Abstract
The purpose of this study was to explore the biopsychosocial consequences of spasmodic dysphonia (SD) as experienced by people with SD. Qualitative research methods were used to investigate the insider's perspective of living with SD. Six adults with SD participated in face-to-face phenomenological interviews. The results are summarized in a model of personal experiences of SD which shows that communication-related quality of life (QOL) is shaped by experiences with multiple physiologic (voice quality, effort, voice dependability); personal (affective responses, changes in self-view, coping strategies) and social (physical environment, other people, participation in social roles) factors. Communication-related QOL is a complex and individualized construct with multidimensional contributors. This study suggests that understanding the nature of communication-related QOL for each individual requires exploration of each component of the model, exploration of the unique relationships among components for each person, and recognition of the multidimensional factors that shape the experience of SD.
Learning outcomes
As a result of this activity the reader will be able to (1) identify general features of the phenomenological research method; (2) identify the three general categories of psychosocial consequences of SD; (3) identify those psychosocial consequences of SD that are under-represented in the literature; and (4) identify key conclusions of the communication-related quality of life model.
Spasmodic dysphonia (SD) is a type of focal dystonia characterized by involuntary spasms of the laryngeal muscles. It is an adult-onset disorder of unknown etiology that is more prevalent in women than in men. The National Spasmodic Dysphonia Association estimates that 50,000 people in North America are affected by SD (National Spasmodic Dysphonia Association). SD can present in a variety of forms, each with somewhat different vocal symptoms. Adductor SD (ADSD) is the most common form of SD and is characterized by irregular tight or strained voice stoppages which are caused by the intermittent hyperadduction of the vocal folds during phonation. Abductor SD (ABSD) is much less common and takes the form of irregular breathy voice breaks that occur when the vocal folds abnormally spasm to an abducted position during speech. Some people with SD exhibit a component of vocal tremor. Speakers with mixed SD might present with any combination of the above forms. Some studies based on laryngeal electromyography (EMG) have suggested that all forms of SD are mixed to some degree with each presentation showing a greater preponderance of one type of symptom or another (Hillel, 2001). Other symptoms of SD include hoarseness, roughness, strain or other forms of dysphonia as well as considerable effort to talk. Since the mid-1980s, localized injection of botulinum toxin (botox) has been the most commonly used treatment for effective, albeit temporary relief of SD symptoms (Duffy & Yorkston, 2003).
Information about the characteristics of SD can be organized according to the World Health Organization's International Classification of Functioning, Disability and Health (ICF) (WHO, 2001). The ICF provides a model of disablement as a means of describing the biological and psychosocial consequences of health conditions. Using the ICF terminology, impairment is defined as a problem in body function or structure. The impairment aspects of SD have been well described using videostroboscopy, acoustic analysis and aerodynamic events as some examples of impairment-related measures (Adams, Hunt, Charles, & Lang, 1993; Edgar, Sapienza, Bidus, & Ludlow, 2001; Langeveld, van Rossum et al., 2001; Ludlow, 1990; Ludlow, Naunton, Sedory, Schulz, & Hallett, 1988; Rhew, Fiedler, & Ludlow, 1994; Zwirner, Murry, Swenson, & Woodson, 1991, 1992; Zwirner, Murry, & Woodson, 1993, 1997). Activity is defined in the ICF as the execution of a task or action by an individual. Speaking can be viewed as an activity. Traditionally, perceptual measures of voice quality have been reported as a measure of speech activity in SD (Adams et al., 1993; Aronson, McCaffrey, Litchy, & Lipton, 1993; Blitzer, Brin, & Stewart, 1998; Brin, Blitzer, Fahn, Gould, & Lovelace, 1989; Langeveld, van Rossum et al., 2001; Zwirner et al., 1993). The ICF defines participation as involvement in life situations. Restrictions in participation, particularly in occupational and social domains have been documented as a consequence of SD (Langeveld, van Rossum et al., 2001; Smith et al., 1993, 1998; Zwirner et al., 1992, 1997). The ICF model also recognizes contextual factors including environmental (external) and personal (internal) factors that help shape the consequences of a health condition. Historically, psychosocial implications that include these contextual factors have received relatively little attention in research literature compared to the focus on impairment and activity factors. However, more recent investigations that explore the psychosocial impact of SD have been conducted using scales designed specifically for voice disorders including the Voice Handicap Index (VHI) (Benninger, Gardner, & Grywalski, 2001; Courey et al., 2000; Jacobson et al., 1997) and the Voice-Related Quality of Life (V-RQOL) (Hogikyan & Sethuraman, 1999; Hogikyan, Wodchis, Spak, & Kileny, 2001; Rubin, Wodchis, Spak, Kileny, & Hogikyan, 2004). Studies have also explored the psychosocial impact of SD using more general health-related questionnaires that do not focus specifically on communication disorders (Cannito, 1991; Cannito, Murry, & Woodson, 1994; Courey et al., 2000; Langeveld, Luteijn, van Rossum, Drost, & Baatenburg de Jong, 2001; Murry, Cannito, & Woodson, 1994).
The increased attention on the psychosocial impact of SD is part of the recognition across the field of healthcare in general (Dijkers, Whiteneck, & El-Jaroudi, 2000; Law, 2002; Whiteneck, 1994) and the field of communication disorders specifically (Benninger, Ahuja, Gardner, & Grywalski, 1998; Cruice, Worrall, & Hickson, 2000; Deary, Wilson, Carding, & MacKenzie, 2003; Ma & Yiu, 2001; Murry & Rosen, 2000; Worrall, McCooey, Davidson, Larkins, & Hickson, 2002) that it is essential to understand the meaning of a disability from the perspective of the individual living with that disability. The insider's perspective is needed in order to plan, implement and evaluate interventions that will produce the greatest benefit for each person. Hayes (1998) argues that the pursuit of evidence-based practice is not complete unless that evidence includes outcome measures based on the patient's perspectives.
Although the research cited above has advanced our understanding of the psychosocial consequences of SD, gaining an authentic view into the insider's perspective of SD continues to be very difficult because of the unique and intricate manner in which the voice disorder interacts with many personal and environmental variables to shape each person's experience. One approach for exploring the insider's perspective that differs from approaches used in prior research is through the use of qualitative research methods. Qualitative methods are well-suited to investigating the consequences of communication disorders because communication is a highly complex, individualized and contextual phenomenon. Through qualitative interviews or other naturalistic observational techniques, participants are able to share with the researchers the information they feel is most relevant to their particular situations. This directs the researchers’ attention to the issues that are of greatest importance for the participants. Qualitative research techniques enable participants to provide insight into the complex interactions among issues that contribute to their experiences. Furthermore, participants can provide insight into reasons for variability in their experiences from one person to the next. This information is not always accessible to researchers when participants are constrained by strict questionnaire forms or structured rating scales. An overview of qualitative research in the field of speech–language pathology is provided by Damico and Simmons-Mackie (2003).
The purpose of this study is to examine the lived experiences of speakers with SD using a qualitative phenomenological inquiry. “Lived experiences,” a common term in phenomenology, refers to the experiences that participants have in the natural contexts of their daily lives. This study focuses on the consequences of SD that participants experience in the context of their daily lives. Better understanding of the consequences of SD from the perspective of the insiders should help guide both clinical and research efforts directed at improving assessment, intervention and overall quality of life (QOL) for people with SD. Applications of this research may follow the example of other qualitative research to ensure that assessment, intervention and outcomes measurement practices are representative of and relevant to the client groups with whom they are used (Dijkers, 2003; Johnston & Miklos, 2002; Simmons-Mackie & Damico, 2001).
1. Methods
1.1. Research approach
This study was conducted following the phenomenological tradition of qualitative inquiry. In a phenomenological study, researchers explore the meaning of the lived experiences of a group of people who share a common phenomenon such as living with SD (Benner, 1994; Creswell, 1998). Through analysis of guided interviews, researchers seek to describe the common experiences as well as the range of different experiences within the group. It is understood that people will have multiple perspectives on these experiences, and that each individual is the expert in how he or she interprets the meaning of the experience for himself or herself. The product of a phenomenological study is a detailed account that provides the reader with an authentic understanding of the meaning of that experience in the words of the persons who have lived that experience. All methods were approved by the institutional review board at the University of Washington.
1.2. Participants
Six participants, five women and one man, volunteered to take part in this study (see Table 1). They were recruited from the clients receiving care for SD at the University of Washington Medical Center. All participants were receiving care from one otolaryngologist/speech–language pathologist team. Inclusion criteria included age of 18 years or older, diagnosis of any form of SD as confirmed by the otolaryngologist and speech pathologist, and completion of a minimum of five botox injections. Participants with any form of SD were included to achieve the objective in this initial exploratory study of identifying a broad range of psychosocial consequences faced by the general population of people with SD. The criterion of a minimum of five injections was chosen so that participants would have had a relatively long-term background of experience with issues related to SD from which to give their overall perspectives. Although the inclusion criterion was a minimum of five injections, all of the participants who were enrolled in the study had had 12 or more injections.
Table 1.
Participant demographic information
| Case | Age | Sex | Occupation | Primary voice demands | Type of SDa | Number of years post first inj.b | Number of inj.c | Voice at interviewd |
|---|---|---|---|---|---|---|---|---|
| I.P. | 49 | F | Not working (unrelated to voice) | Social/volunteer work | ADSD | 8 | 19 | 7−8 |
| B.W. | 53 | F | Technical writer | Work | ADSD | 7 | 22 | 8 |
| A.T. | 59 | F | Substitute elementary teacher | Work/community groups | ABSD | 6 | 12 | 8 |
| M.A. | 57 | M | Small business owner/professional | Work/Social | ADSD | 7 | 19 | 6−7 |
| H.T. | 80 | F | Retired | Social/volunteer work | ADSD and tremore | 6 | 31 | 5 |
| R.N. | 52 | F | Nurse | Work/social | ADSD and tremor | 6 | 23 | 7−8 |
ADSD, adductor SD; ABSD, abductor SD.
Number of years that each participant has been receiving botox injections; inj, injection.
Total number of botox injections that each participant has received.
Participants were asked to rate their voices on the day of interview on a scale with 1, the worst the voice has been and 10 being the best the voice has been since onset of SD.
Participant had familial head tremor in addition to voice tremor.
The final inclusion criterion was the absence of any other significant physical or cognitive impairment that might exert a notable influence on life participation. Examples of other physical or cognitive impairments that would exclude participants were non-ambulatory status, blindness, severe uncorrected hearing impairment or evident signs of dementia. Potential participants were screened for these conditions by the voice clinic team members who referred potential participants for this study. The clinicians screened for this criterion based on review of medical histories of the participants and the clinicians’ experience interacting with these participants through their clinical practice. While it is recognized that other aspects of participants’ medical or psychological histories might interact with the SD to affect their lived experiences, these natural and complex relationships among such variables are accommodated by phenomenological methodology. The purpose of the informal screening was to rule out severe conditions that clearly prevented a person from interacting with their environment as a typical person would. The referring clinicians were not otherwise involved in this study.
1.3. Data collection
1.3.1. Interviews
Each participant attended one face-to-face interview, with follow-up for four of the six participants who were available for additional interviews. Interviews were held in private rooms at either the University of Washington Speech and Hearing Clinic or the University of Washington Medical Center. Participants were encouraged to schedule their primary interviews at a time in their botox treatment cycles that would be most comfortable for them to talk in order to avoid any unnecessary strain or fatigue. The duration of the interviews was typically between 1 and 2 h and participants were offered breaks as they wished. The sessions were audio recorded for later transcription. Two investigators (C.B. and K.Y.) conducted all the interviews jointly. Neither interviewer was involved in the clinical care of the participants.
The interviews were guided in that participants were asked two general questions about how SD had affected them: (a) Tell us about your history with SD, for example when and how did your symptoms start and how did that affect you? and (b) What impact has SD had on your life? Participants were encouraged to talk about their experiences, feelings, and thoughts about these questions or about any other topic related to SD. Within the context of the general questions listed above, the content and direction of the interviews were determined largely by the participants who shared experiences that were most relevant to them. The researchers asked additional questions as needed to clarify points or to seek additional information.
1.3.2. Participants’ self-rated voice quality
Participants were asked to rate their voices on the day of their primary interviews. The purpose of this rating was to provide a general indication of how well their voices were functioning during the interview out of concern for the question that the extent or nature of their participation in the interviews might be affected if they were struggling with SD symptoms of any notable severity. Participants rated their voices on a scale of 1−10 with the anchor points being 1, the worst your voice has been since getting SD; and 10, the best your voice has been since getting SD (including the effects of botox). These data are available in Table 1 and demonstrate that most participants felt their voices were quite good on the day of the interview.
1.4. Analysis
1.4.1. Interview analysis
The interviews were transcribed verbatim from the audio recordings by the primary investigator. Interview analysis followed qualitative guidelines including the steps of coding and summarizing the interviews, interpreting themes, and identifying exemplar cases for illustration (Benner, 1994; Creswell, 1998). In brief, this analysis process started with multiple readings of the interviews to gain in-depth familiarity with the content. Organization of the interview content began by coding the utterances in the transcripts according to their topics. The codes and their definitions were not established a priori but instead were generated from the content of the interviews. For example, a very common topic of discussion was how other people in the participants’ environments react to the participants’ voices through either comments or actions. Any utterances on this topic that arose in the interview texts were coded as, “reactions of others.” The codes were then grouped together according to common issues they addressed. After identifying these main thematic groups, the primary investigator wrote a detailed summary of each interview highlighting the salient comments and quotes from each participant that fell under each thematic category. These summaries were then combined across participants so that the participant experiences within each thematic category could be compared. The development of themes was an iterative process involving the exploration of various alternative interpretations, incorporation of new information gleaned in each interview and modification of themes as needed to ensure that the final themes reflected all interviews commensurately. The interviews and subsequent analyses were conducted by the team of authors which included researchers who have had doctoral training in qualitative methods and have had several years of experience conducting research using the phenomenological approach. This team approach to analysis provided a mechanism for developing and challenging emerging themes to ensure that the final themes represented the most plausible summaries of the interview data from the perspectives of multiple researchers. The goals for the final qualitative analysis were to: (a) identify commonalities and differences among participants’ experiences; (b) reflect the complexities and multiple realities among participants through descriptive accounts; and (c) illustrate the themes through the language of the participants (Benner, 1994).
1.4.2. Credibility
After the primary investigator transcribed the audio recordings of the interviews, a research assistant who was otherwise uninvolved in data collection and analysis listened to each interview in its entirety while reading the full transcript for each interview. This second transcriber made any notations where there were potential discrepancies between what she heard on the recording and what the transcript contained. The two listeners then examined any instance of potential discrepancy to determine if it was minor in that it did not change the meaning of the utterance (i.e. disagreement over whether someone said ‘that's’ or ‘that is’); or whether there was any chance that a discrepancy would change the intended meaning of any utterance. No discrepancies that affected content of utterances were identified.
Additional methods to establish credibility focused on involving multiple professionals familiar with qualitative research and/or SD on the research team to review and challenge the emerging interpretations of data. Two researchers attended all interviews and participated in all stages of analysis to allow discussion and comparison of results and interpretations. Throughout the analysis process, data and emerging interpretations were also evaluated by a qualitative research team as well as by experts in voice disorders.
1.4.3. Verifiability
In qualitative research, the primary method for verifiability is to return the data and emerging analysis to the participants, and to invite them to comment on the degree to which the analysis reflects their own interpretations of their experiences. This provides an opportunity for clarification of any points of potential misinterpretation as well as for confirmation of agreement between the participants’ viewpoints and the researchers’ summaries. Four of the six participants have participated in brief follow-up visits for verification purposes at their routinely scheduled botox injection appointments in the voice clinic.
2. Results
Three major themes and nine sub-themes emerged from the analysis of interview data (Table 2). The first theme, my voice does not work, contained information about how participants experienced changes in voice production. The three sub-themes under this category included my voice sounds different, talking requires physical effort, and my voice is undependable. The second major theme was my personal experience of SD. This theme focused on participants’ views of themselves as a consequence of SD and incorporated three sub-themes: SD changes how I feel about myself, my voice does not represent me, and I just deal with it. The third major theme was communicating in the world around me. This theme addressed the external environmental issues that contributed to the consequences of SD. The sub-themes that highlighted these external environmental influences were some places are hard, people make a difference, and SD has deprived me of certain roles. Each of these themes and sub-themes will be described in greater detail below with quotes from participants to demonstrate how these themes were derived from the interviews to summarize the consequences of SD.
Table 2.
Themes and sub-themes describing the consequences of living with SD
| Themes | Sub-themes | Definitions |
|---|---|---|
| My voice does not work | My voice sounds different | Changes in voice quality (raspy, shaky) |
| Talking requires physical effort | Physical symptoms (effort, fatigue) | |
| My voice is undependable | Changes in speech function such as unpredictability of how voice will sound | |
| My personal experience of SD | SD changes how I feel about myself | Affective issues such as feeling embarrassed or self conscious |
| My voice does not represent me. | The voice “misrepresents” how I feel | |
| I just deal with it | Coping strategies of avoidance, vigilance, and attitude | |
| Communicating in the world around me | Some places are hard | Dealing with environmental issues, i.e. background noise |
| People make a difference | Characteristics and responses of other people influence involvement | |
| SD has deprived me of certain roles | Restrictions in the number/extent of social roles |
2.1. Theme 1: my voice does not work
Participants described changes in the basic function of the voice including altered sound of the voice, increased physical effort, and undependability of the voice. These changes in function created obstacles to communication.
2.1.1. My voice sounds different
The terms that participants used to describe the sounds of their voices were generally unpleasant: raspy, cracking, shaking, hoarse, having a tremor, quavering, screeching, lacking projection, and containing voice breaks, spasms or tension. M.A. (all initials are fictitious) described his voice as sounding, “like some kind of wild chicken screeching out words.” Other participants described a lack of loudness, for example, R.N. suggested that her voice lacked “a big range.” She commented, “I don’t know if I could ever project my voice to be heard in a large auditorium or public speaking.” Participants varied in terms of how well they felt they could describe their voices. Most felt that they were skilled at noticing subtle changes in their voices; however, two participants indicated that they were not good judges of their voices. B.W. stated, “I don’t think I hear it correctly.”
2.1.2. Talking requires physical effort
The most prominent physical symptom described by participants was the tremendous effort required to speak. M.A. described this physical work in the following way, “It just feels like you’re having to grab onto a word and push it out from your throat. The word is down there and you have to force it out.” For many, the physical effort was in response to the sensation of tightness, tension, and constriction. R.N. described the feeling like,
There's a rubber band around my neck. Someone was constricting it. I was trying harder and harder to overcome and produce a good quality voice. It was taking more and more effort. I was just kind of getting on a vicious cycle.
The physical effort required to talk had a cascading effect resulting in other physical symptoms. M.A. described a connection between effort, breathlessness, and fatigue when he said, “I run out of air when I talk—you just get breathless and tired.” Many participants reported becoming fatigued to the point of exhaustion, particularly if their jobs required prolonged periods of speaking. A.T., an elementary school teacher, said, “It's draining. I am really exhausted at the end of teaching ... even now when I go in a half day, I am happy to come home and not speak.” Reports of pain associated with speaking were mixed. Some participants reported experiencing definite pain. B.W. commented, “It feels like you have a sore throat all the time ... like a raw feeling in your throat.” Other participants denied feeling pain. For example, R.N. said, “It's not painful. It just takes energy.”
2.1.3. My voice is undependable
Unreliability of the voice was one of the most troubling consequences of SD for participants. They reported that fluctuating symptoms made it impossible to know how the voice would sound at any given time. I.P. commented, “Sometimes the voice gives out in the middle of speaking. That can kind of be embarrassing sometimes depending on the situation.” For B.W., the inconsistency of her voice caused her to avoid social situations. She reported, “I just get tired of guessing where my voice might be on that day that you schedule your social thing ... so I just don’t socialize.”
2.2. Theme 2: my personal experience of SD
The consequences of SD go beyond changes in voice function. Participants described their internal personal experiences as communicators with SD. These issues included SD changes how I feel about myself and my voice does not represent me. Because the participants felt that they were unable to change their voices, they developed strategies to just deal with it.
2.2.1. SD changes how I feel about myself
Participants reported a wide range of affective responses to SD. Some terms used by participants to describe these feelings included being self-conscious, embarrassed, frustrated, hopeless and disheartened as well as feeling grief over the loss of things that they were no longer able to do. Participants also reported feeling less intelligent, confident, or competent because of their voices. B.W. described her feelings in the following way, “You feel incompetent because you’re not allowed to do anything because your voice won’t work for that situation. So you’re forced into incompetence.”
For some participants, the impact of SD on affective feelings was large. One participant reported a history of depression associated with SD that had required counseling intervention. R.N. stated, “I really got myself in a big, emotional hole.” In contrast, other participants, such as M.A. expressed only mild frustration with the “technical” aspects of SD such as problems speaking over background noise or running out of air when talking.
2.2.2. My voice does not represent me
Most participants described the feeling that their voices were a “façade” (H.T.) that obscured who they really were. There was a mismatch between how they saw themselves and how their voices represented them. Some participants felt that they were essentially the same person they had always been on the inside but that they simply could not express that identity accurately because of their voices. B.W. expressed this as, “Every time you open your mouth you don’t sound like what's in your head.” Other participants felt that their actual identities had changed in response to SD. A.T. summed up this perspective when she said, “I think my personality changed drastically because I used to be very outgoing and now I find myself avoiding those situations. I’ll go sit in the background. It is just because I can’t speak.”
2.2.3. I just deal with it
The participants unanimously reported that there was nothing that they could do physically to control their voices. Instead, coping focused on strategies such as planning ahead, avoiding difficult situations, and maintaining a good attitude.
Speaking required vigilance and planning. R.N. commented, “It was always on my mind ... I thought about it constantly.” She also said, “Speech lost its spontaneity and I had to preplan what I was going to say.” This need for vigilance and planning in conversations reduced the quality of interactions that participants had with other people. R.N. summed up this idea as follows, “It took mental energy to talk. It was hard to just get my mind off my voice. I didn’t feel like I was present with people.” Vigilance was also required in other ways. For example, R.N. found that she had to strategize her daily schedule because of the toll that SD took on her physical as well as mental energy. She could not do all that she wanted to do and had to prioritize her activities, even those that might not require much talking.
Avoidance of talking was a common coping strategy that took several different forms. For example, H.T. stated, “Sometimes I feel I have something to say but I know my voice is bad and I just don’t say it.” Examples of avoidance could be seen in everyday activities such as making phone calls. R.N. stated, “You dread making phone calls. I’ll do one today. I’ll do the next one tomorrow. I’ll space them out.” Other examples related to work. A.T., an elementary teacher described the following situation,
I used to always read chapter books with my first graders and I virtually gave that up. And I just couldn’t believe that you’d give that up, changing your teaching to accommodate your speech. What are the kids losing from this?
Sometimes, avoidance affected potentially life-changing decisions such as pursuing new job opportunities. R.N. commented, “I actually avoided getting a new job for a long time because I just didn’t want to go through the interview.” Other times, avoidance was part of everyday conversations. For example, participants reported avoiding particular sounds or words in various communication situations. A.T. described this avoidance, “You kind of learn what your vocabulary's going to allow you to say which isn’t necessarily good because I think your vocabulary then is beginning to sound more like a first grader.”
Many participants reported that they deal with SD by adopting specific positive attitudes including stoicism, determination to persevere, or hope for a future cure. I.P. said, “I want to be positive. It's something you’ve got to live with so get the best treatment you can and roll with it instead of trying to hide it.” Keeping SD in perspective relative to other medical conditions also reflected a positive attitude. Participants often noted that SD, as bad as it was, was at least not life threatening or of any significant medical consequence. I.P. suggested, “There could be a lot of other things that are a lot worse to have in your life so I just try to have a positive attitude about it.”
2.3. Theme 3: communicating in the world around me
The third major theme reflected the external social consequences related to SD. Categories included the physical environment (some places are hard), characteristics and reactions of other people (people make a difference), and role restrictions (SD has deprived me of certain roles).
2.3.1. Some places are hard
Participants identified two primary features of the physical environment that made communication most difficult with SD. The first was the presence of background noise. Because the participants had no control over the loudness of their voices, they were unable to modify their speech to be heard in background noise. The list of difficult places included restaurants, cars, large social events, sporting events, noisy work environments, and outside environments such as walking down a busy street. The other common complaint about the physical environment was difficulty talking on the phone. Participants felt that they could not project their voices clearly enough to be heard over the phone. M.A. reported, “There's a tenseness on the phone when you have the spasmodic dysphonia that doesn’t seem to happen as much face to face. The phone seems to make me strain more.” He suggested that one of the worst situations was driving and talking on the telephone, a situation that combined both noise and telephone communication.
2.3.2. People make a difference
Reactions of others heavily influenced the experiences of the participants. All shared stories about comments they had received from other people that were unpleasant. The most universal and annoying question dealt with their general health. Participants grew weary of having to explain that they did not have colds or other contagious illnesses. M.A. said, “That's the one comment I get all the time is people say do you have a cold or what do you have? Is it catching?” Some comments showed that other people seemed to hold opinions about the participants’ abilities, attitudes or other qualities, based on the sound of the voice, that the participants felt were inaccurate. These included suggestions that the participants were untruthful or sneaky when they were actually quite honest people; that the participants were nervous and unconfident when they actually felt quite capable; and that they were not skilled or intelligent when they actually were fully qualified. People did not always talk to the participants as equals or colleagues but instead would be more prone to talk down to them. A.T. said, “People become condescending like you’re not capable anymore because you don’t speak well, and that one's really hard to accept.”
In general, the participants reported that communication was much easier with people familiar to them than with unfamiliar people. They suggested two reasons for this difference. First, it is possible to “educate” familiar people whereas telling people about SD was just not worth the trouble if the conversation partner was someone who would be seen only rarely or briefly. Second, familiar people were less likely to form opinions about the participants based on their voices because these people knew so many more things about the participants. As I.P. said about her close friends, “They like me for me.”
Unfortunately, familiarity and knowledge about SD did not always ensure that people well-known to the participants would always be supportive and tolerant. Some participants described situations where people who had known about the SD for a long time seemed to forget or fail to appreciate the struggles the participants had to communicate. A.T. reported a situation where she was asked to speak publicly where she did not feel comfortable,
Yesterday I had to read a letter in a group I belong to and when people hand me those things I actually cringe because I know I’m not going to get through it. And the group knows that I have a speech problem but I don’t think people understand it.
Participants found that unfamiliar people were generally less tolerant of their speaking difficulties, but participants reasoned that this was logical because unfamiliar people did not know about the SD. Participants felt that in most situations, uncomfortable responses from other people were caused by others not knowing what to say or do, or by other people trying to be nice but simply misjudging how to respond. One salient issue was that unfamiliar people often did not seem to have the patience to communicate with the participants when they were difficult to understand. H.T. stated:
I can’t explain it but it's expression or they change the subject or they go to something else. They just don’t want to take the time to worry about it. I’m not talking about good friends. I’m talking about acquaintances.
Familiarity was not the only characteristic of other people that influenced communication. Other challenging communication partners included individuals with poor hearing and young children who were not familiar with the participants’ voices.
2.3.3. SD has deprived me of certain roles
The third sub-theme involved social role restrictions. Most people have multiple roles including professional or occupational roles, their community involvement or leisure roles and their interpersonal relationship roles. Most participants suggested that the number of roles they played decreased, and that participation was restricted in some of the roles they continued to play. The loss of roles came in the form of quitting jobs that they otherwise would have continued, avoiding pursuing new career paths that interested them, giving up community leadership activities that they enjoyed, and not attending social activities. Participants who continued to attend events such as their book club meetings, social gatherings or other activities found that they were not as involved in these situations as they would have liked. They did not talk as much, they were not as active in leading activities or discussions, or they did not take on other responsibilities within the group. When describing taking part in her book club, H.T. said, “My participation is not what I would like.... I go but I don’t participate.” Through these comments, the participants made it clear that really participating in a role meant much more than simply attending the activity. Truly participating meant achieving some level of involvement or interaction with others above and beyond merely being present at an event.
Participants felt that roles were restricted for many reasons. B.W. described how her voice had limited her from pursuing desired professional roles due to a combination of factors that included the unreliability of her voice from day to day, the overall sound of her voice, and misjudgments that other people made about her based on her voice.
There are still some things that I cannot do that I would do if it were an ideal situation; for instance be a lawyer where your tone of voice is very important and you have to be able to rely on that. You can’t sound like you’re lying on certain days.
To summarize the results of this study, participants reported that their voices sounded different, required much effort and were unreliable. In addition, participants felt that their voices did not represent who they were. Successful communication depended on many factors including a participant's ability to cope and use strategies in a variety of environments with different communication partners.
3. Discussion
The purpose of this study was to investigate the consequences of SD from the perspective of the insider using qualitative methods, which provide data about highly individualized, complex and contextualized phenomena from the authentic perspective of the participants as the experts. In this discussion, the results from this study are compared to findings from prior research. Because of the emphasis on the participant perspective, the body of prior research used for comparison consists primarily of studies that document patient self-report of symptoms and experiences associated with SD. The results are then organized into a model that summarizes the consequences of SD as described by participants in this study. Finally, clinical implications and plans for future research are presented.
3.1. The insider's perspective
3.1.1. My voice does not work
The first theme of my voice does not work reflects experiences associated directly with the physical function of the voice. The first sub-theme, my voice sounds different, contains participants’ descriptions of their voices such as cracking, shaking and having voice breaks. These descriptions are consistent with prior literature containing participant self-reports of voice dysfunction. Smith et al. (1998) reported that weak and hoarse voice qualities were the second and third most common symptoms of SD respectively. Several studies have demonstrated that participants generally rate their voices as moderately to severely affected by SD (Aronson et al., 1993; Benninger et al., 2001; Blitzer et al., 1998; Hogikyan et al., 2001; Langeveld, Luteijn et al., 2001; Langeveld, van Rossum et al., 2001; Rubin et al., 2004; Schonweiler, Wohlfarth, Dengler, & Ptok, 1998).
Although participants in the present study briefly described their voice qualities, they did not focus much attention on how their voices sounded from their own perspectives. The sound of the voice in isolation did not appear to be as critical of an issue as what the voice changes meant in their daily lives in terms of being able to fulfill job responsibilities, participate in social activities or meet other desired goals. These findings are similar to those of Yorkston, Klasner and Swanson (2001) in which participants with multiple sclerosis focused less on their discrete physical impairments and more on the functional implications of those impairments in the context of social activities.
Talking requires physical effort is the second sub-theme under the category of my voice does not work. Physical strain to talk and associated symptoms such as fatigue, running out of breath and physical tension were highly pervasive across all participants. The dominance of effort as a symptom of SD is consistent with reports in the literature. For example, Smith et al. (1998) found that effortful speech was the most commonly reported symptom. Other studies have documented the considerable role of effort and fatigue in SD using a variety of patient self-report scales (Aronson et al., 1993; Langeveld, Luteijn et al., 2001; Langeveld, van Rossum et al., 2001; Murry et al., 1994). Both the current study and previous literature suggest the importance of effort and fatigue as consequences of SD. The contribution of effort and fatigue to the psychosocial consequences of SD may be captured in the VHI (Benninger et al., 2001; Courey et al., 2000) and V-RQOL (Hogikyan et al., 2001; Rubin et al., 2004) because each scale contains questions addressing these symptoms. Otherwise, no widely accepted measures focusing specifically on this domain were found in the literature.
Under the theme of my voice does not work, the third sub-theme is my voice is undependable. Participants reported that their voices were inconsistent and unreliable. This was particularly troubling to participants because they could not depend on their voices to consistently sound good, especially in situations such as professional meetings or social interactions where they needed to portray a consistent and confident image. Although all of these participants had lived with SD for many years and were very experienced in dealing with the symptoms, the inconsistency of voice continued to frustrate them. The VHI (Jacobson et al., 1997) and V-RQOL (Hogikyan & Sethuraman, 1999) each include one question regarding predictability of voice. Otherwise, evidence was not found that undependability of voice and its functional manifestations have been investigated specifically as consequences of voice disorders such as SD, and this may be an area warranting further research.
3.1.2. My personal experience of SD
The second theme of my personal experience of SD contains information about the participants’ internal reactions to SD. This theme includes participants’ descriptions of changes they see in themselves because of SD, as well as resources they draw upon from within to cope with SD. This personal factor reflects that each person has his or her own capabilities, perspectives, and goals that he or she draws upon when dealing with a condition such as SD. The individual is not a passive subject upon which physical injuries and environmental conditions act. Instead, the individual is an active being who interprets what the experience will mean for him or herself.
The first sub-theme, SD changes how I feel about myself, summarizes participants’ affective responses to SD. Participants reported feeling frustrated, hopeless, embarrassed and self-conscious to name a few descriptors. There was a wide range of responses among participants in terms of how much SD had impacted their personal feelings. Elevated symptoms of anxiety, depression and other negative affective responses to SD have been documented in other studies using a variety of health-related instruments (Cannito, 1991; Cannito et al., 1994; Courey et al., 2000; Langeveld, Luteijn et al., 2001; Liu et al., 1998; Murry et al., 1994). SD participants also have demonstrated “excessively negative attitudes towards communication” when assessed using the Erickson Scale of Communication Attitudes (Cannito et al., 1994).
My voice does not represent me is the second sub-theme in this group. Participants felt that there was a mismatch between who they really were and what their voices portrayed about them. Some participants felt that their personalities had actually changed in response to SD while others felt that they were still the same person inside, but they could not portray that personality because of their voices. As with the affective responses, there was a wide range of experiences in this sub-theme. The issue of personality and SD has been a topic of discussion in the literature as reviewed by Roy and Bless (2000). Roy, Bless, and Heisey (2000) found that people with SD did not differ from people with other voice disorders or from medical control groups on a personality inventory measure. This and other prior research suggests that people with SD are not characterized by particular personality traits that are an inherent feature or causal factor of SD. The results of the current study are consistent with this suggestion of no particular personality profile associated with SD. Participants in this study represented a wide variety of experiences ranging from minimal to considerable self-perceived changes in personality as a consequence of SD. Caution may be warranted in attempting to further reconcile the findings of the current study with those of prior research using personality or psychological measures. When participants reported that they felt their “personalities” had changed, these experiences may not represent the same constructs that are tapped by the personality profiles used in prior research. The experience of not being able to “be myself’ should not be assumed to necessarily translate into the development of a particular psychological or personality trait as defined by the medical or psychological profiles. The importance of these issues to the participants in this study suggests that factors such as self-perceived personality changes should be the focus of future research.
The third sub-theme in this category is I just deal with it. This theme reflects participants’ discussions of coping strategies. Clearly one of the most common forms of coping with SD is to seek treatment, usually through the form of botox injections. It is beyond the scope of this article to provide a complete description of participants’ experiences with the medical management of SD using botox. This topic will be the focus of a future article. In this present article, other forms of coping with the psychosocial consequences of SD are explored. Despite the fact that all participants in the present study were receiving botox injections, it is notable that there continued to be a wide variety of individual experiences associated with coping with SD.
Participants described two main types of coping. The first was the behavioral strategies that people used, the most common of which was avoidance. Participants avoided noisy settings, certain forms of communication such as the telephone, particular vocabulary words and other situations that caused them difficulty. The second type of coping was attitudinal coping in that participants tried to keep a positive attitude, and they tried to keep SD in perspective compared to other medical conditions. Questions about avoidance of various situations are included in most of the commonly used or recently published voice questionnaires (Deary et al., 2003; Hogikyan & Sethuraman, 1999; Jacobson et al., 1997; Ma & Yiu, 2001) suggesting that this is one coping strategy that contributes to the psychosocial implications of voice disorders in general. Avoidance as a coping strategy may also be one of the reasons behind the reduced participation in occupational and social roles documented in people with SD (Smith et al., 1998; Zwirner et al., 1992, 1997). Although these studies documented reduced participation, their results must be interpreted with caution because they did not specifically explore the mechanisms behind the role reduction (e.g. purposeful avoidance of situations vs. reduced invitations or opportunities to participate in situations). Evidence was not found that coping strategies have been the focus of prior research with people with SD. While coping styles have been explored in teachers with voice disorders (de Jong et al., 2003), caution should be exercised in extrapolating results from that study to the SD population because of different diagnoses and populations. Caution is also warranted in attempting to reconcile psychological coping profiles defined from the researchers’ perspectives with the participants’ interpretations of what it means to cope with a disability.
3.1.3. Communicating in the world around me
The third theme, communicating in the world around me, addresses those issues external to the participants that help to shape the consequences of SD. These external influences could either inhibit or facilitate participation. The first sub-theme is some places are hard and describes characteristics of the physical environment that influence how well people are able to participate in activities. Background noise and telephone use were the two issues in the physical environment that caused the greatest difficulty for participants. Prior research has also documented the problems people with SD have in talking on the phone (Smith et al., 1998) or communicating in situations such as parties or social gatherings where there is background noise (Langeveld, van Rossum et al., 2001; Smith et al., 1998).
The second sub-theme is people make a difference. For most participants, people in their environments exerted a large influence in their experiences with SD. In general, familiar people facilitated participation because familiar people knew about the voice problem and were often accommodating of communication challenges. Friends and family also knew so much more about the participants’ personalities, capabilities and other characteristics that they were much less likely to make inappropriate inferences about the participants based on the sound of the voice. Unfamiliar people tended to be less patient and less accommodating of communication difficulties. However, most participants reported being the recipients of unpleasant comments or reactions from both familiar and unfamiliar people because of their voices. Concern about the reactions of other people such as being ridiculed or ignored has been documented in people with voice disorders (Scott, Robinson, Wilson, & Mackenzie, 1997). Several of the voice questionnaires that explore the psychosocial impact of voice disorders include questions regarding the reactions of other people in the person's environment (Deary et al., 2003; Jacobson et al., 1997; Ma & Yiu, 2001; Wilson et al., 2004). Beyond these examples, research investigating the role of other people in shaping the consequences of SD was not found.
The third sub-theme in this category is SD has deprived me of certain roles. Although there was a range of experiences, most participants found that because of the SD, they had at some time either eliminated roles from their lives that they were no longer able to fulfill (such as quitting a job), or that they were not as fully involved in roles as they would have liked to have been. These findings support prior research showing a moderate to severe impact of SD on participation in occupational or social roles (Smith et al., 1998; Zwirner et al., 1992, 1997). One salient observation was that participation in social roles meant more to participants than simply being present at an event or performing an activity. Success of participation was based on their own judgments of their level and quality of involvement, as well as their interaction or connection with the community surrounding that role. This suggests that participation in social roles may not be adequately evaluated by a tally of how often or even how well someone performs an activity according to some external or normative standard, but that the individual's appraisal of the quality of involvement is the necessary measure (Perenboom & Chorus, 2003).
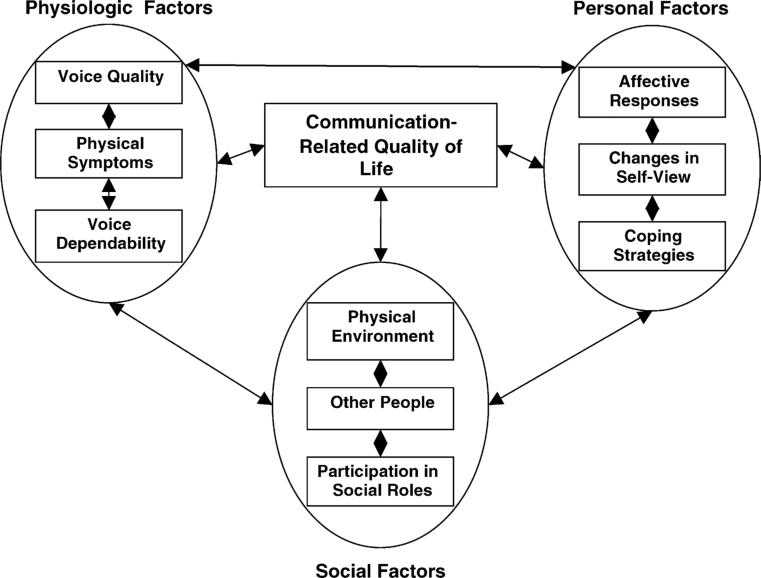
3.2. A proposed model of the consequences of SD
The results of this study suggest that there are complex interactions among the various biological and psychosocial factors that arise as a consequence of SD. One way of appreciating the relationships among factors is to propose a model containing the relevant domains and hypothesizing about potential relationships among the domains. Fig. 1 depicts a model that reflects the results of the current study and is consistent with research literature related to SD. Note that the term ‘communication-related quality of life’ is at the center of the model. Before describing the factors that contribute to this model, some explanation of this term will be provided.
Fig. 1.
A model of the insider's experiences of SD that shape communication-related quality of life.
The term ‘activity-related quality of life’ was introduced by Johnston and Miklos (2002) and refers to an assessment of quality of everyday life that includes both what a person does (functional activities, community participation and behaviors) and that individual's feelings about or appraisal of those activities. An evaluation of activity-related quality of life is an overall judgment that an individual with a disability makes about the quality of his or her performance of functional activities and involvement in life situations. In this study, the term has been modified to apply to situations that relate specifically to communication activities.
In the proposed model, three main factors contribute to communication-related QOL. These factors correspond to the three primary themes identified in this study. These three factors are compatible with the biopsychosocial interpretation of the ICF model (Eadie, 2003; Threats, 2002; Yorkston et al., 2001). However, the model proposed in this study was derived from the insider's perspective of his or her own experiences with the communication disorder. This perspective contrasts with the ICF model that is often interpreted from an outsider's or interventionist's perspective (Peters, 1996).
The first factor in the proposed model is a physiologic factor. This factor corresponds to the theme of my voice does not work and includes experiences that are most directly related to the physical voice impairment. The three primary physiologic factors identified in this study are voice quality (my voice sounds different), physical symptoms (talking requires physical effort), and voice dependability (my voice is undependable). The second factor, the personal factor, relates to the theme of my personal experience with SD and includes the three components of affective responses (SD changes how I feel about myself), changes in self-view (my voice does not represent me), and coping strategies (I just deal with it). The personal factors section of the model captures one portion of the contextual component of the ICF that addresses influences internal to the person. Although the ICF acknowledges the role of personal factors, it does not formally code them in documenting the consequences of disability because of the tremendous individual variability (Schneidert, Hurst, Miller, & Ustun, 2003; Threats, 2002). This lack of detail related to personal factors in assessing the consequences of a disability is of concern because of the important role these factors evidently played in shaping the consequences of SD in this study. Understanding personal factors is necessary for understanding communication-related QOL.
The third factor in the qualitative model is the social factor. This corresponds to the second portion of the contextual component of the ICF—the external environmental influences. In this study the social factors, described by the theme communicating in the world around me, include the physical environment (some places are hard), other people (people make a difference), and participation in social roles (SD has deprived me of certain roles). The explanatory model proposed in this study reflects the premise that these biopsychosocial (physiologic, social and personal) factors interact with one another to directly or indirectly influence communication-related QOL.
3.3. Clinical implications
Improving communication-related QOL is a central goal of most rehabilitation efforts in the field of speech-language pathology. Clinicians strive to identify what communication activities are relevant and important in the lives of individual clients, and then work to help clients achieve a level of involvement in those situations that is functional and satisfactory. In order to meet these goals, it is important to understand the complex interactions among the various biological and psychosocial factors that arise as a consequence of the communication disorder, in this case SD. Achieving that understanding requires integrating information from multiple perspectives including those of the interventionist, the outsider and the insider (Peters, 1996). The clinician needs information from traditional impairment or activity-based measures such as videostroboscopy and voice quality ratings, as well as information from the patient regarding his or her experiences with the physical, personal and social manifestations of the disorder. Although existing voice-related instruments document psychosocial consequences of SD (Benninger et al., 2001; Courey et al., 2000; Hogikyan et al., 2001; Rubin et al., 2004), results from the present study, based on the insider's perspective, suggest that there is still room for further work in this area.
Using a different methodology, this study has explored the biopsychosocial consequences of SD and has highlighted three issues in understanding communication-related QOL that warrant further discussion. These issues have important clinical implications. The first issue is that each of the three primary factors in the communication-related QOL model (physiologic, personal and social) must be evaluated along with all of the subcomponents of these factors. Results of the interviews demonstrate that description of only a few sub-components such as voice quality, physical effort and performance of social roles (which are some of the most common questions asked in clinics) do not fully capture the consequences of SD. All components of the model contained some level of relevancy for all participants and needed to be included to understand what enhanced or detracted from communication-related QOL for each individual. As revealed in the literature review, it appears that some components of the model such as dependability of the voice, the role of other people, coping strategies, and changes in self-view have not been specifically or extensively addressed in prior research. Hence, our understanding of the biopsychosocial consequences of SD is still incomplete.
The second issue raised by this study is that the unique relationships among the components of the model must be identified for each client. While all the components of the model were relevant to some degree for each participant in this study, there were widely varying patterns among participants in terms of what issues contributed most to communication-related QOL, and how these issues interacted for each person. For example, one participant, M.A., felt that the physical symptom of effort and the environmental factor of background noise were the greatest sources of frustration and the most critical issues that limited his communication-related QOL. For this participant, the presence of many familiar and supportive people as well as his own coping philosophy facilitated almost full participation in desired roles, despite the frustration that reduced his communication-related QOL. In contrast, participants such as B.W. and A.T. felt that other people were barriers to participation far more often than they were facilitators of participation. These participants strongly felt that the negative reactions of other people and the inability to be themselves greatly reduced social role participation and detracted from their communication-related QOL. These examples demonstrate that it is not adequate to simply identify the physiologic, personal and social factors as separate components of the model, but that the relationships among the components also require investigation. The results of this study also show that some factors of the model do not appear to consistently predict other factors of the model. For instance, it appeared that similar experiences of impairment-related issues (such as physical effort) did not predict similar degrees of social role restrictions or affective responses across participants. There were somewhat unique interactions and relationships among the components of the model for each participant that ultimately revealed the profile of consequences for each individual. Failure to explore each of the model's components and the relationships among the components may contribute to inadequate appreciation of the consequences of SD.
The third issue raised by this study is that the experience of disability is multidimensional and, therefore, calls for multidimensional interventions (Schneidert et al., 2003). Given a historical tendency to interpret disability primarily from an impairment perspective, the instinctive response of clinicians may be to focus on the physiologic factors as the source of poor communication-related QOL and the most important targets of intervention. For example, when a client with SD complains about insensitive comments from other people or exclusion from occupational opportunities, the tendency is to attribute the cause of the problem to the sound of the voice. This perspective obscures other contributing factors such as lack of understanding and tolerance in the social environment for people with disabilities, as well as potential discriminatory practices in work settings, whether intentional or unintentional. Recognizing that these external social factors can shape communication-related QOL as much as does physical impairment reminds the clinician to search for intervention strategies from multiple approaches. While remediation of physical impairment should surely be a key objective when it is possible, cure of impairment is not currently a feasible option in chronic conditions such as SD. However, helping the client to educate family and friends about SD in such a way that gains the support and assistance of people in the social community can improve communication-related QOL by reducing unpleasant interactions with others. Advocating with the client for appropriate and feasible changes in the workplace might facilitate ongoing productive employment. Similar examples might be drawn for the personal factors that influence the consequences of SD. The key point is to look more broadly at the environmental and personal contextual factors that can contribute to communication-related QOL and are also appropriate targets of intervention.
Clinically, it is essential to understand each individual's communication-related QOL profile including the factors that contribute to the profile, the relationships and interactions among these factors, and the multidimensional causes that shape these factors. This profile can contribute to identifying and implementing meaningful intervention goals. Qualitative methods have been used to understand the behaviors, contexts, people and feelings relevant to communication disorders for clients with chronic aphasia, and these profiles have enabled intervention that has greatly enhanced social participation and quality of life (Simmons-Mackie & Damico, 2001). Similar applications may be helpful in enhancing intervention and documentation strategies for people with SD and other types of chronic dysphonia.
4. Conclusions
This study has presented a perspective of the biopsychosocial consequences of SD as experienced by the insider. The results of this study, as summarized in the model of personal experiences of SD, suggest that communication-related quality of life is shaped by multiple physiologic, personal and social factors. Understanding the biopsychosocial consequences of SD requires consideration of each model component, the unique relationships among components for every individual, and the multidimensional contributors to the insiders’ experiences. This study has identified several features of the model that are not well understood and need further research before achieving the potential clinical implications of applying a better understanding of the experience of SD to assessment and intervention activities.
This study makes several notable contributions to the research literature. First, this study uses the research method of phenomenology that has not been used extensively in prior research on the psychosocial consequences of SD. The application of this method provides a novel approach to understanding this topic and may open up new avenues for understanding the experiences of people with SD in future research. Second, this study has identified several psychosocial consequences of SD that do not appear to have received extensive attention in prior research on this topic but appear highly relevant to the participants in this study. These may be areas in need of further exploration. Finally, this study reinforces the need to recognize that the consequences of SD are complex with multidimensional causes and multidimensional implications that need to be considered in future research and in clinical work.
Although this study included a small number of participants, the large overlap among issues raised across participants suggests that a strong core of consequences of SD has been identified. It would be useful, however, for further studies to use this qualitative format with a larger number of participants to ensure that saturation of these themes is complete. Future research is also needed to explore any potential differences in consequences of SD across different participant characteristics such as type of SD, functional voice demands, and other demographic factors. This research with larger participant groups and exploration of various demographic variables will allow greater generalization of these findings. To gain a more thorough understanding of the consequences of SD, research is currently underway using qualitative methods to examine the effects of botox treatment on communication-related QOL, and to examine how participants make decisions about their botox injections based on their quality of life goals.
An important next step in understanding the consequences of SD will be to empirically test the proposed model by submitting it to statistical analysis to verify the relationships suggested by qualitative research. Testing of the model will require identification or creation of measures for each component of the model as well as for the relationships among the components. After such testing, clinical applications of the model can be pursued.
Acknowledgement
Preparation of this work was supported in part by NIH grant #1 R21 HDO45882−01 and by NIH training grant #T532DC00033.
The authors wish to thank Allen Hillel, M.D. and Patricia Waugh, M.S., CCC-SLP for their assistance in participant recruitment. Appreciation is also expressed to Linda Balsiger for her assistance in transcription verification. Finally, the authors wish to thank the participants for their generous donation of time and insight for this project.
Appendix A. Self-study questions
- This study follows the phenomenological tradition of research. Which statement best describes this method?
- A qualitative research tradition that seeks to explore the lived experiences of participants in their natural contexts.
- An experimental research design that predicts the lived experiences of participants in their natural contexts.
- A qualitative research method in which research variables are strictly controlled to prevent natural contexts from influencing results.
- A quantitative research method that uses mathematical algorithms to determine salient themes in interview data.
- A data collection method in which researchers restrict the information gleaned from subjects through the use of highly defined questionnaire protocols.
- This study identified three primary themes that defined the general psychosocial consequences of SD. What were the three main types of consequences?
- Impact on financial well-being; personality changes; and environmental changes.
- Changes in the sound of the voice, increased physical effort required to produce voice, and altered reliability of the voice.
- Changes in the physical function of the voice, an inner personal experience of SD, and altered function in the external environment.
- Changes in interactions with other people, changes in participants’ personalities, and difficulty coping.
- Difficulty talking on the phone, difficulty talking in noisy settings, and difficulty talking with hard of hearing conversational partners.
- The reactions of other people greatly influenced the consequences that participants experienced related to their SD. What was the characteristic of other people that participants focused on most and seemed to most heavily determine how other people contributed to the consequences of SD?
- Socio-economic status
- Duration of relationship
- Gender
- Familiarity of other person
- Age of other person
- While the general topic of psychosocial consequences of SD would benefit from further research overall, this study identified several psychosocial consequences of SD appear to have received very little or no attention in the research literature. What are two of these consequences that the authors felt are particularly under-represented in the literature?
- The sound of the voice and the reactions of other people.
- The dependability of the voice and the role of other people in shaping consequences.
- Coping strategies and the experience of physical effort and fatigue.
- Conditions in the physical environment and changes in voice quality.
- Affective changes and social role changes.
- The authors summarized the findings in a model called the communication-related quality of life model. The authors emphasized several key points about this model including:
- Each component of the model can be considered in isolation to achieve an understanding of the experience of SD.
- The physical experience of voice change is the dominant component of the model in shaping the consequences of SD.
- Interactions among components of the model are unidirectional in that environmental variables shape inner personal experiences but not vice-versa.
- Each individual has a pattern of interaction among components of the model that is highly similar to other people with SD.
- The experiences of SD are multidimensional, complex and highly individualized, and these features carry important consequences for clinical intervention.
References
- Adams SG, Hunt EJ, Charles DA, Lang AE. Unilateral versus bilateral botulinum toxin injections in spasmodic dysphonia: Acoustic and perceptual results. Journal of Otolaryngology. 1993;22(3):171–175. [PubMed] [Google Scholar]
- Aronson AE, McCaffrey TV, Litchy WJ, Lipton RJ. Botulinum toxin injection for adductor spastic dysphonia: Patient self-ratings of voice and phonatory effort after three successive injections. Laryngoscope. 1993;103:683–692. doi: 10.1288/00005537-199306000-00019. [DOI] [PubMed] [Google Scholar]
- Benner P. Interpretive phenomenology: Embodiment, caring, and ethics in health and illness. SAGE Publications, Inc.; Thousand Oaks: 1994. [Google Scholar]
- Benninger MS, Ahuja AS, Gardner G, Grywalski C. Assessing outcomes for dysphonic patients. Journal of Voice. 1998;12(4):540–550. doi: 10.1016/s0892-1997(98)80063-5. [DOI] [PubMed] [Google Scholar]
- Benninger MS, Gardner G, Grywalski C. Outcomes of botulinum toxin treatment for patients with spasmodic dysphonia. Archives of Otolaryngology Head and Neck Surgery. 2001;127:1083–1085. doi: 10.1001/archotol.127.9.1083. [DOI] [PubMed] [Google Scholar]
- Blitzer A, Brin MF, Stewart CF. Botulinum toxin management of spasmodic dysphonia (laryngeal dystonia): A 12-year experience in more than 900 patients. Laryngoscope. 1998;108:1435–1441. doi: 10.1097/00005537-199810000-00003. [DOI] [PubMed] [Google Scholar]
- Brin MF, Blitzer A, Fahn S, Gould W, Lovelace RE. Adductor laryngeal dystonia (spastic dysphonia): Treatment with local injections of botulinum toxin (Botox). Movement Disorders. 1989;4(4):287–296. doi: 10.1002/mds.870040401. [DOI] [PubMed] [Google Scholar]
- Cannito MP. Emotional considerations in spasmodic dysphonia: Psychometric quantification. Journal of Communication Disorders. 1991;24:313–329. doi: 10.1016/0021-9924(91)90006-5. [DOI] [PubMed] [Google Scholar]
- Cannito MP, Murry T, Woodson GE. Attitudes toward communication in adductor spasmodic dysphonia before and after botulinum toxin injection. Journal of Medical Speech-Language Pathology. 1994;2(2):125–133. [Google Scholar]
- Courey MS, Garrett CG, Billante CR, Stone RE, Portell MD, Smith TL, et al. Outcomes assessment following treatment of spasmodic dysphonia with botulinum toxin. Annals of Otology Rhinology and Laryngology. 2000;109:819–822. doi: 10.1177/000348940010900906. [DOI] [PubMed] [Google Scholar]
- Creswell JW. Qualitative inquiry and research design: Choosing among five traditions. Sage Publications; Thousand Oaks: 1998. [Google Scholar]
- Cruice M, Worrall L, Hickson L. Quality-of-life measurement in speech pathology and audiology. Asia Pacific Journal of Speech, Language and Hearing. 2000;5:1–20. [Google Scholar]
- Damico JS, Simmons-Mackie NN. Qualitative research and speech-language pathology: A tutorial for the clinical realm. American Journal of Speech-Language Pathology. 2003;12(2):131–143. doi: 10.1044/1058-0360(2003/060). [DOI] [PubMed] [Google Scholar]
- de Jong FICRS, Cornelis BE, FL W, Kooijman PGC, Schutte HK, Oudes MJ, et al. A psychological cascade model for persisting voice problems in teachers. Folia Phoniatrica et Logopaedica. 2003;55(2):91–101. doi: 10.1159/000070091. [DOI] [PubMed] [Google Scholar]
- Deary IJ, Wilson JA, Carding PN, MacKenzie K. VoiSS: A patient-derived voice symptom scale. Journal of Psychosomatic Research. 2003;54:483–489. doi: 10.1016/s0022-3999(02)00469-5. [DOI] [PubMed] [Google Scholar]
- Dijkers M. Individualization in quality of life measurement: Instruments and approaches. Archives of Physical Medicine and Rehabilitation. 2003;84(Suppl 2):S3–S14. doi: 10.1053/apmr.2003.50241. [DOI] [PubMed] [Google Scholar]
- Dijkers M, Whiteneck G, El-Jaroudi R. Measures of social outcomes in disability research. Archives of Physical Medicine and Rehabilitation. 2000;81(Suppl 2):S63–S80. doi: 10.1053/apmr.2000.20627. [DOI] [PubMed] [Google Scholar]
- Duffy JR, Yorkston KM. Medical interventions for spasmodic dysphonia and some related conditions: A systematic review. Journal of Medical Speech-Language Pathology. 2003;11(4):ix–lviii. [Google Scholar]
- Eadie TL. The ICF: A proposed framework for comprehensive rehabilitation of individuals who use alaryngeal speech. American Journal of Speech-Language Pathology. 2003;12(2):189–197. doi: 10.1044/1058-0360(2003/065). [DOI] [PubMed] [Google Scholar]
- Edgar JD, Sapienza CM, Bidus K, Ludlow CL. Acoustic measures of symptoms in abductor spasmodic dysphonia. Journal of Voice. 2001;15(3):362–372. doi: 10.1016/S0892-1997(01)00038-8. [DOI] [PubMed] [Google Scholar]
- Hayes C. The use of patient based outcome measures in clinical decision making. Community Dental Health. 1998;15:19–21. [PubMed] [Google Scholar]
- Hillel AD. The study of laryngeal muscle activity in normal human subjects and in patients with laryngeal dystonia using multiple fine-wire electromyography. Laryngoscope. 2001;111(4):1–47. doi: 10.1097/00005537-200104001-00001. [DOI] [PubMed] [Google Scholar]
- Hogikyan ND, Sethuraman G. Validation of an instrument to measure voice-related quality of life (V-RQOL). Journal of Voice. 1999;13(4):557–569. doi: 10.1016/s0892-1997(99)80010-1. [DOI] [PubMed] [Google Scholar]
- Hogikyan ND, Wodchis WP, Spak C, Kileny PR. Longitudinal effects of botulinum toxin injections on voice-related quality of life (V-RQOL) for patients with adductory spasmodic dysphonia. Journal of Voice. 2001;15(4):576–586. doi: 10.1016/S0892-1997(01)00060-1. [DOI] [PubMed] [Google Scholar]
- Jacobson BH, Johnson A, Grywalski C, Silbergleit A, Jacobson G, Benninger MS, et al. The Voice Handicap Index (VHI): Development and validation. American Journal of Speech-Language Pathology. 1997;6:66–70. [Google Scholar]
- Johnston MV, Miklos CS. Activity-related quality of life in rehabilitation and traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 2002;83(Suppl 2):S26–S38. doi: 10.1053/apmr.2002.37100. [DOI] [PubMed] [Google Scholar]
- Langeveld TPM, Luteijn F, van Rossum M, Drost HA, Baatenburg de Jong RJ. Adductor spasmodic dysphonia and botulinum toxin treatment: The effect on well-being. Annals of Otology Rhinology and Laryngology. 2001a;110:941–945. doi: 10.1177/000348940111001009. [DOI] [PubMed] [Google Scholar]
- Langeveld TPM, van Rossum M, Houtman EH, Zwinderman AH, Briaire JJ, Baatenburg de Jong RJ. Evaluation of voice quality in adductor spasmodic dysphonia before and after botulinum toxin treatment. Annals of Otology Rhinology and Laryngology. 2001b;110:627–634. doi: 10.1177/000348940111000707. [DOI] [PubMed] [Google Scholar]
- Law M. Participation in the occupations of everyday life. The American Journal of Occupational Therapy. 2002;56(6):640–649. doi: 10.5014/ajot.56.6.640. [DOI] [PubMed] [Google Scholar]
- Liu C-Y, Yu J-M, Wang N-M, Chen R-S, Chang H-C, Li H-Y, et al. Emotional symptoms are secondary to the voice disorder in patients with spasmodic dysphonia. General Hospital Psychiatry. 1998;20:255–259. doi: 10.1016/s0163-8343(98)00022-x. [DOI] [PubMed] [Google Scholar]
- Ludlow CL. Treatment of speech and voice disorders with botulinum toxin. Journal of the American Medical Association. 1990;264(20):2671–2675. [PubMed] [Google Scholar]
- Ludlow CL, Naunton RF, Sedory SE, Schulz GM, Hallett M. Effects of botulinum toxin injections on speech in adductor spasmodic dysphonia. Neurology. 1988;38:1220–1225. doi: 10.1212/wnl.38.8.1220. [DOI] [PubMed] [Google Scholar]
- Ma EP-M, Yiu EM-L. Voice activity and participation profile: Assessing the impact of voice disorders on daily activities. Journal of Speech Language and Hearing Research. 2001;44:511–524. doi: 10.1044/1092-4388(2001/040). [DOI] [PubMed] [Google Scholar]
- Murry T, Cannito MP, Woodson GE. Spasmodic dysphonia: Emotional status and botulinum toxin treatment. Archives of Otolaryngology Head and Neck Surgery. 1994;120:310–316. doi: 10.1001/archotol.1994.01880270056010. [DOI] [PubMed] [Google Scholar]
- Murry T, Rosen CA. Outcome measurements and quality of life in voice disorders. Otolaryngologic Clinics of North America. 2000;33(4):905–916. doi: 10.1016/s0030-6665(05)70251-6. [DOI] [PubMed] [Google Scholar]
- National Spasmodic Dysphonia Association [July 26, 2004]; from http://www.dysphonia.org/nsda.
- Perenboom RJM, Chorus AMJ. Measuring participation according to the International Classification of Functioning, Disability and Health (ICF). Disability and Rehabilitation. 2003;25(11–12):577–587. doi: 10.1080/0963828031000137081. [DOI] [PubMed] [Google Scholar]
- Peters DJ. Disablement observed, addressed, and experienced: Integrating subjective experience into disablement models. Disability and Rehabilitation. 1996;18(12):593–603. doi: 10.3109/09638289609166320. [DOI] [PubMed] [Google Scholar]
- Rhew K, Fiedler DA, Ludlow CL. Technique for injection of botulinum toxin through the flexible nasolaryngoscope. Otolaryngology – Head and Neck Surgery. 1994;111(6):787–794. doi: 10.1177/019459989411100615. [DOI] [PubMed] [Google Scholar]
- Roy N, Bless DM. Personality traits and psychological factors in voice pathology: A foundation for future research. Journal of Speech Language and Hearing Research. 2000;43:737–748. doi: 10.1044/jslhr.4303.737. [DOI] [PubMed] [Google Scholar]
- Roy N, Bless DM, Heisey DM. Personality and voice disorders: A superfactor trait analysis. Journal of Speech Language and Hearing Research. 2000;43:749–768. doi: 10.1044/jslhr.4303.749. [DOI] [PubMed] [Google Scholar]
- Rubin AD, Wodchis WP, Spak C, Kileny PR, Hogikyan ND. Longitudinal effects of botox injections on voice-related quality of life (V-RQOL) for patients with adductory spasmodic dysphonia. Archives of Otolaryngology Head and Neck Surgery. 2004;130:415–420. doi: 10.1001/archotol.130.4.415. [DOI] [PubMed] [Google Scholar]
- Schneidert M, Hurst R, Miller J, Ustun B. The role of environment in the International Classification of Functioning, Disability and Health (ICF). Disability and Rehabilitation. 2003;25(11–12):588–595. doi: 10.1080/0963828031000137090. [DOI] [PubMed] [Google Scholar]
- Schonweiler R, Wohlfarth K, Dengler R, Ptok M. Supraglottal injection of botulinum toxin type A in adductor type spasmodic dysphonia with both intrinsic and extrinsic hyperfunction. Laryngoscope. 1998;108:55–63. doi: 10.1097/00005537-199801000-00011. [DOI] [PubMed] [Google Scholar]
- Scott S, Robinson K, Wilson JA, Mackenzie K. Patient-reported problems associated with dysphonia. Clinical Otolaryngology. 1997;22:37–40. doi: 10.1046/j.1365-2273.1997.00855.x. [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie NN, Damico JS. Intervention outcomes: A clinical application of qualitative methods. Topics in Language Disorders. 2001;22(1):21–36. [Google Scholar]
- Smith E, Nichols S, Lemke J, Verdolini K, Gray SD, Barkmeier J, et al. Effects of voice disorders on patient lifestyle: Preliminary results. NCVS Status and Progress Report. 1993;4:237–248. [Google Scholar]
- Smith E, Taylor M, Mendoza M, Barkmeier J, Lemke J, Hoffman H. Spasmodic dysphonia and vocal fold paralysis: Outcomes of voice problems on work-related functioning. Journal of Voice. 1998;12(2):223–232. doi: 10.1016/s0892-1997(98)80042-8. [DOI] [PubMed] [Google Scholar]
- Threats TT. Evidence-based practice research using a WHO framework. Journal of Medical Speech-Language Pathology. 2002;10(3):xvii–xxiv. [Google Scholar]
- Whiteneck GG. Measuring what matters: Key rehabilitation outcomes. Archives of Physical Medicine and Rehabilitation. 1994;75:1073–1076. doi: 10.1016/0003-9993(94)90080-9. [DOI] [PubMed] [Google Scholar]
- WHO . International classification of functioning, disability and health: Icf. World Health Organization; Geneva: 2001. [Google Scholar]
- Wilson J, Webb A, Carding P, Steen IN, Mackenzie K, Deary IJ. The Voice Symptom Scale (VoiSS) and the Vocal Handicap Index (VHI): A comparison of structure and content. Clinical Otolaryngology. 2004;29:169–174. doi: 10.1111/j.0307-7772.2004.00775.x. [DOI] [PubMed] [Google Scholar]
- Worrall L, McCooey R, Davidson B, Larkins B, Hickson L. The validity of functional assessments of communication and the activity/participation components of the ICIDH-2: Do they reflect what really happens in real-life? Journal of Communication Disorders. 2002;35:107–137. doi: 10.1016/s0021-9924(02)00060-6. [DOI] [PubMed] [Google Scholar]
- Yorkston KM, Klasner ER, Swanson KM. Communication in context: A qualitative study of the experiences of individuals with multiple sclerosis. American Journal of Speech-Language Pathology. 2001;10:126–137. [Google Scholar]
- Zwirner P, Murry T, Swenson M, Woodson GE. Acoustic changes in spasmodic dysphonia after botulinum toxin injection. Journal of Voice. 1991;5(1):78–84. [Google Scholar]
- Zwirner P, Murry T, Swenson M, Woodson GE. Effects of botulinum toxin therapy in patients with adductor spasmodic dysphonia: Acoustic, aerodynamic, and videoendoscopic findings. Laryngoscope. 1992;102:400–406. doi: 10.1288/00005537-199204000-00006. [DOI] [PubMed] [Google Scholar]
- Zwirner P, Murry T, Woodson GE. Perceptual-acoustic relationships in spasmodic dysphonia. Journal of Voice. 1993;7(2):165–171. doi: 10.1016/s0892-1997(05)80347-9. [DOI] [PubMed] [Google Scholar]
- Zwirner P, Murry T, Woodson GE. Effects of botulinum toxin on vocal tract steadiness in patients with spasmodic dysphonia. European Archives of Otorhinolaryngology. 1997;254:391–395. doi: 10.1007/BF01642557. [DOI] [PubMed] [Google Scholar]