Abstract
BACKGROUND:
Treatments for hypertension and dyslipidemia to prevent the development of cardiovascular disease compete for the same finite number of health care dollars. Therefore, the potential benefits of treating Canadians without cardiovascular disease or diabetes who would currently be targeted by the national treatment guidelines were estimated and compared.
STUDY DESIGN:
Canadian Heart Health Surveys data were used to estimate the number of Canadians requiring intervention. The Cardiovascular Life Expectancy Model, a previously validated Markov model, was used to calculate the increased life expectancy and decreased morbidity associated with treating risk factors to target.
RESULTS:
Among 8.44 million adults 40 to 74 years of age without cardiovascular disease or diabetes, it was estimated that approximately 2.33 million would require treatment for dyslipidemia and 2.34 million for hypertension. The estimated Framingham 10-year coronary risk averaged 12.4% versus 9.6%, respectively. Treating dyslipidemia was associated with an average increased life expectancy of 1.67 years and 1.81 years of life free of cardiovascular disease. Treating hypertension was expected to increase life expectancy by 0.94 years and years of life free of cardiovascular disease by 1.29 years. The population benefits associated with treating dyslipidemia or hypertension would be 2.5 million and 1.4 million person years of life saved, respectively. Overall, the person years of treatment required to save one year of life was estimated to average 20 years for dyslipidemia therapy and 38 years for hypertension.
CONCLUSIONS:
The potential benefits associated with treating hypertension or dyslipidemia to prevent cardiovascular disease are substantial. However, compared with hypertension guidelines, dyslipidemia guidelines target higher-risk patients. Accordingly, given the relative efficacy of each treatment, the forecasted benefits associated with treating dyslipidemia are substantially greater than those associated with hypertension therapy.
Keywords: Hypertension, Lipids, Prevention
Abstract
HISTORIQUE :
Les traitements antihypertensifs ou hypolipidémiants qui visent à prévenir les maladies cardiovasculaires sont, comme toute autre mesure thérapeutique, en butte aux contraintes budgétaires qui prévalent en santé. C’est pourquoi les auteurs ont voulu évaluer et comparer les avantages potentiels du traitement prophylactique chez les Canadiens indemnes de maladie cardiovasculaire ou de diabète, mais néanmoins actuellement ciblés par les directives thérapeutiques nationales.
MODÈLE DE L’ÉTUDE :
Les données de l’Enquête canadienne sur la santé cardiovasculaire ont été utilisées pour estimer le nombre de Canadiens nécessitant une intervention. Le Cardiovascular Life Expectancy Model, un modèle de Markov déjà préalablement validé a été utilisé pour calculer l’augmentation de l’espérance de vie et la baisse de la morbidité pouvant découler d’une correction des facteurs de risque correspondant à des objectifs précis.
RÉSULTATS :
Parmi les 8,44 millions d’adultes de 40 à 74 ans indemnes de maladie cardiovasculaire ou de diabète, on estime qu’environ 2,33 millions auraient besoin d’un traitement pour dyslipidémie et 2,34 millions, d’un traitement pour hypertension. Le risque coronarien moyen à dix ans estimé selon la méthode de Framingham a été de 12,4 % et de 9,6 %, respectivement. Le traitement de la dyslipidémie a été associé à une augmentation moyenne de l’espérance de vie de 1,67 an et à 1,81 an de vie sans maladie cardiovasculaire. Le traitement de l’hypertension pour sa part permettrait une augmentation de l’espérance de vie de 0,94 an et 1,29 an sans maladie cardiovasculaire. Pour la population, les avantages d’un traitement hypolipidémiant ou antihypertensif correspondraient donc à 2,5 millions et 1,4 million d’années de vie-personnes sauvées, respectivement. Globalement, les années-personnes de traitement nécessaires pour sauver une année de vie ont été estimées à une moyenne de 20 ans pour le traitement de la dyslipidémie et de 38 ans pour l’hypertension.
CONCLUSIONS :
Les avantages potentiels associés au traitement antihypertensif ou hypolipidémiant dans le but de prévenir les maladies cardiovasculaires sont substantiels. Par contre, comparativement aux directives antihypertensives, les directives hypolipidémiantes ciblent des patients à risque plus élevé. Par conséquent, compte tenu de l’efficacité relative de chaque traitement, les avantages escomptés du traitement de la dyslipidémie sont substantiellement plus grands que les avantages attendus du traitement antihypertensif.
The clinical and economic burden of cardiovascular disease remains substantial among Canadians despite the continuing improvements in treatments for this disease (1). In addition, the disability associated with coronary artery disease and stroke among both men and women will continue to grow due to the aging population. The direct health care costs associated with treating cardiovascular disease are also a major concern and were estimated to be $6.8 billion in 1998 (2). Accordingly, the treatment of modifiable risk factors such as hypertension and dyslipidemia to prevent or delay the development of cardiovascular disease constitutes an essential component of contemporary public health policy and medical management (1,3,4).
The clinical indications for treating hypertension and dyslipidemia to prevent cardiovascular disease are expanding with the publication of new clinical trials that demonstrate therapeutic efficacy among previously untreated or undertreated patients. The expanding thresholds for initiating therapy and more aggressive treatment targets require greater numbers of asymptomatic adults to start therapy for hypertension or dyslipidemia. Therefore, the significant health care costs associated with treating these two conditions will demand a substantial portion of the national health care budget in the foreseeable future. In Canada, the pharmaceutical costs alone in 2004 were $1.98 billion for antihypertensives and diuretics, and $1.39 billion for lipid-lowering drugs (IMS Canada, personal communication).
The treatments for dyslipidemia and hypertension compete for the same increasingly constrained health care resources. We therefore estimated and compared the potential benefits associated with treating Canadians who would be targeted by the national treatment guidelines.
METHODS
The benefits associated with treating dyslipidemia and/or hypertension among Canadians free of cardiovascular disease and diabetes were estimated from population risk factor data collected by the Canadian Heart Health Surveys, current Canadian treatment guidelines and a previously published Markov model (the Cardiovascular Disease Life Expectancy Model) to calculate the increased life expectancy and decreased morbidity associated with treating risk factors to target (3–6). Finally, the proportion of individuals treated who could realistically reach the target was also estimated.
The Canadian Heart Health Surveys
The Canadian Heart Health Surveys represent the main findings of provincial population-based surveys completed between 1986 and 1992 (5). In each province, the sampling design included a stratified two-stage sampling procedure to provide representative data on both men and women between the ages of 18 and 74 years living in the community. At an initial home interview, a trained nurse elicited each participant’s general knowledge regarding cardiovascular disease risk factors. Also collected were data on sociodemographic characteristics, self-reported risk factors and smoking habits. Approximately two weeks following this interview, subjects were invited for a clinic visit, during which time a physical examination was performed, a fasting blood sample was drawn, anthropometric measurements were taken and blood pressure was assessed twice.
It was assumed that these data gathered between 1989 and 1991 continued to reflect the risk factor burden of Canadians in 2006. Data for men and women between the ages of 40 and 74 years attending the clinic visit were analyzed. Survey participants who reported having had a stroke, heart attack or diabetes were excluded from the analysis. Total plasma cholesterol (TC), high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C) levels were obtained from tests performed on the blood samples collected at the clinic visit. Systolic and diastolic blood pressures were taken as the average of the two clinical assessments made, and smoking status was determined from self-reported tobacco use. Subjects taking lipid or blood pressure medication were included in the analysis if they were not controlled to prescribed target levels. Among subjects identified for blood pressure intervention, 24.9% were already taking medication, and among subjects identified for lipid intervention, 6.7% were already taking medication.
Once a representative cohort had been assembled, the potential benefits of risk factor management were estimated for each participant based on that individual’s data. The population benefits were then extrapolated by weighing the data for each individual based on sampling weights assigned by the Canadian Heart Health Surveys.
The Cardiovascular Disease Life Expectancy Model
The Cardiovascular Disease Life Expectancy Model is a Markov model that estimates the annual probability of fatal and nonfatal cardiovascular disease events based on multivariate logistic regression equations developed based on a 15% random sample of the Lipid Research Clinic’s follow-up cohort (6,7). Independent risk factors include age, sex, mean blood pressure, LDL-C and HDL-C levels, cigarette smoking, diabetes and diagnosed cardiovascular disease at baseline.
In brief, a cohort of patients is entered into the model with specified levels of risk factors. Each year, a subject may die of coronary artery disease, cerebrovascular disease or other causes. The surviving subjects age one year and re-enter the model for the following year. The mean life expectancy is calculated by summing across the total person years of life experienced by the cohort and dividing by the subjects at risk on entry into the model. The results are expressed as years of life saved and years of life free of cardiovascular disease for the individual. Among the adult Canadian population, the benefits are summarized as person years of life saved and person years of treatment to save one year of life. Because the forecasted benefits occur at different times, these analyses were repeated after discounting future benefits by 3% annually.
The model has been previously described in detail and shown to reasonably estimate events in nine clinical trials of dyslipidemia or hypertension (6), a published analysis of diabetic subjects in the Scandinavian Simvastatin Survival Study (4S [8]) and a study on the life expectancy of American adults (9). The model was also validated by forecasting the life expectancy of adults at specific ages using risk factor data provided by the Canadian Heart Health Surveys (5). The resulting forecasted life expectancies were then compared with published Canadian life tables (10). The person years of treatment to save one year of life were derived by dividing the person years of treatment forecasted for each individual divided by the projected increased life expectancy. To adjust for the time preferences associated with treatment preceding the eventual reduction in cardiovascular events, both treatment years and life years gained were discounted 3% annually.
Guidelines for lipid treatment
The 2003 Canadian Working Group on Hypercholesterolemia and Other Dyslipidemias guidelines for the management of dyslipidemia recommended that target levels include an LDL-C level below 2.5 mmol/L and a TC/HDL-C ratio below 4 for people at high risk for cardiovascular disease (calculated 10-year Framingham risk of coronary artery disease of 20% or higher), an LDL-C level below 3.0 mmol/L and a TC/HDL-C ratio below 5 for people at moderate risk (calculated 10-year risk of 10% to 20%), and an LDL-C level below 4.0 mmol/L and a TC/HDL-C ratio below 6 for people at low risk (calculated 10-year risk of 10% or lower) (4).
The benefits of treating LDL-C levels and the TC/HDL-C ratio to these target levels among individuals in the Canadian Heart Health Surveys who would qualify for treatment were evaluated based on their baseline risk factors and calculated global cardiovascular risk. Cardiovascular disease risk was assessed using the Framingham global risk assessment equation recommended by both the American National Cholesterol Education Program (11) and the Canadian Working Group on Hypercholesterolemia and Other Dyslipidemias (4). It was assumed that only individuals with an LDL-C level above target by at least 0.5 mmol/L or a TC/HDL-C ratio above target by 0.5 would be treated.
Guidelines for hypertension management
In 2004, the Canadian Hypertension Education Program recommended a systolic blood pressure of 140 mmHg or lower and a diastolic blood pressure of 90 mmHg or lower (3). Among individuals with baseline blood pressure values above these targets, the benefits of treating blood pressure to these targets were evaluated. It was assumed that only individuals with systolic or diastolic blood pressure above target by at least 5 mmHg would be treated.
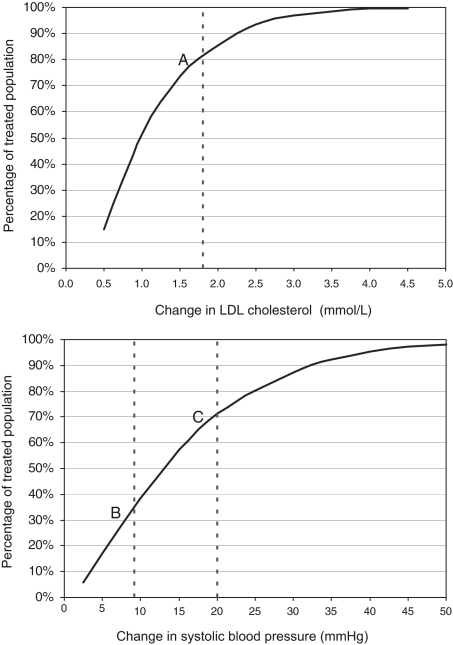
Estimating the likelihood of reaching treatment targets
Previous analyses by Law et al (12,13) suggested that the average reduction in LDL-C level achieved in clinical trials is 1.8 mmol/L and the average systolic blood pressure reduction achieved is 9.1 mmHg. The use of three antihypertensive drugs is associated with a 20 mmHg reduction in systolic blood pressure. These estimates were applied to the distribution of baseline levels of LDL-C and systolic blood pressures from the Canadian Heart Health Survey’s data to determine the proportion of patients who would reach treatment targets given the available therapy.
Role of study sponsor
The present investigator-initiated study was supported by a research grant from AstraZeneca Canada. The principal investigator had full control over the study design, data analysis and manuscript preparation.
RESULTS
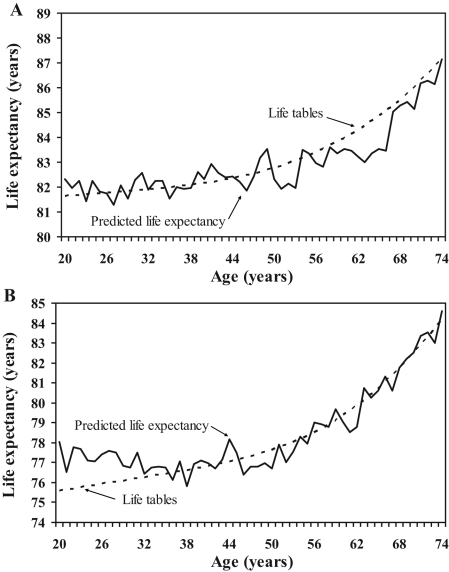
It was estimated that in 2006, there would be approximately 8.4 million adults 40 to 74 years of age without cardiovascular disease or diabetes if one assumes that the 1991 Canada Heart Health Surveys were still representative of the Canadian population. Population characteristics and cardiovascular risk factors are presented in Table 1. It was estimated that nearly 2.33 million individuals would require lipid treatment and 2.34 million would require blood pressure treatment. The cardiovascular life expectancy model was initially validated by comparing life expectancy forecasts for Canadians with those from published national life tables (10). The model forecasts based on risk factor data reasonably approximated from the life table estimates (Figure 1).
TABLE 1.
Canadian Heart Health Surveys population characteristics and cardiovascular disease risk factors among Canadians 40 to 74 years of age without cardiovascular disease or diabetes
| All | Eligible for lipid treatment | Eligible for BP management | |
|---|---|---|---|
| Sample size, n | 7189 | 2572 | 2424 |
| Population estimate (×103) | 8443 | 2333 | 2337 |
| Men, % | 47.5 | 67.5 | 52.8 |
| Age, years | 53.6 | 57.4 | 58.2 |
| Body mass index, kg/m2 | 26.3 | 27.3 | 27.7 |
| Current cigarette smoking, % | 20.0 | 28.2 | 15.5 |
| Systolic BP, mmHg | 128.6 | 134.4 | 149.3 |
| Diastolic BP, mmHg | 79.8 | 81.6 | 88.5 |
| Currently on hypertension medication, % | 11.5 | 16.9 | 24.9 |
| Total cholesterol, mmol/L | 5.5 | 6.4 | 5.7 |
| Low-density lipoprotein cholesterol, mmol/L | 3.4 | 4.3 | 3.6 |
| High-density lipoprotein cholesterol, mmol/L | 1.3 | 1.1 | 1.3 |
| Currently on lipid medication, % | 6.6 | 6.7 | 4.8 |
| 10-year Framingham risk, % | 6.05 | 12.42 | 9.55 |
BP Blood pressure
Figure 1).
Validation of the Cardiovascular Life Expectancy Model (6) against Canadian life tables (10). Representative age-specific risk factor data from the Canadian Heart Health Surveys (5) were entered into the model to forecast the life expectancy of Canadian women (A) and men (B) at each year of life. The results were compared with published life tables (10)
There would be substantially more women requiring blood pressure therapy than lipid therapy, and this was consistent across all age groups (Table 2). On the other hand, more men would require therapy for dyslipidemia than hypertension. The undiscounted and discounted (3% annually) increases in life expectancy associated with treating hypertension or dyslipidemia to target were estimated and are shown in Tables 3 and 4. Across all age groups, the average increase in life expectancy for both men and women would be greater after the treatment of dyslipidemia than of hypertension. The same holds true for the average increase in years of life free of cardiovascular disease. Overall, treating dyslipidemia was estimated to be associated with an average increased life expectancy of 1.67 years (0.86 years discounted) and with 1.81 years of life free of cardiovascular disease (1.14 years discounted). Meanwhile, the treatment of hypertension was expected to be associated with an average increase in life expectancy of 0.94 years (0.48 years discounted) and 1.29 years of life free of cardiovascular disease (0.80 years discounted).
TABLE 2.
Recommended treatments for Canadian adults 40 to 74 years of age without cardiovascular disease (CVD) or diabetes
| Sex | Age group, years | Population (×103) | Treatment recommended for | |
|---|---|---|---|---|
| Hyperlipidemia, % | Hypertension, % | |||
| Women | 40–49 | 1687 | 3.3 | 3.8 |
| 50–59 | 1299 | 6.8 | 17.4 | |
| 60–69 | 1041 | 15.2 | 32.1 | |
| 70–74 | 409 | 23.0 | 40.0 | |
| Total | 4435 | 8.9 | 17.8 | |
| Men | 40–49 | 1787 | 19.1 | 5.4 |
| 50–59 | 1118 | 25.5 | 17.5 | |
| 60–69 | 844 | 41.0 | 31.6 | |
| 70–74 | 258 | 50.2 | 36.5 | |
| Total | 4007 | 27.5 | 16.3 | |
| Overall | 8443 | 17.7 | 17.1 | |
TABLE 3.
Benefits of treating lipid levels to target among Canadians without cardiovascular disease (CVD) or diabetes
| Undiscounted | |||||
|---|---|---|---|---|---|
| Sex | Age group, years | Years of life saved | Years of life free of CVD | Total person years of life saved (×103) | Person years of treatment required to save one year of life |
| Women | 40–49 | 1.73 | 2.23 | 95 | 34 |
| 50–59 | 1.25 | 1.59 | 110 | 37 | |
| 60–69 | 1.09 | 1.40 | 172 | 27 | |
| 70–74 | 0.91 | 1.13 | 85 | 23 | |
| Total | 1.17 | 1.50 | 462 | 29 | |
| Men | 40–49 | 2.23 | 2.58 | 762 | 19 |
| 50–59 | 2.25 | 2.25 | 643 | 16 | |
| 60–69 | 1.40 | 1.33 | 485 | 17 | |
| 70–74 | 1.17 | 1.08 | 151 | 14 | |
| Total | 1.85 | 1.93 | 2042 | 17 | |
| Overall | 1.67 | 1.81 | 2504 | 20 | |
| Discounted | |||||
|---|---|---|---|---|---|
| Sex | Age group, years | Years of life saved | Years of life free of CVD | Total person years of life saved (×103) | Person years of treatment required to save one year of life |
| Women | 40–49 | 0.66 | 1.10 | 36 | 59 |
| 50–59 | 0.63 | 0.97 | 55 | 58 | |
| 60–69 | 0.62 | 0.96 | 98 | 37 | |
| 70–74 | 0.58 | 0.84 | 54 | 30 | |
| Total | 0.62 | 0.95 | 244 | 43 | |
| Men | 40–49 | 0.96 | 1.43 | 327 | 31 |
| 50–59 | 1.17 | 1.44 | 332 | 23 | |
| 60–69 | 0.83 | 0.93 | 287 | 22 | |
| 70–74 | 0.77 | 0.82 | 99 | 18 | |
| Total | 0.95 | 1.20 | 1046 | 25 | |
| Overall | 0.86 | 1.14 | 1289 | 29 | |
TABLE 4.
Lifetime benefits of treating blood pressure to target among Canadians without cardiovascular disease (CVD) or diabetes
| Undiscounted | |||||
|---|---|---|---|---|---|
| Sex | Age group, years | Years of life saved | Years of life free of CVD | Total person years of life saved (×103) | Person years of treatment required to save one year of life |
| Women | 40–49 | 1.01 | 1.76 | 65 | 56 |
| 50–59 | 1.02 | 1.79 | 230 | 42 | |
| 60–69 | 0.82 | 1.19 | 272 | 43 | |
| 70–74 | 0.69 | 1.04 | 113 | 39 | |
| Total | 0.86 | 1.38 | 681 | 43 | |
| Men | 40–49 | 1.46 | 1.95 | 141 | 32 |
| 50–59 | 1.25 | 1.43 | 244 | 32 | |
| 60–69 | 0.83 | 0.91 | 221 | 33 | |
| 70–74 | 0.68 | 0.68 | 64 | 28 | |
| Total | 1.02 | 1.19 | 669 | 32 | |
| Overall | 0.94 | 1.29 | 1350 | 38 | |
| Discounted | |||||
|---|---|---|---|---|---|
| Sex | Age group, years | Years of life saved | Years of life free of CVD | Total person years of life saved (×103) | Person years of treatment required to save one year of life |
| Women | 40–49 | 0.38 | 0.87 | 25 | 104 |
| 50–59 | 0.46 | 1.02 | 103 | 68 | |
| 60–69 | 0.45 | 0.80 | 149 | 61 | |
| 70–74 | 0.42 | 0.74 | 69 | 53 | |
| Total | 0.44 | 0.86 | 346 | 65 | |
| Men | 40–49 | 0.57 | 0.98 | 55 | 53 |
| 50–59 | 0.63 | 0.88 | 123 | 47 | |
| 60–69 | 0.48 | 0.63 | 129 | 45 | |
| 70–74 | 0.44 | 0.52 | 42 | 35 | |
| Total | 0.53 | 0.74 | 349 | 45 | |
| Overall | 0.48 | 0.80 | 695 | 56 | |
Overall, a similar number of Canadians were expected to require treatment for hypertension or dyslipidemia – 17.1% versus 17.7%, respectively. However, from a population perspective, the forecasted benefits of treating dyslipidemia were estimated to be greater than the benefits of treating hypertension. Treatment for dyslipidemia was associated with 2.5 million person years of life saved (1.3 million years discounted), compared with 1.4 million person years of life saved with the treatment of hypertension (695,000 years discounted). Accordingly, the person years of treatment required to save one year of life averaged 20 years for dyslipidemia therapy versus 38 years for hypertension therapy (29 years versus 56 years discounted, respectively).
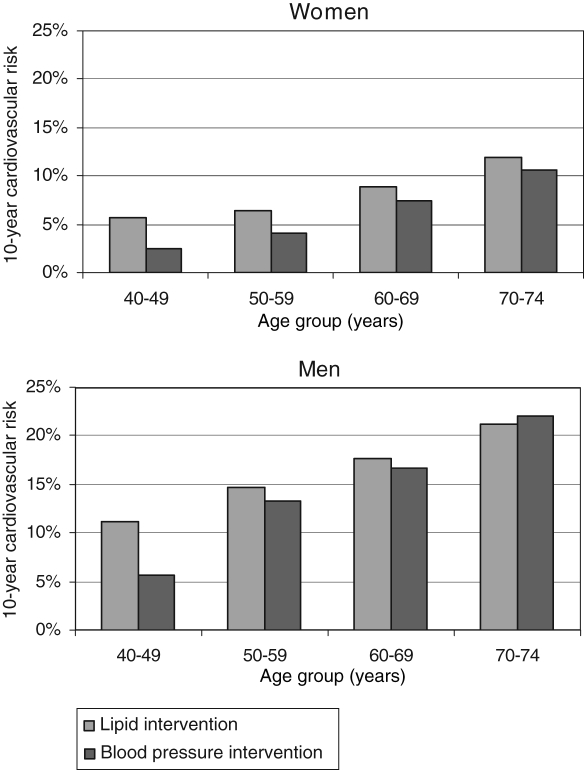
The greater forecasted benefits associated with treating dyslipidemia than hypertension are due to two main factors. In the model, there is a stronger association between cardiovascular events and blood lipids than blood pressure (6). This is particularly true for coronary artery disease, in which blood pressure is a relatively weak risk factor. The second issue is that current Canadian guidelines for dyslipidemia therapy target individuals at higher absolute risk than those who would be treated for hypertension (Figure 2). This holds true for all age groups except men 70 to 74 years of age; in this group, individuals targeted for hypertension are at slightly higher absolute risk (22.3% versus 23.3%).
Figure 2).
Average 10-year Framingham risk of coronary disease among Canadians free of diabetes and heart disease who require intervention for hypertension or dyslipidemia. Those requiring treatment for dyslipidemia have a higher risk than those requiring hypertension therapy (except men 70 to 74 years of age)
Finally, using the drug efficacy estimates provided by Law et al (12,13) and the Canadian Heart Health Surveys data, the proportions of the treated population who would achieve treatment targets are summarized in Figure 3. Approximately 90% of patients treated for dyslipidemia may potentially reach target with the currently available statins. On the other hand, slightly more than 40% of individuals would be expected to reach target with a single antihypertensive agent. Using three drugs that are associated with a 20 mmHg reduction in systolic pressure would result in approximately 80% of individuals reaching the target blood pressure (12).
Figure 3).
Distribution of the changes required to attain lipid level and blood pressure targets among Canadians selected for treatment based on the distribution of risk factors in the Canadian Heart Health Surveys. Given an average reduction in low-density lipoprotein (LDL) cholesterol of 1.8 mmol/L observed in clinical trials (13), approximately 90% of individuals will attain LDL cholesterol targets on currently available statins (point A). An average 9 mmHg reduction in systolic blood pressure observed in clinical trials (12) with monotherapy would result in approximately 40% of individuals reaching target (point B). Triple-drug therapy results in approximately 80% of individuals reaching target after a 20 mmHg drop in systolic blood pressure (point C) (12)
DISCUSSION
These analyses suggest that the potential benefits of treating hypertension or dyslipidemia among Canadian adults are substantial. It remains to be determined whether these potential benefits represent good value, given the substantial direct health care costs associated with treating these risk factors, against the cost savings of preventing cardiovascular events. The potential benefits associated with treating dyslipidemia appear to be greater than those associated with treating hypertension.
In the absence of a head-to-head comparison in a randomized clinical trial, these results must be considered with caution. The Canadian Heart Health Surveys are somewhat dated, and reflect the distribution of risk factors among Canadians between 1989 and 1991 (5). The presence of diabetes was based on participant self-reports; hence, some individuals included in our analysis probably had undetected diabetes. Accordingly, we have probably overestimated the number of individuals without diabetes who would be eligible for treatment. Nevertheless, we believe that the estimates presented in these analyses remained relevant in 2006. There are a number of potentially important factors that might have changed during this time, including the size and age of the population, as well as the distribution of risk factors. Comparing the most recent census data (14) from 2001 to five years earlier (1996), the total population grew from 29.6 million to 31.0 million adults (increase of 5% over five years), suggesting that the size of the treatable community might have grown as much as 15% over 15 years. Moreover, the growth of the population would have no effect on the age- and sex-specific results presented in Tables 2 to 4 other than on the total person years of life saved. Although the mean age of the population had increased, the analyses were restricted to those without diabetes or cardiovascular disease from 40 to 74 years of age, thereby minimizing this factor.
The most important issue is the possible change in risk factors among Canadians during the past 15 years. While there has not yet been an update of this national survey, we have recently completed a national study that reaffirmed that data collected in 2002 to 2003 are not much different from those collected in 1989 to 1991. The Canadian Study of Erectile Dysfunction (CANSED [15]) was a cross-sectional survey of Canadian men that identified cardiovascular risk factors associated with erectile dysfunction. Risk factor levels among nearly 3000 Canadian men screened from 2002 to 2003 were very similar to those of the 1989 to 1991 estimates summarized in Table 1.
Finally, it should be noted that the 1989 to 1991 Canadian Heart Health Surveys data capture risk factor levels primarily among untreated Canadians. This information is critical for estimating the baseline risk of cardiovascular events and the potential benefits of therapy. Given the increasing use of drugs for hypertension and dyslipidemia, a more current data set may provide a less accurate estimate of baseline risk before treatment.
These results are also influenced by the association between cardiovascular risk and blood lipids or blood pressure. The Cardiovascular Life Expectancy Model is based on data from the Lipid Research Clinic’s follow-up cohort, and the resulting multivariate equations assign a stronger risk to increases in LDL-C level than systolic or diastolic blood pressure (6). The same is true of the Framingham risk equations, in which the change in cardiovascular risk is greater with a one-unit change in TC or LDL-C level than in systolic or diastolic blood pressure (4). Using a similar methodology based on prospective cohort studies, Law et al (12) have estimated that hypertension monotherapy would reduce ischemic heart disease events by 19% and cerebrovascular events by 29%. If three antihypertensive drugs would be used, coronary events could drop by as much as 46%, along with 63% for cerebrovascular events. Similarly, Law et al (13) estimated that statin therapy would be associated with a 61% reduction in coronary events and a 17% reduction in stroke.
The event reduction actually observed in clinical trials also supports these results. To date, there have been three randomized trials of statins versus placebo in the prevention of cardiovascular events among individuals without known disease. Two primary prevention trials include the West Of Scotland COronary Prevention (WOSCOP) study (16) and the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS [17]). There was also a subgroup of patients without cardiovascular disease enrolled in the Anglo-Scandinavian Cardiac Outcomes Trial – Lipid Lowering Arm (ASCOT-LLA [18]). In these three trials, five years of statin therapy was associated with an RR reduction in major coronary events of approximately 30% to 35%. In the ASCOT-LLA study, the subgroup without previous vascular disease was also shown to benefit significantly, with approximately a 40% reduction in major coronary events.
The primary prevention of cardiovascular disease with antihypertensive therapy is less clearly documented. To date, there are three published clinical trials that evaluated antihypertensive drug use among individuals without baseline cardiovascular disease. Unfortunately, these studies were substantially smaller than the statin trials and may not have been adequately powered to demonstrate a benefit of antihypertensive therapy. In the Oslo study (19), it was found that five years of hypertension treatment among men 40 to 49 years of age without target organ damage but with systolic blood pressure between 150 mmHg and 179 mmHg and diastolic pressure below 110 mmHg was not associated with any major effect on cardiovascular morbidity. This was despite differences in blood pressure between treatment arms of 17 mmHg (systolic) and 10 mmHg (diastolic) over approximately five years. There were also seven strokes in the control group and none in the treatment group. However, despite the significant reduction in strokes, there were slightly more coronary events in the treatment arm, such that there was an even number of cardiovascular events in both arms of the study.
Two other small studies also demonstrated no benefits of antihypertensive therapy among individuals without cardiovascular disease at baseline. This included the Veterans Administration-National Heart, Lung, and Blood Institute (VA-NHLBI) study, in which approximately 1000 individuals were randomly assigned (20). Only 13 coronary events occurred overall, and no strokes were observed. The US Public Health Services Hospitals Cooperative Study Group (21) also published the results of a 10-year intervention trial with fewer than 400 patients enrolled. Again, there were few outcomes and no observed benefits of therapy. Nonetheless, among individuals with a sufficiently high absolute risk of future cardiovascular events, it was estimated that antihypertensive therapy would be beneficial. Mulrow et al (22) completed an overview analysis of 13 trials involving elderly persons (60 years of age and older) and found that antihypertensive therapy resulted in approximately a 20% risk reduction in coronary events and a 30% reduction in cerebrovascular events. Similar results were observed among younger and middle-aged adults. However, the authors noted that given the lower absolute risk of events among younger subjects versus older subjects, two to four times as many will need to be treated to observe a reduction in cardiovascular events. While most of these studies included individuals with previous cardiovascular events or diabetes, the actual prevalence of these conditions was less than 5% across all studies. Accordingly, one can probably generalize these results to primary prevention, recognizing that the absolute benefits of blood pressure therapy would probably be lower in primary prevention.
Current Canadian guidelines for dyslipidemia focus primarily on absolute cardiovascular risk. On the other hand, current Canadian hypertension guidelines, while advocating global risk assessment, do not specify that treatment be initiated only when a critical threshold of absolute risk has been reached. Accordingly, one of the reasons that the benefits of lipid therapy are projected to be greater than hypertension therapy is the substantially higher absolute risk of these patients (Table 1). Specifically, the average 10-year cardiovascular risk for those eligible for lipid therapy would be 12.4%, compared with 9.6% for those eligible for blood pressure therapy.
It must be recognized that these analyses depend on a number of critical assumptions, one of which is that all patients will reach the currently recommended treatment targets. A number of recent studies (23–30) have clearly demonstrated that this is often not the case. Physicians often do not treat to target, and many patients are often not 100% compliant with their prescribed medications. Accordingly, these results represented the maximum possible benefits and therefore overestimated the benefits that would actually be achieved in real life. It is therefore reasonable to ask whether the risk factor modification used in these analyses is achievable with currently available treatments. As summarized in Figure 3, when the relative efficacy of specific treatments are considered against the changes required to reach targets, Canadian patients are more likely to reach lipid targets than the blood pressure targets.
CONCLUSION
If Canadian adults were to follow current treatment guidelines, the potential benefits of treating hypertension or dyslipidemia would be substantial in reducing the burden of cardiovascular disease. However, given the current treatment guidelines, the estimated average benefits of treating dyslipidemia are approximately two times greater than those associated with treating hypertension. The population benefits would also be approximately 50% greater following the treatment of dyslipidemia than the treatment of hypertension. Increasing the effectiveness of hypertension therapy will require greater attention to the absolute risk of the individuals recommended for treatment and to multidrug therapy to ensure that treatment targets are achievable.
REFERENCES
- 1.Heart and Stroke Foundation of Canada The Growing Burden of Heart Disease and Stroke in Canada, 2003Heart and Stroke Foundation of Canada, 2003. <www.cvdinfobase.ca/cvdbook> (Version current at March 19, 2007).
- 2.Health Canada. Economic burden of illness in Canada 1998Health Canada Publications, 2002<www.phac-aspc.gc.ca/publicat/ebic-femc98/pdf/ebic1998.pdf> (Version current at March 19, 2007).
- 3.Khan NA, McAlister FA, Campbell NRC, et al. Canadian Hypertension Education Program The 2004 Canadian recommendations for the management of hypertension: Part II –therapy. Can J Cardiol. 2004;20:41–54. [Google Scholar]
- 4.Genest J, Frohlich J, Fodor G, McPherson R, Working Group on Hypercholesterolemia and Other Dyslipidemias Recommendations for the management of dyslipidemia and the prevention of cardiovascular disease: Summary of the 2003 update CMAJ 2003169921–4.(Erratum in 2003;169:1149). [PMC free article] [PubMed] [Google Scholar]
- 5.MacLean DR, Petrasovits A, Nargundkar M, et al. Canadian Heart Health Surveys: A profile of cardiovascular risk. Survey methods and data analysis. Canadian Heart Health Surveys Research Group. CMAJ. 1992;146:1969–74. [PMC free article] [PubMed] [Google Scholar]
- 6.Grover SA, Paquet S, Levinton C, Coupal L, Zowall H.Estimating the benefits of modifying risk factors of cardiovascular disease: A comparison of primary vs secondary prevention Arch Intern Med 1998158655–62.(Erratum in 1998;158:1228). [DOI] [PubMed] [Google Scholar]
- 7.Heiss G, Tamir I, Davis CE, et al. Lipoprotein-cholesterol distributions in selected North American populations: The Lipid Research Clinics Program prevalence study. Circulation. 1980;61:302–15. doi: 10.1161/01.cir.61.2.302. [DOI] [PubMed] [Google Scholar]
- 8.Grover SA, Coupal L, Zowall H, Dorais M. Cost-effectiveness of treating hyperlipidemia in the presence of diabetes: Who should be treated? Circulation. 2000;102:722–7. doi: 10.1161/01.cir.102.7.722. [DOI] [PubMed] [Google Scholar]
- 9.Grover SA, Coupal L, Gilmore N, Mukherjee J. Impact of dyslipidemia associated with Highly Active Antiretroviral Therapy (HAART) on cardiovascular risk and life expectancy. Am J Cardiol. 2005;95:586–91. doi: 10.1016/j.amjcard.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Statistics Canada Life tables: Canada, Provinces and Territories 1995–1997. [84-537-XIE] Ottawa: Statistics Canada; 2002. <www.statcan.ca:8096/bsolc/english/bsolc?catno=84-537-X> (Version current at March 19, 2007). [Google Scholar]
- 11.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 12.Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: Analysis of 354 randomised trials. BMJ. 2003;326:1427–34. doi: 10.1136/bmj.326.7404.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: Systematic review and meta-analysis. BMJ. 2003;326:1423–7. doi: 10.1136/bmj.326.7404.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Statistics Canada. Population and growth components (1851–2001 censuses) Statistics Canada 2005. <www40.statcan.ca/l01/cst01/defdemo03.htm> (Version current at March 19, 2007).
- 15.Grover SA, Lowensteyn I, Kaouache M, et al. The prevalence of erectile dysfunction in the primary care setting: Importance of risk factors for diabetes and vascular disease. Arch Intern Med. 2006;166:213–9. doi: 10.1001/archinte.166.2.213. [DOI] [PubMed] [Google Scholar]
- 16.Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1990;323:1301–7. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 17.Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: Results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–22. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 18.Sever PS, Dahlof B, Poulter NR, et al. ASCOT investigators Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial – Lipid Lowering Arm (ASCOT-LLA): A multicentre randomised controlled trial. Lancet. 2003;361:1149–58. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 19.Helgeland A. Treatment of mild hypertension: A five year controlled drug trial. The Oslo study. Am J Med. 1980;69:725–32. doi: 10.1016/0002-9343(80)90438-6. [DOI] [PubMed] [Google Scholar]
- 20.Evaluation of drug treatment in mild hypertension: VA-NHLBI feasibility trial Plan and preliminary results of a two-year feasibility trial for a multicenter intervention study to evaluate the benefits versus the disadvantages of treating mild hypertension. Prepared for the Veterans Administration-National Heart, Lung, and Blood Institute Study Group for Evaluating Treatment in Mild Hypertension. Ann NY Acad Sci. 1978;304:267–92. doi: 10.1111/j.1749-6632.1978.tb25604.x. [DOI] [PubMed] [Google Scholar]
- 21.Smith WM. Treatment of mild hypertension: Results of a ten-year intervention trial. Circ Res. 1977;40(Suppl 1):I98–105. [PubMed] [Google Scholar]
- 22.Mulrow CD, Cornell JA, Herrera CR, Kadri A, Farnett L, Aguilar C. Hypertension in the elderly. Implications and generalizability of randomized trials. JAMA. 1994;272:1932–8. [PubMed] [Google Scholar]
- 23.Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–63. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 24.Nieto FJ, Alonso J, Chambless LE, et al. Population awareness and control of hypertension and hypercholesterolemia. The Atherosclerosis Risk in Communities study. Arch Intern Med. 1995;155:677–84. [PubMed] [Google Scholar]
- 25.Caro JJ, Speckman JL, Salas M, Raggio G, Jackson JD. Effect of initial drug choice on persistence with antihypertensive therapy: The importance of actual practice data. CMAJ. 1999;160:41–6. [PMC free article] [PubMed] [Google Scholar]
- 26.Stephenson J. Noncompliance may cause half of antihypertensive drug “failures”. JAMA. 1999;282:313–4. doi: 10.1001/jama.282.4.313. [DOI] [PubMed] [Google Scholar]
- 27.Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP): A multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–67. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 28.Schrott HG, Bittner V, Vittinghoff E, Herrington DM, Hulley S. Adherence to National Cholesterol Education Program Treatment goals in postmenopausal women with heart disease. The Heart and Estrogen/Progestin Replacement Study (HERS). The HERS Research Group. JAMA. 1997;277:1281–6. [PubMed] [Google Scholar]
- 29.Schectman G, Hiatt J. Drug therapy for hypercholesterolemia in patients with cardiovascular disease: Factors limiting achievement of lipid goals. Am J Med. 1996;100:197–204. doi: 10.1016/s0002-9343(97)89459-4. [DOI] [PubMed] [Google Scholar]
- 30.McBride P, Schrott HG, Plane MB, Underbakke G, Brown RL. Primary care practice adherence to National Cholesterol Education Program guidelines for patients with coronary heart disease. Arch Intern Med. 1998;158:1238–44. doi: 10.1001/archinte.158.11.1238. [DOI] [PubMed] [Google Scholar]