Abstract
OBJECTIVE
To evaluate the association of neighborhood-level income and individual-level education with post-myocardial infarction (MI) mortality in community patients.
PATIENTS AND METHODS
From November 1, 2002, through May 31, 2006, 705 (mean ± SD age, 69±15 years; 44% women) residents of Olmsted County, MN, who experienced an MI meeting standardized criteria were prospectively enrolled and followed up. The neighborhood's median household income was estimated by census tract data; education was self-reported. Demographic and clinical variables were obtained from the medical records.
RESULTS
Living in a less affluent neighborhood and having a low educational level were both associated with older age and more comorbidity. During follow-up (median, 13 months), 155 patients died. Neighborhood income (hazard ratio [HR], 2.10; 95% confidence interval [CI], 1.42-3.12; for lowest [median, $34,205] vs highest [median, $60,652] tertile) and individual education (HR, 2.21; 95% CI, 1.47-3.32; for <12 vs >12 years) were independently associated with mortality risk. Adjustment for demographics and various post-MI prognostic indicators attenuated these estimates, yet excess risk persisted for low neighborhood income (HR, 1.62; 95% CI, 1.08-2.45). Modeled as a continuous variable, each $10,000 increase in annual income was associated with a 10% reduction in mortality risk (adjusted HR, 0.90; 95% CI, 0.82-0.99).
CONCLUSION
In this geographically defined cohort of patients with MI, low individual education and poor neighborhood income were associated with a worse clinical presentation. Poor neighborhood income was a powerful predictor of mortality even after controlling for a variety of potential confounding factors. These data confirm the socioeconomic disparities in health after MI.
Measures of social position have long been associated with post-myocardial infarction (MI) risk.1,2 However, much of this complex interaction has yet to be elucidated. Socioeconomic status (SES) is a multidimensional construct comprising various factors acting at different levels3-5 such that both individual-level and area-level measures could affect cardiovascular health through complementary mechanisms.4,6-8
In view of this concept, a “double jeopardy” (ie, a multidimensional vulnerability related to SES) theory was formulated but never formally tested.9,10 Indeed, most previous studies examining the interaction between SES and risk after MI were limited to a single indicator or a few indicators measured at a single level.11-21 Given that the effects of each SES indicator can in part be either explained by or mediated through other indicators,5 these data are incomplete. Further, most prior studies were conducted in selected populations such as clinical trial participants or women,2,13,18 took place in different health care systems,12,14-16,19,21 or used administrative or registry data and lacked essential clinical details.10,12,15-17,19 These limitations are important because failing to control for key clinical factors leaves substantial potential for residual confounding and thus inconclusive results. Therefore, both the internal and external validity of these results can be challenged, and their applicability to the community is uncertain.22,23
Our study was undertaken to address these knowledge gaps by examining the association between primary SES indicators and post-MI mortality in patients from a geographically defined population. Specifically, we evaluated the prognostic importance of individual education and neighborhood-based income in defining risk after MI.
PATIENTS AND METHODS
The study was conducted in Olmsted County, MN, where Mayo Clinic and the Olmsted Medical Center provide medical care for all county residents. Each institution uses a unit medical record in which the details of care for a patient, regardless of setting, are available in one place. The records are easily retrievable because Mayo Clinic maintains extensive indices that, through the Rochester Epidemiology Project, are extended to the records of other health care providers in the county, linking all records from all sources of care through a centralized system.24
Olmsted County (2000 census population, 124,277) is 144 km southeast of Minneapolis and St Paul; approximately 70% of its population resides in Rochester. Its population is largely middle class; 91% of adults have graduated from high school, 2.4% are uninsured, and 6.4% have incomes below poverty level.25 With the exception of a higher proportion working in the health care industry, population characteristics are similar to those of US whites.
The current analysis grew out of an observational parent study that prospectively investigated the effect of the new definition of MI on case ascertainment. Details of the enrollment procedures have been described previously.26 Between November 1, 2002, and May 31, 2006, 705 patients were enrolled. The mean ± SD age of the cohort was 69±15 years; 44% were women. All residents presenting to an Olmsted County facility with a cardiac troponin T level of 0.03 ng/mL or greater (to convert to μg/L, multiply by 1.0), the cutoff value used at Mayo Clinic and the value at which the coefficient of variation for the assay is 10% or less,27 were prospectively identified within 12 hours of the blood draw through the electronic files of the Department of Laboratory Medicine. Nurse coordinators sought written consent from all patients to measure cardiac biomarkers in unused blood samples initially stored for additional clinical need. If a blood sample was unavailable, an additional sample was drawn, in conjunction with a clinically indicated draw when possible.
Standardized criteria were used to determine MI status,28 on the basis of cardiac pain, electrocardiographic data (using Minnesota coding), and biomarker levels.
The participation rate was 82% for the overall study and was higher among patients with confirmed MI.29 The Mayo Clinic and Olmsted Medical Center institutional review boards approved all aspects of the study.
Socioeconomic Indicators and Risk Factors
Education (ie, years of school completed) was self-reported by a demographic questionnaire. Neighborhood-level SES was obtained by linking the patients' addresses (at the time of the index date) to 2000 census data (US Census Bureau).25 A total of 33 census tracts were included (Table 1). The census tract's median household income was chosen for analysis, on the basis of recommendations by Geronimus and Bound.30
TABLE 1.
Residents in Each Census Tract
| Census tract No. | No. of residents (%) | Median household income ($) |
|---|---|---|
| 1 | 40 (5.7) | 14,668 |
| 2 | 25 (3.5) | 34,205 |
| 3 | 20 (2.8) | 37,460 |
| 4 | 24 (3.4) | 53,561 |
| 5 | 13 (1.8) | 33,107 |
| 6 | 43 (6.1) | 28,732 |
| 7 | 14 (2.0) | 49,435 |
| 9.01 | 11 (1.6) | 48,750 |
| 9.02 | 14 (2.0) | 48,125 |
| 9.03 | 13 (1.8) | 74,034 |
| 10 | 33 (4.7) | 50,091 |
| 11 | 15 (2.1) | 58,143 |
| 12.01 | 17 (2.4) | 83,494 |
| 12.02 | 15 (2.1) | 56,006 |
| 12.03 | 10 (1.4) | 110,820 |
| 13.01 | 20 (2.8) | 55,625 |
| 13.02 | 15 (2.1) | 68,021 |
| 14.01 | 28 (4.0) | 45,318 |
| 14.02 | 21 (3.0) | 77,391 |
| 15.01 | 21 (3.0) | 59,635 |
| 15.02 | 17 (2.4) | 54,865 |
| 15.03 | 14 (2.0) | 60,652 |
| 16.01 | 32 (4.5) | 47,400 |
| 16.02 | 13 (1.8) | 71,125 |
| 16.03 | 18 (2.6) | 70,048 |
| 17.01 | 23 (3.3) | 51,343 |
| 17.02 | 16 (2.3) | 40,417 |
| 17.03 | 5 (0.7) | 86,766 |
| 18 | 18 (2.6) | 58,672 |
| 19 | 32 (4.5) | 56,992 |
| 20 | 37 (5.2) | 49,509 |
| 21 | 32 (4.5) | 44,665 |
| 22 | 29 (4.1) | 55,492 |
| Othersa | 7 (1.0) | |
| Total | 705 |
Census tract unknown (neighborhood income estimated by zip code).
Inpatient and outpatient medical records were used to ascertain cardiovascular risk factors, comorbidity, MI characteristics and severity, and medical treatment given during the index hospitalization. Smoking was categorized as current vs non-current smoking. Diabetes, hypertension, and dyslipidemia were defined clinically. Comorbidity was assessed by the Charlson index31 and analyzed categorically. Revascularization included percutaneous transluminal coronary angioplasty and coronary artery bypass grafting performed during the index hospitalization.
Mortality Follow-up
Follow-up was completed by surveillance of medical records. The comprehensive approach in place under the auspices of the Rochester Epidemiology Project ensures complete ascertainment of deaths, as it incorporates several sources of information. First, all death certificates for Olmsted County residents are obtained every year from the county office. Second, the Mayo Clinic registration office monitors the obituaries and notices of death in the local newspapers to update the record. Finally, electronic files of death certificates are obtained from the State of Minnesota Department of Vital and Health Statistics.24,32
Statistical Analyses
Analyses were performed using the statistical software package SAS, version 9.1 (SAS Institute, Cary, NC). For comparisons of baseline characteristics, participants were divided into neighborhood income tertiles and 3 education categories (defined as fewer than, equal to, and greater than 12 years of schooling). Income tertiles were defined as median (25th-75th percentile): (1) $34,205 ($28,732-$44,665); (2) $50,091 ($49,435-$53,561); and (3) $60,652 ($56,992-$74,034).
Survival across income and education categories, estimated using the Kaplan-Meier method with right censoring at the time of last follow-up, was compared by the log-rank test. Cox proportional hazards models were constructed to evaluate the unadjusted and covariate-adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for death in income and education categories. No missing values in the variables were used in the regression analyses, except for ejection fraction (19%), for which an indicator variable reflecting a missing value was included when appropriate. The proportional hazards assumption was tested using the Schoenfeld residuals, with no violations detected. All P values were 2-tailed.
RESULTS
The baseline characteristics across income tertiles and education categories are presented in Table 2. On average, patients living in less affluent areas were older and more likely to be female and of races other than white. They also presented with more comorbidity and included a higher proportion of smokers than their more affluent counterparts. No other differences were observed after adjustment for age and sex. The percentages of patients with fewer than, equal to, and greater than 12 years of education were 15% (n=105), 36% (n=252), and 49% (n=338), respectively. Lower education was associated with older age, races other than white, higher prevalence of smoking and diabetes, more comorbidity, and a lower ejection fraction.
TABLE 2.
Baseline Characteristics by Neighborhood Income and Individual Educationa
| Income tertiles |
Education categories |
|||||
|---|---|---|---|---|---|---|
| Characteristic | First (n=219) | Second (n=238) | Third (n=248) | <12y (n=105) | 12 y (n=252) | >12y (n=338) |
| Median | $34,205 | $50,091 | $60,652 | 8y | 12 y | 16 y |
| Demographics | ||||||
| Age (y), mean ± SD | 73±15 | 67±15 | 67±14b | 77±13 | 69±14 | 66±15b |
| Female | 120 (55) | 89 (37) | 100 (40)c | 54 (51) | 124 (49) | 133 (39) |
| White | 204 (93) | 231 (97) | 239 (96)c | 97 (92) | 244 (97) | 326 (96)c |
| Cardiovascular risk factors | ||||||
| Prior MI | 17 (8) | 7 (3) | 11 (4) | 9 (9) | 15 (6) | 13 (4) |
| Hypertension | 167 (76) | 152 (64) | 179 (72) | 84 (80) | 182 (72) | 234 (69) |
| Diabetes | 55 (25) | 55 (23) | 58 (23) | 38 (36) | 64 (25) | 68 (20)b |
| Hyperlipidemia | 133 (61) | 148 (62) | 148 (60) | 58 (55) | 159 (63) | 206 (61) |
| Current smoking | 39 (18) | 55 (23) | 44 (18)c | 16 (15) | 69 (27) | 49 (15)b |
| BMI, mean ± SDd | 27.8±6.0 | 29.0±6.4 | 28.8±6.4 | 27.9±6.0 | 28.5±6.5 | 28.7±6.1 |
| MI characteristics and comorbidity | ||||||
| ST elevation | 35 (16) | 45 (19) | 62 (25) | 19 (18) | 48 (19) | 75 (22) |
| Ejection fraction | ||||||
| ≥50 | 116 (68) | 137 (68) | 139 (70) | 45 (56) | 146 (70) | 196 (71)b |
| 35-49 | 37 (22) | 40 (20) | 47 (24) | 21 (26) | 43 (21) | 58 (21) |
| <35 | 18 (11) | 25 (12) | 13 (7) | 15 (19) | 18 (9) | 22 (8) |
| Comorbidity index, points | ||||||
| 0 | 44 (20) | 84 (35) | 99 (40)a | 13 (12) | 74 (29) | 130 (39)a |
| 1-2 | 81 (37) | 80 (34) | 73 (29) | 41 (39) | 73 (29) | 117 (35) |
| ≥3 | 94 (43) | 74 (31) | 76 (31) | 51 (49) | 104 (41) | 91 (27) |
| Treatmente | ||||||
| PTCA | 88 (40) | 119 (50) | 124 (50) | 39 (37) | 115 (46) | 170 (50) |
| CABG | 13 (6) | 15 (6) | 23 (9) | 8 (8) | 17 (7) | 26 (8) |
| Statins | 139 (64) | 174 (73) | 165 (67) | 65 (62) | 173 (69) | 235 (70) |
| β-Blockers | 201 (92) | 215 (90) | 215 (90) | 92 (88) | 225 (89) | 312 (92) |
| Aspirin | 198 (90) | 219 (92) | 232 (94) | 94 (90) | 231 (92) | 314 (93) |
Data are presented as number (percentage) unless otherwise specified. BMI = body mass index; CABG = coronary artery bypass grafting; MI = myocardial infarction; PTCA = percutaneous transluminal coronary angioplasty.
Age- and sex-adjusted P for trend ≤.05.
Age- and sex-adjusted P for trend ≤.01.
Calculated as weight in kilograms divided by the square of height in meters.
During the index hospitalization.
Over a median follow-up of 13 months (25th-75th percentile, 7-19 months), 155 patients died. The 1-year survival estimates across income tertiles (lowest to highest) were 75%, 83%, and 86%, respectively (P<.001). Similarly, for education the survival estimates at 1 year were 67%, 81%, and 85% for patients with fewer than, equal to, and greater than 12 years, respectively (P<.001). Modeled as mutually exclusive groups containing income and education categories, both socioeconomic measures showed a dose-response pattern with mortality after adjustment for age and sex (Figure). For example, compared with high-income patients (upper tertile) who had 13 years of education or more (reference category), the adjusted HRs (95% CIs) for death were 2.86 (1.40-5.84) for low-income (bottom tertile) patients with fewer than 12 years of education, 2.33 (1.19-4.57) for low-income patients with 13 years of education or more, 2.23 (1.01-4.95) for high-income patients not completing high school, and 2.12 (1.07-4.22) for average-income patients with 12 years of education.
FIGURE.
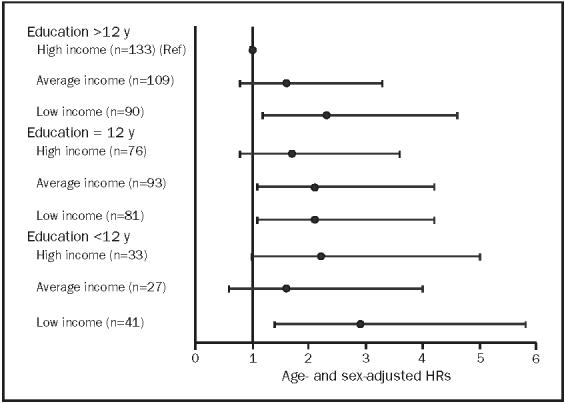
Age- and sex-adjusted hazard ratios (HRs) (95% confidence intervals) for mortality after myocardial infarction in mutually exclusive groups defined by income tertiles (census tract-derived) and education level. Ref = reference group.
Evaluated simultaneously, both neighborhood income for lowest vs highest tertile (HR, 2.10; 95% CI, 1.42-3.12) and individual education for 11 years or fewer vs 13 years or more (HR, 2.21; 95% CI, 1.47-3.32) were independently associated with mortality. After adjustment for age, sex, and race, these estimates were reduced by approximately half; further adjustment for comorbidity, cardiovascular risk factors, MI severity indicators, and medical treatment given during the index hospitalization accounted for most of the remaining effect of education but did not alter the association with neighborhood income appreciably (Table 3). Further adjustment for the time from symptom onset to hospital arrival and from presentation to percutaneous transluminal coronary angioplasty and coronary artery bypass grafting resulted in an HR of 1.66 (95% CI, 1.09-2.52) associated with the lowest vs highest income tertile. Additional analysis adjusting for the individual components of the Charlson index separately (rather than lumping components into categories) did not attenuate the income-mortality association for the lowest vs highest tertile (adjusted HR, 1.73; 95% CI, 1.13-2.65). Modeled as a continuous variable, the HRs (95% CIs) for death associated with each $10,000 increment in the annual neighborhood's median household income were 0.82 (0.75-0.90) before adjustment and 0.90 (0.82-0.99) after adjustment for demographics, education, comorbidity, cardiovascular risk factors, MI severity indicators, and medical treatment given during the index hospitalization. All possible 2-way interactions between age, sex, income, and education were examined, as well as the quadratic term of age. None reached statistical significance.
TABLE 3.
Association Between Death After Myocardial Infarction and Neighborhood Income and Individual Educationa
| Median household income tertiles |
Education categories |
|||||||
|---|---|---|---|---|---|---|---|---|
| Adjustment | First | Second | Thirdb | P value for trend | <12y | 12 y | >12yb | P value for trend |
| Income and education | 2.10 (1.42-3.12) | 1.33 (0.87-2.04) | 1 | <.001 | 2.21 (1.47-3.32) | 1.25 (0.87-1.81) | 1 | <.001 |
| Age, sex, and race added | 1.60 (1.07-2.40) | 1.21 (0.78-1.85) | 1 | .02 | 1.43 (0.94-2.17) | 1.21 (0.84-1.75) | 1 | .09 |
| Full modelc | 1.62 (1.08-2.45) | 1.10 (0.69-1.75) | 1 | .02 | 1.01 (0.65-1.56) | 0.92 (0.63-1.36) | 1 | .95 |
All data are presented as hazard ratio (95% confidence interval), unless otherwise indicated.
Reference value.
Adjusted for income and education, age, sex, race, comorbidity, ejection fraction, hypertension, hyperlipidemia, smoking, body mass index, STelevation myocardial infarction, coronary artery bypass grafting, percutaneous transluminal coronary angioplasty, statins, β-blockers, and aspirin.
DISCUSSION
Measures of SES are well-established determinants of overall health, quality of life, and life expectancy.33,34 However, because SES is a complex multidimensional construct, the mechanisms by which it affects health are still incompletely understood. Although SES has traditionally been treated as an intrinsic characteristic of individuals, contextual effects of SES on health are theoretically important. Indeed, growing evidence suggests that a person's health can be influenced by the socioeconomic characteristics of the neighborhood in which he or she lives, above and beyond that person's individual SES. This influence might be related to several factors, including the availability and accessibility of health services, infrastructure features (eg, recreational facilities, high-quality schools, stores selling healthy foods), prevailing attitudes toward health and health-related behavior (such as smoking, diet, and physical activity), stress, and degree of social support.4,6,9 Despite this, few health studies measure neighborhood features along with, rather than as proxies for, individual-level SES measures.3,4
With regard to cardiovascular disease, a few primary prevention studies have evaluated the combined effects on disease incidence of SES indicators measured at both individual and area levels. These studies generally found an increased risk associated with area-level SES measures, even after controlling for individual-level measures.7,35,36 However, to our knowledge, our study is the first to present such data for patients after MI.
Studies Using Individual-Level SES Measures
Several studies have examined the association between individual-level measures of SES and post-MI outcomes.13-16,20 Patients with low SES who were hospitalized with MI were generally observed to exhibit a worse clinical profile and receive inferior treatment. Nearly all studies have demonstrated increased risk associated with low SES. For example, Alter et al,14 studying 3407 patients with MI hospitalized in 53 hospitals in Canada, found a strong inverse relationship between income and 2-year mortality rate (HR, 0.45 for highest vs lowest tertile). However, the association was markedly attenuated after controlling for age, preexisting cardiovascular events, and risk factors (adjusted HR, 0.77). Similarly, in the Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy (PURSUIT) trial,13 low income was strongly associated with worse outcome in unadjusted analysis, but the association was reduced after adjustment (adjusted HR, 1.4 for low- vs high-income patients). Thus, although individual-level SES measures are associated with adverse outcome after MI, the extent to which this relationship is accounted for by differences in baseline characteristics and post-MI management remains uncertain.
Studies Using Area-Level SES Measures
Similar to findings on individual-level SES indicators, increasing evidence suggests that patients with MI living in low-SES neighborhoods are older, are more likely to be female, and have more cardiovascular risk factors and comorbidity. Yet, despite their higher risk, these patients are less likely to receive evidence-based medical therapies (ie, aspirin, statins, and β-blockers) or to be treated aggressively with invasive cardiac procedures.11,12,17,19,21,37,38 Further, previous studies uniformly revealed an association between low SES and mortality. For instance, Tonne et al11 studied the relationship of several area-level SES measures to mortality in 3423 community patients with MI from Worcester, MA. A 43% higher death rate was found among patients living in census tracts with the highest percentage of residents living below the poverty line, compared with the wealthiest tracts (top vs bottom quintile). Adjustment for demographic and clinical characteristics yielded a relative risk of 1.30 (95% CI, 1.08-1.56). Similar associations were observed for other SES measures. Alter et al,12 studying 51,591 patients with MI in Ontario, reported that for each $10,000 increase in the neighborhood median income, there was an approximately 10% reduction in the adjusted risk of death within 1 year. Associations of the same magnitude have been observed in other studies,17,19 including ours. Thus, data linking area-level SES measures to mortality after MI are consistent, although the estimated effects are generally modest relative to individual-level measures.
What This Study Adds
To the best of our knowledge, this study is the first to evaluate the combined effects of individual-level and area-level SES measures after MI. Moreover, although most previous studies were conducted in selected populations, our study reports on the comprehensive experience of community-dwelling persons, and so its findings can be generalized more readily.
Our findings of older age, female sex, excess comorbidity, and increased mortality associated with low SES are consistent with prior studies. However, unlike previous reports, our study found no strong evidence of treatment disparities related to SES, either for evidence-based medical therapies or for invasive cardiac procedures. This could be related to the fact that few patients were uninsured in this community, which is characterized by easy access to high-quality care.
Interestingly, despite the higher-than-average SES of this population, the associations of individual education and neighborhood income with death after MI were stronger than those reported in many previous studies. We think our approach of evaluating 2 different and complementary indicators of SES allowed us to capture a wider spectrum of this complex construct. As such, our results are commensurate with the double-jeopardy theory,9,10 whereby patients carrying multiple adverse SES characteristics are particularly vulnerable. Although the risk associated with education was markedly attenuated after controlling for multiple demographic and clinical variables, this attenuation could represent an overadjustment, because many of the variables adjusted for are likely to be intermediate factors on the education-mortality pathway.
Possible Mechanisms
The strong association shown between neighborhood income and death suggests a contextual effect. Alternatively, neighborhood income could merely act as a proxy for unmeasured dimensions of individual-level SES. We think both mechanisms are likely to have a role. The association observed for education could be related to its indirect positive effect on job opportunities, income, housing, access to nutritious foods, health insurance, and more. Higher levels of education could also directly affect health through greater knowledge acquired during schooling and greater empowerment and self-efficacy. As recently reported, education is strongly associated with health literacy, which in turn affects one's ability to obtain, process, and understand basic health information and services needed to make appropriate health decisions.39
More specific mechanisms linking low SES to worse MI prognosis could include its substantial adverse influences on functional recovery from MI,40 attendance at cardiac rehabilitation programs,20,41 and adherence to postdischarge medications and lifestyle recommendations.2,42
Potential Limitations
Several issues should be considered in the interpretation of these data. Our sample size is relatively modest, and although Olmsted County is becoming more diverse, the study population consists primarily of US whites. However, the mean census tract percentage of residents living below the poverty line in this cohort was 8%, which does not greatly differ from the US average of 12%. Further, it was previously shown that, even among populations with relatively high SES, the most advantaged have better health status than the less advantaged.6 Individual-level SES was assessed solely by education; consequently, the risk associated with neighborhood income might be overestimated because it could also have acted as a proxy for unmeasured individual socioeconomic characteristics.
CONCLUSION
In this community-based cohort of MI, low neighborhood income and lower levels of individual education were associated with a worse clinical presentation. Further, both measures showed a dose-response relationship with mortality. The association between low neighborhood income and increased mortality risk persisted even after controlling for a variety of potential confounders. These findings indicate the importance of SES in determining prognosis after MI.
Acknowledgments
This study was funded by grants from the Public Health Service and the National Institutes of Health (AR30582, R01 HL 59205, and R01 HL 72435). Dr Roger is an Established Investigator of the American Heart Association.
We are indebted to Ellen E. Koepsell, RN, and Susan Stotz, RN, for valuable assistance in study coordination and data collection.
Glossary
- CI
confidence interval
- HR
hazard ratio
- MI
myocardial infarction
- SES
socioeconomic status
REFERENCES
- 1.Weinblatt E, Ruberman W, Goldberg JD, Frank CW, Shapiro S, Chaudhary BS. Relation of education to sudden death after myocardial infarction. N Engl J Med. 1978;299(2):60–65. doi: 10.1056/NEJM197807132990202. [DOI] [PubMed] [Google Scholar]
- 2.Tofler GH, Muller JE, Stone PH, Davies G, Davis VG, Braunwald E. Multicenter Investigation of the Limitation of Infarct Size (MILIS). Comparison of long-term outcome after acute myocardial infarction in patients never graduated from high school with that in more educated patients. Am J Cardiol. 1993;71(12):1031–1035. doi: 10.1016/0002-9149(93)90568-w. [DOI] [PubMed] [Google Scholar]
- 3.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 4.Diez-Roux AV. Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am J Public Health. 1998;88(2):216–222. doi: 10.2105/ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lahelma E, Martikainen P, Laaksonen M, Aittomaki A. Pathways between socioeconomic determinants of health. J Epidemiol Community Health. 2004;58(4):327–332. doi: 10.1136/jech.2003.011148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 8.Anderson RT, Sorlie P, Backlund E, Johnson N, Kaplan GA. Mortality effects of community socioeconomic status. Epidemiology. 1997;8(1):42–47. doi: 10.1097/00001648-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 10.Shen JJ, Wan TT, Perlin JB. An exploration of the complex relationship of socioecologic factors in the treatment and outcomes of acute myocardial infarction in disadvantaged populations. Health Serv Res. 2001;36(4):711–732. [PMC free article] [PubMed] [Google Scholar]
- 11.Tonne C, Schwartz J, Mittleman M, Melly S, Suh H, Goldberg R. Long-term survival after acute myocardial infarction is lower in more deprived neighborhoods. Circulation. 2005 Jun 14;111(23):3063–3070. doi: 10.1161/CIRCULATIONAHA.104.496174. Epub 2005 Jun 6. [DOI] [PubMed] [Google Scholar]
- 12.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999;341(18):1359–1367. doi: 10.1056/NEJM199910283411806. [DOI] [PubMed] [Google Scholar]
- 13.Rao SV, Kaul P, Newby LK, et al. Poverty, process of care, and outcome in acute coronary syndromes. J Am Coll Cardiol. 2003;41(11):1948–1954. doi: 10.1016/s0735-1097(03)00402-9. [DOI] [PubMed] [Google Scholar]
- 14.Alter DA, Chong A, Austin PC, et al. Socioeconomic status and mortality after acute myocardial infarction. Ann Intern Med. 2006;144(2):82–93. doi: 10.7326/0003-4819-144-2-200601170-00005. [DOI] [PubMed] [Google Scholar]
- 15.Salomaa V, Miettinen H, Niemela M, et al. Relation of socioeconomic position to the case fatality, prognosis and treatment of myocardial infarction events: the FINMONICA MI Register Study. J Epidemiol Community Health. 2001;55(7):475–482. doi: 10.1136/jech.55.7.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasmussen JN, Rasmussen S, Gislason GH, et al. Mortality after acute myocardial infarction according to income and education. J Epidemiol Community Health. 2006;60(4):351–356. doi: 10.1136/jech.200X.040972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rao SV, Schulman KA, Curtis LH, Gersh BJ, Jollis JG. Socioeconomic status and outcome following acute myocardial infarction in elderly patients. Arch Intern Med. 2004;164(10):1128–1133. doi: 10.1001/archinte.164.10.1128. [DOI] [PubMed] [Google Scholar]
- 18.Lee JR, Paultre F, Mosca L. The association between educational level and risk of cardiovascular disease fatality among women with cardiovascular disease. Women's Health Issues. 2005;15(2):80–88. doi: 10.1016/j.whi.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 19.Chang WC, Kaul P, Westerhout CM, Graham MM, Armstrong PW. Effects of socioeconomic status on mortality after acute myocardial infarction. Am J Med. 2007;120(1):33–39. doi: 10.1016/j.amjmed.2006.05.056. [DOI] [PubMed] [Google Scholar]
- 20.Bernheim SM, Spertus JA, Reid KJ, et al. Socioeconomic disparities in outcomes after acute myocardial infarction. Am Heart J. 2007;153(2):313–319. doi: 10.1016/j.ahj.2006.10.037. [DOI] [PubMed] [Google Scholar]
- 21.Barakat K, Stevenson S, Wilkinson P, Suliman A, Ranjadayalan K, Timmis AD. Socioeconomic differentials in recurrent ischaemia and mortality after acute myocardial infarction. Heart. 2001;85(4):390–394. doi: 10.1136/heart.85.4.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steg PG, Lopez-Sendon J, Lopez de Sa E, et al. GRACE Investigators External validity of clinical trials in acute myocardial infarction. Arch Intern Med. 2007;167(1):68–73. doi: 10.1001/archinte.167.1.68. [DOI] [PubMed] [Google Scholar]
- 23.Tu JV, Willison DJ, Silver FL, et al. Investigators in the Registry of the Canadian Stroke Network. Impracticability of informed consent in the Registry of the Canadian Stroke Network. N Engl J Med. 2004;350(14):1414–1421. doi: 10.1056/NEJMsa031697. [DOI] [PubMed] [Google Scholar]
- 24.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71(3):266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 25.US Census Bureau. American FactFinder http://factfinder.census.gov/home/saff/main.html?_lang=en. Accessed March 20, 2008.
- 26.Roger VL, Killian JM, Weston SA, et al. Redefinition of myocardial infarction: prospective evaluation in the community. Circulation. 2006 Aug 22;114(8):790–797. doi: 10.1161/CIRCULATIONAHA.106.627505. Epub 2006 Aug 14. [DOI] [PubMed] [Google Scholar]
- 27.Apple FS, Wu AH, Jaffe AS. European Society of Cardiology and American College of Cardiology guidelines for redefinition of myocardial infarction: how to use existing assays clinically and for clinical trials. Am Heart J. 2002;144(6):981–986. doi: 10.1067/mhj.2002.124048. [DOI] [PubMed] [Google Scholar]
- 28.Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003 Nov 18;108(20):2543–2549. doi: 10.1161/01.CIR.0000100560.46946.EA. Epub 2003 Nov 10. [DOI] [PubMed] [Google Scholar]
- 29.Gerber Y, Jacobsen SJ, Killian JM, Weston SA, Roger VL. Participation bias assessment in a community-based study of myocardial infarction, 2002-2005. Mayo Clin Proc. 2007;82(8):933–938. doi: 10.4065/82.8.933. [DOI] [PubMed] [Google Scholar]
- 30.Geronimus AT, Bound J. Use of census-based aggregate variables to proxy for socioeconomic group: evidence from national samples. Am J Epidemiol. 1998;148(5):475–486. doi: 10.1093/oxfordjournals.aje.a009673. [DOI] [PubMed] [Google Scholar]
- 31.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 32.Gerber Y, Jacobsen SJ, Frye RL, Weston SA, Killian JM, Roger VL. Secular trends in deaths from cardiovascular diseases: a 25-year community study. Circulation. 2006 May 16;113(19):2285–2292. doi: 10.1161/CIRCULATIONAHA.105.590463. Epub 2006 May 8. [DOI] [PubMed] [Google Scholar]
- 33.Department of Health and Social Security . Inequalities in health: report of a research working group (The Black Report) DHSS; London, UK: 1980. [Google Scholar]
- 34.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993;329(2):103–109. doi: 10.1056/NEJM199307083290207. [published correction appears in N Engl J Med. 1993;329(15):1139] [DOI] [PubMed] [Google Scholar]
- 35.Stjarne MK, Fritzell J, De Leon AP, Hallqvist J, SHEEP Study Group Neighborhood socioeconomic context, individual income and myocardial infarction. Epidemiology. 2006;17(1):14–23. doi: 10.1097/01.ede.0000187178.51024.a7. [DOI] [PubMed] [Google Scholar]
- 36.Sundquist K, Winkleby M, Ahlen H, Johansson SE. Neighborhood socioeconomic environment and incidence of coronary heart disease: a follow-up study of 25,319 women and men in Sweden. Am J Epidemiol. 2004;159(7):655–662. doi: 10.1093/aje/kwh096. [DOI] [PubMed] [Google Scholar]
- 37.Philbin EF, McCullough PA, DiSalvo TG, Dec GW, Jenkins PL, Weaver WD. Socioeconomic status is an important determinant of the use of invasive procedures after acute myocardial infarction in New York State. Circulation. 2000;102(19)(suppl 3):III107–III115. doi: 10.1161/01.cir.102.suppl_3.iii-107. [DOI] [PubMed] [Google Scholar]
- 38.Rathore SS, Berger AK, Weinfurt KP, et al. Race, sex, poverty, and the medical treatment of acute myocardial infarction in the elderly. Circulation. 2000;102(6):642–648. doi: 10.1161/01.cir.102.6.642. [DOI] [PubMed] [Google Scholar]
- 39.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 40.Ickovics JR, Viscoli CM, Horwitz RI. Functional recovery after myocardial infarction in men: the independent effects of social class. Ann Intern Med. 1997;127(7):518–525. doi: 10.7326/0003-4819-127-7-199710010-00003. [DOI] [PubMed] [Google Scholar]
- 41.Melville MR, Packham C, Brown N, Weston C, Gray D. Cardiac rehabilitation: socially deprived patients are less likely to attend but patients ineligible for thrombolysis are less likely to be invited. Heart. 1999;82(3):373–377. doi: 10.1136/hrt.82.3.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ho PM, Spertus JA, Masoudi FA, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166(17):1842–1847. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]


