Abstract
Hip resurfacing is femoral bone preserving, but there is controversy regarding the amount of bone removed at the acetabular side. We therefore compared the implanted acetabular cup sizes in primary THAs between two resurfacing devices and a conventional press-fit cup using a series of 2134 THAs (Allofit® cup 1643 hips, Durom® Hip Resurfacing 249 hips, and Birmingham Hip® Resurfacing 242 hips). The effects of patient demographics and cup position in the horizontal plane also were assessed. After controlling for gender, patients were matched for height, weight, body mass index, and age. The mean size for Allofit® cups was smaller than the sizes for Durom® and Birmingham Hip® Resurfacing cups in women (49.9 mm, 51.6 mm, 52.3 mm, respectively) and men (55.1 mm, 56.7 mm, 57.8 mm; respectively). Although patient height was associated with the implanted cup size, the cup position in the horizontal plane had no effect on the size used. Larger cups were used with hip resurfacing than for THA with a conventional press-fit cup. However, additional studies are needed to determine whether these small differences have any clinical implications in the long term. The association of cup size and patient height should be considered in future studies comparing component sizes among different implants.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Metal-on-metal hip resurfacing arthroplasty (HRA) has had encouraging short- to midterm results in predominantly young and active patients [1, 2, 10, 17]. The life expectancy of these patients, mainly in their 40s and 50s, may exceed 30 years. Many patients seek hip arthroplasty relatively early and do not accept activity restrictions after surgery [17, 18]. Therefore many of these patients likely will require additional hip surgery or revision arthroplasty later in their lives. One benefit of HRA is preservation of femoral bone stock, which might ease future revision surgery [5, 21]. Preservation of acetabular bone during primary THA is similarly important as treatment of acetabular bone deficiency during revision arthroplasty is demanding and surgery becomes more technically difficult with decreasing bone stock [7–9, 16, 22]. However, controversy exists regarding the amount of bone removed from the acetabular side. Two studies suggest removal of acetabular bone during HRA is comparable to that of conventional THA [15, 23], whereas another study reported increased acetabular bone resection for HRA [13]. These studies are difficult to compare because they have some methodologic limitations (ie, small series of unmatched patients [13], no data for patient height or weight [15], heavier patients in the THA cohort [23]) and different implants (ie, Allofit® and Durom® [13], Allofit®, Ancafit®, Trident®, and Birmingham Hip® Resurfacing [BHR®] [15], AGB™ II, Trilogy®, and BHR® [23]) and implantation techniques used [13, 15, 23].
Considering the aforementioned background, our study addresses the following questions: (1) Does HRA require larger acetabular components than conventional THA using a press-fit cup? (2) Do any demographic patient variables correlate with the implanted acetabular component sizes? (3) Does cup position along the horizontal plane (medialization/lateralization) have an effect on the required cup sizes?
Material and Methods
We retrospectively analyzed prospectively recorded data for all patients who underwent THA at our clinic between January 2003 and December 2007. During this period, 2946 primary THAs were performed, of which 491 were HRAs. The standard press-fit cup used for stem-type THA was the Allofit® cup (Zimmer, Inc, Warsaw, IN). The Allofit® cup was implanted in 1643 hips using a posterior approach. This cup has a titanium grit-blasted surface, providing a total wall thickness of 2.9 mm. The cup has a flattened pole and an expanded rim and does not represent a full hemisphere. For resurfacing surgery, in which a posterior approach also was used, the Durom® Hip Resurfacing System (Zimmer) was implanted in 249 hips, and the Birmingham Hip® Resurfacing System (BHR®; Smith & Nephew, Solothurn, Switzerland) was implanted in 242 hips. The Durom® resurfacing system has a cobalt-chrome acetabular component with a titanium vacuum plasma-sprayed coating, providing a 4-mm wall thickness. It has a flattened pole and a peripheral fin and does not have a full hemisphere. The femoral components are available in 2-mm increments and match one cup size, which is 6 mm larger. The hemispheric BHR® component has a hydroxyapatite-coated surface, providing a 4-mm wall thickness. The femoral components of the BHR® are available in 4-mm increments only and match two cup sizes, which are 6 or 8 mm larger. Hip replacements (overall 812) in which other cups were used and/or in which an approach different from the posterior approach was performed (12 different cups in 691 hips and/or anterolateral approach in 281 hips, lateral approach in 324 hips) were excluded. Indications for HRA comprised young age (ie, normally younger than 60 years), active lifestyle (ie, participation in impact sports, such as jogging, tennis, and downhill skiing, or regular heavy labor, eg, mechanic, warehouseman, construction worker, or carpenter), the absence of radiographically visible osteoporosis or cystic degeneration of the femoral head, and the absence of severe anatomic abnormalities of the proximal femur. All HRAs were performed by two experienced orthopaedic senior surgeons; conventional THA was performed by eight different orthopaedic surgeons from our clinic. Surgical preparation of the acetabulum was similar for resurfacing and conventional THA components. We began reaming at 40 mm down to the natural bottom of the acetabulum; in some cases, the central osteophyte was removed first. Sequential reaming in 2-mm increments using the same standard reamer in all cases followed to the intended component size for the Allofit® and Durom® components (eg, 54 mm for a Size 54 cup); for the BHR® cup, we underreamed 2 mm (eg, 52 mm for a Size 54 cup). Peripheral osteophytes were removed back to the implant rim after placement of the cup to assure bony coverage particularly at the anterior wall. Both surgeons who performed HRA followed similar surgical steps, with implantation of the acetabular component after defining the minimum size of the femoral component. During the study period, both surgeons also performed 1088 stem-type primary THAs.
The sizes of the acetabular components used were obtained from the operative notes. For analyses, we controlled for gender by separating patients into women and men. Matched groups were created as follows: starting with the smallest cohort (BHR®), all patients whose height, weight, body mass index (BMI), and age were greater or less than two standard deviations (SD) of each mean were removed. Afterward, patients were selected randomly from the two larger cohorts (Durom® and Allofit®) and matched to the patients with BHR® prostheses for height, weight, BMI, and age. This matching procedure created comparable groups of 56 women and 125 men each (Tables 1, 2). The cup sizes of the different implants were compared using unpaired t tests after testing for normal distribution (Shapiro-Wilk W test). To account for underreaming of the BHR®, we repeated the analyses for the last used reamer size, which was 2 mm smaller than the cups in hips with the BHR® prostheses.
Table 1.
Matched groups (women)
| Variable | Acetabular component | p Value | ||
|---|---|---|---|---|
| Allofit® | Durom® | BHR® | ||
| Number of hips | 56 | 56 | 56 | |
| Age (years) | 48.7 ± 11.0 (21–71) | 48.7 ± 11.1 (20–73) | 48.7 ± 11.1 (19–68) | > 0.9 |
| Height (cm) | 166.1 ± 6.3 (155–179) | 166.1 ± 6.2 (152–180) | 166.1 ± 6.5 (151–178) | > 0.9 |
| Weight (kg) | 66.4 ± 11.8 (50–98) | 66.5 ± 12.8 (50–98) | 66.5 ± 10.4 (50–95) | > 0.9 |
| BMI (kg/m2) | 23.9 ± 5.1 (19.4–32.3) | 24.0 ± 3.5 (19.2–35.6) | 24.1 ± 3.6 (18.7–34.9) | > 0.9 |
Values are expressed as mean ± standard deviation, with range in parentheses; BHR® = Birmingham Hip® Resurfacing System; BMI = body mass index.
Table 2.
Matched groups (men)
| Variable | Acetabular component | p Value | ||
|---|---|---|---|---|
| Allofit® | Durom® | BHR® | ||
| Number of hips | 125 | 125 | 125 | |
| Age (years) | 54.8 ± 7.2 (32–69) | 54.3 ± 8.2 (34–69) | 53.9 ± 8.4 (34–69) | > 0.5 |
| Height (cm) | 178.2 ± 5.3 (164–192) | 178.2 ± 4.8 (165–190) | 178.2 ± 4.9 (166–190) | > 0.9 |
| Weight (kg) | 85.0 ± 8.4 (70–102) | 85.0 ± 8.6 (70–102) | 85.0 ± 4.5 (70–104) | > 0.9 |
| BMI (kg/m2) | 26.8 ± 2.2 (23.0–31.6) | 26.8 ± 2.3 (23.0–31.6) | 26.8 ± 2.2 (23.1–31.6) | > 0.9 |
Values are expressed as mean ± standard deviation, with range in parentheses; BHR® = Birmingham Hip® Resurfacing System; BMI = body mass index.
To determine whether any demographic patient variables were associated with acetabular cup size, we correlated height, weight, BMI, and age with the sizes of the implanted cups using Pearson correlation coefficients after testing for normal distribution (Shapiro-Wilk W test).
To assess the effect of the cup position in the horizontal plane, one of the authors who was not involved in surgery (MSK) measured the preoperative and postoperative horizontal distances between the hip center and a vertical line drawn through the medial edge of the ipsilateral teardrop on plain anteroposterior radiographs [11]. If the teardrop was not visible, the ilioischial line (Kohler’s line) was used as reference [11]. We subtracted the postoperatively measured distance from the preoperatively measured distance and correlated the obtained values with the cup sizes using Pearson correlation coefficients after testing for normal distribution (Shapiro-Wilk W test). We also compared the sizes of the 15 most medialized cups with those of the 15 most lateralized cups (unpaired t tests after testing for normal distribution).
All statistical tests were performed using SPSS® (Version 13; SPSS Inc, Chicago, IL). Unless otherwise stated, all data are presented as the mean ± SD.
Results
Combining the data of both resurfacing implants, HRAs required larger cups than conventional THAs in women (52.0 ± 3.0 mm versus 49.9 ± 2.6 mm; p = 0.000012) and in men (57.3 ± 2.4 mm versus 55.1 ± 3.0 mm; p = 4.1E−14). The last used reamer size was greater in HRAs than in conventional THAs in women (51.0 ± 3.0 mm versus 49.9 ± 2.6 mm; p = 0.015) and in men (56.3 ± 2.4 mm vs. 55.1 ± 3.0 mm; p = 1.7E−05).
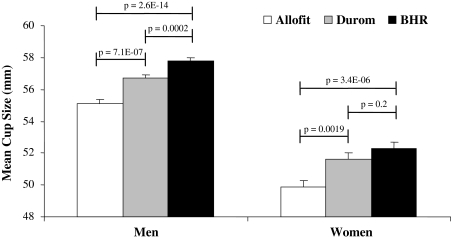
In women, we found the Allofit® components were smaller than Durom® cups and smaller than BHR® cups, while there were no differences between Durom® and BHR® shells (Fig. 1). In men, Allofit® components were smaller than Durom® cups and smaller than BHR® cups, and Durom® components were smaller than the BHR® shells (Fig. 1).
Fig. 1.
A graph shows the implanted cup sizes of three different acetabular components for primary THA after matching the patients for height, weight, BMI, and age. In men, Allofit® cups were smaller than Durom® (p = 7.1E−07) and BHR® (p = 2.6E−14) cups. Durom® cups were smaller (p = 0.0002) than BHR® shells. In women, Allofit® components were similarly smaller than Durom® (p = 0.0019) and BHR® (p = 3.4E−06) components. There was no size difference (p = 0.2) between Durom® and BHR® cups.
The last used reamer size was smaller in Allofit® hips than in BHR® hips in men, and in women and men, the last used reamer size was smaller in BHR® hips than in Durom® hips (Table 3).
Table 3.
Comparisons of the last used reamer sizes
| Implant | Female patients | Male patients | ||
|---|---|---|---|---|
| Last reamer size (mm) | p Value | Last reamer size (mm) | p Value | |
| Allofit® | 49.9 ± 2.6 | * | 55.1 ± 3.0 | † |
| Durom® | 51.6 ± 3.2 | * | 56.7 ± 2.2 | † |
| BHR® | 50.3 ± 2.7 | * | 55.8 ± 2.4 | † |
Values are expressed as mean ± standard deviation; BHR® = Birmingham Hip® Resurfacing System; *Allofit®/Durom®: p = 0.0019; Allofit®/BHR®: p = 0.36; Durom®/BHR®: p = 0.023; †Allofit®/Durom®: p = 7.1E−07; Allofit®/BHR®: p = 0.024; Durom®/BHR®: p = 0.003.
Acetabular component size correlated with patient height (r = 0.67; p = 4.9E−275), as did patient weight (r = 0.48; p = 2.4E−121) and BMI (r = 0.15; p = 3.0E−012). Patient age did not correlate (r = − 0.02; p = 0.26) with acetabular component size.
The position of the cup in the horizontal plane did not correlate with the used cup size (Table 4). Similarly, the mean cup size of the most medially placed components did not differ from the mean cup size of the most laterally placed components (Table 5).
Table 4.
Correlation between cup medialization and cup sizes
| Implant | Female patients | Male patients | ||
|---|---|---|---|---|
| Correlation coefficient (r) | p Value | Correlation coefficient (r) | p Value | |
| Allofit® | 0.07 | 0.610 | −0.06 | 0.527 |
| Durom® | −0.06 | 0.656 | −0.12 | 0.204 |
| BHR® | −0.05 | 0.751 | 0.10 | 0.295 |
Correlations expressed as Pearson coefficients; BHR® = Birmingham Hip® Resurfacing System.
Table 5.
Effects of cup position in the horizontal plane on implanted cup sizes
| Implant | Female patients | Male patients | ||||
|---|---|---|---|---|---|---|
| Size of most medialized cups | Size of most lateralized cups | p Value | Size of most medialized cups | Size of most lateralized cups | p Value | |
| Allofit® | 50.0 ± 2.7 (46–56) | 49.9 ± 2.3 (46–54) | 0.886 | 54.8 ± 2.9 (50–58) | 55.2 ± 3.1 (48–60) | 0.718 |
| Durom® | 52.0 ± 2.0 (50–56) | 52.0 ± 4.7 (46–62) | 0.898 | 56.8 ± 2.5 (52–60) | 56.9 ± 2.3 (52–60) | 0.879 |
| BHR® | 52.4 ± 3.4 (48–58) | 52.5 ± 2.1 (48–56) | 1.000 | 58.0 ± 2.5 (52–60) | 57.5 ± 2.7 (52–62) | 0.577 |
Values are expressed as mean ± standard deviation, with range in parentheses; BHR® = Birmingham Hip® Resurfacing System.
Discussion
Although HRA preserves femoral bone, there is controversy regarding the amount of bone resected on the acetabular side. Two previous studies suggest removal of acetabular bone during HRA is comparable to that of conventional THA [15, 23], whereas another report suggests increased acetabular bone resection is required for resurfacing surgery [13]. However, these reports are difficult to compare because they had methodologic limitations, used different implants and techniques, and had different patient demographics [13, 15, 23]. We therefore addressed the following questions: (1) Does HRA require larger acetabular components than conventional THA using a press-fit cup? (2) Which demographic patient variables correlate with the implanted acetabular component sizes? (3) Does the cup position in the horizontal plane (medialization/lateralization) have an effect on the required cup sizes?
Our study has certain limitations. The major limitation is that we cannot conclude whether the observed small differences have any long-term implications for implant survival or number of future revisions in these young patients. This important issue should be addressed in future investigations with long-term clinical followup. The retrospective study design offers the advantage that the surgeons were not biased by a known comparison of their implanted cup sizes. The collection of data from several surgeons might be considered a limitation of our study, however, it more accurately reflects clinical reality. A comparison of the distribution of cup sizes used by the different surgeons revealed no differences (data not shown).
Our data showed HRA used larger acetabular components and larger reamers compared with conventional THA using a standard press-fit cup. Our data compare with that of Loughead et al. [13], who reported the mean implanted acetabular diameter was 56.5 mm in the BHR® group and 52.0 mm in the THA group, using either the AGB™ II (Stryker Orthopaedics, Mahway, NJ) or Trilogy® (Zimmer) cup (Table 6). In contrast, Vendittoli et al. [23] reported no difference in the size of the acetabular components between the press-fit Allofit® cup (54.7 mm) and the Durom® resurfacing implant (54.9 mm). The mean cup size they reported for the Durom® cup was smaller than the value we found. This might be explained by different demographic patient variables, particularly gender distribution, patient height, and patient weight. Vendittoli et al. [23] stated they made no attempt to seat all components to the natural bottom of the acetabulum, but our results refute the possible hypothesis that consequential cup lateralization might have resulted in the use of smaller components. Our data suggest the amount of medialization or lateralization did not correlate with the used component sizes, and similarly, the mean size of the most medially placed cups did not differ from that of the most laterally placed cups. The presumption that patient demographics have a stronger association with acetabular component size than cup position in the horizontal plane is supported by comparison of our results with those of Moonot et al. [15]. They performed a matched-group analysis separately for women and men comparing BHR® and THA cup sizes. Contrary to our findings, they reported no differences in men and smaller outside diameters of the BHR® components than those of the THA components in women [15]. Additionally, the mean cup sizes they presented were larger than those we found. These differences again might be related to relevant differences in patient demographics. Moonot et al. [15] performed only an age- and gender-matched analysis, without providing data on patient height or weight. Our data suggest patient height and weight are associated with the implanted acetabular component size, but not patient age. Nevertheless, in comparison to other studies, particularly studies of US patients, the comparatively low BMI values in our cohort must be considered.
Table 6.
Comparison of resurfacing and conventional THA cup sizes
| Study | Cup size (mm) | p Value | |
|---|---|---|---|
| Resurfacing | Conventional THA | ||
| Current authors | 52.0 (46–62)* | 49.9 (46–58)* | 0.000012 |
| 57.3 (50–64)† | 55.1 (48–62)† | 4.1E−14 | |
| Loughead et al. [13] | 56.5 | 52.0 | < 0.001 |
| Moonot et al. [15] | 51.6 (46–58)* | 53.6 (46–66)* | < 0.001 |
| 57.8 (52–64)† | 57.6 (52–64)† | 0.77 | |
| Vendittoli et al. [23] | 54.9 (44–64) | 54.7 (48–62) | 0.77 |
Values are expressed as mean, with range in parentheses; *female patients only; †male patients only.
Conservation of bone stock, not only on the femoral side, is an increasingly important issue in THA, considering the demographics of patients are changing toward an increasing proportion of younger and more active individuals [17–19]. These patients in their 40s and 50s are likely to undergo revision THA later during life, which would be aggravated by compromised bone stock owing to excessive bone removal during primary THA [3, 19]. It is true that HRA preserves bone on the femoral side. However, the minimum size of the femoral component is defined by the femoral neck diameter; otherwise notching will occur, resulting in an increased risk for femoral neck fractures, a major cause of failure in HRA [4, 6, 14, 20]. Therefore, considering the large femoral components and minimum wall diameter of the acetabular cups necessary to provide sufficient internal rigidity [24], additional bone resection on the acetabular side might be the result of femoral bone preservation [12]. This assumption was affirmed by Loughead et al. [13] and by our results. However, we are not aware of studies showing larger cup sizes or removal of more bone during primary THA will lead to earlier failures or more revisions in the future. Despite published evidence that conservation of acetabular bone is eminently important for revision THA and that technical difficulties during revision increase with decreasing bone stock [7–9, 16, 22], it is unclear if the small differences we observed, despite being statistically significant, will have any clinical implications in the long term. The differences of approximately 2 mm correspond to one incremented cup size, and if the last reamer size is considered, these differences are reduced to approximately 1 mm; this 1-mm difference could be easily explained by the different wall thickness: 4 mm in HRA and 2.9 mm in Allofit® components. Therefore, it seems, with proper surgical techniques, differences in cup sizes between HRA and conventional THA can be reduced to implant design specifics. The small differences we observed between the Durom® and BHR® prostheses might be related to implant characteristics, with a hemispheric cup design of the BHR® and a nonhemispheric design of the Durom®, and availability of 2-mm increments for the Durom® femoral component but only 4-mm increments for the BHR®.
Our study showed HRA required larger (52.0 versus 49.9 mm in women and 57.3 versus 55.1 mm in men) acetabular components than THA using a conventional press-fit cup and differences between the BHR® and Durom® resurfacing systems were marginal. Future studies should investigate if these small differences have any clinical implications in the long term. Although cup position in the horizontal plane had no effect, patient height was associated with the size of the implanted acetabular components. These observations should be considered in future studies comparing component sizes among implants or between HRA and conventional THA.
Acknowledgments
We thank Franco M. Impellizzeri for help with the study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC, Ball ST, Le Duff MJ, Dorey FJ. Resurfacing THA for patients younger than 50 year: results of 2- to 9-year followup. Clin Orthop Relat Res. 2007;460:159–164. [DOI] [PubMed]
- 2.Amstutz HC, Beaulé PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed]
- 3.Amstutz HC, Campbell P, Le Duff MJ. Metal-on-metal hip resurfacing: what have we learned? Instr Course Lect. 2007;56:149–161. [PubMed]
- 4.Anglin C, Masri BA, Tonetti J, Hodgson AJ, Greidanus NV. Hip resurfacing femoral neck fracture influenced by valgus placement. Clin Orthop Relat Res. 2007;465:71–79. [DOI] [PubMed]
- 5.Ball ST, Le Duff MJ, Amstutz HC. Early results of conversion of a failed femoral component in hip resurfacing arthroplasty. J Bone Joint Surg Am. 2007;89:735–741. [DOI] [PubMed]
- 6.Beaulé PE, Poitras P. Femoral component sizing and positioning in hip resurfacing arthroplasty. Instr Course Lect. 2007;56:163–169. [PubMed]
- 7.Boscainos PJ, Kellett CF, Maury AC, Backstein D, Gross AE. Management of periacetabular bone loss in revision hip arthroplasty. Clin Orthop Relat Res. 2007;465:159–165. [DOI] [PubMed]
- 8.Gross AE. Restoration of acetabular bone loss 2005. J Arthroplasty. 2006;21(4 suppl 1):117–120. [DOI] [PubMed]
- 9.Gross AE, Duncan CP, Garbuz D, Mohamed EM. Revision arthroplasty of the acetabulum in association with loss of bone stock. Instr Course Lect. 1999;48:57–66. [PubMed]
- 10.Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years: an independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89:1431–1438. [DOI] [PubMed]
- 11.Incavo SJ, DiFazio FA, Howe JG. Cementless hemispheric acetabular components 2–4-year results. J Arthroplasty. 1993;8:573–580. [DOI] [PubMed]
- 12.Lachiewicz PF. Metal-on-metal hip resurfacing: a skeptic’s view. Clin Orthop Relat Res. 2007;465:86–91. [DOI] [PubMed]
- 13.Loughead JM, Starks I, Chesney D, Matthews JN, McCaskie AW, Holland JP. Removal of acetabular bone in resurfacing arthroplasty of the hip: a comparison with hybrid total hip arthroplasty. J Bone Joint Surg Br. 2006;88:31–34. [DOI] [PubMed]
- 14.Marker DR, Seyler TM, Jinnah RH, Delanois RE, Ulrich SD, Mont MA. Femoral neck fractures after metal-on-metal total hip resurfacing: a prospective cohort study. J Arthroplasty. 2007;22(7 suppl 3):66–71. [DOI] [PubMed]
- 15.Moonot P, Singh PJ, Cronin MD, Kalairajah YE, Kavanagh TG, Field RE. Birmingham hip resurfacing: is acetabular bone conserved? J Bone Joint Surg Br. 2008;90:319–323. [DOI] [PubMed]
- 16.Murphy SB. Management of acetabular bone stock deficiency. J Arthroplasty. 2005;20 (4 suppl 2):85–90. [DOI] [PubMed]
- 17.Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35:705–711. [DOI] [PubMed]
- 18.Naal FD, Schmied M, Munzinger U, Leunig M, Hersche O. Outcome of hip resurfacing arthroplasty in patients with developmental hip dysplasia. Clin Orthop Relat Res. 2008 Aug 22. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 19.Schmalzried TP. Why total hip resurfacing. J Arthroplasty. 2007;22(7 suppl 3):57–60. [DOI] [PubMed]
- 20.Shimmin AJ, Bare J, Back DL. Complications associated with hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:187–193. [DOI] [PubMed]
- 21.Shimmin A, Beaulé PE, Campbell P. Metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am. 2008;90:637–654. [DOI] [PubMed]
- 22.Sporer SM, Paprosky WG, O’Rourke M. Managing bone loss in acetabular revision. J Bone Joint Surg Am. 2005;87:1620–1630. [DOI] [PubMed]
- 23.Vendittoli PA, Lavigne M, Girard J, Roy AG. A randomised study comparing resection of acetabular bone at resurfacing and total hip replacement. J Bone Joint Surg Br. 2006;88:997–1002. [DOI] [PubMed]
- 24.Yew A, Jin ZM, Donn A, Morlock MM, Isaac G. Deformation of press-fitted metallic resurfacing cups Part 2: Finite element simulation. Proc Inst Mech Eng H. 2006;220:311–319. [DOI] [PubMed]