Abstract
Purpose
To evaluate two clinical procedures, MEM and Nott retinoscopy, for detecting accommodative lags 1.00 diopter (D) or greater in children as identified by an open-field autorefractor.
Methods
168 children 8 to <12 years old with low myopia, normal visual acuity, and no strabismus participated as part of an ancillary study within the screening process for a randomized trial. Accommodative response to a 3.00 D demand was first assessed by MEM and Nott retinoscopy, viewing binocularly with spherocylindrical refractive error corrected, with testing order randomized and each performed by a different masked examiner. The response was then determined viewing monocularly with spherical equivalent refractive error corrected, using an open-field autorefractor, which was the gold standard used for eligibility for the clinical trial. Sensitivity and specificity for accommodative lags of 1.00 D or more were calculated for each retinoscopy method compared to the autorefractor.
Results
116 (69%) of the 168 children had accommodative lag of 1.00 D or more by autorefraction. MEM identified 66 children identified by autorefraction for a sensitivity of 57% (95% CI = 47% to 66%) and a specificity of 63% (95% CI = 49% to 76%). Nott retinoscopy identified 35 children for a sensitivity of 30% (95% CI = 22% to 39%) and a specificity of 81% (95% CI = 67% to 90%). Analysis of receiver operating characteristic (ROC) curves constructed for MEM and for Nott retinoscopy failed to reveal alternate cut points that would improve the combination of sensitivity and specificity for identifying accommodative lag ≥ 1.00 D as defined by autorefraction.
Conclusions
Neither MEM nor Nott retinoscopy provided adequate sensitivity and specificity to identify myopic children with accommodative lag ≥ 1.00 D as determined by autorefraction. A variety of methodological differences between the techniques may contribute to the modest to poor agreement.
The accommodative response of an individual who is not presbyopic is typically less than the demand if the stimulus to accommodation exceeds about 1.00 diopter (D).1, 2 When the accommodative response is less than the demand, the point of focus lies behind the point of fixation and a lag of accommodation is present.1 The lag of accommodation typically increases with increasing demand2 and has been reported to vary with refractive error.3-6
Some recent studies7-9 suggest that lag of accommodation may play a role in myopic progression. In the Correction of Myopia Evaluation Trial (COMET), the three year adjusted myopic progression as determined by cycloplegic autorefraction was 0.20 D less in 229 children randomly assigned to progressive addition lenses (PALs) compared to 233 children randomly assigned to single vision lenses (SVLs).8 The COMET study also found that PALs slowed the three-year adjusted progression of myopia by 0.64 ± 0.21 D more than SVLs in a subgroup of 76 children with large accommodative lags (determined by an open-field autorefractor) and near esophoria.9 This finding led to the development of the COMET2 study, a prospective, multicenter, double-masked randomized, treatment trial to compare the effect of PALs to SVLs on myopic progression in children with these characteristics. Eligibility for the COMET2 study was limited to children 8 to <12 years of age with low myopia, esophoria at near, and a lag of accommodation of at least 1.00 D for a 3.00 D demand as determined by the Grand Seiko autorefractor (WR-5100K, Japan), an open-field autorefractor.
Open-field autorefraction which allow specific accommodative demands to be created through the placement of real targets in free space is commonly used as a standardized, objective method of measuring accommodation in research studies.9-12 In clinical situations, however, few eye care practices have open-field autorefractors. Thus, to identify children with large accommodative lags in a typical clinical situation, it is important to have simple, reliable and inexpensive alternative methods.
The current study compares two clinical methods for measuring the accommodative response, the monocular estimate method (MEM) retinoscopy1 and Nott retinoscopy,13 with an open-field autorefractor. In MEM retinoscopy the patient binocularly fixates a target in the plane of the retinoscope positioned at the near reading distance. The examiner observes the retinoscopic reflex and briefly introduces spherical lenses in front of one of the patient's eyes until the first neutral reflex is observed. In Nott retinoscopy the patient binocularly fixates a target positioned at the specified near distance. The examiner is positioned at the target location and moves with the retinoscope (while the fixation target remains stationary) until a neutral reflex is observed and the retinoscope is conjugate with the point of focus on the retina. The primary aim of the current study is to determine how well MEM and Nott retinoscopy detect accommodative lags of 1.00 D or greater in myopic children as identified by an open-field of view autorefractor, the gold standard for the current study.
Methods
This study was supported by a cooperative agreement with the National Eye Institute of the National Institutes of Health and conducted by the Correction of Myopia Evaluation Trial 2 (COMET2) Study Group for the Pediatric Eye Disease Investigator Group (PEDIG) at 8 community- and university-based clinical sites and private colleges of optometry. The respective institutional review boards (IRBs) approved the protocol and HIPAA-compliant informed consent forms. The parent or guardian of each child gave written informed consent and the child gave written assent for this ancillary study as part of the informed consent for screening for the randomized trial.
The study was conducted as an ancillary study within the screening process for a randomized trial comparing the effect of PALs to SVLs on myopic progression in children with low myopia, large accommodative lags and near esophoria. The major eligibility criteria for the ancillary study included age 8 to <12 years; best-corrected visual acuity of 20/20 or better in each eye; no strabismus; no current or prior use of PALs, bifocals, or contact lenses; refractive error determined by subjective refraction without cycloplegia of -0.50 to -3.00 D spherical equivalent in each eye; no more than 1.50 D of astigmatism in each eye; and no more than 1.00 D spherical equivalent of anisometropia. Children who met these criteria were eligible to participate in the ancillary study and did not need to meet the other eligibility criteria for the randomized trial. Because two different examiners were needed for this ancillary study, eligible children could participate only when two examiners were available at the clinical site.
Medical and ocular history and previous spectacle wear were noted. Subjective refraction was determined and the near phoria (at 33 cm) was measured by the alternate cover test with prism neutralization through the subjective refraction. At a single visit, the accommodative response of the right eye was measured by two different dynamic retinoscopy methods, MEM and Nott retinoscopy, and by autorefraction (Grand Seiko WR-5100K, Japan). The two retinoscopy methods were performed prior to autorefraction, with the order of MEM and Nott retinoscopy determined by random assignment. MEM and Nott retinoscopy were each performed by a different certified examiner, with the second examiner masked to the initial examiner's results. Three measurements were taken by MEM retinoscopy and by Nott retinoscopy and five measurements were then taken by autorefraction (by any certified examiner).
Accommodation Testing Procedures
To emulate clinical practice, the accommodative target for the two retinoscopy methods was the grade 6 Welch Allyn card (Welch Allyn 18250 Fixation Cards, Skaneateles Falls, NY) consisting of words arranged around a center hole that allowed for the retinoscope beam and the examiner to be either on or very close to the child's visual axis. During the retinoscopy procedures the children either read the words on the card out loud, or called out the letters in the words if the words were beyond their reading level.
MEM retinoscopy was performed under moderate room illumination with the child seated 33 cm from the retinoscope with the Welch Allyn fixation card attached to the head of the retinoscope. This test distance was held constant using a 33 cm string attached to the retinoscope. The examiner assessed the motion in the horizontal meridian in the right eye as the child read the words on the Welch Allyn fixation card through the subjective refraction placed in a trial frame. The examiner introduced a lens estimated to neutralize the perceived motion. The examiner quickly estimated the result without leaving the lens in place long enough to interfere with the child's binocular vision or for the child's accommodative response to change. The examiner continued to try lenses (in 0.25 D steps) until the lowest power lens that resulted in neutrality was determined and this lens was recorded. If there was no lens that created neutrality (e.g., +0.50 D lens showed ‘with’ motion, +0.75 D lens showed ‘against’ motion), the average of the two lenses was recorded. The lens power or the interpolated power that achieved neutrality is the lag of accommodation if positive or the lead of accommodation if negative.
Nott retinoscopy was performed with the child seated 33 cm from the Welch Allyn fixation card positioned in front of the child's right eye and held in place by a near point rod extending from a phoropter rotated 90 degrees from the child's face plane. The child viewed the card binocularly under moderate room illumination through his or her subjective refraction placed in a trial frame. The examiner, initially positioned just behind the stationary word card and aligned with the hole in the card and the child's right eye, neutralized the retinoscopic reflex in the horizontal meridian by varying his/her distance from the child. The distance of the examiner from the stationary card to the point at which neutrality was observed was recorded along with whether the point of neutrality was behind or in front of the card. The total distance from the child's right eye to the point of neutrality was then calculated in centimeters and converted to diopters (100 divided by the number of centimeters) to yield the accommodative response. When the accommodative response was subtracted from the 3.00 D accommodative demand, a positive value indicated a lag of accommodation while a negative value indicated a lead of accommodation.
The Grand Seiko autorefractor was used to measure accommodation of the child's right eye in response to a self-illuminated row of 20/100 letters positioned 33 cm from the child. The left eye was occluded and measurements were made with the room lights off. To reduce reflections from multiple lenses, the child's right eye viewed the target through the spherical equivalent of the subjective refraction placed in a trial frame. The child was instructed to look at the central letter and to keep it clear. Using the joystick to maintain focus of the corneal reflections on the monitor, the examiner took the accommodation measurements. The sign of the spherical equivalent accommodation reading was changed (plus to minus or minus to plus) to yield the accommodative response, which when subtracted from the 3.00 D demand yielded the accommodative lag if positive or the accommodative lead if negative.
Statistical Analysis
The accommodative lag/lead measurements used for analysis were the median value from the three trials of MEM retinoscopy, the median value calculated from the three trials of Nott retinoscopy, and the median value calculated from the five spherical equivalent measures of accommodative response by autorefraction.
Based on the accommodative lag/lead calculated from the gold standard autorefraction, a classification was made as to whether the subject had an accommodative lag of 1.00 D or more for the 3.00 D demand. Using this same 1.00 D cut point for the two retinoscopy techniques, the sensitivity and specificity for each retinoscopy technique was calculated. In addition, for each retinoscopy method, receiver operating characteristic (ROC) curves were constructed to evaluate the sensitivity and specificity of other cut points for determining an accommodative lag of 1.00 D or more as defined by autorefraction. The area under the ROC curve was calculated as a measure of each retinoscopy method's overall accuracy for differentiating subjects with accommodative lag ≥ 1.00 D from those with accommodative lags less than 1.00 D. For the optimum cut point for each retinoscopy method, point estimates for sensitivity and specificity and 95% confidence intervals (CI) were calculated.
As an exploratory analysis, the difference between the lag/lead of accommodation obtained by each retinoscopy method and that derived from the autorefraction measurements was assessed for each subject. Linear regression was used to evaluate whether the difference between the amount of accommodative lag/lead based on the dynamic retinoscopy method and on autorefraction was associated with the average of the two measurements.
An additional exploratory analysis used linear regression to determine whether the difference between the amount of accommodative lag/lead obtained by the two dynamic retinoscopy methods was associated with the average of the lag/lead by MEM and Nott retinoscopy and/or the amount of accommodative lag as derived from autorefraction.
All reported P values are two-tailed. Analyses were conducted using SAS version 9.1 (SAS Institute, Cary, NC).
Results
Between May 2005 and March 2007, 168 children with a mean age of 10.0 ± 1.1 years participated in this study. Fifty-seven percent of the children were female and 49% were white. At near (33 cm), esophoria >1 prism diopter (PD) was present in 70% of children, exophoria > 1 PD in 21%, and orthophoria in 10%. Additional characteristics of the children are included in Table 1.
Table 1. Characteristics of the Cohort (N=168).
| N (%) | |
|---|---|
|
| |
| Gender: Female | 96 (57) |
|
| |
| Race / Ethnicity | |
| White | 82 (49) |
| African-American | 16 (10) |
| Hispanic or Latino | 47 (28) |
| Other* | 23 (14) |
|
| |
| Age, years | |
| Mean (SD) | 10.0 (1.1) |
| Range | 8.0 to 12.0 |
| 8-<9 | 35 (21) |
| 9-<10 | 50 (30) |
| 10-<11 | 43 (26) |
| 11-<12 | 40 (24) |
|
| |
| Refractive error, spherical equivalent** | |
| Mean (SD) | -1.67 (0.63) |
| Range | -0.50 to -3.00 |
| -0.50 to -1.00 D | 34 (20) |
| -1.01 to −1.50 D | 51 (30) |
| -1.51 to −2.00 D | 34 (20) |
| -2.01 to −2.50 D | 34 (20) |
| -2.51 to −3.00 D | 15 (9) |
|
| |
| Spectacle wear (SVLs) | |
| Currently | 125 (74) |
| In the past but not currently | 3 (2) |
| Never | 40 (24) |
|
| |
| Near phoria | |
| Esophoria | 117 (70) |
| 2 to <5 PD | 47 (40) |
| 5 to <10 PD | 56 (48) |
| 10 to <15 PD | 9 (8) |
| >=15 PD | 5 (4) |
| Orthophoria (1 PD esophoria to 1 PD exophoria) | 16 (10) |
| Exophoria | 35 (21) |
| 2 to <5 PD | 23 (66) |
| 5 to <10 PD | 9 (26) |
| 10 to <15 PD | 2 (6) |
| >=15 PD | 1 (3) |
16 patients were Asian, 5 were of more than one race, and 2 had unknown race.
Right eye refractive error as assessed by subjective refraction.
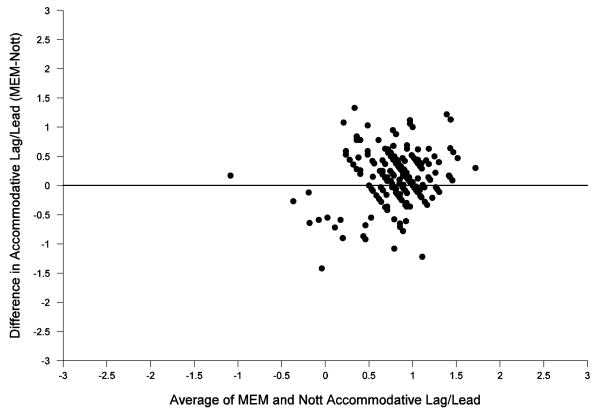
Comparison of MEM and Nott Retinoscopy to Autorefraction
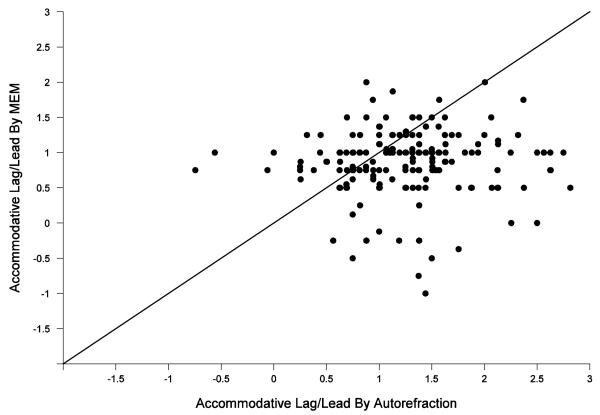
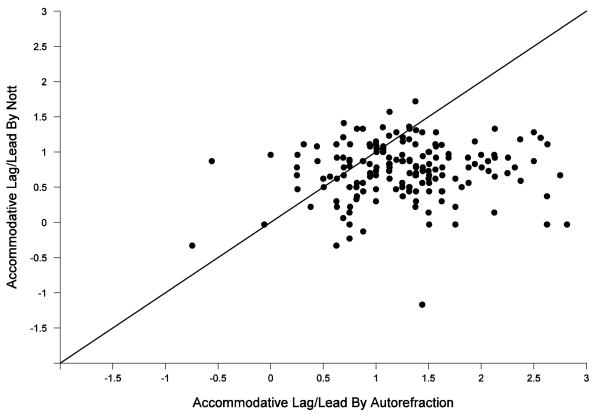
The distribution of accommodative lag/lead as measured by the three different techniques is shown in Table 2. Accommodative lag/lead by Grand Seiko autorefraction ranged from a lead of -0.75 D to a lag of 2.82 D with a median lag of 1.26 D compared with a median lag of 1.00 D (range -1.00 D to 2.00 D) measured by MEM retinoscopy and a median lag of 0.78 D (range -1.17 D to 1.72 D) by Nott retinoscopy. The mean difference between the accommodative lag determined by MEM retinoscopy and autorefraction was 0.40 D ± 0.76 D; the mean difference between the accommodative lag determined by Nott retinoscopy and autorefraction was 0.52 D ± 0.70 D. Eighty six (51%) of the MEM retinoscopy values fell within 0.50 D of autorefraction values and 77 (46%) of the Nott retinoscopy values fell within 0.50 D of autorefraction values (not shown in Table 2 but may be extrapolated from Figure 1).
Table 2. Accommodative Lag/Lead (N=168).
| Grand Seiko Autorefraction | MEM Retinoscopy | Nott Retinoscopy | |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
|
| |||
| Accommodative Lag/Lead, in diopters* | |||
| Median | 1.26 | 1.00 | 0.78 |
| Mean (SD) | 1.26 (0.61) | 0.86 (0.48) | 0.74 (0.41) |
| Range | -0.75 to 2.82 | -1.00 to 2.00 | -1.17 to 1.72 |
| -1.50 to <-1.00 D | 0 (0) | 0 (0) | 1 (<1) |
| -1.00 to <-0.50 D | 2 (1) | 2 (1) | 0 (0) |
| -0.50 to <0.00 D | 1 (<1) | 8 (5) | 10 (6) |
| 0.00 to <0.50 D | 9 (5) | 5 (3) | 26 (15) |
| 0.50 to <1.00 D | 40 (24) | 68 (40) | 86 (51) |
| 1.00 to <1.50 D | 61 (36) | 70 (42) | 43 (26) |
| 1.50 to <2.00 D | 33 (20) | 13 (8) | 2 (1) |
| 2.00 to <2.50 D | 14 (8) | 2 (1) | 0 (0) |
| 2.50 to <3.00 D | 8 (5) | 0 (0) | 0 (0) |
Accommodative lag/lead for a 33 cm target (i.e. 3.00 diopter demand). Negative values indicate accommodative lead; positive values indicate accommodative lag.
Figure 1.
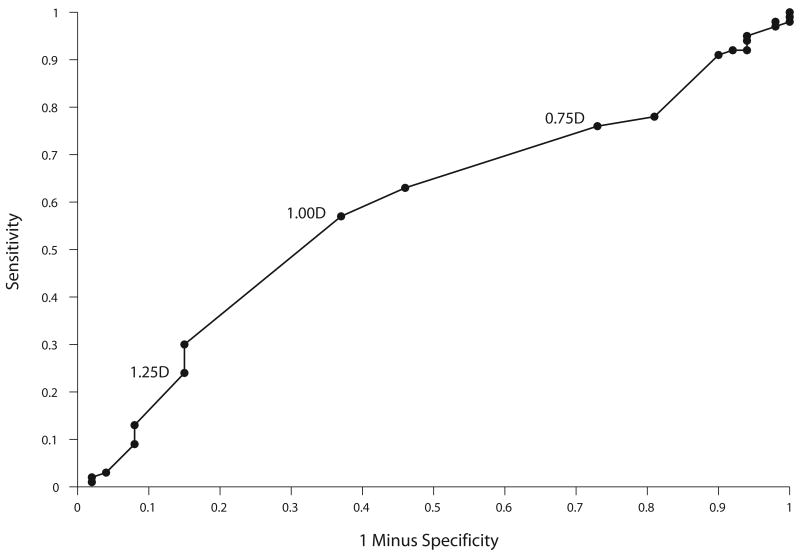
Figure 1 shows the accommodative lag/lead determined by dynamic retinoscopy (Fig 1A – MEM retinoscopy, Fig 1B – Nott retinoscopy) compared to that measured by autorefraction. The line of unity (indicating perfect agreement) does not fit the data well, particularly for higher accommodative lags as determined by autorefraction, and indicates poor agreement between the two measures.
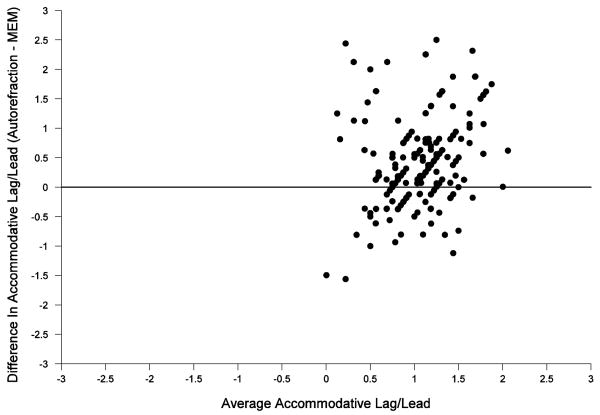
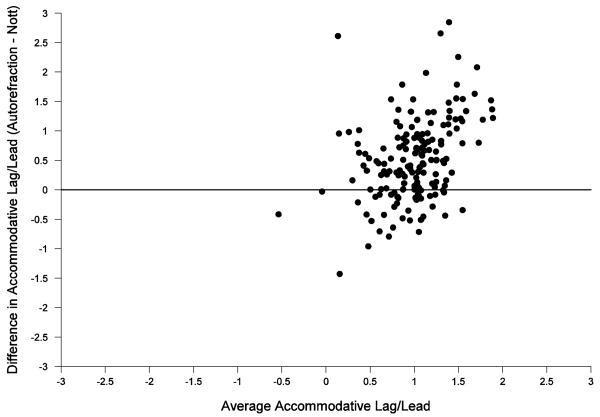
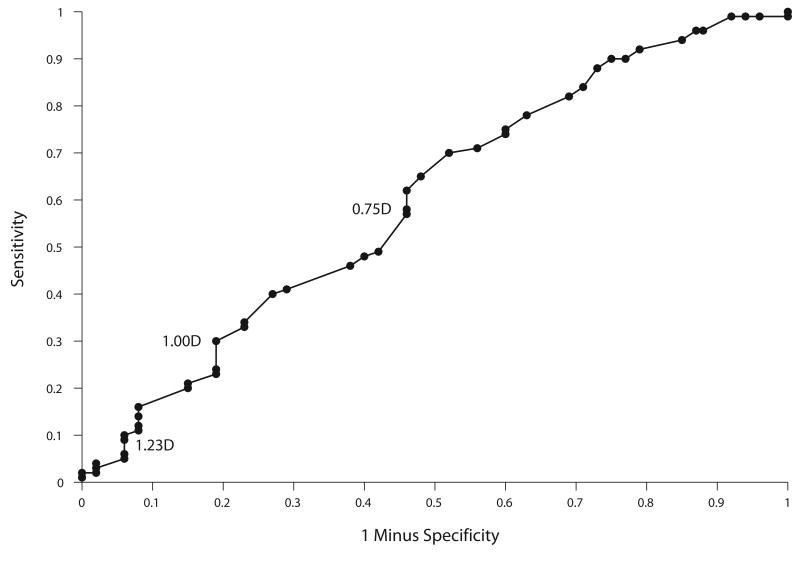
Figure 2 shows a Bland-Altman plot14 of the difference in the accommodative lag/lead measured by the autorefractor and the dynamic retinoscopy methods compared to the average amount of accommodative lag/lead between the two methods. Larger differences between autorefraction and dynamic retinoscopy were associated with larger average accommodative lags (P = 0.002 for MEM retinoscopy and P = <0.001 for Nott retinoscopy).
Figure 2.
The autorefractor classified 116 (69%) children as having a lag of accommodation ≥ 1.00 D, MEM retinoscopy classified 85 (51%) children with a lag ≥ 1.00 D and Nott retinoscopy classified 45 (27%) children with ≥ 1.00D of accommodative lag. Of the 116 children with an accommodative lag ≥ 1.00D by the autorefractor, 66 children were classified by MEM retinoscopy and 35 by Nott retinoscopy as having an accommodative lag ≥ 1.00 D, yielding a sensitivity of 57% (95% CI = 47% to 66%) for MEM retinoscopy and 30% (95% CI = 22% to 39%) for Nott retinoscopy (Table 3). Of the 52 children classified with an accommodative lag < 1.00 D by autorefraction, 33 children were classified by MEM retinoscopy and 42 children by Nott retinoscopy as having accommodative lags < 1.00 D, yielding a specificity of 63% (95% CI = 49% to 76%) for MEM retinoscopy and 81% (95% CI = 67% to 90%) for Nott retinoscopy.
Table 3. MEM and Nott Retinoscopy Accommodative Lag Classifications According to Classification By Grand Seiko Autorefraction (Gold Standard) of Lag ≥ 1.00 D (N=168).
| Accommodative Lag ≥ 1.00 D by Grand Seiko Autorefractor
(Gold Standard) |
||
|---|---|---|
| Present
(N=116) |
Absent
(N= 52) |
|
| Accommodative Lag ≥ 1.00 D by MEM Retinoscopy N (%) | ||
| Present | 66 (57) | 19 (37) |
| Absent | 50 (43) | 33 (63) |
| Accommodative Lag ≥ 1.00 D by Nott Retinoscopy, N (%) | ||
| Present | 35 (30) | 10 (19) |
| Absent | 81 (70) | 42 (81) |
To determine if altering the cut points used for MEM and Nott retinoscopy methods would improve the ability of these methods to identify individuals with an accommodative lag ≥ 1.00 D as determined by the autorefractor, receiver operating characteristic (ROC) curves were generated and are shown in Figure 3. When the curve rises rapidly and lies close to the true positive values plotted on the ordinate, the area under the curve will be large, indicating the technique is accurate and both the sensitivity and specificity will be high. As seen in Figure 3, the shape of the ROC curves for MEM and for Nott retinoscopy approaches the 45 degree diagonal and the area under the ROC curves is 0.59 and 0.60 respectively, demonstrating that neither technique accurately differentiates subjects with accommodative lag ≥ 1.00 D from those with accommodative lag < 1.00 D based on the autorefractor. Changing the cut point for either method does not improve either method's performance for identifying accommodative lag ≥ 1.00 D as determined by the autorefractor. For example, lowering the MEM retinoscopy cut point to 0.75 D accommodative lag would yield a sensitivity and specificity of 76% and 27%, respectively; lowering the Nott retinoscopy cut point to 0.75 D accommodative lag would yield a sensitivity and specificity of 58% and 54%, respectively.
Figure 3.
Comparison of MEM vs. Nott Retinoscopy
Comparing MEM retinoscopy to Nott retinoscopy, the difference in accommodative lag/lead (MEM retinoscopy minus lag/lead calculated by Nott retinoscopy) ranged from -1.42 D to +1.33 D with a mean difference of +0.12 D, with 121 (72%) of the MEM retinoscopy values falling within 0.50 D of the Nott retinoscopy values. Figure 4 shows a Bland-Altman plot14 of the difference between the lag/lead determined by MEM and Nott retinoscopy as a function of the average accommodative lag/lead from MEM and Nott retinoscopy. Larger differences between these dynamic retinoscopy methods are associated with larger accommodative lags as determined by the average of the MEM and Nott retinoscopy measurements (P = 0.03). However, larger differences between these two dynamic retinoscopy methods are not associated with larger accommodative lag/lead as determined by autorefraction (P=0.57).
Figure 4.
Discussion
Agreement between the objective assessment of accommodative lag/lead by open-field autorefraction and either dynamic retinoscopy method was modest to poor. For accommodative lags of 1.00 D or greater as determined by autorefraction, the sensitivity for MEM retinoscopy was 57% and Nott retinoscopy was 30%. Although the specificity was better than sensitivity for each of the retinoscopy procedures, 63% for MEM retinoscopy and 81% for Nott retinoscopy, for most clinical applications the ability to accurately identify a child who does not have a large accommodative lag is often less important than to identify those with higher lags of accommodation. The shape and area of the ROC curves failed to reveal alternate cut points that would improve the combination of sensitivity and specificity for identifying accommodative lag ≥ 1.00 D as defined by autorefraction.
Comparison of the results of this study to similar studies in the literature is limited by the paucity of previous investigations and the lack of studies with children. McClelland and Saunders15 compared accommodative responses obtained by Nott retinoscopy and the Grand Seiko WV500 autorefractor for a 10.00 D, 6.00 D, and 4.00 D accommodative demand in 41 subjects 6 to 43 years of age (mean age 24.45 years, SD 9.82 years) while wearing their habitual distance correction for both methods. As stated by the authors, on average, the accommodative response measured with Nott retinoscopy was closer to the 4.00 D target demand (i.e., smaller accommodative lags) than those obtained with autorefraction (consistent with the results reported herein), but the mean difference between the two techniques was small (0.06 D for the 4.00 D stimulus) leading the authors to conclude that Nott retinoscopy “may be confidently used to assess objectively accommodative function ….”15 Rosenfield and coworkers16 compared a number of measures of accommodative response in 24 adults with a mean age of 25 years (range 22.5 to 30.1). The comparison relevant to this investigation is between Nott retinoscopy and the Canon R1, an open-field autorefractor. For a 2.50 D demand they report a mean difference of -0.02 D with 95% limits of agreement of ± 0.65 D, leading the authors to conclude that Nott retinoscopy was an appropriate method for clinical assessment of accommodative response.16 One explanation for the smaller differences between lag/lead by Nott retinoscopy and autorefraction reported previously15, 16 compared to the larger difference reported in the present study is that the range of accommodative lags by autorefraction was much smaller in the previous studies than in the current study. As reported here and shown in Figure 2, the magnitude of the differences in the amount of accommodative lag/lead measured by autorefraction and dynamic retinoscopy increases as the average of accommodative lag/lead measured by autorefraction and dynamic retinoscopy increases.
Significant procedural differences between each of the retinoscopy techniques and the autorefractor could have contributed to the modest to poor agreement and the higher accommodative lags measured by autorefraction. The current study was designed to compare MEM and Nott retinoscopy as performed routinely in clinical practice to the Grand Seiko autorefractor. MEM and Nott retinoscopy were performed through a trial frame with the most current subjective refraction while autorefraction was done through the spherical equivalent of the subjective refraction. Although the entrance criteria restricted astigmatic refractive errors to 1.50 D or less, uncorrected astigmatic errors during autorefraction resulting from the use of the spherical equivalent correction could introduce errors in the measured response if the children biased their accommodation towards one meridian over the other rather than choosing the mid-point where both meridians would be equally blurred. However, previous work by Rosenfield and Ciuffreda17 suggests that when adults are presented with two dioptrically disparate stimuli (separated by 2 or 4 D), the individual's responses are variable and not predictable. They found that while the majority of subjects' accommodative responses fell between the two stimulus levels, some accommodated for the proximal and others for the distal target. Therefore it is not possible to predict what effect the difference in refractive correction may have introduced in our study, but it is unlikely to have introduced a systematic error that would account for all the differences reported here.
Another important procedural difference is that both MEM and Nott retinoscopy were done with both eyes open, while autorefraction was performed monocularly, allowing the vergence loop to remain open. Vergence-associated accommodation present during the binocular retinoscopy procedures would be expected to result in smaller lags of accommodation.18 In fact, several authors have reported statistically significant smaller lags of accommodation for targets viewed binocularly compared to monocular viewing conditions. Using the Canon R-1 open-field autorefractor in a group of 14 young adults, Jiang and colleagues19 found larger accommodative responses (smaller lags of accommodation) for a 2.50 D accommodative stimulus under binocular viewing than found under monocular viewing. Nakatsuka et al4 also reported smaller lags of accommodation with binocular viewing compared to monocular viewing, using the Grand Seiko open-field autorefractor, the same autorefractor used in the study reported here. For the 3.00 D demand, the accommodative lag for the 28 myopic adults was 0.35 D ± 0.35 D (SD) under monocular viewing and 0.16 D ± 0.35 D (SD) under binocular viewing. These previous reports of smaller lags of accommodation under binocular viewing conditions than under monocular viewing when tested with the same technique (autorefraction) are consistent with the differences reported in the current study and suggest that differences in viewing conditions between binocular retinoscopy and monocular autorefraction may be contributing to the poor agreement.
Both retinoscopy procedures were performed under moderate room illumination while autorefraction was done with the room lights off. The decreased illumination during autorefraction provides fewer proximal cues that would be consistent with less accurate accommodation or the larger accommodative lags found with autorefraction.20 Although the target size was similar in the present study for both retinoscopy procedures (about 20/80) and autorefraction (20/100), the cognitive demands of the test were greater during retinoscopy. The children were engaged during the retinoscopy procedure by the examiner asking them to read the words or letters aloud, but were only instructed to keep the letters clear during autorefraction. Increased cognitive demand has been associated with greater accommodation21 and therefore smaller lags of accommodation.
Although each dynamic retinoscopy procedure was performed by a different masked examiner, in random-assigned order, it is possible that one type of examiner bias may have contributed to a portion of the differences between the 3 methods. Although examiners received standardized training on each procedure, examiners may have been biased by the accommodative lag typically found in this age group. The expected accommodative lag for children with normal vision (kindergarten to grade 6) by MEM retinoscopy is 0.33 D,22 much lower than the mean amount of accommodative lag found in our study. When performing MEM or Nott retinoscopy it is difficult to determine how or if this expectation affects the results, but the fact that the lag/lead of accommodation when measured by the two retinoscopy methods was smaller than that obtained by autorefraction is consistent with a bias that could be present based on the expected accommodative lag for this age group. When performing Nott retinoscopy, lags of accommodation are neutralized by increasing the distance between the child and the examiner while the accommodative demand remains stationary at the 33 cm test distance. To measure an accommodative lag of 1.50 D for the 3.00 D demand, the examiner would need to be positioned at 67 cm from the subject, or would move back 33 cm (almost 13 inches) behind the accommodative target. Considering the retinoscope is conjugate with the participant's point of focus in this technique, it may be difficult for the examiner to accept that the participant would be focused 33 cm behind the plane of the target.
Another factor that might have contributed to the differences between methods is the examiner's ability to insure that the accommodative response is stable before taking a measurement with MEM or Nott retinoscopy. If the accommodative response is fluctuating, the examiner performing MEM and Nott retinoscopy is able to observe these fluctuations in the retinoscopic reflex and may tend to take the measurement that s/he feels is most representative of the accommodative response, although this could vary greatly across examiners. In contrast, there is no opportunity to directly monitor the accommodative response with autorefraction and take the most stable measurement. A related issue is that if the examiner notes a significant change in the accommodative response during retinoscopy, the examiner can redirect the attention of the child prior to taking the measurement. This interaction between examiner and subject during retinoscopy would be expected to result in a smaller lag of accommodation compared to the responses measured with the autorefractor, a prediction consistent with the results of this study.
The agreement between MEM and Nott retinoscopy found in this study (72% of values of MEM retinoscopy falling with ± 0.50 D of Nott retinoscopy) is similar to that reported previously.16, 23, 24 The better agreement of MEM and Nott retinoscopy with each other compared with that between either technique and autorefraction suggests that both retinoscopy techniques may be measuring a similar factor, but perhaps not the same measured by the autorefractor.
Strengths of the current study include a large number of children with an extensive range of accommodative lag/leads, improving the generalizability of the results. The two retinoscopy procedures were performed by different examiners, masked to the results of each other. Additionally, all examiners were trained and certified to perform the procedures.
One limitation of the current study is selection bias related to the sample. As this study was conducted as an ancillary study within the screening process for a randomized clinical trial, some sites pre-screened potential subjects, recruiting into the present study only those most likely to be eligible for the randomized trial. As a result, the proportion of children with esophoria at near (an inclusion criterion for the randomized trial) is much higher than would be expected in a typical sample of myopic children.8 The average lag of accommodation is also greater than that of typical myopic children in this age range8 measured previously with the Canon R1 open-field autorefractor. Another limitation is the test order effect. Although the order of the two retinoscopy techniques was randomized, the objective measurement of autorefraction was always performed last to maintain masking throughout the retinoscopy procedures. Therefore, the possibility of fatigue or wandering attention during measurements by autorefraction could have led to greater accommodative lag. There is also a trade-off between a larger sample gained by participation from multiple sites and the greater variability that results from the multiple examiners at the different sites.
In summary, MEM and Nott retinoscopy underestimated the lag of accommodation when compared to the objective, open-field autorefractor. The modest sensitivity of MEM and the poor sensitivity of Nott retinoscopy reported here indicate that using these methods according to the protocols employed in this study will not provide a viable alternative to autorefraction for the identification of lags of accommodation of 1.00 D or more in myopic children. A variety of modifiable methodological differences among the techniques may be contributing to the modest to poor agreement. Additional investigations will be required to determine if modification of the dynamic retinoscopy techniques and/or those used for autorefraction would result in better agreement between the different measures of accommodative lag.
Acknowledgments
Supported by National Institutes of Health Grant EY011751 (PEDIG), Department of Health and Human Services.
Writing Committee: Lead authors: Ruth E. Manny, OD, PhD; Danielle L. Chandler, MSPH; Mitchell M. Scheiman, OD; Jane E. Gwiazda, PhD. Additional writing committee members (alphabetical): Susan A. Cotter, OD, MS; Donald F. Everett, MA; Jonathan M. Holmes, BM, BCh; Leslie G. Hyman, PhD; Marjean T. Kulp, OD, MS; Don W. Lyon, OD; Wendy Marsh-Tootle, OD; Noelle Matta, B. Michele Melia, ScM; Thomas T. Norton, PhD; Michael X. Repka, MD; David I. Silbert, MD; Erik M. Weissberg, OD.
The Correction of Myopia Evaluation Trial 2 (COMET2) Study Group
Clinical Sites that Participated in this Protocol:
Sites are listed in order by number of patients enrolled into the study. Personnel are indicated as investigator (I), coordinator (C), or tester (T).
Houston, TX – University of Houston College of Optometry (42)
Ruth E. Manny (I), Soyung A. Kim (I), Mamie R. Batres (C), Giselle M. Garza (C), Jennifer A. McLeod (C), Julio C. Quiralte (C), Gabynely G. Solis (C), Heather A. Anderson (T), Karen D. Fern (T)
Indianapolis, IN - Indiana University School of Optometry(33)
Don W. Lyon (I), Donna K. Carter (C), Sara C. Long (C), Stephanie K. Sims (C), Michelle L. Varvel (C), Julia A. Wilhite (C), Scott J. Caughell (T), Kathryn Gray (T), Danielle F. Warren (T)
Fullerton, CA - Southern California College of Optometry (31)
Susan A. Cotter (I), Carmen N. Barnhardt (I), Catherine L. Heyman (I), Kristine Huang (I), Yvonne F. Flores (C), Jamie H. Morris (C), Sue Parker (C), Monique M. Nguyen (T), Michael W. Rouse (T)
Columbus, OH - The Ohio State University (26)
Marjean T. Kulp (I), Jeffrey J. Walline (I), Mark A. Bullimore (I), Maureen E. Biddle (C), Freda D. Dallas (C), Nancy E. Stevens (C), David Berntsen (T), Andrew J. Toole (T)
Birmingham, AL - University of Alabama at Birmingham School of Optometry (22)
Wendy L. Marsh Tootle (I), Marcela Frazier (I), Kristine T. Hopkins (I), Katherine K. Weise (I), Cathy H. Baldwin (C), Terra L. Brackett (C), Michael P. Hill (C), Blake T. Samper (C), Maria S. Voce (C)
Lancaster, PA - Family Eye Group (13)
David I. Silbert (I), Don D. Blackburn (I), Troy J. Hosey (I), Eric L. Singman (I), Noelle S. Matta (C)
Philadelphia, PA - Pennsylvania College of Optometry (2)
Mitchell M. Scheiman (I), Karen E. Pollack (C), Melissa A. Carr (T), Michael F. Gallaway (T), Janet X. Swiatocha (T), Thuy Mong T. Vu (T)
Boston, MA - New England College of Optometry (1)
Erik W. Weissberg (I), Robert E. Owens (C), Elise N. Harb (T)
Correction of Myopia Evaluation Trial 2 (COMET2) Steering Committee:
Jane Gwiazda, Danielle Chandler, Susan Cotter, Donald F. Everett, Jonathan M. Holmes, Leslie Hyman, Marjean Kulp, Don W. Lyon, Ruth E. Manny, Wendy Marsh-Tootle, Noelle Matta, Michele Melia, Thomas Norton, Michael X. Repka, Mitchell Scheiman, David Silbert, Erik Weissberg
PEDIG Coordinating Center: Roy W. Beck, Gladys N. Bernett, Christina M. Cagnina-Morales, Danielle L. Chandler, Katrina L. Dawson, Quayleen Donahue, Michelle D. Drew, Mitchell Dupre, Raymond T. Kraker, Stephanie V. Lee, Shelly T. Mares, Amanda R. McCarthy, Michele Melia, Pamela S. Moke, Stephanie Morgan-Bagley
National Eye Institute - Bethesda, MD: Donald F. Everett
PEDIG Executive Committee: Roy W. Beck, Eileen E. Birch, Stephen P. Christiansen, Susan A. Cotter, Sean P. Donahue, Donald F. Everett, Jonathan M. Holmes, Darren L. Hoover, Pamela A. Huston, Raymond T. Kraker, Michael X. Repka, Nicholas A. Sala, Mitchell M. Scheiman, David K. Wallace
Footnotes
The writing committee and a list of the members of the Correction of Myopia Evaluation Trial 2 (COMET2) Study Group appear in the acknowledgements.
No conflicting relationships exist
References
- 1.Sheard C. Dynamic skiametry. Am J Optom. 1929;6(11):609–23. [Google Scholar]
- 2.Morgan MW., Jr Accommodation and its relationship to convergence. Am J Optom Arch Am Acad Optom. 1944;21:183–95. [Google Scholar]
- 3.Ramsdale C. Monocular and binocular accommodation. Ophthal Opt. 1979;19:602–22. [Google Scholar]
- 4.Nakatsuka C, Hasebe S, Nonaka F, Ohtsuki H. Accommodative lag under habitual seeing conditions: comparison between adult myopes and emmetropes. Jpn J Ophthalmol. 2003;47(3):291–8. doi: 10.1016/s0021-5155(03)00013-3. [DOI] [PubMed] [Google Scholar]
- 5.McBrien NA, Millodot M. The effect of refractive error on the accommodative response gradient. Ophthalmic Physiol Opt. 1986;6(2):145–9. [PubMed] [Google Scholar]
- 6.Gwiazda J, Thorn F, Bauer J, Held R. Myopic children show insufficient accommodative response to blur. Invest Ophthalmol Vis Sci. 1993;34(3):690–4. [PubMed] [Google Scholar]
- 7.Allen PM, O'Leary DJ. Accommodation functions: co-dependency and relationship to refractive error. Vision Res. 2006;46(4):491–505. doi: 10.1016/j.visres.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44(4):1492–500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 9.Gwiazda J, Hyman L, Norton TT, et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004;45(7):2143–51. doi: 10.1167/iovs.03-1306. [DOI] [PubMed] [Google Scholar]
- 10.Rosenfield M, Desai R, Portello J. Do progressing myopes show reduced accommodative responses. Optom Vis Sci. 2002;79:268–73. doi: 10.1097/00006324-200204000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Mutti DO, Mitchell GL, Hayes JR, et al. Accommodative lag before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2006;47(3):837–46. doi: 10.1167/iovs.05-0888. [DOI] [PubMed] [Google Scholar]
- 12.Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom Vis Sci. 2005;82(4):273–8. doi: 10.1097/01.opx.0000159363.07082.7d. [DOI] [PubMed] [Google Scholar]
- 13.Nott IS. Dynamic skiametry, accommodation and convergence. Am J Physiol Opt. 1925;6(4):490–503. [Google Scholar]
- 14.Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. The Statistician. 1983;32(3):307–17. [Google Scholar]
- 15.McClelland JF, Saunders KJ. The repeatability and validity of dynamic retinoscopy in assessing the accommodative response. Ophthalmic Physiol Opt. 2003;23(3):243–50. doi: 10.1046/j.1475-1313.2003.00113.x. [DOI] [PubMed] [Google Scholar]
- 16.Rosenfield M, Portello JK, Blustein GH, Jang C. Comparison of clinical techniques to assess the near accommodative response. Optom Vis Sci. 1996;73(6):382–8. doi: 10.1097/00006324-199606000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Rosenfield M, Ciuffreda KJ. Accommodative responses to conflicting stimuli. J Opt Soc Am A. 1991;8(2):422–27. doi: 10.1364/josaa.8.000422. [DOI] [PubMed] [Google Scholar]
- 18.Fincham EF, Walton J. The reciprocal actions of accommodation and convergence. J Physiol. 1957;137(3):488–508. doi: 10.1113/jphysiol.1957.sp005829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang BC, Tea YC, O'Donnell D. Changes in accommodative and vergence responses when viewing through near addition lenses. Optometry. 2007;78:129–34. doi: 10.1016/j.optm.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 20.Rosenfield M, Ciuffreda KJ. Proximal and cognitively-induced accommodation. Ophthal Physiol Opt. 1990;10(3):252–6. [PubMed] [Google Scholar]
- 21.Kruger PB. The effect of cognitive demand on accommodation. Am J Optom Physiol Optics. 1980;57(7):440–5. doi: 10.1097/00006324-198007000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Rouse M, Hutter R, Shiftlett R. A normative study of the accommodative lag in elementary school children. Am J Optom Physiol Optics. 1984;61:693–7. doi: 10.1097/00006324-198411000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Locke LC, Somers W. A comparison study of dynamic retinoscopy techniques. Optom Vis Sci. 1989;66(8):540–4. doi: 10.1097/00006324-198908000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Goss DA, Groppel P, Dominguez L. Comparison of MEM retinoscopy & Nott retinoscopy & their interexaminer repeatabilities. J Behav Optom. 2005;16(6):149–55. [Google Scholar]