Abstract
von Hippel-Lindau (VHL) disease is an autosomal dominant inherited tumor syndrome characterized by the development of tumors in the eye, brain, spinal cord, inner ear, adrenal gland, pancreas, kidney, and epididymis, associated with germline mutations in the VHL gene. We used sequentially sequencing method and multiple ligation-dependent probe amplification (MLPA) analysis and detected germline mutations in the VHL in 15/15 (100%) of VHL patients fulfilling the clinical criteria. Of the 15 distinct mutations detected, large deletions were detected in 5/15 (33.3%) patients, including 4/15 (26.7%) partial deletions and 1/15 (6.6%) deletion of the entire VHL gene by MLPA and the remainder were point mutations detected by sequencing method, of which five mutations were novel. Using MLPA analysis, we detected large deletions including both partial deletions and complete gene deletion, which has not been reported in Korean VHL patients. In conclusion, sequential application of sequencing method and MLPA analysis might make possible to identify germline mutations in most patients with VHL.
Keywords: VHL, MLPA, Gene Deletion, Korean
INTRODUCTION
von Hippel-Lindau (VHL) disease (MIM#193300) is a rare, dominantly inherited disease characterized by predisposition to the development of a combination of benign and malignant tumors affecting multiple organs including central nervous system, kidney, pancreas, adrenal gland, eye and endolymphatic sac (1-5). Reported birth incidence ranges from 1:36,000 to 1:45,000 (6). Penetrance is essentially complete at 65 yr of age and subjects at risk may develop a combination of clinical manifestations during their lifetime (7).
Predisposition to VHL disease results from germline mutations in the VHL tumor suppressor gene, while loss of the wild type VHL allele or inactivating mutations are additionally found in tumors, either malignant (renal cell carcinomas, RCCs) or benign (cerebellar hemangioblastoma [HB] or pheochromocytoma [PH]) (8). The VHL gene was mapped to 3p25-26 (9) and cloned in 1993 by an international cooperative study (10). Several groups in North America, Europe, and Japan have collectively reported more than 224 distinct intragenic germline mutations (HGMD online), although the frequency of mutation detection has varied considerably among studies (11-17). The spectrum of known mutations in the VHL gene includes missense and nonsense mutations, deletions or insertions of one to several nucleotides, splice site mutations, and rearrangements consisting of partial or complete deletion of the gene. Previous studies showed a frequency of point mutation detected by sequencing the VHL gene of 60-80% and large deletion of the VHL gene including partial and complete gene deletion of 20-40% in the VHL families (18, 19). Southern blotting has been the most conventional technique used for the detection of large deletion of the VHL gene. However, it was labor intensive and time-consuming.
Recently, a new technique, multiple ligation-dependent probe amplification (MLPA), has been described that allows detection of large genetic rearrangements by simultaneous amplification of up to 45 target sequences (20, 21). Here, we report the nature of VHL gene mutations in Korean VHL patients. The aim of this study is to estimate the frequencies of point mutations and large deletions missed by sequencing analysis in Korean VHL patients and verify the usefulness of the MLPA technique in the diagnosis of VHL.
MATERIALS AND METHODS
Subjects
From October 2001 to September 2006, 26 unrelated patients suspicious of VHL disease were referred to Samsung Medical Center, Seoul, Korea for VHL gene study. Among them, 15 patients fulfilled the clinical criteria for VHL disease (Table 1). The VHL disease could be diagnosed on the basis of clinical criteria in the presence of a single HB, PH, multiple pancreatic cysts, or RCC in a patient with family history. For clinical diagnosis of isolated cases of VHL, at least two HB or a single HB in association with a visceral manifestation (RCC, PH, or multiple pancreatic cysts) were required (1, 7). Currently, VHL is subclassified into type 1 and type 2 according to the low or high risk of developing PH. The Institutional Review Board at Samsung Medical Center Clinical Research Institute approved this study protocol, and written informed consent was obtained from each subject prior to the commencement of this study.
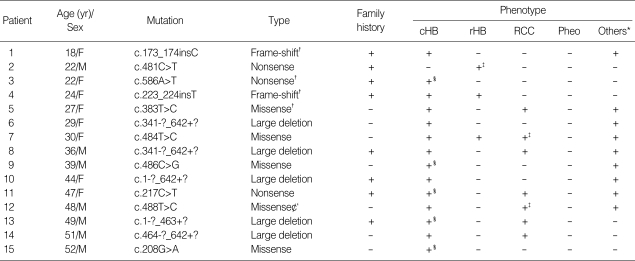
Table 1.
Germline mutations in the VHL gene and related phenotypes in 15 unrelated VHL patients
*, Others include pancreatic neuroendocrine tumors (PNETs), renal and pancreatic cysts and central nervous system tumors; †, Novel mutations; ‡, Bilateral involvements; §, Multiple involvements.
cHB, hemangioblastomas of the central nervous system; rHB, hemangioblastomas of retina; RCC, renal cell carcinomas; Phe, pheochromocytomas.
Mutation analysis
Sequencing of the VHL gene
Blood samples were collected from the patients. The genomic DNA was isolated from the peripheral blood leukocytes using a Wizard genomic DNA purification kit according to the manufacturer's instructions (Promega, Madison, WI, U.S.A.). The three exons of the VHL gene as well as their flanking introns were amplified using the primer sets designed by the authors: 1F 5' AGCGCGTTCCATCCTCTAC 3' and 1R 5' GGGCTTCAGACCGTGCTAT 3'; 2F 5' TCCCAAAGTGCTGGGATTAC 3' and 2R 5' TGGGCTTAATTTTTCAAGTGG 3'; 3F 5' GTTGGCAAAGCCTCTTGTTC 3' and 3R 5' AAGGAAGGAACCAGTCCTGT 3'. A polymerase chain reaction (PCR) was carried out using a thermal cycler (model 9700; Applied Biosystems, Foster City, CA, U.S.A.) as follows: 32 cycles of denaturation at 94℃ for 30 sec, annealing at 60℃ for 30 sec, and extension at 72℃ for 30 sec. After treating the amplicon (5 µL) with 10 U shrimp alkaline phosphatase and 2 U exonuclease I (USB Corp., Cleveland, OH, U.S.A.), direct sequencing was performed using the BigDye Terminator Cycle Sequencing Ready Reaction kit (Applied Biosystems) on an ABI Prism 3100 genetic analyzer (Applied Biosystems). For the patients identified with mutations, the process of re-PCR and resequencing with alliquot of stored DNA was done. All novel missense mutations were confirmed by sequencing the 400 control chromosomes.
MLPA analysis
MLPA analysis to detect large deletions in the VHL gene was carried out using the SALSA P016B VHL probe kit (MRC-Holland, Amsterdam, Netherlands). The kit contains eight probes to the VHL gene (four in exon 1 and two in each of exon 2 and 3), an additional five probes to three other genes on 3p and two control probes to regions telomeric and centromeric from VHL, and 14 probes to regions of other chromosomes. Briefly, 100 ng DNA was denaturated at 98℃ for 5 min, the MLPA probe cocktail was added to a total volume of 8 µL and allowed to hybridize for 16 hr at 60℃. Following addition of Ligase-65 and ligation at 54℃ for 15 min, the ligase was inactivated at 98℃ for 5 min. PCR primers, dNTP, and polymerase mix were then added and PCR was carried out for 33 cycles of (95℃ for 30 sec, 60℃ for 30 sec, and 75℃ for 60 sec). Products were then analyzed using an ABI PRISM 3130x Genetic Analyzer (Applied Biosystems) with ROX-500-labeled internal size standard. Data was generated using GeneMapper (GeneMapper® Software Version 4.0, Applied Biosystems). Five healthy control samples were included in each MLPA test. We determined VHL gene dosage by using an Excel template offered by manufacturer, available at the MRC-Holland web site (www.mrcholland.com). Cut-off levels for loss of relative copy numbers were set at 0.7 (22).
RESULTS
We were able to define germline VHL mutations in all patients who fulfilled the clinical criteria for VHL (Table 1). No mutation of the VHL was detected in other patients who did not meet the clinical criteria for VHL and mostly had only RCC or single HB without family history. Sequencing of the VHL gene detected mutations in 10 patients. In five patients without mutation by sequencing, four partial deletions and one complete deletion were detected by means of MLPA (Fig. 1, 2). We observed 10 different intragenic mutations in 10/15 (66.7%) patients: five missense mutations, three nonsense mutations and two frame-shift mutations. Four different mutations were found in the second half of exon 1, one mutation in exon 2, and five mutations in the 5' part of exon 3. We observed five novel mutations (173_174insC, 223_224insT, 383T>C, 488T>C, 586A>T) unique to Korean population. Both novel nonsense (586A>T) and frameshift (223_224insT, 173_174insC) mutations introduce a premature stop codon leading to a truncated protein and the missense mutations (383T>C, 488T>C) were not detected in normal subjects from the Korean population. Large deletions were detected in 5/15 (33.3%) patients, including 4/15 (26.7%) partial deletions and 1/15 (6.6%) deletion of the entire VHL gene. Partial deletions were heterozygous in size and position: one removed exon 3, two deletions involved exon 2 and 3 and one deletion involved exon 1 and 2.
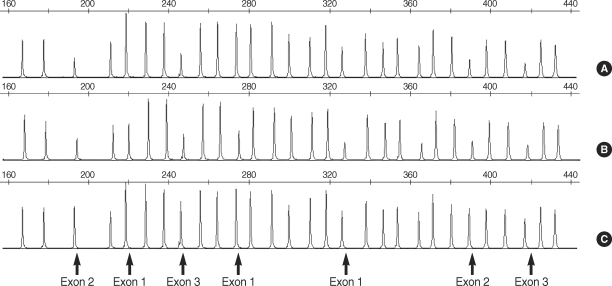
Fig. 1.
Multiplex ligation-dependent probe amplification (MLPA) analysis of VHL exons 1-3. Signal intensity reveals only a single copy of VHL exon 2 and 3 in a patient with VHL due to deletion of VHL exon 2 and 3 (A) and only a single copy of each VHL exon in a patient with VHL due to deletion of whole VHL gene deletion (B) when compared to a healthy control (C).
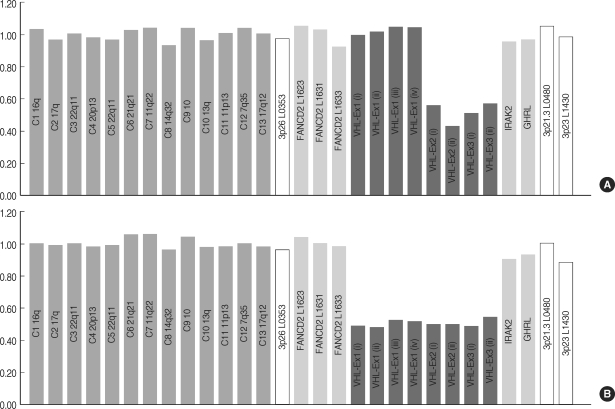
Fig. 2.
DNA dosage profiles estimated by MLPA analysis. Ratios on each DNA dosage are plotted relative to single DNA samples from five unrelated healthy controls. Cut-off levels for loss of relative copy numbers were set at 0.7. A patient with VHL (patient 6) due to deletion of VHL exon 2 and 3 (A) and a patient with VHL (patient 10) due to deletion of whole VHL gene deletion (B). Ex×1, Exon 1; Ex×2, Exon 2; Ex×3, Exon 3.
All patients with VHL mutations were classified as type 1 VHL (without PH). Female patient with complete gene deletion, presented with multiple spinal hemangioblastomas diagnosed at age of 44, which was confirmed by histopathology of tumor tissue and upon evaluation of VHL disease, multiple cysts in pancreas and both kidneys were identified by abdomen-pelvis CT. Her father was died of RCC and her younger sister presented with medullary HB at the age of 37 and multiple RCC in both kidneys at the age of 38, harbored the same mutation observed in her elder sister, proband. Seven (46.7%) patients with germline mutations were found to have no family history of VHL disease. In all cases, samples from both parents were not available and evidence of de novo mutations could not further be evaluated.
DISCUSSION
In the present study, we have detected germline VHL mutations in 15/15 (100%) of patients fulfilling the clinical criteria for VHL, in agreement with previous studies (18, 19). These results imply that most cases fulfilling clinical criteria are related to mutations in the VHL gene and mutation detection strategies covering all mutation type are necessary for risk assessment and counseling of patients and their relatives. Many methods are available for the detection of large deletions in the VHL gene in a diagnostic setting including long PCR with three overlapping pairs of primers (23), universal primer quantitative fluorescent multiplex (UPQFM) PCR (24), quantitative Southern analysis (18) and fluorescent in situ hybridization (FISH). Recently, another method for quantitative genomic screening of copy numbers at specific target sequences has been developed: MLPA (20). In this study, we used MLPA analysis in the diagnosis of large deletions of the VHL gene in VHL patients. The identification of large deletions of the VHL gene is a crucial point in order to increase the detection rate of mutations in VHL patients and to plan the surveillance for early detection of tumors considering genotype-phenotype correlation. The obtained results in our study showed MLPA analysis is a simple rapid reliable tool for the detection of large deletions of the VHL gene (Fig. 1, 2). MLPA approach involves a reduction in labor intensity compared with multiplex PCR, quantitative Southern analysis and FISH, while showing the superior sensitivity as these techniques.
Usually the VHL disease presents with a family history, but de novo mutations have been reported in as many as 23% of VHL patients (25). In our study, we could not confirm the de novo mutations using DNA samples of patients' parents but, the maximum 46.7% of patients would be expected to have de novo mutations. Previous studies showed a frequency of partial VHL gene deletion of 23-30% and complete VHL gene deletion in 8-10% in the VHL patients (18, 19, 26). We showed similar results of a frequency of partial deletion and whole gene deletion; approximately 26.7% and 6.6%, respectively.
The incidence of HB, retinal angioma (RA), RCC and PH are approximately 93.8%, 18.8%, 50.0%, and 0.0% respectively in our study. In four large previous studies including 83, 152, 215, and 522 individuals, RCCs were recognized in 14, 28, 37, and 31% of cases, respectively (6, 13, 27, 28). It was suggested that mutations leading to truncated protein are more likely to promote renal tumorigenesis than missense changes, with a 40% increase in the relative risk of harboring RCC (29) and among VHL families with missense mutations, two mutation cluster regions (MCR-1 and MCR-2) specifically expose to renal involvement (30). We identified no considerable genotype-phenotype correlation in VHL patients with RCC.
Similar mutation associated phenotypes were reported in VHL families of different origin. Germline mutations predicted to inactivate the pVHL have been reported to be associated with RCCs and CNS HBs without PH (VHL type 1); germline mutations predicted to produce full length pVHL to be associated with PH in addition to the other manifestations of VHL (VHL type 2) (16, 31, 32). Non-missense mutations (10/15, 66.7%) predominated in Korean VHL type 1 patients (Table 1), as in type 1 patients from north America, Japan, western Europe and Poland (16, 24, 31, 32). Among missense mutations observed in our patients, 486C>G (C162-W) was reported in Caucasian type 2 VHL families, but no member with PH has been found in this patient's families. We considered that a large number of affected members and a longer period of follow up would be necessary for phenotypic correlation with this mutation.
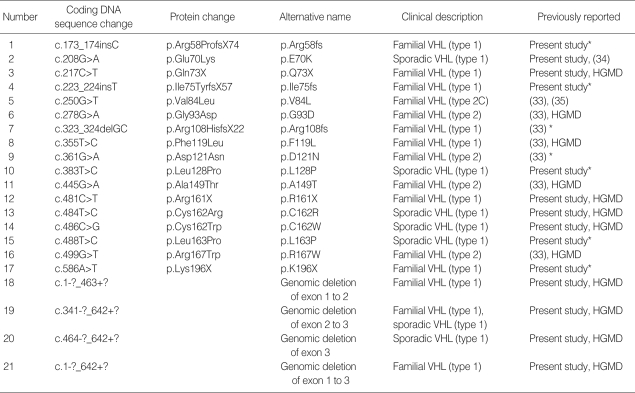
This is the first description of a wide spectrum of germline VHL mutations including large deletions in Korean VHL patients. We have contributed five novel germline mutations, including two missense mutation, two frameshift mutations and one nonsense mutation. In addition, using MLPA analysis, we identified large deletion mutations of the VHL, which did not reported in Korean patients (33) (Table 2) because of limitation of sequencing technique for the detection of large deletions. The improved ability to detect germline VHL mutations primarily reflected the use of MLPA analysis to detect large deletions of the VHL gene.
Table 2.
Germline VHL mutations in Korean VHL patients
Previously reported, HGMD (Human Gene Mutation Database: http://uwcmml1s.uwcm.ac.uk/uwcm/mg/search/120488,html).
*, Novel mutations.
Mutations are described using 'p.' when referring to the VHL protein sequence, and 'c.' for the VHL cDNA sequence. Amino acids are in single-letter notation. Mutations are reported in accordance with the nomenclature for the description of sequence variations as proposed by the Human Genome Variation Society (www.hgvs.org/mutnomen/). The A of the ATG of the initiator Methionine codon (nt. 213 in VHL coding DNA reference sequence NM000551.2) was denoted as nt. +1.
References
- 1.Melmon KL, Rosen SW. Lindau's disease. Review of the literature and study of a large kindred. Am J Med. 1964;36:595–617. doi: 10.1016/0002-9343(64)90107-x. [DOI] [PubMed] [Google Scholar]
- 2.Choyke PL, Glenn GM, Walther MM, Patronas NJ, Linehan WM, Zbar B. von Hippel-Lindau disease: genetic, clinical, and imaging features. Radiology. 1995;194:629–642. doi: 10.1148/radiology.194.3.7862955. [DOI] [PubMed] [Google Scholar]
- 3.Choyke PL, Glenn GM, Wagner JP, Lubensky IA, Thakore K, Zbar B, Linehan WM, Walther MM. Epididymal cystadenomas in von Hippel-Lindau disease. Urology. 1997;49:926–931. doi: 10.1016/s0090-4295(97)00074-5. [DOI] [PubMed] [Google Scholar]
- 4.Manski TJ, Heffner DK, Glenn GM, Patronas NJ, Pikus AT, Katz D, Lebovics R, Sledjeski K, Choyke PL, Zbar B, Linehan WM, Oldfield EH. Endolymphatic sac tumors. A source of morbid hearing loss in von Hippel-Lindau disease. JAMA. 1997;277:1461–1466. doi: 10.1001/jama.277.18.1461. [DOI] [PubMed] [Google Scholar]
- 5.Richard S, David P, Marsot-Dupuch K, Giraud S, Beroud C, Resche F. Central nervous system hemangioblastomas, endolymphatic sac tumors, and von Hippel-Lindau disease. Neurosurg Rev. 2000;23:1–22. doi: 10.1007/s101430050024. discussion 23-4. [DOI] [PubMed] [Google Scholar]
- 6.Maddock IR, Moran A, Maher ER, Teare MD, Norman A, Payne SJ, Whitehouse R, Dodd C, Lavin M, Hartley N, Super M, Evans DG. A genetic register for von Hippel-Lindau disease. J Med Genet. 1996;33:120–127. doi: 10.1136/jmg.33.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maher ER, Iselius L, Yates JR, Littler M, Benjamin C, Harris R, Sampson J, Williams A, Ferguson-Smith MA, Morton N. Von Hippel-Lindau disease: a genetic study. J Med Genet. 1991;28:443–447. doi: 10.1136/jmg.28.7.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaelin WG., Jr Molecular basis of the VHL hereditary cancer syndrome. Nat Rev Cancer. 2002;2:673–682. doi: 10.1038/nrc885. [DOI] [PubMed] [Google Scholar]
- 9.Seizinger BR, Rouleau GA, Ozelius LJ, Lane AH, Farmer GE, Lamiell JM, Haines J, Yuen JW, Collins D, Majoor-Krakauer D, Bonner T, Mathew C, Rubenstein A, Halperin J, Mcconkie-Rosell A, Green JS, Trofatter JA, Ponder BA, Eierman L, Bowmer MI, Schimke R, Oostra B, Aronin N, Smith DI, Drabkin H, Waziri MH, Hobbs WJ, Martuza RL, Conneally PM, Hsia YE, Gusella JF. Von Hippel-Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma. Nature. 1998;332:268–269. doi: 10.1038/332268a0. [DOI] [PubMed] [Google Scholar]
- 10.Latif F, Tory K, Gnarra J, Yao M, Duh FM, Orcutt ML, Stackhouse T, Kuzmin I, Modi W, Geil L, Schmidt L, Zhou F, Li H, Wei MH, Chen F, Glenn G, Choyke P, Walter MM, Weng Y, Duan DS, Dean M, Glavac D, Richards FM, Crossey PA, Ferguson-Smith MA, Paslier DL, Chumakov I, Cohen D, Chinault AC, Maher ER, Linehan WM, Zbar B, Lerman MI. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993;260:1317–1320. doi: 10.1126/science.8493574. [DOI] [PubMed] [Google Scholar]
- 11.Crossey PA, Richards FM, Foster K, Green JS, Prowse A, Latif F, Lerman MI, Zbar B, Affara NA, Ferguson-Smith MA, Maher ER. Identification of intragenic mutations in the von Hippel-Lindau disease tumour suppressor gene and correlation with disease phenotype. Hum Mol Genet. 1994;3:1303–1308. doi: 10.1093/hmg/3.8.1303. [DOI] [PubMed] [Google Scholar]
- 12.Whaley JM, Naglich J, Gelbert L, Hsia YE, Lamiell JM, Green JS, Collins D, Neumann HP, Laidlaw J, Li FP, Klein-Szanto AJP, Seizinger BR, Kley N. Germ-line mutations in the von Hippel-Lindau tumor-suppressor gene are similar to somatic von Hippel-Lindau aberrations in sporadic renal cell carcinoma. Am J Hum Genet. 1994;55:1092–1102. [PMC free article] [PubMed] [Google Scholar]
- 13.Chen F, Kishida T, Yao M, Hustad T, Glavac D, Dean M, Gnarra JR, Orcutt ML, Duh FM, Glenn G. Germline mutations in the von Hippel-Lindau disease tumor suppressor gene: correlations with phenotype. Hum Mutat. 1995;5:66–75. doi: 10.1002/humu.1380050109. [DOI] [PubMed] [Google Scholar]
- 14.Clinical Research Group for VHL in Japan. Germline mutations in the von Hippel-Lindau disease (VHL) gene in Japanese VHL. Hum Mol Genet. 1995;4:2233–2237. doi: 10.1093/hmg/4.12.2233. [DOI] [PubMed] [Google Scholar]
- 15.Maher ER, Webster AR, Richards FM, Green JS, Crossey PA, Payne SJ, Moore AT. Phenotypic expression in von Hippel-Lindau disease: correlations with germline VHL gene mutations. J Med Genet. 1996;33:328–332. doi: 10.1136/jmg.33.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zbar B, Kishida T, Chen F, Schmidt L, Maher ER, Richards FM, Crossey PA, Webster AR, Affara NA, Ferguson-Smith MA, Brauch H, Glavac D, Neumann HP, Tisherman S, Mulvihill JJ, Gross DJ, Shuin T, Whaley J, Seizinger B, Kley N, Olschwang S, Boisson C, Richard S, Lips CH, Linehan WM, Lerman M. Germline mutations in the Von Hippel-Lindau disease (VHL) gene in families from North America, Europe, and Japan. Hum Mutat. 1996;8:348–357. doi: 10.1002/(SICI)1098-1004(1996)8:4<348::AID-HUMU8>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 17.Kamada M, Suzuki K, Kato Y, Okuda H, Shuin T. von Hippel-Lindau protein promotes the assembly of actin and vinculin and inhibits cell motility. Cancer Res. 2001;61:4184–4189. [PubMed] [Google Scholar]
- 18.Stolle C, Glenn G, Zbar B, Humphrey JS, Choyke P, Walther M, Pack S, Hurley K, Andrey C, Klausner R, Linehan WM. Improved detection of germline mutations in the von Hippel-Lindau disease tumor suppressor gene. Hum Mutat. 1998;12:417–423. doi: 10.1002/(SICI)1098-1004(1998)12:6<417::AID-HUMU8>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 19.Rocha JC, Silva RL, Mendonca BB, Marui S, Simpson AJ, Camargo AA. High frequency of novel germline mutations in the VHL gene in the heterogeneous population of Brazil. J Med Genet. 2003;40:e31. doi: 10.1136/jmg.40.3.e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schouten JP, McElgunn CJ, Waaijer R, Zwijnenburg D, Diepvens F, Pals G. Relative quantification of 40 nucleic acid sequences by multiplex ligation-dependent probe amplification. Nucleic Acids Res. 2002;30:e57. doi: 10.1093/nar/gnf056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sellner LN, Taylor GR. MLPA and MAPH: new techniques for detection of gene deletions. Hum Mutat. 2004;23:413–419. doi: 10.1002/humu.20035. [DOI] [PubMed] [Google Scholar]
- 22.Scarciolla O, Stuppia L, De Angelis MV, Murru S, Palka C, Giuliani R, Pace M, Di Muzio A, Torrente I, Morella A, Grammatico P, Giacanelli M, Rosatelli MC, Uncini A, Dallapiccola B. Spinal muscular atrophy genotyping by gene dosage using multiple ligation-dependent probe amplification. Neurogenetics. 2006;7:269–276. doi: 10.1007/s10048-006-0051-3. [DOI] [PubMed] [Google Scholar]
- 23.Cybulski C, Krzystolik K, Maher ER, Richard S, Kurzawski G, Gronwald J, Lubinski J. Long polymerase chain reaction in detection of germline deletions in the von Hippel-Lindau tumour suppressor gene. Hum Genet. 1999;105:333–336. doi: 10.1007/s004399900137. [DOI] [PubMed] [Google Scholar]
- 24.Cybulski C, Krzystolik K, Murgia A, Gorski B, Debniak T, Jakubowska A, Martella M, Kurzawski G, Prost M, Kojder I, Limon J, Nowacki P, Sagan L, Bialas B, Kaluza J, Zdunek M, Omulecka A, Jaskolski D, Kostyk E, Koraszewska-Matuszewska B, Haus O, Janiszewska H, Pecold K, Starzycka M, Slomski R, Cwirko M, Sikorski A, Gliniewicz B, Cyrylowski L, Fiszer-Maliszewska L, Gronwald J, Toloczko-Grabarek A, Zajaczek S, Lubinski J. Germline mutations in the von Hippel-Lindau (VHL) gene in patients from Poland: disease presentation in patients with deletions of the entire VHL gene. J Med Genet. 2002;39:E38. doi: 10.1136/jmg.39.7.e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sgambati MT, Stolle C, Choyke PL, Walther MM, Zbar B, Linehan WM, Glenn GM. Mosaicism in von Hippel-Lindau disease: lessons from kindreds with germline mutations identified in offspring with mosaic parents. Am J Hum Genet. 2000;66:84–91. doi: 10.1086/302726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glavac D, Neumann HP, Wittke C, Jaenig H, Masek O, Streicher T, Pausch F, Engelhardt D, Plate KH, Hofler H, Chen F, Zbar B, Brauch H. Mutations in the VHL tumor suppressor gene and associated lesions in families with von Hippel-Lindau disease from central Europe. Hum Genet. 1996;98:271–280. doi: 10.1007/s004390050206. [DOI] [PubMed] [Google Scholar]
- 27.Maher ER, Yates JR, Harries R, Benjamin C, Harris R, Moore AT, Ferguson-Smith MA. Clinical features and natural history of von Hippel-Lindau disease. Q J Med. 1990;77:1151–1163. doi: 10.1093/qjmed/77.2.1151. [DOI] [PubMed] [Google Scholar]
- 28.Richard S, Campello C, Taillandier L, Parker F, Resche F French VHL Study Group. Haemangioblastoma of the central nervous system in von Hippel-Lindau disease. J Intern Med. 1998;243:547–553. doi: 10.1046/j.1365-2796.1998.00337.x. [DOI] [PubMed] [Google Scholar]
- 29.Gallou C, Joly D, Mejean A, Staroz F, Martin N, Tarlet G, Orfanelli MT, Bouvier R, Droz D, Chretien Y, Marechal JM, Richard S, Junien C, Beroud C. Mutations of the VHL gene in sporadic renal cell carcinoma: definition of a risk factor for VHL patients to develop an RCC. Hum Mutat. 1999;13:464–475. doi: 10.1002/(SICI)1098-1004(1999)13:6<464::AID-HUMU6>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 30.Gallou C, Chauveau D, Richard S, Joly D, Giraud S, Olschwang S, Martin N, Saquet C, Chretien Y, Mejean A, Correas JM, Benoit G, Colombeau P, Grunfeld JP, Junien C, Beroud C. Genotype-phenotype correlation in von Hippel-Lindau families with renal lesions. Hum Mutat. 2004;24:215–224. doi: 10.1002/humu.20082. [DOI] [PubMed] [Google Scholar]
- 31.Yoshida M, Ashida S, Kondo K, Kobayashi K, Kanno H, Shinohara N, Shitara N, Kishida T, Kawakami S, Baba M, Yamamoto I, Hosaka M, Shuin T, Yao M. Germ-line mutation analysis in patients with von Hippel-Lindau disease in Japan: an extended study of 77 families. Jpn J Cancer Res. 2000;91:204–212. doi: 10.1111/j.1349-7006.2000.tb00933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Friedrich CA. Genotype-phenotype correlation in von Hippel-Lindau syndrome. Hum Mol Genet. 2001;10:763–767. doi: 10.1093/hmg/10.7.763. [DOI] [PubMed] [Google Scholar]
- 33.Kang HC, Kim IJ, Park JH, Shin Y, Jang SG, Ahn SA, Park HW, Lim SK, Oh SK, Kim DJ, Lee KW, Choi YS, Park YJ, Lee MR, Kim DW, Park JG. Three novel VHL germline mutations in Korean patients with von Hippel-Lindau disease and pheochromocytomas. Oncol Rep. 2005;14:879–883. [PubMed] [Google Scholar]
- 34.Olschwang S, Richard S, Boisson C, Giraud S, Laurent-Puig P, Resche F, Thomas G. Germline mutation profile of the VHL gene in von Hippel-Lindau disease and in sporadic hemangioblastoma. Hum Mutat. 1998;12:424–430. doi: 10.1002/(SICI)1098-1004(1998)12:6<424::AID-HUMU9>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 35.Crossey PA, Eng C, Ginalska-Malinowska M, Lennard TW, Wheeler DC, Ponder BA, Maher ER. Molecular genetic diagnosis of von Hippel-Lindau disease in familial pheochromocytoma. J Med Genet. 1995;32:885–886. doi: 10.1136/jmg.32.11.885. [DOI] [PMC free article] [PubMed] [Google Scholar]