Abstract
Porous tantalum nonmodular tibial components for TKA were introduced in 1999. We revised three well-fixed tantalum tibial trays. For removal, we used osteotomes and revision oscillating saw blades. Removal of the components was laborious and resulted in generation of abundant tantalum debris that seeded the periarticular soft tissues despite meticulous protection with gauze. The retained metallic debris that is visible on postoperative radiographs has the potential for generation of third-body wear. We alert the orthopaedic community about this phenomenon and recommend minimizing the use of motorized revision instruments for removal of trabecular metal implants.
Introduction
Porous tantalum, a metal with an appearance similar to cancellous bone, currently is available for use in several orthopaedic applications, including hip and knee arthroplasties [5]. The open-cell structure of tantalum is produced via carbon vapor deposition/infiltration of commercially pure tantalum onto a vitreous carbon scaffolding. This transition metal is characterized by a high volumetric porosity (70%–80%), low modulus of elasticity (3 MPa), and high frictional characteristics. It provides excellent bone and fibrous ingrowth properties allowing for rapid and substantial bone and soft tissue attachment [5].
The initial results of uncemented porous tantalum fixation in THA are encouraging [2, 6]. Porous tantalum nonmodular tibial components for TKA were introduced in 1999. The design rationale combines the advantages of tantalum porous fixation [1, 5] and a nonmodular plastic insert, thus eliminating cement fixation and backside wear. Eight years after their introduction, we were not able to find any published reports on the early clinical performance of these uncemented components in primary knee arthroplasty.
Nasser and Poggie [7] reported encouraging results with the use of a porous tantalum implant for augmentation or arthroplasty of the patella in 11 patients who underwent revision TKA with poor patellar bone stock preventing the use of conventional implants.
Recently, Klein et al. [4] recognized the potential for generation of tantalum debris during removal of well-fixed knee arthroplasty tantalum implants. It is concerning that the metallic debris potentially can seed the periarticular soft tissues and may be difficult to completely remove during surgery.
We report the cases of three patients who underwent revision of well-fixed tantalum tibial trays with generation of abundant tantalum debris.
Case Reports
One of us (AGDV) revised a well-fixed uncemented trabecular metal (tantalum) monoblock tibial component in three patients for painful arthrofibrosis (Table 1). All removed implants were NexGen® Complete Knee Solution Legacy® Posterior Stabilized Knee components (Zimmer, Inc, Warsaw, IN). All patellar components and one of the three femoral components were fixed with cement. All patients were referred from outside institutions.
Table 1.
Demographic and preoperative and postoperative variables
| Variable | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Demographic and preoperative | |||
| Age (years) | 50 | 60 | 74 |
| Gender | Female | Male | Male |
| Side | Left | Right | Right |
| Body mass index (kg/m2) | 36 | 25.5 | 33.8 |
| Previous surgeries | 2 (arthroscopy—unicondylar knee replacement) | None | 1 (arthroscopy) |
| Time in situ (months) | 21 | 15 | 14 |
| Alignment | 6° varus | 6° valgus | 4° valgus |
| Posterior tibial slope | 3° | 5° | 4° |
| Range of motion | 0°–80° | 50°–90° | 20°–80° |
| Pain during ambulation | Severe | Severe | Severe |
| Postoperative variables | |||
| Followup (months) | 9 | 3 | 9 |
| Knee Society score | 69–90 | 64–85 | 59–61 |
One of the patients presented with limited flexion and the other two with severe limitation of flexion and extension (Table 1). Our decision for recommending revision of both components was based on (1) long-standing and severe limitation of motion and pain (Table 1); (2) the fact that the nonmodular tibia tray does not allow downsizing the polyethylene insert; and (3) the limited value of soft tissue releases for treatment of arthrofibrosis [3].
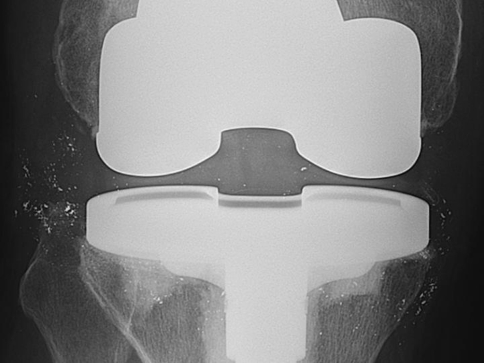
Revision surgery was performed between April 2007 and August 2007 under combined spinal and epidural anesthesia. A midline longitudinal incision combined with a standard medial parapatellar arthrotomy was used. No extended surgical exposure techniques were necessary. Arthrofibrosis was detected in all cases, with dense fibrous tissue extending into the medial and lateral gutters, suprapatellar pouch, and the prepatellar area. All tibial and femoral components were well sized and well fixed (Fig. 1). Femoral and tibial components were revised in all patients. The well-fixed femoral components were removed with minimal bone loss. Removal of the tantalum tibial components was laborious in all patients. We used narrow osteotomes in the anterior and medial aspects of the bone-tantalum interface. For the deeper portion of the interface, we used thin revision oscillating saw blades. Progressive opening of the bone-tantalum interface was associated with generation of abundant tantalum debris. We attempted to contain dispersion of the debris by covering the periarticular soft tissues with moist gauze; however, the posterior aspect of the gutters and posterior pseudocapsule remained unprotected and were seeded with abundant debris. To remove the tantalum debris, we thoroughly irrigated the periarticular soft tissues with pulsatile lavage.
Fig. 1.
A preoperative radiograph shows a well-fixed, sized, and aligned TKA.
After removal of the components, the tibial bone bed had abundant metallic debris. The tantalum pegs were removed with thin osteotomes in two of the patients in whom the surgeon judged removal of the pegs would not jeopardize integrity of the proximal tibia. In one of the three revisions, the lateral tantalum fixation peg was at the outermost lateral edge of the tibial plateau, violating the lateral cortex. It was not removed to avoid associated loss of bone support. After component removal, there was a solid tibial bone bed that allowed use of standard revision tibial trays without the need for blocks or wedges.
Postoperative radiographs showed abundant metallic debris in the periarticular soft tissues (Figs. 2, 3).
Fig. 2.
A postoperative radiograph in the lateral view (Patient 2) shows abundant metallic debris predominantly located in the posterior knee pseudocapsule.
Fig. 3.
A postoperative radiograph in the anteroposterior view (Patient 3) shows abundant metallic debris predominantly located in the medial and lateral gutters.
After followups of 9, 3, and 9 months, none of the patients had osteolysis or polyethylene wear (Table 1). We continue to monitor these patients closely at 12-month intervals to determine if there is any migration of the metallic particles or signs of early osteolysis attributable to third-body wear.
Discussion
Tantalum monoblock tibial components do not offer the advantage of modularity during revision knee surgery. Therefore, during revision surgery, the surgeon may need to remove a well-fixed tantalum tibial component. In this limited experience, the revisions of these components were more laborious than those of well-fixed cemented components and were associated with the unwanted dispersion of metallic debris.
Our findings during and after revision surgery are concerning. Despite a meticulous surgical technique and attention to minimizing metallic dispersion, postoperative radiographs showed abundant debris with potential for local inflammatory reaction and third-body wear [4].
Recently, Klein et al. [4] reported the use of a broad 3-cm flat osteotome inserted at the tantalum-bone interface in four revision cases, which they suggested minimized metallic debris generation and preserved bone stock. They recommended beginning anterior to the tibial pegs. Once the tibial pegs are encountered, firm impaction of the osteotome will separate the tibial pegs from the prosthesis. After this, the posterior tantalum-bone interface can be disrupted by careful osteotome impaction [4]. In addition, they mentioned these two fixation pegs can be left in the proximal tibia or removed, depending on clinical indication, surgeon preference, and the space required for the stem or keel of the revision tibial prosthesis [4].
Another option for removal of the well-fixed implants in our patients would have been choosing a lower resection plane distal to the bone tantalum interface. Although generation of metallic debris would have diminished, this would have resulted in unnecessary loss of bone stock. Moreover, some metallic debris would have been generated during section of the fixation pegs.
We recommend against using motorized saw blades for removal of well-fixed porous tantalum tibial components. Despite attention to detail and an attempt to remove visible debris, postoperative radiographs showed abundant metallic particles around the new revision implants. We are closely monitoring our patients for signs of third-body wear.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Cohen R. A porous tantalum trabecular metal: basic science. Am J Orthop. 2002;31:216. [PubMed]
- 2.Cohn R, González Della Valle A, Cornell C. Similar wear in total hip arthroplasties with metallic and Zirconia femoral heads. HSS J. 2008;4:107–111. [DOI] [PMC free article] [PubMed]
- 3.González Della Valle A, Leali A, Haas S. Etiology and surgical interventions for stiff total knee replacements. HSS J. 2007;3:182–189. [DOI] [PMC free article] [PubMed]
- 4.Klein GR, Levine HB, Hartzband MA. Removal of a well-fixed trabecular metal monoblock tibial component. J Arthroplasty. 2008;23:619–622. [DOI] [PubMed]
- 5.Levine BR, Sporer S, Poggie RA, Della Valle CJ, Jacobs JJ. Experimental and clinical performance of porous tantalum in orthopedic surgery. Biomaterials. 2006;27:4671–4681. [DOI] [PubMed]
- 6.Malizos KN, Bargiotas K, Papatheodorou L, Hantes M, Karachalios T. Survivorship of monoblock trabecular metal cups in primary THA: midterm results. Clin Orthop Relat Res. 2008;466:159–166. [DOI] [PMC free article] [PubMed]
- 7.Nasser S, Poggie RA. Revision and salvage patellar arthroplasty using a porous tantalum implant. J Arthroplasty. 2004;19:562–572. [DOI] [PubMed]