Abstract
There have been technologic advances in the methods for repairing torn rotator cuffs. We compared the clinical and structural outcomes of three different forms of rotator cuff repair with up to 24 months’ followup. We wished to assess how surgical technique affected clinical outcomes and see how these correlated to repair integrity. Three cohorts of patients had repair of a symptomatic rotator cuff tear using (1) an open technique (n = 49); (2) arthroscopic knotted (n = 53); or (3) arthroscopic knotless (n = 57) by one surgeon. Standardized patient- and examiner-determined outcomes were obtained preoperatively and at 6 weeks, 3 and 6 months, and 2 years postoperatively. Ultrasound studies were performed with a validated protocol at 6 months and 2 years postsurgery. Clinical outcomes were similar with the exception that the arthroscopic groups had, on average, 20% better American Shoulder and Elbow Surgeons scores than the open group at 6 months and 2 years. Retear correlated with tear size and operation time and occurred more frequently after open repair (39%) than after arthroscopic knotted (25%) and arthroscopic knotless (16%) repair. An intact cuff on ultrasound corresponded to better results for supraspinatus strength, patient outcomes, and rotator cuff functional ability.
Level of Evidence: Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Rotator cuff tears are a common cause of shoulder pain and dysfunction in the adult shoulder. Surgical repair aims to reestablish the normal anatomic relationship of the rotator cuff tendons while restoring the shoulder to a pain-free state with normal motion, strength, and function. Good functional results have been observed using open [8, 12] and arthroscopic techniques [27, 38]. There are fewer studies [19, 24, 33, 37] comparing the results of open and arthroscopic repairs.
Reported rotator cuff repair retear rates range between 15% and 90% [3, 21, 22, 31] using open or arthroscopic methods. Two studies showed rotator cuff integrity is important to rotator cuff function [20, 36]. Proposed benefits of arthroscopic techniques include less postoperative pain, decreased risk of deltoid adhesions, improved observation and mobilization of large tears, and possible accelerated recovery and rehabilitation [14, 35]. Potential disadvantages of arthroscopic repair include longer operative time and less secure repairs with higher retear rates [39].
We hypothesized that arthroscopic techniques would produce better clinical and structural outcomes. We prospectively assessed the clinical outcomes of open repair versus knotted arthroscopic repair versus arthroscopic knotless repair and correlated these results with the integrity of the cuff as determined by ultrasonographic evaluation. The primary research question was to determine how the technique affected clinical outcomes as assessed by the American Shoulder and Elbow Score (ASES) for shoulder function at 6 months and 2 years postsurgery. The second question assessed how repair technique influenced postoperative pain, cuff strength, and range of motion (ROM). The final question aimed to correlate clinical outcomes with repair integrity at 6 months and 2 years postsurgery.
Materials and Methods
Ethical approval for this retrospective study of prospectively collected data was granted by the South Eastern Sydney and Illawara Ethics Committee. Between February 2003 and March 2006, 312 consecutive patients with symptomatic rotator cuff tears underwent rotator cuff repair by one surgeon (GACM) using suture anchors to reattach the torn tendon(s) to bone. Patients with glenohumeral arthritis, fracture, previous shoulder surgery, osteonecrosis, and partial-thickness rotator cuff tears and those who were unable or unwilling to undergo ultrasound examination at 6 months and 2 years postoperatively were excluded. Patients who underwent rotator cuff repair within the first 6 weeks of the surgeon changing to new arthroscopic techniques were excluded to take into consideration the initial learning curve associated with the new technique. Of the 312 consecutive patients undergoing rotator cuff repair, 153 were excluded as per the exclusion criteria, including nine with glenohumeral arthritis (defined radiographically and at arthroscopy), seven with shoulder fractures, 18 with previous shoulder surgery, 35 with isolated partial-thickness tears, 62 who were unable or unwilling to undergo ultrasound examination at 6 months, and 22 who fell into the 6-week period identified before the study as the arthroscopic repair learning curve period, leaving 159 patients with 6 months’ clinical followup. All 159 patients underwent ultrasound examination 6 months postsurgery. At 2 years postoperatively, an additional 76 (48%) patients were excluded because they were unable to undergo ultrasound examination, leaving 87 (55%) patients for clinical and structural evaluations at 2 years of followup.
From February 2003 to March 2004, the surgeon performed open rotator cuff surgery using metallic suture anchors (Mitek RC Quickanchor™; Depuy Mitek Inc, Raynham, MA) (open group, n [6 months] = 49, n [2 years] = 20). Between December 2003 and August 2005, the surgeon changed to arthroscopic repair of rotator cuff tears and patients underwent arthroscopic rotator cuff repair with a screw-in metallic suture anchor (Mitek Fastin®; Depuy Mitek Inc) (arthroscopic knotted group, n [6 months] = 53, n [2 years] = 29). During the transition period from open to arthroscopic repair (December 2003 to March 2004), the decision to perform arthroscopic repair was based on tear size, with large and massive tears repaired using the mini-open technique. In August 2005, the surgeon changed to an arthroscopic knotless technique and patients underwent rotator cuff repair using a metallic knotless suture anchor (ArthroCare Opus Magnum; ArthroCare Corp, Sydney, Australia) (arthroscopic knotless group, n [6 months] = 57, n [2 years] = 38).
At all points up to and including the 6-month review, there were 21 men and 28 women in the open group with a mean age of 58 years (range, 28–87 years), 24 men and 29 women in the arthroscopic knotted group with a mean age of 64 years (range, 40–90 years), and 28 men and 29 women in the arthroscopic knotless group with a mean age of 59 years (range, 34–86 years) (Table 1). The mean times from initial injury to surgical repair were 13 months (range, 0.5–81 months), 7 months (range, 0.8–39 months), and 6 months (range, 0.2–31 months) in the open, arthroscopic knotted, and arthroscopic knotless groups, respectively. The mean time from initial injury to surgical repair was longer (p < 0.05) in the open than in the two arthroscopic groups.
Table 1.
Demographics of patients in the groups
| Variable | Open | Knotted arthroscopic | Knotless arthroscopic | Open versus arthroscopic knotted* | Open versus arthroscopic knotless* | Arthroscopic knotted versus arthroscopic knotless* |
|---|---|---|---|---|---|---|
| Number of patients | ||||||
| 6 months | 49 | 52 | 57 | NS | NS | NS |
| 2 years | 20 | 29 | 38 | |||
| Male:female | ||||||
| 6 months | 21:28 | 24:29 | 28:29 | NS | NS | NS |
| 2 years | 10:10 | 10:19 | 20:18 | |||
| Age at surgery (years)† | ||||||
| 6 months | 58 (28–87) | 64 (40–90) | 59 (34–86) | p < 0.01 | NS | p < 0.05 |
| 2 years | 60 (48–73) | 63 (79) | 61 (34–86) | |||
| Time from initial injury to repair (months)† | ||||||
| 6 months | 13 (0.5–81) | 7.0 (0.8–39) | 6.0 (0.2–31) | p < 0.05 | NS | NS |
| 2 years | 15 (0.7–81) | 7.2 (1.0–39) | 6.6 (0.5–31) | |||
| Affected shoulder | ||||||
| Right | ||||||
| 6 months | 28 | 38 | 45 | |||
| 2 years | 9 | 19 | 30 | |||
| Left | ||||||
| 6 months | 21 | 15 | 12 | |||
| 2 years | 11 | 10 | 8 | |||
| Dominant arm | ||||||
| 6 months | 32/49 | 40/53 | 43/57 | NS | NS | NS |
| 2 years | 12/20 | 19/29 | 29/38 | |||
| Tear size (cm2)† | ||||||
| 6 months | 4.1 (0.5–14) | 3.9 (1–13.5) | 3.7 (1–16.5) | NS | NS | NS |
| 2 years | 4.3 (1–14) | 3.9 (1–13.5) | 3.6 (1–15.75) | NS | NS | NS |
| Number of anchors used‡ | ||||||
| 6 months | 4.0 ± 0.1 (2–8) | 2.1 ± 0.7 (1–4) | 2.5 ± 0.1 (1–5) | p < 0.001 | p < 0.001 | p < 0.01 |
| 2 years | 4.4 ± 0.1 (2–8) | 2.0 ± 0.7 (1–4) | 2.5 ± 0.2 (1–5) | |||
| Operation time (minutes)† | ||||||
| 6 months | 60 (35–100) | 55 (30–90) | 41 (20–60) | NS | p < 0.001 | p < 0.01 |
| 2 years | 61 (35–100) | 54 (30–85) | 40 (20–60) | |||
| Number of retears requiring surgery | ||||||
| 6 months | 3 | 4 | 5 | NS | NS | NS |
| 2 years | 4 | 5 | 7 | NS | NS | NS |
* Comparisons between groups using Mann-Whitney rank sum tests; †values expressed as means, with ranges in parentheses; ‡values expressed as mean ± standard error of the mean, with range in parentheses; NS = no significance.
At the 2-year assessment, there were 10 men and 10 women in the open group with a mean age of 60 years (range, 48–73 years), 10 men and 19 women in the arthroscopic knotted group with a mean age of 63 years (range, 40–79 years), and 28 men and 29 women in the arthroscopic knotless group with a mean age of 61 years (range, 34–86 years) (Table 1). The mean times from initial injury to surgical repair were 15 months (range, 0.7–81 months), 7.2 months (range, 1.0–39 months), and 6.6 months (range, 0.5–31 months) in the open, arthroscopic knotted, and arthroscopic knotless groups, respectively. The mean time from initial injury to surgical repair was longer (p < 0.05) in the open than the two arthroscopic groups.
All procedures were performed under interscalene block with the patient in the upright beach chair position as day case surgery. All patients were given a preoperative dose of the same antibiotic (1 g cefazolin intravenously) and one additional dose of this antibiotic 4 hours after completion of the procedure. All patients underwent initial arthroscopic assessment through a standard three-portal technique. A posterior portal was established for initial inspection of the glenohumeral joint. An anterior portal through the rotator interval was established as a working portal for intraarticular débridement. Another lateral accessory portal was created for inspection and decompression of the subacromial space plus rotator cuff repair in the arthroscopic groups. Operative time was defined as the time in minutes from first skin incision until wound closure.
Our surgical technique for open rotator cuff repair was described previously [6]. Briefly, it included partial splitting of the deltoid in line with its fibers, detachment and later reattachment of the coracoacromial ligament at the level of the anterior acromion, and anterior acromioplasty and bursectomy. Appropriate soft tissue releases (subacromial and extraarticular adhesion, coracohumeral ligament, rotator cuff interval) were performed before rotator cuff repair.
The suture anchors (Mitek RC Quickanchor™) were impacted directly into the bone of the proximal humerus without predrilling of the bone. When possible (ie, when there was enough excursion of the torn tendon), a two-row anchor technique was used for fixation. The suture material used in the above anchors was either Number 2 braided, nonabsorbable polyester suture or Number 2 absorbable Panacryl™ (Ethicon, Inc, Somerville, NJ) suture. The tendons were grasped with the suture material by a horizontal mattress stitch configuration.
Arthroscopic repair was performed using the standard three-portal technique as described by Gartsman and Hammerman [13]. After arthroscopic acromioplasty, the rotator cuff tear edge was débrided and the landing site at the greater tuberosity was gently débrided and smoothed with an arthroscopic burr. Mobilization techniques were performed to permit anatomic repair of the tendon to the greater tuberosity and reduce tension on the repair. After the mobilization techniques were performed, all tears, including those with asymmetric retraction, could be mobilized to the lateral-most aspect of the greater tuberosity with the arm at 0° abduction. All patients underwent direct repair of the tendon to the bone without medialization of the repair site or a margin convergence type of repair.
For arthroscopic knotted repair, the rotator cuff was repaired to bone in a single row using two simple sutures per anchor. The 5-mm metal double suture loaded corkscrew anchors (Mitek Fastin®) were inserted through the lateral accessory portal anteriorly to posteriorly in a single row in the rotator cuff footprint.
For arthroscopic knotless repair, the rotator cuff was repaired to bone in a single row using one inverted mattress suture per anchor. The torn rotator cuff was grasped with the Opus SmartStitch® Suture Device (ArthroCare Corp), which delivers a Number 2 polyester mattress suture into the cuff through the lateral portal. A hole was punched at the desired position on the landing site through the lateral portal. Both limbs of the suture were passed through the Opus Magnum Knotless Implant; the implant then was inserted into the prepared bone hole and deployed in the bone. The suture then was wound through the anchor reducing the tendon to the bone before locking the suture in the anchor.
Mean preoperative tear sizes were not different among the 6-month cohorts: 4.1 cm2 (range, 0.5–14 cm2), 3.9 cm2 (range, 1–13.5 cm2), and 3.7 cm2 (range, 1–16.5 cm2) in the open, knotted, and knotless groups, respectively (Tables 1, 2). The open group used double-row fixation techniques in 45 of 49 (92%) cases, with the remaining cases using a standard single-row fixation. The open group had repair with 3 ± 0.4 absorbable sutures in 14 patients and 4 ± 0.6 nonabsorbable sutures in 35 patients. Mean preoperative tear sizes were not different among the groups of the 2-year followup cohort: 4.3 cm2 (range, 1.0–14 cm2), 3.9 cm2 (range, 1–13.5 cm2), and 3.6 cm2 (range, 1–15.75 cm2) in the open, knotted, and knotless groups, respectively (Tables 1, 2). The open group had double-row fixation techniques in 19 of 20 (92%) cases, with the remaining case having a standard single-row fixation. The open group had repair with 3 ± 0.4 absorbable sutures in three patients and 4 ± 0.6 nonabsorbable sutures in 17 patients.
Table 2.
Individual preoperative tear sizes and retear rates
| Tear size (cm2) | Open | Knotted | Knotless |
|---|---|---|---|
| 6 months | n = 49 | n = 53 | n = 57 |
| Small (< 1) | 5 (2) | 10 (0) | 9 (1) |
| Medium (1–3) | 24 (5) | 22 (4) | 29 (3) |
| Large (3–5) | 8 (3) | 9 (2) | 5 (1) |
| Massive (>5) | 13 (9) | 13 (7) | 13 (4) |
| Retear rate | 19/49 (39%) | 13/52 (25%) | 9/57 (16%) |
| 2 years | n = 20 | n = 29 | n = 38 |
| Small (< 1) | 3 (1) | 7 (0) | 9 (1) |
| Medium (1–3) | 8 (1) | 12 (5) | 16 (1) |
| Large (3–5) | 2 (1) | 3 (2) | 4 (1) |
| Massive (>5) | 7 (5) | 6 (3) | 8 (4) |
| Retear rate | 8/20 (40%) | 10/29 (34%) | 7/38 (18%) |
Figures in parentheses denote the number of retorn cuffs in each tear size category.
A greater number of anchors (p < 0.001) were used for fixation in the open group (mean, 4.0) than in the knotted group (mean, 2.1) and the knotless group (mean, 2.5) in the 6-month and 2-year cohorts, consistent with a two-row technique in the open surgery group. There also was a greater number of anchors (p < 0.01) used in the knotless group than in the knotted group at 6 months and 2 years.
No difference in operation time was noted between open (mean, 60 minutes) and arthroscopic knotted cuff repairs (mean, 55 minutes). Arthroscopic knotless repair (mean, 41 minutes) was faster than open cuff repair (p < 0.001) and arthroscopic knotted repair (p < 0.01).
After surgery, patients initially wore either a shoulder sling (open group) or an ultrasling (sling with a small abduction pillow) (arthroscopic groups) for 6 weeks. They began a gradually progressive home rehabilitation program as described by Hayes et al. [16]. They began immediate postoperative ROM pendulum exercises. After the first postoperative visit at Day 8, the patients began passive forward flexion, external rotation, and abduction ROM exercises. Active ROM and simple isometric strengthening exercises were initiated at the 6-week postoperative visit. Active overhead activities and lifting 5 kg or more usually began 3 months postoperatively.
Standardized patient-determined [16] and examiner-determined outcomes [16, 18] were obtained preoperatively and at 6 weeks, 3 months, 6 months, and 2 years postoperatively. This included the Shoulder Service Questionnaire, which was based on the Shoulder Rating Questionnaire (L’Insalata et al. [25]) for assessment of functional capacity and physical symptoms. The information gathered allowed calculation of preoperative and postoperative ASES scores. The ASES score is based on activities of daily living scale and pain score and has a maximum of 100 points and was used as the primary outcome measure.
Intraoperative data were collected on standardized forms. The cross-sectional size of the rotator cuff tear was estimated and recorded on a diagram as described previously [4]. The number and type of suture anchors used in the rotator cuff repair, and any additional procedures, were recorded.
Clinical testing was performed by a blinded independent observer (BB, JM, XW) and included visual estimation of ROM for forward flexion, abduction, external rotation, and internal rotation as described by Hayes et al. [17]. Quantitative strength measurements of the shoulder in four orientations were measured using a HFG-45 Hand-Held Force Gauge (Transducer Techniques, Temecula, CA) as described by Hayes et al. [18]. These measurements were used to calculate the rotator cuff functional index as described by Osbahr and Murrell [29].
After the 6-month and 2-year postoperative evaluations, patients in each group had a standardized shoulder ultrasound study as described by Bryant et al. [4]. Ultrasound accuracy has been validated at our institution for evaluation of cuff tear size preoperatively [4]. Ultrasonography was performed on either an Acuson 128XP™ or Sequoia™ machine (Acuson Corp, Mountain View, CA) with a 7.5- to 12-MHz linear transducer or a General Electric Logiq® 9 (GE Corp, Fairfield, CT) with a 12-MHz linear transducer. Studies were performed by six experienced musculoskeletal sonographers following the standardized protocol. The ultrasonographic examination was performed as described by Teefey et al. [36]. Static and dynamic imaging were performed. First, the biceps tendon was examined in the short axis from the level of the acromion inferiorly to the point where the tendon merged with the biceps muscle. The biceps tendon also was examined in the long axis. From the short axis biceps position, the subscapularis tendon was examined by externally rotating the arm. Images of the supraspinatus tendon were made with the shoulder extended, the elbow flexed, and the hand fully supinated. This position allowed maximum exposure of the supraspinatus tendon from under the acromion. The transducer orientation was maintained parallel to the tendon to observe the fibers in a longitudinal plane, and it was moved anteriorly and posteriorly and proximally and distally to observe the entire supraspinatus and infraspinatus tendons. The findings were reported on a form specifically designed to represent in two dimensions any defect in the rotator cuff [4].
Results are reported as mean ± standard error of the mean. To answer the first and second questions, comparisons between groups were made with two-way paired Student’s t tests for parametric data, Mann-Whitney U tests for nonparametric data, the chi square test, and Kruskal-Wallis one-way analysis of variance on ranks. Correlations relating to the first and second questions were calculated using Pearson’s coefficient and multiple linear regression analysis. Analysis for the third question used Pearson’s coefficient and multiple logistic and linear regression calculations. Dunn’s test was applied to the regression analysis, which is a method that corrects for multiple comparisons, using the Bonferroni adjustment. To determine if the learning curve of arthroscopic repair had an effect on retear rate, the case number (where 1 was the first arthroscopic rotator cuff repair performed by the surgeon, 2 the second, and so forth) was included in the multiple regression analysis. All data were analyzed using SigmaStat®, Version 3.1 (Systat Software Inc, Richmond, CA).
Results
There were similar numbers of patients (10%) in each group (n = 4 in open, n = 5 in arthroscopic knotted, and n = 7 in arthroscopic knotless) requiring revision surgery during the followup period. All of these patients, except one in the knotted group in which an anchor pulled out 5 months postsurgery, required surgery as a result of traumatic events.
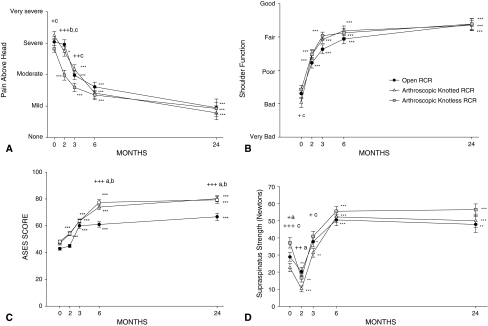
Overall shoulder function improved (p < 0.001) at 6 weeks, 3 months, 6 months, and 2 years postsurgery compared with preoperative levels in all groups (Fig. 1). There were improvements in the mean ASES score between the preoperative and 6-week visits in the arthroscopic groups (p < 0.001) and at the 3- and 6-month and 2-year followups in all groups (p < 0.001). The mean ASES score was lower (p < 0.001) in the open group compared with the arthroscopic groups. A two-way analysis of variance using an open surgical technique produced a lower (p < 0.001) ASES score compared with both arthroscopic techniques at 6 months and 2 years postsurgery. Multiple regression analyses revealed better ASES scores in the arthroscopic groups correlated with supraspinatus strength (p < 0.001) and technique used (p < 0.001). Stiffness, rotator cuff functional index, operative time, preoperative tear size, retear size or rate, and surgical learning curve were found to have no correlation to ASES scores.
Fig. 1A–D.
The graphs show comparisons among open, arthroscopic knotted, and arthroscopic knotless rotator cuff repairs (RCR) for (A) pain severity at rest, (B) overall shoulder function, (C) ASES score, and (D) supraspinatus strength. The data are displayed as mean ± standard error of the mean (n = 49 for open group, n = 53 for knotted arthroscopic group, and n = 57 for knotless arthroscopic group up to 6 months; n = 20 for open group, n = 27 for knotted arthroscopic group, and n = 38 for knotless arthroscopic group at 24 months). * = p < 0.05, ** = p < 0.01, *** = p < 0.001 compared with preoperative values using Mann-Whitney rank sum test. + = p < 0.05, ++ = p < 0.01, +++ = p < 0.001 comparing a = open versus arthroscopic knotted, b = open versus arthroscopic knotless, and c = knotted versus knotless arthroscopic using Kruskal-Wallis one-way analysis of variance on ranks and corrected for multiple comparison using Dunn’s method.
All pain scores improved (p < 0.001) between the preoperative visit and 6-month and 2-year followups in all groups (Table 3). Pain severity was less in the arthroscopic knotless group at 6 weeks compared with the open and knotted groups (p < 0.001) and at 3 months compared with the knotted group (p < 0.01). The arthroscopic groups had less pain at night (p < 0.05) than the open group at 6 months; however, no difference was detected at 2 years postsurgery. Patient-perceived shoulder stiffness improved between the preoperative visit and 6 months postsurgery in the open (p < 0.05) and arthroscopic groups (p < 0.001), which was maintained at the 2-year followup. Patient-perceived stiffness was considerably greater (p < 0.05) in the open group compared with the arthroscopic knotless cohort at 2 years. No other differences in stiffness were noted among groups.
Table 3.
Comparison of outcome scores measured preoperatively and at 6-month followup
| Outcome | Open | Arthroscopic knotted | Arthroscopic knotless | Open versus arthroscopic knotted* | Open versus arthroscopic knotless* | Arthroscopic knotted versus arthroscopic knotless* |
|---|---|---|---|---|---|---|
| Pain severity | ||||||
| At rest (0–4) | ||||||
| Preoperative | 2.4 ± 0.2 | 2.2 ± 0.1 | 1.7 ± 0.2 | NS | p < 0.01 | p < 0.05 |
| 6 months | 1.0 ± 0.1§ | 1.0 ± 0.1§ | 0.7 ± 0.1§ | NS | NS | NS |
| 2 years | 0.5 ± 0.1§ | 0.6 ± 0.1§ | 0.6 ± 0.1§ | NS | NS | NS |
| At night (0–4) | ||||||
| Preoperative | 2.5 ± 0.2 | 2.3 ± 0.2 | 2.2 ± 0.1 | NS | NS | NS |
| 6 months | 1.4 ± 0.1§ | 1.0 ± 0.1§ | 0.8 ± 0.1§ | p < 0.05 | p < 0.001 | NS |
| 2 years | 0.9 ± 0.2§ | 0.9 ± 0.1§ | 0.9 ± 0.1§ | NS | NS | NS |
| Stiffness (0–4) | ||||||
| Preoperative | 1.9 ± 0.2 | 2.1 ± 1 | 1.9 ± 0.2 | NS | NS | NS |
| 6 months | 1.3 ± 0.2† | 1.0 ± 1§ | 1.2 ± 0.2‡ | NS | NS | NS |
| 2 years | 1.1 ± 0.3† | 0.9 ± 0.7§ | 0.7 ± 0.2§ | NS | p < 0.05 | NS |
| Overall shoulder function (1–5) | ||||||
| Preoperative | 2.3 ± 0.1 | 2.0 ± 0.2 | 2.4 ± 0.1 | NS | NS | p < 0.05 |
| 6 months | 3.9 ± 0.1§ | 4.2 ± 0.1§ | 4.1 ± 0.1§ | NS | NS | NS |
| 2 years | 4.4 ± 0.1§ | 4.3 ± 0.1§ | 4.4 ± 0.1§ | NS | NS | NS |
| Rotator cuff functional index | ||||||
| Preoperative | −16 ± 3 | −25 ± 3 | −20 ± 3 | NS | NS | NS |
| 6 months | −1 ± 3§ | 3 ± 3§ | −1 ± 2§ | NS | NS | NS |
| 2 years | −8 ± 4§ | −4 ± 2§ | −3 ± 3§ | NS | NS | NS |
| ASES score (0–100) | ||||||
| Preoperative | 43 ± 1 | 47 ± 1 | 48 ± 1 | NS | p < 0.01 | NS |
| 6 months | 61 ± 2§ | 74 ± 2§ | 78 ± 2§ | p < 0.001 | p < 0.001 | NS |
| 2 years | 67 ± 1§ | 80 ± 2§ | 79 ± 1§ | p < 0.001 | p < 0.001 | NS |
Values are expressed as mean ± standard error of the mean; * comparisons between groups using Kruskal-Wallis one-way analysis of variance on ranks and corrected for multiple comparison using Dunn’s method; †p < 0.05, ‡p < 0.01, §p < 0.001, using Mann-Whitney rank sum test; ASES = American Shoulder and Elbow Surgeons; NS = no significance.
Forward flexion and abduction ROM improved in all groups between the preoperative examination and the 2-year followup (Table 4). No improvements in external rotation ROM were noted at any followup visit in the open repair group. The arthroscopic groups had improved (p < 0.001) external rotation ROM 6 months and 2 years postoperatively compared with the open group. An arthroscopic technique correlated with increased external rotation at 6 months (r = 0.4; p < 0.001). Improvements (p < 0.01) in all planes of shoulder strength measurement were noted between preoperative testing and the 2-year evaluation in all groups, except for internal rotation strength in the arthroscopic knotless repair cohort (Table 4). All groups showed a decrease (p < 0.01) in supraspinatus strength at the 6-week postoperative visit, which then improved (p < 0.001) at all postoperative visits. An arthroscopic knotless technique produced greater (p < 0.05) supraspinatus strength at 2 years compared with both other groups.
Table 4.
Comparison of range of motion and strength preoperatively and at 6 months and 2 years postoperatively
| Range of motion/strength | Open | Arthroscopic knotted | Arthroscopic knotless | Open versus arthroscopic knotted* | Open versus arthroscopic knotless* | Arthroscopic knotted versus arthroscopic knotless* |
|---|---|---|---|---|---|---|
| Range of motion (°) | ||||||
| Forward flexion | ||||||
| Preoperative | 151 ± 4 | 123 ± 7 | 146 ± 5.0 | p < 0.01 | NS | p < 0.05 |
| 6 months | 163 ± 4‡ | 163 ± 4§ | 168 ± 2.5§ | NS | p < 0.05 | NS |
| 2 years | 164 ± 4‡ | 165 ± 4§ | 165 ± 3§ | NS | NS | NS |
| External rotation | ||||||
| Preoperative | 53 ± 3 | 47 ± 2 | 54 ± 2.7 | NS | NS | NS |
| 6 months | 53 ± 2 | 66 ± 3§ | 69 ± 2.5§ | p < 0.001 | p < 0.001 | NS |
| 2 years | 52 ± 2 | 62 ± 2‡ | 68 ± 3§ | p < 0.001 | p < 0.001 | NS |
| Abduction | ||||||
| Preoperative | 135 ± 5 | 112 ± 6 | 133 ± 5.5 | p < 0.05 | NS | p < 0.05 |
| 6 months | 154 ± 4‡ | 159 ± 5§ | 163 ± 3.3§ | NS | p < 0.05 | NS |
| 2 years | 149 ± 5† | 141 ± 5§ | 152 ± 4‡ | NS | NS | p < 0.05 |
| Strength (N) | ||||||
| Supraspinatus | ||||||
| Preoperative | 29 ± 3 | 23 ± 2 | 37 ± 3 | p < 0.05 | NS | p < 0.001 |
| 6 months | 50 ± 3§ | 52 ± 3§ | 56 ± 2.8§ | NS | NS | NS |
| 2 years | 48 ± 3§ | 50 ± 2§ | 57 ± 2§ | NS | p < 0.05 | p < 0.05 |
| External rotation | ||||||
| Preoperative | 39 ± 3 | 32 ± 2 | 46 ± 2.7 | NS | NS | p < 0.01 |
| 6 months | 62 ± 4§ | 60 ± 3§ | 61 ± 2.7§ | NS | NS | NS |
| 2 years | 53 ± 4† | 52 ± 3‡ | 62 ± 3§ | NS | p < 0.05 | p < 0.05 |
| Liftoff | ||||||
| Preoperative | 29 ± 2 | 20 ± 2 | 29 ± 2.6 | p < 0.001 | NS | p < 0.01 |
| 6 months | 45 ± 4‡ | 38 ± 3§ | 40 ± 2.1§ | NS | NS | NS |
| 2 years | 47 ± 4‡ | 49 ± 4§ | 50 ± 2§ | NS | NS | NS |
Values are expressed as mean ± standard error of the mean; * comparisons between groups using Kruskal-Wallis one-way analysis of variance on ranks and corrected for multiple comparison using Dunn’s method; †p < 0.05, ‡p < 0.01, §p < 0.001 using Mann-Whitney rank sum test; NS = no significance.
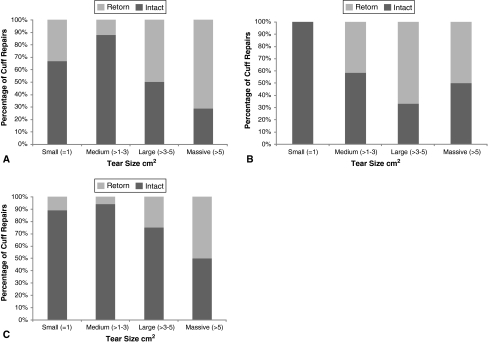
The overall retear rates as detected by ultrasound, including tears that underwent revision surgery, were 26% (41 of the 159 shoulders) at 6 months and 29% (25 of the 87 shoulders) at 2 years. All of the retears were of the supraspinatus tendon. Structural outcomes between 6 months and 2 years showed no major change in the rate of retear compared with the original size of tear (Table 2). At 6 months postsurgery, 70% of tears greater than 5 cm2 fixed using an open technique had a retear compared with 54% in the arthroscopic knotted and 31% in the arthroscopic knotless cohorts. By 2 years, the retear rates of tears greater than 5 cm2 were 20% greater in the open group (71%) than both arthroscopic groups (50%) (Fig. 2).
Fig. 2A–C.
The graphs show comparisons between intact and retorn rotator cuff repairs at 2 years postsurgery for preoperative tear size in (A) open (n = 20), (B) arthroscopic knotted (n = 27), and (C) arthroscopic knotless (n = 27) rotator cuff repairs.
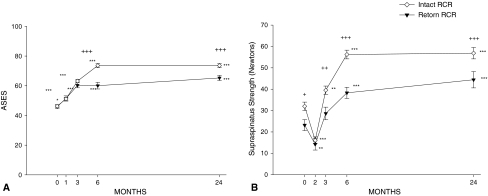
The data were reanalyzed according to whether there was an ultrasound-determined defect in the repair at 6 months and 2 years regardless of the repair technique (Table 5). All outcome scores (pain, ASES, stiffness, strength, rotator cuff functional index, and ROM) in the intact cuff group improved (p < 0.01) apart from internal rotation ROM between preoperative and 6-month and 2-year followups. No differences between intact and retorn cuff repairs were found at 6-month and 2-year followups for pain at rest, shoulder stiffness, forward flexion, abduction, external rotation, adduction strength, and internal and external rotation strength (Fig. 3). Differences in pain with overhead activity (p < 0.05), pain at night (p < 0.05), ASES score (p < 0.001), rotator cuff functional index (p < 0.001), and supraspinatus strength (p < 0.001) were found between the intact and retorn groups at 6 months and 2 years with poorer results in the retear group. At 2 years, patient-perceived stiffness was greater (p < 0.05) in retorn cuffs versus intact cuffs.
Table 5.
Effect of repair integrity on outcome scores, range of motion, and strength
| Outcome | 6 months’ followup | 2 years’ followup | ||||
|---|---|---|---|---|---|---|
| Intact (n = 118) | Retear (n = 41) | p Value* | Intact (n = 62) | Retear (n = 25) | p Value* | |
| Pain with overhead activity (0–4) | ||||||
| Preoperative | 3.1 ± 0.1 | 2.9 ± 0.1 | NS | 3.3 ± 0.2 | 3.2 ± 0.3 | NS |
| Followup | 1.3 ± 0.2§ | 1.7 ± 0.2§ | p < 0.05 | 1.2 ± 0.2§ | 1.9 ± 0.2§ | p < 0.05 |
| Stiffness (0–4) | ||||||
| Preoperative | 2.0 ± 0.1 | 1.8 ± 0.1 | NS | 2.2 ± 0.2 | 1.9 ± 0.1 | NS |
| Followup | 1.1 ± 0.1§ | 1.4 ± 0.2 | NS | 0.9 ± 0.1§ | 1.6 ± 0.2 | p < 0.05 |
| ASES score (0–100) | ||||||
| Preoperative | 46 ± 1 | 46 ± 1 | NS | 50 ± 3 | 48 ± 2 | NS |
| Followup | 74 ± 1§ | 60 ± 2§ | p < 0.001 | 77 ± 1§ | 64 ± 2§ | p < 0.001 |
| Rotator cuff functional index | ||||||
| Preoperative | −19 ± 2 | −26 ± 4 | p < 0.05 | −25 ± 2 | −32 ± 4 | NS |
| Followup | 2 ± 2§ | −19 ± 4 | p < 0.001 | 1 ± 1§ | −12 ± 4 | p < 0.001 |
| Forward flexion (°) | ||||||
| Preoperative | 141 ± 4 | 136 ± 6 | NS | 138 ± 4 | 141 ± 6 | NS |
| Followup | 167 ± 2§ | 152 ± 6† | NS | 170 ± 3§ | 158 ± 6† | NS |
| External rotation (°) | ||||||
| Preoperative | 51 ± 2 | 52 ± 3 | NS | 48 ± 3 | 50 ± 3 | NS |
| Followup | 64 ± 2§ | 62 ± 3 | NS | 60 ± 2§ | 58 ± 3 | NS |
| Supraspinatus strength (N) | ||||||
| Preoperative | 32 ± 3 | 23 ± 3 | p < 0.05 | 31 ± 2 | 21 ± 4 | |
| Followup | 56 ± 2§ | 38 ± 3§ | p < 0.001 | 56 ± 2§ | 44 ± 4§ | p < 0.01 |
| External rotation strength (N) | ||||||
| Preoperative | 42 ± 2 | 32 ± 3 | NS | 40 ± 2 | 36 ± 3 | NS |
| Followup | 63 ± 2‡ | 56 ± 4† | NS | 58 ± 2§ | 53 ± 4† | NS |
Values are expressed as mean ± standard error of the mean; * comparisons between groups using Kruskal-Wallis one-way analysis of variance on ranks and corrected for multiple comparison using Dunn’s method; †p < 0.05, ‡p < 0.01, §p < 0.001 using Mann-Whitney rank sum test; NS = no significance; ASES = American Shoulder and Elbow Surgeons.
Fig. 3A–B.
The graphs show comparisons between intact and retorn rotator cuff repairs (RCR) for (A) ASES score and (B) supraspinatus strength. The data are displayed as mean ± standard deviation of the mean (n = 119 for intact group and n = 41 for retorn group up to 6 months; n = 62 for intact group and n = 25 for retorn group at 24 months). * = p < 0.05, ** = p < 0.01, *** = p < 0.001 using Mann-Whitney rank sum test. + = p < 0.05, ++ = p < 0.01, +++ = p < 0.001 using Kruskal-Wallis one-way analysis of variance on ranks and corrected for multiple comparison using Dunn’s method.
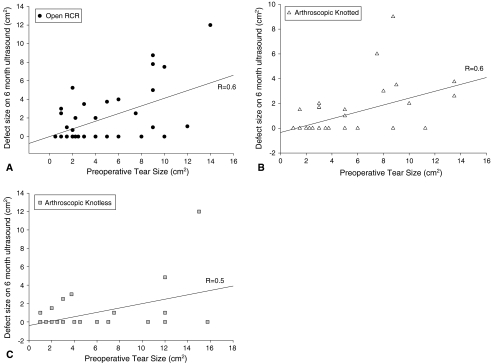
Multiple regression analyses found associations between the defect size on the followup ultrasound for preoperative tear size (r = 0.5; p < 0.001) and rotator cuff functional index score at the preoperative examination (r = −0.2; p < 0.05) and 6-month examination (r = −0.5; p < 0.001) (Fig. 4). Shorter operative time was associated with a lower retear rate (r = 0.3; p < 0.001), whereas the use of an open technique correlated with an increased retear rate (r = 0.2; p < 0.01). No association (r = −0.04; p = 0.5) was found between arthroscopic rotator cuff repair experience and the presence or absence of retears at 6 months and 2 years postsurgery (Table 6).
Fig. 4A–C.
The graphs compare preoperative tear size versus defect size at the 6-month ultrasound for (A) open (n = 49), (B) arthroscopic knotted (n = 53), and (C) arthroscopic knotless (n = 57) rotator cuff repairs (RCR). R = Pearson correlation coefficient.
Table 6.
Correlation coefficients for retear size and rate compared with patient factors
| Patient factor | Retear size on ultrasound (r) | p Value | Rate of retear (r) | p Value |
|---|---|---|---|---|
| Preoperative tear size | 0.5 | < 0.001 | 0.6 | < 0.01 |
| Preoperative rotator cuff functional index | −0.2 | < 0.05 | −0.3 | < 0.05 |
| Operative time | 0.3 | < 0.01 | 0.3 | < 0.001 |
| Open technique | 0.3 | < 0.01 | 0.2 | < 0.01 |
| Arthroscopic rotator cuff learning curve | 0.01 | 0.6 | −0.04 | 0.5 |
| Duration of symptoms before surgery | −0.03 | 0.7 | 0.04 | 0.2 |
| Patient age | 0.1 | 0.3 | 0.07 | 0.3 |
| Preoperative flexion | 0.1 | 0.3 | 0.2 | 0.8 |
| Preoperative ASES score | 0.1 | 0.2 | 0.2 | 0.3 |
| ASES score at 2 years | 0.2 | 0.2 | 0.1 | 0.09 |
| Preoperative supraspinatus strength | 0.03 | 0.6 | 0.05 | 0.2 |
| Supraspinatus strength at 2 years | 0.2 | 0.5 | 0.2 | 0.6 |
| Type of suture in open group (absorbable versus nonabsorbable) | 0.1 | 0.1 | 0.09 | 0.3 |
ASES = American Shoulder and Elbow Surgeons.
Discussion
We prospectively assessed the clinical outcomes of open repair versus knotted arthroscopic repair versus arthroscopic knotless repair and correlated these results with the integrity of the cuff as determined by ultrasonographic evaluation. Our hypothesis was that rotator cuff repair with an arthroscopic technique would result in better clinical and structural outcomes than double-row open rotator cuff repair.
The limitations of the study include the study design. The groups were three temporal cohorts rather than randomized groups. The shift in practice toward arthroscopic techniques may have changed surgical indications and postoperative regimes. More than one sonographer performed all postoperative imaging, and patients (62 of 312) who were not available for ultrasound evaluation at 6 months postsurgery were excluded. A large proportion of patients (48%) were lost to followup by 2 years postsurgery relating to the senior author’s practice where patients are followed up routinely for 1 year postsurgery and only return through self-referral. The high number of traumatic cuff tears in this study may relate to the Australian population, which is very active in the older age subsets, but also may affect the outcomes in this study as fewer tears were truly degenerative. Finally, the difference in postoperative immobilization between open and arthroscopic groups may account for the significant findings between these groups.
All clinical outcomes were similar at followup except that the ASES score was 20% better in the arthroscopic groups at 2 years postsurgery. An intact cuff corresponded to better clinical outcomes at 6 months and 2 years postsurgery.
Good clinical outcomes using either open or arthroscopic techniques for rotator cuff repair are well documented [8, 12, 14, 27, 38]. The short-term results for arthroscopic and mini-open rotator cuff repairs appear to be similar [33, 37], and recently, no differences were observed between clinical outcomes of open and arthroscopic techniques regardless of preoperative tear size at greater than 2 years of followup [40]. We found mini-open repair resulted in a reduced mean ASES score compared with both arthroscopic techniques at 6 months and 2 years postoperatively. Multiple regression analysis showed the ASES score could be best predicted by what surgical technique was used and by the supraspinatus strength. The difference in ASES scores appeared to be related to the 10-question functional section in the ASES scale, because there were no differences in the other components of the ASES, strength, pain, and stability. These results suggest patients perceive an open repair as functionally less satisfactory than arthroscopic repair. It also is interesting that the ASES scores at 6 months and 2 years postoperatively did not correlate with the size or incidence of retear. This seems to indicate the parameters tested in the ASES score are not sensitive enough to indicate a structural defect. The positive correlations between rotator cuff functional index and tear size/incidence, however, suggest a method of clinically assessing cuff functionality may better assess cuff integrity postsurgery.
There is debate regarding the importance of an intact rotator cuff after repair. Rotator cuff repair retear rates have been as much as 90% [5], with some studies having retear rates ranging from 13% to 35% [3, 10, 21, 22, 31]. Some studies have shown patients with a retear have poorer shoulder function than those with an intact cuff [1, 2, 36], whereas others have suggested integrity does not affect functional outcomes [5, 29]. In our study, when analyzing the effect of retear on clinical outcome, regardless of technique, intact cuffs scored better with respect to pain with overhead activity, mean ASES score, rotator cuff function index, and supraspinatus strength than retorn cuff repairs. This suggests the poorer clinical outcomes in patients with a retear are because their rotator cuff is weaker (supraspinatus strength) and they have decreased functional ability (rotator cuff functional index).
Recent studies suggest double-row fixation provides a superior biomechanical structure at time zero than single-row configurations [30, 34], which may account for reports suggesting a low retear rate with arthroscopic double-row constructs [23, 28]. However, comparative clinical studies have failed to show improvements in outcomes between single- and double-row arthroscopic repairs [9, 32]. Thus, our open repairs with a double-row configuration should have been mechanically stronger than the arthroscopic repairs at time zero and possibly produced the lowest retear rate. Despite the current evidence, our open technique produced a greater number of retears than the knotless technique and both arthroscopic techniques combined. It may be that the difference in retear rate is the result of the less invasive nature of arthroscopic techniques. When all factors were considered, a longer operative time on its own was associated with a greater likelihood of a retear. Another consideration is postoperative care. The open group had a regular sling rather than an ultrasling postoperatively, which may have increased tension in the open group at the early stages of the cuff repair compared with the arthroscopic groups. Another possible reason may have been the result of a change in attitude of treating cuff tears more aggressively earlier in their natural course. However, there was no association between duration of symptoms before surgery and retear rate. In the 7.5% of cases needing revision surgery in the first 6 months, 11 of the 12 cases experienced one or more traumatic events after the start of active overhead lifting 3 months postsurgery.
Increasing age [3], large initial tear size [11], large tears fixed arthroscopically [2], and injuries involving more than one tendon [31] have been described as negative prognostic factors with respect to cuff integrity. We found no associations between age, duration of symptoms, forward flexion, supraspinatus strength, and ASES score at preoperative and postoperative visits and the retear rate. However, our data do confirm there is a substantial incidence of retears during the first 6 months after rotator cuff repair [7, 15]. Temporal analysis shows, across all tear sizes (small to massive), there was no significant increase in the retear rate between 6 months and 2 years, again suggesting retears occur early in the postoperative course and earlier structural assessment may provide the surgeon with a good indicator on the long-term outcome of cuff repair.
Small rotator cuff tears have been shown to have the greatest potential to heal with increased fibroblast cellularity and inflammatory cells, whereas large/massive tears may have a reduced ability to repair and regenerate as a result of highly degenerate tissue [26]. Our results support this hypothesis because in tears less than 3 cm2 only 16% (nine of 59) retore, whereas tears greater than 3 cm2 had a 53% (16/30) chance of retear at 2 years postsurgery. A caveat to this observation, however, is the larger tears fixed with the arthroscopic knotless technique had a better chance of healing at 6 months than tears repaired using the other two techniques. Potential reasons for this include the greater mean number of anchors used in the knotless repairs than in the knotted group and the fact that the knotless procedure was started 2.5 years after the senior surgeon began performing arthroscopic repairs, which may contribute to the reduced operative time and may relate to better technique. The only other outcome improved with the knotless technique was a reduction in early postoperative pain. This may be related to reduced operative time and subsequent shoulder swelling.
Results of our study showed rotator cuff repair, whether performed through an open or arthroscopic technique, resulted in improvements in pain, motion, strength, and function. An intact cuff on ultrasound corresponded to better results for supraspinatus strength, patient-determined outcomes, and rotator cuff functional ability.
Acknowledgments
We thank SN Jeanette Marshall and SN Belinda Bosley for assistance with clinical examination and data collection.
Footnotes
One or more of the authors have received funding from Mitek Australia (GACM) and ArthroCare Australia/United Kingdom (GACM, NLM).
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Anderson K, Boothby M, Aschenbrener D, van Holsbeeck M. Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: minimum 2-year follow-up. Am J Sports Med. 2006;34:1899–1905. [DOI] [PubMed]
- 2.Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290–299. [DOI] [PubMed]
- 3.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. [DOI] [PubMed]
- 4.Bryant L, Shnier R, Bryant C, Murrell GA. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elbow Surg. 2002;11:219–224. [DOI] [PubMed]
- 5.Calvert PT, Packer NP, Stoker DJ, Bayley JI, Kessel L. Arthrography of the shoulder after operative repair of the torn rotator cuff. J Bone Joint Surg Br. 1986;68:147–150. [DOI] [PubMed]
- 6.Cummins CA, Murrell GA. Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J Shoulder Elbow Surg. 2003;12:128–133. [DOI] [PubMed]
- 7.Fealy S, Adler RS, Drakos MC, Kelly AM, Allen AA, Cordasco FA, Warren RF, O’Brien SJ. Patterns of vascular and anatomical response after rotator cuff repair. Am J Sports Med. 2006;34:120–127. [DOI] [PubMed]
- 8.Fealy S, Kingham TP, Altchek DW. Mini-open rotator cuff repair using a two-row fixation technique: outcomes analysis in patients with small, moderate, and large rotator cuff tears. Arthroscopy. 2002;18:665–670. [DOI] [PubMed]
- 9.Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB, Maffulli N, Denaro V. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35:1254–1260. [DOI] [PubMed]
- 10.Fuchs B, Gilbart MK, Hodler J, Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88:309–316. [DOI] [PubMed]
- 11.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224. [DOI] [PubMed]
- 12.Galatz LM, Griggs S, Cameron BD, Iannotti JP. Prospective longitudinal analysis of postoperative shoulder function: a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2001;83:1052–1056. [PubMed]
- 13.Gartsman GM, Hammerman SM. Full-thickness tears: arthroscopic repair. Orthop Clin North Am. 1997;28:83–98. [DOI] [PubMed]
- 14.Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 1998;80:832–840. [DOI] [PubMed]
- 15.Hashimoto T, Nobuhara K, Hamada T. Pathologic evidence of degeneration as a primary cause of rotator cuff tear. Clin Orthop Relat Res. 2003;415:111–120. [DOI] [PubMed]
- 16.Hayes K, Ginn KA, Walton JR, Szomor ZL, Murrell GA. A randomised clinical trial evaluating the efficacy of physiotherapy after rotator cuff repair. Aust J Physiother. 2004;50:77–83. [DOI] [PubMed]
- 17.Hayes K, Walton JR, Szomor ZR, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 2001;47:289–294. [DOI] [PubMed]
- 18.Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg. 2002;11:33–39. [DOI] [PubMed]
- 19.Ide J, Maeda S, Takagi K. A comparison of arthroscopic and open rotator cuff repair. Arthroscopy. 2005;21:1090–1098. [DOI] [PubMed]
- 20.Jost B, Pfirrmann CW, Gerber C, Switzerland Z. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82:304–314. [DOI] [PubMed]
- 21.Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88:472–479. [DOI] [PubMed]
- 22.Klepps S, Bishop J, Lin J, Cahlon O, Strauss A, Hayes P, Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722. [DOI] [PubMed]
- 23.Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533–1541. [DOI] [PubMed]
- 24.Liem D, Bartl C, Lichtenberg S, Magosch P, Habermeyer P. Clinical outcome and tendon integrity of arthroscopic versus mini-open supraspinatus tendon repair: a magnetic resonance imaging-controlled matched-pair analysis. Arthroscopy. 2007;23:514–521. [DOI] [PubMed]
- 25.L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79:738–748. [DOI] [PubMed]
- 26.Matthews TJ, Hand GC, Rees JL, Athanasou NA, Carr AJ. Pathology of the torn rotator cuff tendon: reduction in potential for repair as tear size increases. J Bone Joint Surg Br. 2006;88:489–495. [DOI] [PubMed]
- 27.Murray TF Jr, Lajtai G, Mileski RM, Snyder SJ. Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to 6-year follow-up. J Shoulder Elbow Surg. 2002;11:19–24. [DOI] [PubMed]
- 28.Nho SJ, Yadav H, Pensak M, Dodson CC, Good CR, MacGillivray JD. Biomechanical fixation in arthroscopic rotator cuff repair. Arthroscopy. 2007;23:94–102, 102 e101. [DOI] [PubMed]
- 29.Osbahr DC, Murrell GA. The rotator cuff functional index. Am J Sports Med. 2006;34:956–960. [DOI] [PubMed]
- 30.Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:469–476. [DOI] [PubMed]
- 31.Ratti C, Murena L, Surace MF, Rolla PR. Clinical and ultrasound results after arthroscopic repair of the rotator cuff. Chir Organi Mov. 2005;90:95–104. [PubMed]
- 32.Reardon DJ, Maffulli N. Clinical evidence shows no difference between single- and double-row repair for rotator cuff tears. Arthroscopy. 2007;23:670–673. [DOI] [PubMed]
- 33.Sauerbrey AM, Getz CL, Piancastelli M, Iannotti JP, Ramsey ML, Williams GR Jr. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcome. Arthroscopy. 2005;21:1415–1420. [DOI] [PubMed]
- 34.Tashjian RZ, Levanthal E, Spenciner DB, Green A, Fleming BC. Initial fixation strength of massive rotator cuff tears: in vitro comparison of single-row suture anchor and transosseous tunnel constructs. Arthroscopy. 2007;23:710–716. [DOI] [PubMed]
- 35.Tauro JC. Arthroscopic rotator cuff repair: analysis of technique and results at 2- and 3-year follow-up. Arthroscopy. 1998;14:45–51. [DOI] [PubMed]
- 36.Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff: a comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498–504. [PubMed]
- 37.Verma NN, Dunn W, Adler RS, Cordasco FA, Allen A, MacGillivray J, Craig E, Warren RF, Altchek DW. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy. 2006;22:587–594. [DOI] [PubMed]
- 38.Wolf EM, Pennington WT, Agrawal V. Arthroscopic rotator cuff repair: 4- to 10-year results. Arthroscopy. 2004;20:5–12. [DOI] [PubMed]
- 39.Yamaguchi K, Levine WN, Marra G, Galatz LM, Klepps S, Flatow EL. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 2003;52:81–92. [PubMed]
- 40.Youm T, Murray DH, Kubiak EN, Rokito AS, Zuckerman JD. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg. 2005;14:455–459. [DOI] [PubMed]