Abstract
Navigation systems have been developed to achieve more reliable prosthetic alignment in TKAs. However, the component alignment in the sagittal plane is reportedly less reliable than in the coronal plane even with navigation systems. We measured and compared sagittal prosthetic alignments for TKAs with the conventional technique and three navigation approaches to establish reference frames, using radiographs of the entire lower extremity while standing. The sagittal alignments simulated on the radiographs with the conventional technique and navigation systems differed by a mean of 2° to 4°. Use of navigation systems resulted in a mean of 1° to 4° hyperextension between the femoral and tibial components and use of the conventional technique resulted in a mean of 1° flexion. Use of different reference points on the distal femoral condyle for the navigation systems resulted in differences of as much as 3° alignment in the sagittal plane. Although optimal prosthetic alignment for TKA in the sagittal plane is unknown, surgeons and technicians using navigation systems should be aware of this difference in the sagittal plane and the risk of hyperextension between the femoral and tibial components, which might be associated with osteolysis and anterior post-cam impingement.
Introduction
Alignment of the prosthesis is one factor in determining the longevity of a TKA [1, 6, 12, 16, 17]. Navigation systems have been developed to provide more reliable alignment and are coming into widespread use. Previous studies showed navigation systems for TKA improve mean alignment only a few degrees in, but reduce the number of outliers of femoral and tibial component alignment relative to the mechanical axis in the coronal plane compared with conventional techniques [3, 7, 10, 14, 15]. However, the component alignment in the sagittal plane is less reliable than in the coronal plane even with navigation systems [3, 7, 10, 14, 15]. Although the relationship between sagittal alignment and long-term outcomes is unknown, hyperextension between the femoral and tibial components reportedly increases the risk of osteolysis [4] and anterior tibial post impingement with posterior-stabilized prostheses [2, 8]. Therefore, sagittal component alignment is important.
Optimal prosthetic alignment for a TKA in the sagittal plane is unknown. Thus, the methods used to decide sagittal prosthetic alignment using conventional techniques and navigation systems are conceptually different. With conventional techniques, sagittal prosthetic alignment is based on limited anatomic features that are palpable during surgery and determined intraoperatively with intramedullary or extramedullary rods. With navigation systems, sagittal prosthetic alignment is based on the mechanical axis of the entire femur and tibia. Thus, sagittal alignments intended with conventional techniques and navigation systems might differ. If the intended sagittal alignments between these techniques differ, then postoperative sagittal alignments between these techniques inherently differ. Therefore, it is important to analyze the sagittal alignments intended with conventional techniques and navigation systems. The targeted sagittal prosthetic alignment toward femoral and tibial axes differs according to the prosthetic design, because some prostheses are designed to be implanted with a posterior slope toward these axes. Even for such prostheses, however, sagittal prosthetic alignment was established on the basis of the femoral and tibial axes.
Our first purpose was to determine if the sagittal alignments targeted by conventional TKA instruments and by navigation systems were substantially different by comparing the axes for the sagittal prosthetic alignments. Our second purpose was to determine if the intended sagittal angles between the femoral and tibial components while standing were in the extended position by comparing the relationship between the femoral and tibial axes for sagittal prosthetic alignments.
Materials and Methods
We obtained standing sagittal radiographs from 20 lower limbs from 10 male Japanese volunteers (mean age, 27 years; range, 24–31 years) who had no radiographic abnormalities of the lower extremities. Their mean height was 172 cm (range, 160–178 cm) and mean body weight was 68 kg (range, 52–90 kg). Using lateral radiographs of the subject’s whole lower extremity while in one-legged stance, we simulated the sagittal femoral and tibial axes for TKA with the conventional technique and navigation systems. Differences between the axes using the conventional technique and three navigation approaches were evaluated to establish reference frames and the relationship between femoral and tibial axes while standing were analyzed. Owing to the lack of previous long-term clinical reports measuring sagittal alignment, a clinically important size of difference was unclear. Previous reports on TKA navigation often used 3° as the threshold for outliers of component alignment in coronal and sagittal planes [3, 7, 10, 14, 15]. Therefore, we used 3° as effect size. Our results showed the standard deviations of navigation femoral axis (NFA) 1–3, navigation tibial axis (NTA), conventional femoral axis (CFA), and conventional tibial axis (CTA) were smaller than 3°. We thus used 3° as standard deviation for a post hoc power analysis. When the power was set at 0.9 (relatively high power) and the significance was set at p < 0.05, 12 cases were required. Each volunteer provided informed consent to participate in this study, which was approved by our Institutional Review Board.
Lateral radiographs of the lower extremity with the patients in one-legged stance were obtained using the method described by Minoda et al. (Fig. 1) [11]. Film size 252 x 905 mm (SR-G; Konica, Tokyo, Japan) and a screen (LC-S3; Toshiba, Tokyo, Japan) were used. The xray beam was centered at the knee at a distance of 200 cm. A grid (film-focus distance, 130 cm-∞; grid ratio, 6:1; grid line, 34/cm) (Mitaya Co, Tokyo, Japan) was used. The settings of the xray beam were 90 kV and 20 to 40 mA, depending on limb size. Radiographs were obtained in the following manner: (1) the knee was fully extended in weightbearing; (2) subjects were instructed to face laterally so the posterior edges of the medial and lateral femoral condyles were aligned; and (3) a graduated, lead-loaded acrylic filter (0.2 mpb) was placed in front of the collimated xray beam for lateral radiographs so the femoral head received high-energy exposure with the knee and ankle receiving relatively low-energy exposure. If both posterior condyles were not aligned, another radiograph was taken.
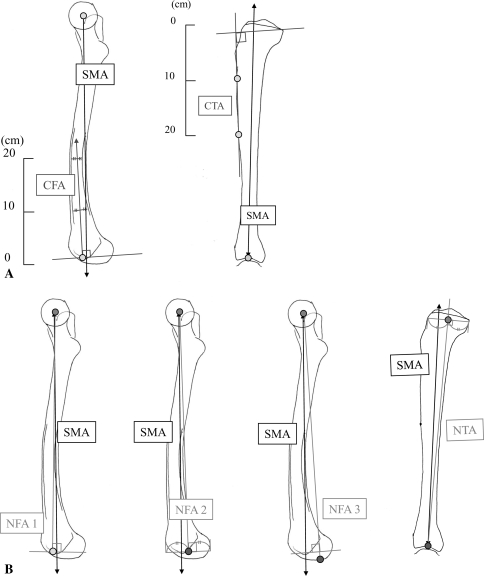
Fig. 1.
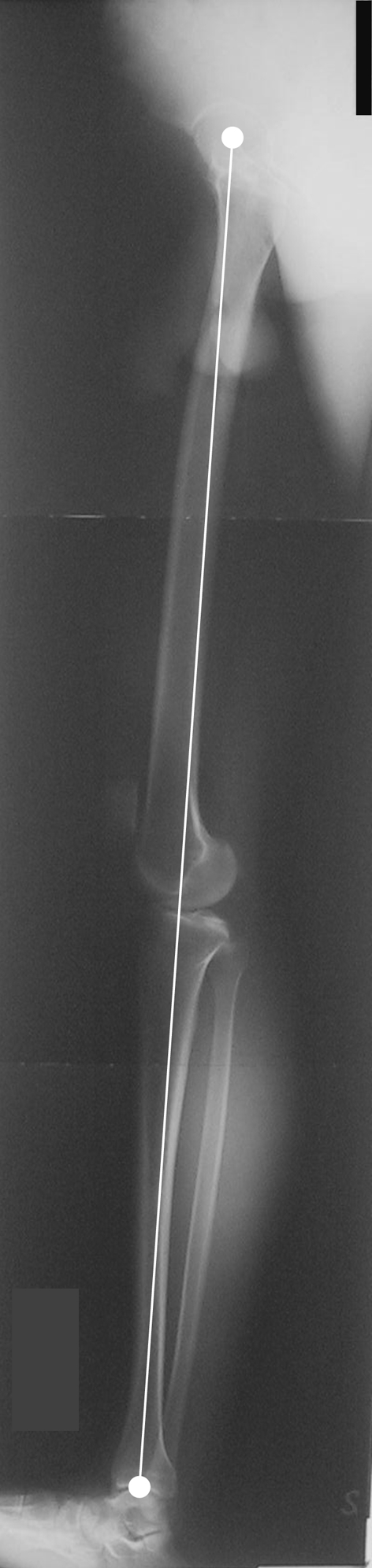
A lateral radiograph of the lower extremity is shown. The sagittal mechanical axis is the line drawn from the center of the femoral head to the center of the talocrural joint (white line).
Because few parameters have been reported for analysis of sagittal alignment of the lower extremity during weightbearing [11], we defined the following parameters: (1) The sagittal mechanical axis was defined as the line drawn from the center of the femoral head, as detected by a concentric circle template, to the center of the talocrural joint (Fig. 1) [11]. We considered the sagittal mechanical axis the baseline for analysis of sagittal alignment of the lower extremity during weightbearing; (2) With the conventional technique, the targeted femoral axis is usually the direction of the intramedullary guide rod, whereas the targeted tibial axis is usually the direction of the extramedullary guide rod. We therefore defined the CFA as the line through the center of the femoral canal at 10 cm and 20 cm proximal to the distal femoral condyle and the CTA as the line through the anterior edge of tibial cortex at 10 cm and 20 cm distal to the tibial plateau, which is commonly used as the anatomic reference landmark during surgery (Fig. 2A); (3) For the navigation systems, we defined the femoral axis as one of three lines from the center of the femoral head to one of the following three points: (a) point of insertion of the intramedullary rod, the CFA was used to determine the direction of the intramedullary rod (navigation femoral axis 1 [NFA1]), (b) the center of the anteroposterior direction of the femoral condyle (NFA2), and (c) the most distal point of the femoral condyle (NFA3) (Fig. 2B). If the most distal points of the medial and lateral femoral condyles were not same, the midpoint between the most distal points of the medial and lateral femoral condyles was used; and (4) The targeted tibial axis with the navigation systems (navigation tibial axis [NTA]) is defined as the line from the center of the talocrural joint to the center of the tibial plateau in an anteroposterior direction. The center of the tibial plateau in the sagittal plane is defined as the midpoint of the line vertical to the NTA and 10 mm distal to the tibial joint surface, because the usual thickness of the tibial cut and tibial component is approximately 10 mm.
Fig. 2A–B.
(A) The diagrams show the targeted prosthetic alignments for the femoral and tibial components using the (A) conventional technique and (B) navigation systems. CFA = conventional femoral axis; CTA = conventional tibial axis; SMA = sagittal mechanical axis. NFA = navigation femoral axis; NTA = navigation tibial axis.
If the bone cut was perpendicular to these axes, the angle between the femoral and tibial axes represented the intercomponent angle between the femoral and tibial components while standing. We thus defined the intercomponent angle while standing as the angle between the femoral and tibial axes on lateral radiographs of the patient’s lower extremity in one-legged stance.
One experienced surgeon (YM) measured the angles between the sagittal mechanical axis and the six defined axes. If the axis was in flexion to the sagittal mechanical axis, degrees were assigned positive values, whereas if the axis was in extension to the sagittal mechanical axis, degrees were assigned negative values. If the alignment between the femoral and tibial components was in flexion, the intercomponent angle was assigned positive values, whereas if it was in extension, the intercomponent angle was assigned negative values. All parameters on radiographs were measured using computer software (Quick Grain Standard; Inotech, Hiroshima, Japan) and calculated to two decimal places. Interobserver and intraobserver variability were assessed for each measurement using a subset of 10 cases, and 95% confidence limits (CLs) were defined (ie, mean ± 2 standard deviations). Intraobserver analysis indicated mean differences of 0.11 to 0.42° in each parameter. Interobserver analysis indicated mean differences of 0.16 to 0.44° in each parameter (Table 1).
Table 1.
Interobserver and intraobserver difference in each parameter
| Axes of sagittal plane | Interobserver difference (degrees) | Intraobserver difference (degrees) | ||||
|---|---|---|---|---|---|---|
| Mean | 95% CLs | Mean | 95% CLs | |||
| lower | upper | lower | upper | |||
| Femoral component | ||||||
| CFA | 0.44 | −0.23 | 1.11 | 0.28 | −0.06 | 0.62 |
| NFA 1 | 0.38 | −0.25 | 1.02 | 0.42 | −1.57 | 2.40 |
| NFA 2 | 0.16 | −0.02 | 0.34 | 0.11 | −0.18 | 0.39 |
| NFA 3 | 0.21 | −0.02 | 0.43 | 0.12 | −0.10 | 0.35 |
| Tibial component | ||||||
| CTA | 0.32 | −0.26 | 0.89 | 0.17 | −0.06 | 0.39 |
| NTA | 0.35 | −0.03 | 0.74 | 0.11 | −0.10 | 0.32 |
CLs = confidence limits.
Differences between the femoral axes (CFA, NFA 1, NFA2, NFA3) and between the intercomponent angles (CFA-CTA, NFA1-NTA, NFA2-NTA, NFA3-NTA) were determined using analysis of variance and Fisher’s post hoc test. Difference between the tibial axes (CTA and NTA) was determined using the paired t test. Computer software (StatView®5.0; Abacus Concepts, Berkeley, CA) was used for analysis.
Results
Femoral sagittal alignment targeted by two navigation approaches to establish reference frames (NFA2 [p = 0.01] and NFA3 [p = 0.0007]) were more flexed than femoral sagittal alignment targeted by one navigation approach (NFA1) (Table 2). Thus, the different reference points on the distal femur for the navigation systems resulted in different targeted sagittal axes for the femoral component. However, femoral sagittal alignment targeted by conventional TKA instruments was similar to femoral sagittal alignment targeted by three navigation approaches to establish reference frames. The tibial sagittal alignment targeted by a navigation approach (NTA) was more flexed than tibial sagittal alignment targeted by conventional TKA instruments (CTA) (p < 0.0001) (Table 2). Therefore, the targeted sagittal axes for the tibial component with the conventional technique and navigation systems were different.
Table 2.
Femoral and tibial axes to determine reference frames
| Axes of sagittal plane | Alignment to SMA (°)* | p Value | |
|---|---|---|---|
| Mean ± SD | Range | ||
| Femoral component | |||
| CFA | 0.45 ± 2.28 | −3.04 to 4.56 | |
| NFA1 | −0.70 ± 2.12 | −3.86 to 3.53 | |
| NFA2 | 1.07 ± 2.05 | −2.22 to 5.47 | 0.0102† |
| NFA3 | 1.67 ± 2.05 | −1.22 to 5.71 | 0.0007† |
| Tibial component | |||
| CTA | −1.63 ± 2.83 | −4.72 to 6.87 | |
| NTA | 1.84 ± 2.77 | −2.15 to 9.77 | < 0.0001‡ |
*If the axis was in flexion to SMA, degrees were assigned positive values, whereas if the axis was in extension, degrees were assigned negative values; †compared with NFA1 using analysis of variance; ‡compared with CTA using paired t test; SMA = sagittal mechanical axis; SD = standard deviation; CFA = conventional femoral axis, NFA = navigation femoral axis; CTA = conventional tibial axis, NTA = navigation tibial axis.
Navigation systems placed the mean intercomponent angle in approximately 2° to 5° greater extension than the conventional technique (Table 3). Intercomponent angles by two navigation approaches (NFA2-NTA [p = 0.007] and NFA3-NTA [p = 0.002]) were more extended than the intercomponent angle by conventional TKA instruments (CFA-CTA).
Table 3.
Intercomponent anglea
| Conventional technique CFA - CTA |
Navigation approaches | ||
|---|---|---|---|
| NFA 1 - NTA | NFA 2 - NTA | NFA 3 - NTA | |
| −1.19 +/- 4.65 | 1.13 +/- 4.67 | 2.91 +/- 4.59* | 3.51 +/- 4.60* |
aIf the alignment between femoral and tibial component was in flexion, degrees were assigned positive values, whereas if the alignment was in extension, degrees were assigned negative values; *Statistical significance was observed compared with conventional technique with ANOVA (p < 0.01); CFA = conventional femoral axis; CTA = conventional tibial axis; NFA = navigation femoral axis; NTA = navigational tibial axis; SMA = sagittal mechanical axis.
Discussion
Navigation systems have been developed to provide more reliable alignment and their use is becoming more widespread. Previous studies suggest navigation systems for TKA improve mean component alignment by only a few degrees, if at all but reduce the number of outliers of femoral and tibial component alignment compared with conventional techniques [3, 7, 10, 14, 15]. However, the methods used to decide sagittal prosthetic alignment using conventional techniques and navigation systems are conceptually different. Thus, sagittal alignments intended with conventional techniques and navigation systems might differ. To our knowledge, there is no information on this issue. If the intended sagittal alignments between the conventional technique and navigation systems differ, postoperative sagittal alignments between these techniques inherently differ. Therefore, it is important to analyze the sagittal alignments intended with conventional techniques and navigation systems. We thus compared the axes for chosen sagittal prosthetic alignments of TKA with the conventional technique and various navigation approaches to establish reference frames.
There are some limitations to this study. First, the subjects were healthy Japanese men, and results of this study therefore may not be directly applicable to nonJapanese subjects or elderly women, who are the main candidates for TKA. Elderly women have shorter and more anteriorly bowed femurs [5]. In such patients, the differences in the femoral axes between the conventional technique and navigation systems might be even more marked than those we observed. Second, the evaluation performed in our study was two-dimensional and not three-dimensional. However, it is difficult to perform CT while the patient is standing. The effective radiation dose is approximately 10 times as large as that required for radiographs [5]. Owing to potential radiation hazards to the gonads, our method using radiographs is more desirable than using CT, because our subjects were young volunteers. Third, although the relationship between postoperative implant alignment in the coronal plane and long-term clinical results has been reported [6, 16, 17], there have been only a few reports on the relationship between the implant alignment in the sagittal plane and long-term clinical results [2, 4]. To assess implant alignment accurately, it was necessary to obtain coronal and sagittal radiographs of the entire lower extremity on weightbearing with the knee in full extension. However, it was technically difficult to obtain a sagittal radiograph of the entire lower extremity [14]. This technical difficulty has made it difficult to analyze the relationship between implant alignment in the sagittal plane and long-term clinical results [11]. Even the studies using short film, which was less reliable in assessing implant alignment, revealed an excessive extended angle of the femoral component relative to the tibial component, owing to flexion of the femoral component or/and posterior slope of the tibial component, which led to osteolysis [2, 4], polyethylene wear of the anterior post, [2, 8] or post fracture [2, 8]. Additional studies using more precise methods, such as long films for the entire leg using our method [11] or CT, could determine whether the difference in sagittal alignment affects long-term outcomes. We suspect those outcomes would be implant-specific.
Our data suggest the targeted sagittal alignments using the conventional technique and navigation systems differ within a mean of 2° to 4°. Thus, the postoperative sagittal prosthetic alignment in TKA using the conventional technique and those using navigation systems theoretically produce different values. The difference was small, but clinical reports suggest navigation systems improve alignment by only a few degrees in mean alignment [3, 7, 10, 14, 15]. Simple comparison of mean postoperative sagittal prosthetic alignment between the conventional technique and navigation systems might not be appropriate for evaluation of these methods, because intended sagittal alignments might differ.
Extension between the femoral and tibial components risks anterior tibial post impingement with posterior-stabilized prostheses, which may lead to excessive polyethylene wear of the anterior part of the tibial post and post fracture [2, 8]. Extension of 10° between components increased the odds ratio of osteolysis by 1.4 times, even with cruciate-retaining prostheses that do not have a tibial post [4]. Some have recommended 5° to 7° of posterior tibial slope toward the tibial axis in the sagittal plane for a better postoperative flexion angle [9]. If 7° of posterior tibial slope toward the tibial axis in the sagittal plane is planned with navigation systems, extended alignment between the femoral and tibial components will be more prominent, and 30% to 50% of our cases with the navigation systems resulted in greater than 10° extended alignment between the components (30% with NFA1 and NTA, 45% with NFA2 and NTA, and 50% with NFA3 and NTA). This might lead to excessive polyethylene wear and osteolysis. For the intercomponent angle, the insertion point of the intramedullary rod (NFA1) was preferred to the reference point on the distal femur for the navigation systems, and there should be no excessive posterior tibial slope.
The most important problem with use of navigation systems in TKA is that optimal prosthetic alignment on the sagittal plane is not uniform and might differ from patient to patient depending on their anatomy, activities, and other considerations including implant design. The reliability of navigation systems in the sagittal plane is reportedly less than that in the coronal plane [3, 7, 10, 14, 15]. Matziolis et al. [10], in a prospective, randomized study of conventional technique and a navigation system for TKA, evaluated postoperative implant alignment using a precise three-dimensional technique. In the coronal plane, the mean deviation was 1.0° ± 0.6° for the femoral component and 1.4° ± 0.9° for the tibial component. In the sagittal plane, however, it was 3.4° ± 2.7° for the femoral component and 2.1° ± 1.3° for the tibial component. They concluded the navigation system was more reliable for coronal alignment, but not sagittal alignment, compared with the conventional technique. They also mentioned it was unclear whether sagittal alignment corresponding to the mechanical or anatomic axis should be sought.
Our data suggest the targeted sagittal prosthetic alignments of TKA with the conventional technique and various navigation systems differed by 2° to 4°. Use of navigation systems resulted in 1° to 4° hyperextension between the femoral and tibial components. Surgeons and technicians using navigation systems for TKA should be aware of the existence of this difference in the sagittal plane.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47. [PubMed]
- 2.Callaghan JJ, O’Rourke MR, Goetz DD, Schmalzried TP, Campbell PA, Johnston RC. Tibial post impingement in posterior-stabilized total knee arthroplasty. Clin Orthop Relat Res. 2002;404:83–88. [DOI] [PubMed]
- 3.Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM. Computer-assisted total knee replacement: a controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT Protocol). J Bone Joint Surg Br. 2004;86:818–823. [DOI] [PubMed]
- 4.Collier MB, Engh CA Jr, McAuley JP, Ginn SD, Engh GA. Osteolysis after total knee arthroplasty: influence of tibial baseplate surface finish and sterilization of polyethylene insert. Findings at five to ten years postoperatively. J Bone Joint Surg Am. 2005;87:2702–2708. [DOI] [PubMed]
- 5.Egol KA, Chang EY, Cvitkovic J, Kummer FJ, Koval KJ. Mismatch of current intramedullary nails with the anterior bow of the femur. J Orthop Trauma. 2004;18:410–415. [DOI] [PubMed]
- 6.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709–714. [DOI] [PubMed]
- 7.Kim YH, Kim JS, Yoon SH. Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. J Bone Joint Surg Br. 2007;89:471–476. [DOI] [PubMed]
- 8.Li G, Papannagari R, Most E, Park SE, Johnson T, Tanamal L, Rubash HE. Anterior tibial post impingement in a posterior stabilized total knee arthroplasty. J Orthop Res. 2005;23:536–541. [DOI] [PubMed]
- 9.Massin P, Gournay A. Optimization of the posterior condylar offset, tibial slope, and condylar roll-back in total knee arthroplasty. J Arthroplasty. 2006;21:889–896. [DOI] [PubMed]
- 10.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty: three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236–243. [DOI] [PubMed]
- 11.Minoda Y, Kobayashi A, Iwaki H, Sugama R, Iwakiri K, Kadoya Y, Ohashi H, Takaoka K. Sagittal alignment of the lower extremity while standing in Japanese male. Arch Orthop Trauma Surg. 2008;128:435–442. [DOI] [PubMed]
- 12.Oswald MH, Jakob RP, Schneider E, Hoogewoud HM. Radiological analysis of normal axial alignment of femur and tibia in view of total knee arthroplasty. J Arthroplasty. 1993;8:419–426. [DOI] [PubMed]
- 13.Sato T, Koga Y, Omori G. Three-dimensional lower extremity alignment assessment system: application to evaluation of component position after total knee arthroplasty. J Arthroplasty. 2004;19:620–628. [DOI] [PubMed]
- 14.Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A. Positioning of total knee arthroplasty with and without navigation support: a prospective, randomised study. J Bone Joint Surg Br. 2003;85:830–835. [PubMed]
- 15.Stulberg SD. How accurate is current TKR instrumentation? Clin Orthop Relat Res. 2003;416:177–184. [DOI] [PubMed]
- 16.Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br. 1985;67:551–556. [DOI] [PubMed]
- 17.Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res. 1994;299:31–43. [PubMed]