DJ. Insurance expenditures on bipolar disorder: clinical and parity implications. Am J Psychiatry. 2003;160:1286–1290. doi: 10.1176/appi.ajp.160.7.1286. [DOI] [PubMed] [Google Scholar]
- Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the "top 10" physical and mental health conditions affecting six large US employers in 1999. Occup Environ Med. 2003;45:5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Stensland MD, Jacobson JG, Nyhuis A. Service utilization and associated direct costs for bipolar disorder in 2004: an analysis in managed care. J Affect Disord. 2007;101:187–193. doi: 10.1016/j.jad.2006.11.019. [DOI] [PubMed] [Google Scholar]
- Wyatt RJ, Henter I, Leary MC, Taylor E. An economic evaluation of schizophrenia, 1991. Soc Psychiatry Psychiatr Epidemiol. 1995;30:196–205. doi: 10.1007/BF00789054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs GS, Printz DJ, Kahn DA, Carpenter D, Docherty JP. The expert consensus guideline series: medication treatment of bipolar disorder 2000. Postgrad Med. 2000:1–104. [PubMed] [Google Scholar]
- Sachs GS, Thase ME. Bipolar disorder therapeutics: maintenance treatment. Biol Psychiatry. 2000;48:573–81. doi: 10.1016/S0006-3223(00)00991-4. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Martínez-Arán A, Reinares M, Benabarre A, Gastó C. Clinical factors associated with treatment noncompliance in euthymic bipolar patients. J Clin Psychiatry. 2000;61:549–555. doi: 10.4088/jcp.v61n0802. [DOI] [PubMed] [Google Scholar]
- Lehmann SW, Rabins PV. Factors related to hospitalization in elderly manic patients with early and late-onset bipolar disorder. Int J Geriatr Psychiatry. 2006;21:1060–1064. doi: 10.1002/gps.1607. [DOI] [PubMed] [Google Scholar]
- Svarstad BL, Shireman TI, Sweeney JK. Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv. 2001;52:805–811. doi: 10.1176/appi.ps.52.6.805. [DOI] [PubMed] [Google Scholar]
- Scott J, Pope M. Self-reported adherence to treatment with mood stabilizers, plasma levels, and psychiatric hospitalization. Am J Psychiatry. 2002;159:1927–1929. doi: 10.1176/appi.ajp.159.11.1927. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, McElroy SL, Strakowski SM, Stanton SP, Kizer DL, Balistreri TM, Bennett JA, Tugrul KC, West SA. Factors associated with pharmacologic noncompliance in patients with mania. J Clin Psychiatry. 1996;57:292–297. [PubMed] [Google Scholar]
- Jamison KR, Gerner RH, Goodwin FK. Patient and physician attitudes toward lithium: relationship to compliance. Arch Gen Psychiatry. 1979;36:866–869. doi: 10.1001/archpsyc.1979.01780080040011. [DOI] [PubMed] [Google Scholar]
- Sajatovic M, Valenstein M, Blow FC, Ganoczy D, Ignacio RV. Treatment adherence with antipsychotic medications in bipolar disorder. Bipolar Disord. 2006;8:232–241. doi: 10.1111/j.1399-5618.2006.00314.x. [DOI] [PubMed] [Google Scholar]
- International Society for Pharmacoeconomics and Outcomes Research ISPOR Medication Compliance and Persistence Special Interest Group (MCP): Standardizing Definition of Terms http://www.ispor.org/sigs/MCP_accomplishments.asp#definition
- Cantrell CR, Eaddy MT, Shah MB, Regan TS, Sokol MC. Methods for evaluating patient adherence to antidepressant therapy: a real-world comparison of adherence and economic outcomes. Med Care. 2006;44:300–303. doi: 10.1097/01.mlr.0000204287.82701.9b. [DOI] [PubMed] [Google Scholar]
- Mattke S, Jain AK, Sloss EM, Hirscher R, Bergamo G, O'Leary JF. Effect of disease management on prescription drug treatment: what is the right quality measure? Dis Manag. 2007;10:91–100. doi: 10.1089/dis.2006.635. [DOI] [PubMed] [Google Scholar]
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, McElroy SL, Strakowski SM, Bourne ML, West SA. Compliance with maintenance treatment in bipolar disorder. Psychopharmacol Bull. 1997;33:87–91. [PubMed] [Google Scholar]
- Olfson M, Marcus SC, Wilk J, West JC. Awareness of illness and nonadherence to antipsychotic medications among persons with schizophrenia. Psychiatr Serv. 2006;57:205–211. doi: 10.1176/appi.ps.57.2.205. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E. Treatment adherence in bipolar patients. Clin Appr Bipolar Dis. 2002;1:49–56. [Google Scholar]
- Lew KH, Chang EY, Rajagopalan K, Knoth RL. The effect of medication adherence on health care utilization in bipolar disorder. Manag Care Interface. 2006;19:41–46. [PubMed] [Google Scholar]
- Scranton RE, Lawler E, Botteman M, Chittamooru S, Gagnon D, Lew R, Harnett J, Gaziano JM. Effect of treating erectile dysfunction on management of systolic hypertension. Am J Cardiol. 2007;100:459–463. doi: 10.1016/j.amjcard.2007.03.045. [DOI] [PubMed] [Google Scholar]
- Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med. 2007;120:26–32. doi: 10.1016/j.amjmed.2006.06.028. [DOI] [PubMed] [Google Scholar]
- Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27:2149–2153. doi: 10.2337/diacare.27.9.2149. [DOI] [PubMed] [Google Scholar]
- Cramer J, Rosenheck R, Kirk G, Krol W, Krystal J, VA Naltrexone Study Group 425 Medication compliance feedback and monitoring in a clinical trial: predictors and outcomes. Value Health. 2003;6:566–573. doi: 10.1046/j.1524-4733.2003.65269.x. [DOI] [PubMed] [Google Scholar]
- Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- Waeber B, Leonetti G, Kolloch R, McInnes GT. Compliance with aspirin or placebo in the Hypertension Optimal Treatment (HOT) study. J Hypertens. 1999;17:1041–1045. doi: 10.1097/00004872-199917070-00022. [DOI] [PubMed] [Google Scholar]
- Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–1310. doi: 10.1016/S0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- World Health Organization Adherence to long-term therapies: evidence for action http://www.who.int/chp/knowledge/publications/adherence_report/en/index.html