Abstract
Femoral neck fracture is one of the most common complications of hip resurfacing and considered by some to be related to reduced blood flow as a consequence of the surgical approach. We measured oxygen concentration during hip resurfacing through the trochanteric flip approach (n = 15 patients) and compared this approach with previous data for the posterior and anterolateral approaches. With the trochanteric flip the average femoral oxygenation decreased during the procedure to approximately 50% of that at the start, however it recovered to starting level by the end of the procedure. Preservation of oxygenation with the trochanteric flip was similar to that observed with the anterolateral approach, but with less variation during the procedure. Both of these approaches were superior in terms of oxygenation preservation to the posterior approach which resulted in a dramatic reduction in oxygenation.
Introduction
Resurfacing hip arthroplasty is becoming a popular alternative to THA, particularly for young active patients [5, 14]. Successful resurfacing relies on the viability of the bone in the remaining head and neck of the femur. The residual bone needs to retain its load-transmitting properties for the resurfaced femur to fulfill its mechanical function [10]. If the viability of the remaining bone is compromised, the whole construct will be weakened and this could contribute to early failures resulting from fracture because of resorption [3, 9, 12] or later fatigue failure resulting in femoral head collapse [3].
The most commonly used approach for resurfacing surgery is the extended posterior approach [11]; this approach provides good visibility for the acetabular and femoral component preparation and implantation [13]. However, some authors report this approach leads to compromise of the femoral head and neck blood supply [8, 20]. The main blood supply to the head and neck is from the deep branch of the medial femoral circumflex artery (MFCA) [7, 21]. During resurfacing through the extended posterior approach, the branches of the MFCA passing along the short external rotators to the femoral head are destroyed [20]. It also is possible to use an anterolateral approach for resurfacing [13, 17]; this approach appears to preserve the femoral head and neck blood supply but blood flow in the femoral head depends on intraoperative leg positioning [18], suggesting the branches of the MFCA are temporarily occluded. Ganz et al. [6] advocated the trochanteric flip for preserving femoral blood supply.
The majority of revisions of hip resurfacing reportedly are attributable to atraumatic fracture of the femoral neck [15, 16, 19, 22]. These fractures have been attributed to devascularization-induced weakening of the bone [9]. The standard posterior approach for hip resurfacing reduces the femoral head blood supply [1, 8, 20], therefore it is likely devascularization is a result of the surgical technique. There also is evidence the anterolateral approach leads to less disruption of blood supply during hip resurfacing which is explained by preservation of the deep branch of the medial femoral circumflex artery [18].
We wished to (1) measure intraoperative femoral head oxygenation during hip resurfacing using the trochanteric flip and (2) compare the oxygenation with that reported in previous studies of the posterior [20] and anterolateral [18] approaches.
Materials and Methods
We recruited 15 patients undergoing routine metal-on-metal hip resurfacing for primary osteoarthritis. All procedures were performed by two surgeons (DF, MN) with the patients under spinal anesthesia. We performed the trochanteric flip approach in each case. All patients received the uncemented Cormet hip resurfacing prosthesis (Corin Group Plc, Cirencester, UK). There were 10 male and five female patients. Their mean age was 50 years (range, 39–62 years). The preoperative diagnosis was osteoarthritis for all but one patient; this patient had avascular necrosis (AVN). Informed consent for participation in the study was obtained from each patient. The study had local ethical committee approval.
The measurements from this group of patients undergoing the trochanteric flip approach were compared with previously reported measurements made on patients receiving hip resurfacing using the posterior [20] and the anterolateral approaches (Table 1) [18].
Table 1.
Patients’ details
| Approach | Number of patients | Gender ratio M:F | Mean age (years) | Age range (years) | Diagnosis | Anesthesia | Ventilation |
|---|---|---|---|---|---|---|---|
| Extended posterior | 15 | 66:33 | 55.8 | 24–70 | OA (100%) | General | Intubation |
| Anterolateral | 12 | 50:50 | 58 | 39–73 | OA (100%) | Spinal | Face mask |
| Trochanteric flip | 15 | 66:33 | 50 | 39–62 | OA (93%) AVN (7%) |
Spinal | Laryngeal mask (9) Face mask (6) |
OA = osteoarthritis; AVN = avascular necrosis.
We measured oxygen (O2) concentration using gas-sensitive electrodes. The measurement principle of the electrodes, also known as Clark electrodes [4], is based on the electrochemical reduction of oxygen. The technique for measuring oxygen and nitrous oxide in bone was described previously [20], however, we will provide a brief synopsis here.
Oxygen reduction at the surface of a silver (Ag) measurement electrode occurs when it is polarized at −0.65 V with respect to a reference silver/silver chloride (Ag/AgCl) electrode; this gives rise to a current flow, which is proportional to the oxygen concentration present. All the measurement electrodes were individually calibrated preoperatively in a solution of phosphate-buffered normal saline with known dissolved concentrations of O2.
We used spinal anesthesia in each case. Six patients received an oxygen-air mix through a face mask (open anesthetic system). The remaining nine patients received ventilation through a laryngeal mask. In each case, constant oxygen concentrations were maintained in the anesthetic gas mix throughout the entire surgery.
After spinal anesthesia, the patient was positioned laterally and the pelvis stabilized by a padded support. A standard incision for a soft tissue-sparing trochanteric flip approach was made [6]. Once the fascia lata was split, a Kirschner (K-) wire (2.3-mm diameter) was introduced into the femoral neck below the greater trochanter. It was advanced up the femoral neck under fluoroscopic guidance until the end of the wire was positioned superolaterally in the femoral head, near the head-neck junction; the K-wire then was removed. The resulting tunnel mouth in the cortical bone was widened slightly using a drill, and a size 14 Ag measurement electrode was inserted into the femur; this was held in place with a suture. Correct electrode placement was confirmed fluoroscopically. An Ag/AgCl reference electrode then was placed in the gluteus medius muscle; this reference electrode completes the measurement circuit, and it is relative to this reference that the measurement electrodes are polarized, there is no separate measurement made from this reference electrode. Both electrodes were connected to a potentiostat (Model MEC V1, optoelectronic head stage: Model MHS V1, power supply unit: Model MPS V1; EMS, Newbury, UK), which generated the correct polarizing voltages for the measurement electrode. The connections were made using 2-m long signal wires to reach beyond the sterile field. The data collection system consisted of an analog to digital converter (PowerLab; ADInstruments Ltd, Chalgrove, UK), which sampled the output current at 10 Hz, connected to a personal computer.
Baseline measures were established for oxygen in the femoral head. The operating surgeon then continued the standard trochanteric flip approach [6].
The split in the iliotibial band was continued distally and proximally between the tensor fascia lata and the gluteus maximus. The posterior border of the medius was identified and the greater trochanteric osteotomy was marked with a cautery. The vastus lateralis fascia then was elevated while keeping its integrity to the trochanteric fragment. With a thin saw blade, the trochanteric osteotomy was performed.
The vastus lateralis was elevated distally. The remainder of the attachment of the gluteus medius was released from the femur. The leg was flexed and externally rotated. After exposure of the posterosuperior and anterior aspects of the hip capsule, an incision was made along the axis of the femoral neck. The hip was dislocated and the trochanteric flip fragment was folded in anteriorly. Careful attention was paid to not damage the retinacular vessels going up to the lateral aspect of the femoral neck [2]. The resurfacing then was performed in the normal manner.
The electrodes were removed after reattachment of the trochanteric osteotomy. Validation measurements, relating gas concentration to current output, were made immediately after their removal. A more complete recalibration with three different known gas concentrations was performed in the laboratory at a later stage.
The analysis was performed in an identical manner to those in previous studies of the posterior and anterolateral approaches to facilitate a direct comparison.
We converted the intraoperative current measurements into oxygen concentrations on the basis of each electrode calibration. Baseline concentrations were considered to be the values measured immediately after electrode insertion. The subsequent gas concentration measurements were represented as a percentage of the baseline gas concentration; thus only changes relative to the baseline concentration at the start of the procedure were compared. The surgical steps were grouped in the following manner and were used as a standardized event-based time line to facilitate comparison between patients: (1) Start: measurements were taken immediately after electrode placement; (2) Approach: this step included the muscle/soft tissue divisions, capsulotomy, and dislocation. The measurement was made at the end of the approach; (3) Implantation: this step included preparation of the femur and acetabulum and insertion/fixation of the components. The measurement was made after insertion of the second component; and (4) End: the replaced joint was reduced and the capsule was repaired. The measurement was made during closure of the fascia lata.
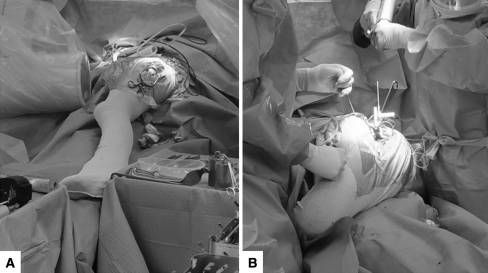
During surgery, we placed the leg in various positions to facilitate the different steps of the procedure. There were five main changes in position, going from: (1) neutral with no hip rotation and slight hip and knee flexion (Fig. 1A); (2) hip externally rotated and flexed and knee flexed (Fig. 1B); (3) neutral; (4) hip externally rotated and flexed and knee flexed; and (5) neutral.
Fig. 1A–B.
The intraoperative photographs show (A) the neutral position and (B) the hip rotated and flexed with knee flexed position.
Using the Wilcoxon signed rank test, we compared the following matched pairs of oxygen concentration at these surgical points: Start and Approach, Approach and Implantation, Implantation and End, and Start and End. We then performed a subanalysis of the oxygenation changes as a function of position to investigate the effects of the different leg positions used during surgery. The relative oxygen concentration values recorded at the end of each period spent with the leg in Positions 1 to 5 were analyzed in the following pair groups using the Wilcoxon signed rank test for matched pair analysis: Position 1 (neutral) and Position 2 (hip rotated), Position 2 and Position 3 (neutral), Position 3 and Position 4 (hip rotated), and Position 4 and Position 5 (neutral). We used SPSS, version 14.0 (SPSS Inc, Chicago, IL) for analysis.
Results
There were no surgical complications related to the oxygen concentration measurements in the femoral head. Successful data collection was achieved for all 15 patients.
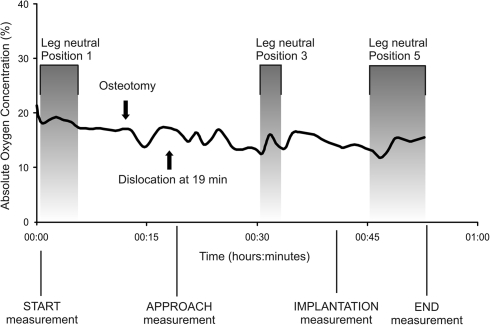
The pattern of changes in oxygen concentration was variable across the patient cohort. In an illustrative case for this cohort, baseline absolute oxygen concentration at Start in the femoral head was 22% (Fig. 2). This decreased to approximately 16% at the time of dislocation and remained consistent until the end of the Approach. During the femoral preparation (Position 2, hip rotated), the oxygen concentration remained at approximately 15%. Only minor changes in femoral head oxygen concentration (± 1%) occurred while the leg was placed in Position 3 (leg neutral) and in Position 4 (hip rotated). By the End, oxygen concentration was at approximately 15% in this patient.
Fig. 2.
The absolute oxygen concentrations in the femoral head during surgery in Positions 1, 3, and 5 are shown.
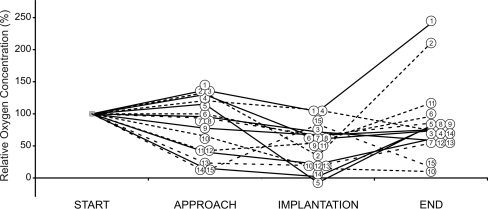
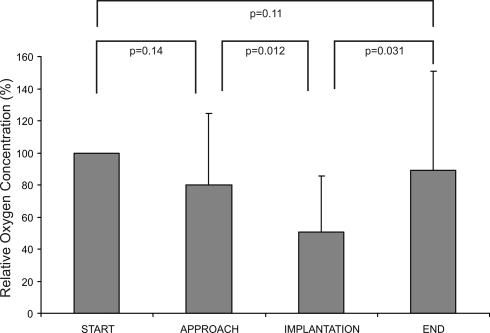
Qualitatively, we observed a similar pattern of femoral head oxygenation level changes for the entire cohort with some variation in response between patients (Fig. 3). The overall pattern was one of some decrease in femoral head oxygenation from the baseline level by the end of Approach. In all but one case, there was a decrease in relative oxygenation concentration during the preparation and component implantation phase (Fig. 3), the cohort average decreased to 51% (standard deviation [SD], 35%) relative oxygen concentration (Fig. 4); this was a reduction (p = 0.012) compared with the value at the end of Approach. All but two patients showed an increase in relative oxygen concentration by the End measurement (Fig. 3), the cohort average increasing to 89% (SD, 62%) (Fig. 4); this was an increase (p = 0.031) from the end of Implantation, but similar to the Start.
Fig. 3.
Intraoperative femoral head relative oxygenation changes for each patient during trochanteric approach are shown. The numbers on the curves identify individual patients (n = 15); the lines are alternately dashed and solid for clarity. The baseline value of oxygenation was taken as that at the start of the procedure, therefore, all plots show 100% at the Start. The majority of traces show a decrease in oxygenation during Implantation with a recovery at the End.
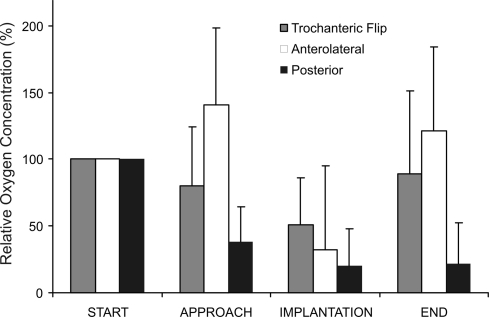
Fig. 4.
The relative femoral head oxygenation changes averaged for the cohort (n = 15) during the trochanter flip approach and results of the Wilcoxon signed rank test for matched pair analyses are shown (error bars = standard deviations). The data show oxygenation decreased during the procedure but recovered at the end.
Changes in leg position from neutral to either of the rotated positions, Position 2 or Position 4, did not reduce relative oxygen concentration in the femoral head. Conversely, straightening the leg from either of the two rotated positions did not increase femoral head relative oxygen concentration.
Discussion
The majority of revisions of hip resurfacing reportedly are attributable to atraumatic fracture of the femoral neck [15, 16, 19, 22]. These fractures have been attributed to devascularization-induced weakening of the bone [9]. We previously showed the extended posterior approach reduces oxygen concentration in the femur during resurfacing; the deep branch of the medial femoral circumflex artery is destroyed when the extended posterior approach is used [20]. In the current study, we determined whether the trochanteric flip approach maintains oxygenation of the femur and compared the effects of this approach with those of the extended posterior and anterolateral approaches.
A limitation of the current study is the fact that the ventilation method was not consistent across the entire cohort; six patients received an oxygen-air mix through a face mask and the remaining nine patients received ventilation through a laryngeal mask. However, care was taken to ensure the oxygen concentration provided in every case was maintained at a constant value throughout the procedure. In addition the analyses were performed using relative oxygen concentration changes, where the baseline measurement was the concentration at the start of the procedure for each case, and absolute oxygen concentrations were not compared.
Previous studies suggest the extended posterior approach impairs blood supply to the femoral head [1, 8, 20]. The anterolateral approach appears to preserve the blood supply, but the oxygenation was highly dependent on leg position during surgery [18]. Our data suggest the trochanteric flip approach also appears to preserve the blood supply to the femoral head, as oxygenation at the end of the procedure did not differ from that at the start. Comparing the current study results with those from a previous study of posterior and anterolateral approaches [18], clear differences between the three approaches can be observed (Fig. 5). For the anterolateral approach and the trochanteric flip approach, there was recovery of femoral oxygenation at the end of the surgery; the anterolateral approach the relative oxygenation showed more variation throughout the procedure than with the trochanteric flip approach. In contrast, the posterior approach resulted in a dramatic reduction in femoral oxygenation. These data support the concept that the main blood supply to the head is from the MFCA, and this is destroyed during the posterior approach but not with the other two approaches. During the anterolateral approach, the oxygen tension decreased when the hip was placed in extreme rotation and increased again when it was returned to a more neutral position. This suggests the MFCA was temporarily occluded. With the trochanteric flip, this positional effect was not observed, suggesting the vessels are not occluded. This difference is probably because more external rotation is needed to gain adequate exposure with the anterolateral approach than with the trochanteric flip approach. It is not clear whether the temporary decrease in oxygenation occurring during the anterolateral approach will cause problems. It may be there is no lasting effect as with a temporary tourniquet.
Fig. 5.
Our comparison between the trochanteric flip, anterolateral, and posterior approaches showed the posterior approach decreased oxygenation by the end of the procedure, in contrast to the anterolateral and trochanteric flip approaches. The anterolateral approach resulted in more variation of oxygenation levels during the procedure than the trochanteric approach.
Although the trochanteric flip provides good exposure for resurfacing, there are complications that must be considered. The most important complication is trochanteric nonunion, which may require additional surgery. Although the reported incidences are low, approximately 1.5% [6] in some series, they might be higher in others. To minimize the risk of nonunion, patients usually are restricted to partial weightbearing for 6 weeks.
Complications of hip resurfacing such as femoral neck fracture and AVN may be reduced by using blood supply-conserving surgical approaches. Preservation of blood supply also may enhance the fixation of cementless femoral components. At the end of the procedure with the trochanteric flip and anterolateral approaches, femoral head oxygenation is the same as at the start, whereas with the posterior approach, it is considerably worse. During surgery through the trochanteric flip approach, the oxygen concentration is more consistent than during surgery through the anterolateral approach. The trochanteric flip approach is blood supply-conserving and may be the optimal approach for hip resurfacing in terms of ensuring femoral head and neck viability and cementless femoral fixation.
Acknowledgments
We thank Barbara Marks and Jo Copp for their invaluable organizational help during this study.
Footnotes
One or more of the authors (DWM & HSG) have received institutional funding from the Furlong Research Foundation.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amarasekera HW, Costa ML, Foguet P, Krikler SJ, Prakash U, Griffin DR. The blood flow to the femoral head/neck junction during resurfacing arthroplasty: a comparison of two approached using laser Doppler flowmetry. J Bone Joint Surg Br. 2008;90:442–445. [DOI] [PubMed]
- 2.Beaule PE, Campbell PA, Hoke R, Dorey F. Notching of the femoral neck during resurfacing arthroplasty of the hip: a vascular study. J Bone Joint Surg Br. 2006;88:35–39. [DOI] [PubMed]
- 3.Campbell P, Beaule PE, Ebramzadeh E, LeDuff M, De Smet K, Lu Z, Amstutz HC. The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res. 2006;453:35–46. [DOI] [PubMed]
- 4.Clark LC Jr, Kaplan S, Matthews EC, Edwards FK, Helmsworth JA. Monitor and control of blood oxygen tension and pH during total body perfusion. J Thorac Surg. 1958;36:488–496. [PubMed]
- 5.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. [DOI] [PubMed]
- 6.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. [DOI] [PubMed]
- 7.Gautier E, Ganz K, Krugel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679–683. [DOI] [PubMed]
- 8.Khan A, Yates P, Lovering A, Bannister GC, Spencer RF. The effect of surgical approach on blood flow to the femoral head during resurfacing. J Bone Joint Surg Br. 2007;89:21–25. [DOI] [PubMed]
- 9.Little CP, Ruiz AL, Harding IJ, McLardy-Smith P, Gundle R, Murray DW, Athanasou NA. Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:320–323. [DOI] [PubMed]
- 10.Little JP, Taddei F, Viceconti M, Murray DW, Gill HS. Changes in femur stress after hip resurfacing arthroplasty: response to physiological loads. Clin Biomech (Bristol, Avon). 2007;22:440–448. [DOI] [PubMed]
- 11.McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip: experience of the McMinn prothesis. Clin Orthop Relat Res. 1996;329 (suppl):S89–98. [DOI] [PubMed]
- 12.Morlock MM, Bishop N, Ruther W, Delling G, Hahn M. Biomechanical, morphological, and histological analysis of early failures in hip resurfacing arthroplasty. Proc Inst Mech Eng [H]. 2006;220:333–344. [DOI] [PubMed]
- 13.Nork SE, Schar M, Pfander G, Beck M, Djonov V, Ganz R, Leunig M. Anatomic considerations for the choice of surgical approach for hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:163–170, viii. [DOI] [PubMed]
- 14.Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip: a five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. [DOI] [PubMed]
- 15.Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg Br. 2005;87:463–464. [DOI] [PubMed]
- 16.Shimmin AJ, Bare J, Back DL. Complications associated with hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:187–193, ix. [DOI] [PubMed]
- 17.Soni RK. An anterolateral approach to the hip joint. Acta Orthop Scand. 1997;68:490–494. [DOI] [PubMed]
- 18.Steffen R, O’Rourke K, Gill HS, Murray DW. The anterolateral approach leads to less disruption of the femoral head-neck blood supply than the posterior approach during hip resurfacing. J Bone Joint Surg Br. 2007;89:1293–1298. [DOI] [PubMed]
- 19.Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, McLardy-Smith P, Murray DW, Gill HS. The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg Br. 2008;90:436–441. [DOI] [PubMed]
- 20.Steffen RT, Smith SR, Urban JP, McLardy-Smith P, Beard DJ, Gill HS, Murray DW. The effect of hip resurfacing on oxygen concentration in the femoral head. J Bone Joint Surg Br. 2005;87:1468–1474. [DOI] [PubMed]
- 21.Trueta J, Harrison MH. The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg Br. 1953;35:442–461. [DOI] [PubMed]
- 22.Witzleb WC, Arnold M, Krummenauer F, Knecht A, Ranisch H, Gunther KP. Birmingham Hip Resurfacing arthroplasty: short-term clinical and radiographic outcome. Eur J Med Res. 2008;13:39–46. [PubMed]