Abstract
While a significant amount of clinical information has been reported concerning intestinal involvement in Behçet's disease (BD), esophageal involvement in BD has not yet been studied extensively. The aim of this study was to evaluate the prevalence of esophageal involvement in BD and its clinical characteristics. We retrospectively reviewed the medical records of 842 patients diagnosed with BD at a single tertiary institution in Korea between January 1990 and June 2006. Of the 842 patients with BD, 129 patients (15.3%) experienced upper gastrointestinal symptoms that required inspection through esophagogastroduodenoscopy. Esophageal involvement was found in 6 (4.7%) of the 129 patients. The activity index of Behçet's disease did not differ among patients with or without esophageal involvement. All patients with esophageal involvement responded well to medical treatment and no one experienced serious complications. The results of our study demonstrate that the prevalence of esophageal involvement in BD is very low and that most patients with such involvement face few complications and respond well to medical treatment.
Keywords: Behçets Disease, Esophageal Ulcer, Intestinal Behçet's Disease, Endoscopy
INTRODUCTION
Behçet's disease (BD) has been recognized as a systemic disorder of recurrent acute inflammation, characterized by the involvement of multiple organs and resulting in orogenital ulcers, uveitis, gastrointestinal ulcers, and skin lesions (1). Its incidence is relatively high from eastern Asia to the Mediterranean and is estimated to affect approximately 1-10 out of 10,000 people in those areas, while in U.K. and North America, only 1-2 cases are found for every 1,000,000 people (2). While the etiology and pathogenesis of the syndrome are still obscure, it is thought that autoimmune mechanisms play a role because vasculitis is the primary pathological lesion, and circulating autoantibodies to human oral mucous membranes are found in approximately 50% of cases (3).
The prognosis of BD varies. However, involvement of the central nervous system, vessels, and intestines often leads to a poor prognosis. Digestive manifestations in BD have been reported in up to 1-60% of cases, although this rate varies in different countries. The most frequent sites of gastrointestinal involvement are the ileocecal region with extension into the ascending colon (4). While esophageal involvement in BD is known to be very rare, anecdotal studies report esophageal involvement can cause serious complications such as strictures, bleeding, perforation, or fistulas (5, 6). Despite a relatively high rate of intestinal involvement in Korean BD patients (7), patterns of esophageal involvement in Korean patients with BD remain unclear in terms of the prevalence and clinical characteristics. Moreover, treatment response is controversial. Some major issues have been examined for intestinal involvement in BD, but esophageal involvement has been not been sufficiently studied. Accordingly, in this study, we aimed to evaluate the prevalence and clinical characteristics of esophageal involvement in Korean BD patients.
MATERIALS AND METHODS
The medical records of 842 consecutive de novo BD patients cared at Severance Hospital, Yonsei University College of Medicine, Seoul, Korea between January 1990 and June 2006 were retrospectively analyzed. Diagnosis of BD was based on a combination of clinical, enodoscopic, radiologic, and pathologic findings. To define BD, various diagnostic criteria have been proposed. In this study, two diagnostic criteria, suggested by the Behçet's disease Research Committee of Japan in 1987 (8) and the International Study Group for Behçet's disease (ISGBD) in 1990 (9), were applied. By using the classification of the Research Committee of Japan, types were categorized into 'complete', 'incomplete', and 'suspicious'. The other criterion, proposed by the ISGBD, was used as a supplement to certify the diagnosis of BD. Demographic characteristics, endoscopic findings, clinical features, treatment responsiveness, and complications were evaluated. Esophageal involvement in BD was confirmed when a discrete, punched-out ulcer, like those found in the intestines of similar patients, was detected during endoscopic examination and other causes, such as acid reflux-related, viral, or drug-induced esophagitis, were ruled out. Malignant diseases such as lymphoma or cancer were also excluded. Histological examination was performed in all cases for the differential diagnosis of esophageal ulceration. Biopsy specimens were obtained using standard-sized biopsy forceps from both the base and the margin of ulcerated lesions. For more accurate diagnosis of undetermined cases, serologic tests or quantitative polymerase chain reaction assays were additionally undertaken to exclude viral esophagitis. Finally, these diagnostic processes were combined with the responses to specific therapy for esophageal involvement of BD and follow-up endoscopic findings.
The activity index of BD was investigated at the timed of esophagogastroduodenoscopy (EGD) due to upper-gastrointestinal symptoms. The clinical activity score was calculated by summing of each clinical manifestation present according to a previously proposed system (2). Statistical analyses of the data were conducted using SPSS 12.0 computer software (Chicago, IL, U.S.A.) for comparison of BD activity with/without esophageal involvement. p value<0.05 were considered statistically significant and all p values correspond to two-sided significance tests.
This study was approved by the Institutional Review Board of Severance Hospital and informed consent was obtained from all patients before endoscopic examinations.
RESULTS
Among the 842 patients with BD, 129 (15.3%) patients experienced gastrointestinal symptoms; all 129 underwent both EGD and ileocolonoscopy. Gastrointestinal symptoms or signs which led them to endoscopic examinations, were as follows: abdominal pain in 58 patients (45.0%), poor oral intake complicated with oral ulcer in 30 (23.2%), melena or hematochezia in 32 (24.8%), chest-pain in 4 (3.1%), dysphagia in 4 (3.1%), and hematemesis in one patient (0.8%). The clinical characteristics of the 129 patients are shown in Table 1 and their endoscopic findings are listed in Table 2. Six patients were shown to have esophageal ulcerations suggestive of esophageal involvement in BD (Fig. 1). The patients with esophageal involvement had a higher disease activity score numerically compared to those without esophageal involvement, which had no statistical significance (p=0.08). Other esophageal diseases found through EGD examinations include gastroesophageal reflux disease (5 patients), esophageal candidiasis (2 patients), hiatal hernia (2 patients), Barrett's esophagus (one patient), esophageal polyp (one patient), and esophageal varices (one patient). Of the 129 patients, intestinal BD was found in 69 patients (53.5%) through colonoscopic examinations.
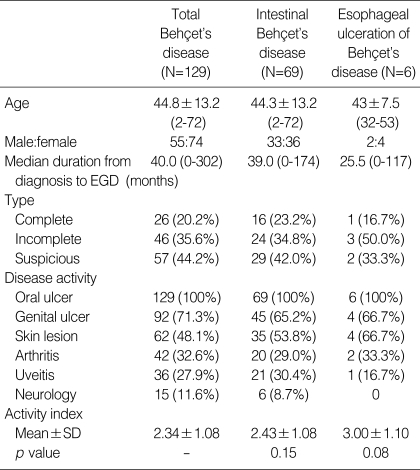
Table 1.
The clinical characteristics of study subjects
EGD, esophagogastroduodenoscopy; SD, standard deviation.
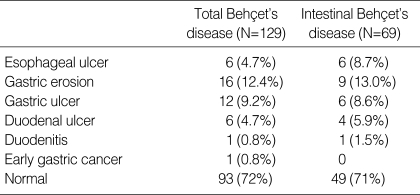
Table 2.
The Esophagogastroduodenoscopic findings in Behçet's disease patients
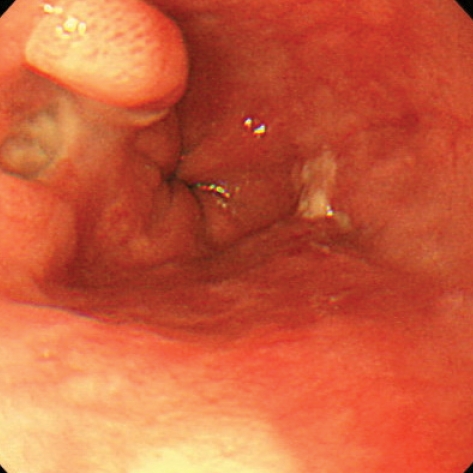
Fig. 1.
Esophageal involvement of Behçet's disease. A 53-yr-old woman with known Behçet's disease complained of intermittent epigastric pain. Endoscopic examination revealed a small punched-out, active ulceration in the distal esophagus of the patient.
Clinical characteristics of esophageal involvement in BD are given in Table 3. Esophageal ulcerations of most patients could be controlled by proton pump inhibitors/histamine-2 receptor blockers, colchicines, and/or 5-aminosalicylic acids. The chest pain of one patient was controlled by oral corticosteroids. The median follow up period of the six patients was 39.5 months (14-78 months) after the diagnosis of esophageal ulceration. Follow-up EGD was performed on all the 6 patients. Of them, in 3 patients, active ulceration previously noted was not found any more and the other 3 patients experienced the improvement of ulcers. No recurrence of symtpoms occurred in all 6 patients during the follow up. Moreover, no patients experienced serious complications, such as esophageal stricture, esophageal bleeding, or esophageal perforations, during follow-up.
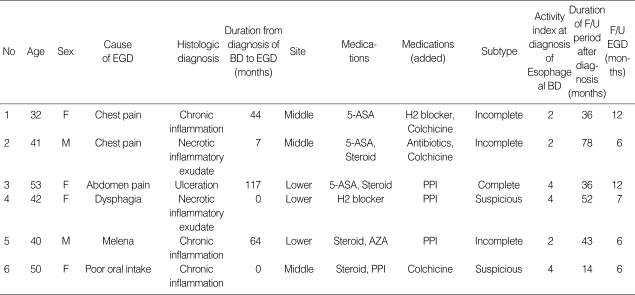
Table 3.
Characteristics of esophageal ulceration in Behçet's disease
EGD, Esophagogastroduodenoscopy; BD, Bechçet's disease; 5-ASA, 5-aminosalicylic acid; PPI, Proton pump inhibitor; AZA, Azathioprine; F/U, Follow up.
DISCUSSION
Gastrointestinal manifestations have been known to lead to severe morbidity in BD patients and are commonly referred to as "Intestinal Behçet's syndrome". The frequency of intestinal involvement in patients with BD was known to be 0-60%, with geographic differences (10). Symptomatic intestinal involvement is rare in Mediterranean patients with BD, but in East Asian patients, including Koreans, intestinal involvement is more common. Shimizu et al. (11) reported that gastrointestinal symptoms are present in at least 50% of the patients with BD in Japan. The intestinal lesions are usually resistant to medical treatment and recur frequently (25-78%) after surgical management, especially in people of Western or Chinese origin (10). The terminal ileum and the cecum are the most frequently involved parts of the gastrointestinal tract with esophageal involvement being very rare. Esophageal ulcerations in BD are diverse and nonspecific. The ulcerations can be single or multiple, shallow or deep, small or large, or clearly or unevenly marginated. Esophageal lesions are most commonly located in the middle esophagus, although diffuse esophagitis and stenosis have also been reported (15). The histological aspects of esophageal ulceration in BD reportedly involve acute or chronic nonspecific infiltrates and granulation tissue and fibroblasts are typically seen at the base of the ulceration. In addition, serious complications such as stricture, bleeding, or perforations have been rarely described. Since the first case of esophageal ulceration of this syndrome was presented by Brodie and Ochsner in 1973 (12), to date, less than 50 cases worldwide of Behçet's patients with esophageal ulcers have been reported. However, the actual prevalence of esophageal involvement in BD is still uncertain and the proper management of this condition has yet to be established (13-15). Thus, the purpose of this study was to investigate the prevalence of esophageal involvement in BD through a large cohort study in a single tertiary institution and to evaluate its clinical characteristics, especially in terms of therapeutic responsiveness and prognosis. Our study investigated the largest population ever reported, and it was found that esophageal ulcerations were detected in only 6 of 129 BD patients (4.7%), which suggests that the prevalence of esophageal involvement in BD is quite low. Moreover, such involvement may not be correlated with systemic disease activity, disease duration, disease activity, or any other aspect of BD. Bottomley et al. (16), conducted the first prospective study of the esophagus in patients with BD. This study involved 9 patients who underwent EGD; three patients were asymptomatic and 6 had upper gastrointestinal symptoms at the time of endoscopy. The prevalence of esophageal involvement in BD was low (11%) and non-specific, but was much higher than that of our data. However, this rate of esophageal involvement might be under- or overestimated because the case number was very small and endoscopic examination was not performed in all cases. In another anecdotal investigation, it was suggested that the esophageal abnormalities in BD were found rather frequently (14/21, 66.6%) and occur even in asymptomatic patients (13). However, in this series, gross endoscopic abnormality was detected in only one patient (4.8%), which yields a rate that is consistent with that of our study. Furthermore, such involvement was not associated with any other features of BD.
Because of a lack of randomized, controlled trials for treatment of various manifestations of BD, the standard treatment remains controversial. The usual initial management is combined drug therapies, involving drugs such as colchicines, non-steroidal anti-inflammatory drug (NSAIDs), glucocorticosteroids, immunosuppressive, or cytotoxic medications. For mucocutaneous lesions, colchicines and NSAIDs are administered (17, 18). However, intestinal lesions are reportedly difficult to treat. Furthermore, intestinal involvement is regarded as a serious manifestation of BD, like neurological symptoms or retinal vascultitis, and more potent drugs are usually chosen. Sonta et al. have suggested that mesalazine is effective for treatment of intestinal BD (19). Glucocorticoids and/or immunosuppressives have also proved effective in treating intestinal BD (20). In addition, several cases and trials reported the successful use of thalidomide, mesalazine, and anti-TNF-α. However, at present, the appropriate treatment for esophageal involvement in BD remains controversial. Corticosteroids represent the major therapeutic agent, but as stated by Brodie and Oshsner, corticosteroid therapy may cause esophageal perforation (12). In our series, the esophageal manifestations respond well to treatment with proton pump inhibitors, mesalazine, and/or colchicines. Moreover, any serious complications, such as esophageal stricture, bleeding, or perforations, did not develop during follow-up.
Our study has several limitations. It is a retrospective design, which causes various investigational limitations. Moreover, we did not perform EGD for all the patients with BD, which may have lead to underestimation of the exact incidence of esophageal involvement in BD. Regarding its treatment, further research is necessary to validate the appropriate treatment of esophageal involvement in BD through randomized prospective studies.
In conclusion, our study demonstrated that upper gastrointestinal symptoms are common in BD patients, but esophageal involvement is very rare and serious complications may be negligible. Moreover, the clinical characteristics of BD with esophageal involvement seem to be similar to those of BD without involvement.
References
- 1.Al-Mutawa SA, Hegab SM. Behcet's disease. Clin Exp Med. 2004;4:103–131. doi: 10.1007/s10238-004-0045-0. [DOI] [PubMed] [Google Scholar]
- 2.Kurokawa MS, Yoshikawa H, Suzuki N. Behcet's disease. Clin Exp Med. 2004;3:10–20. doi: 10.1007/s10238-004-0033-4. [DOI] [PubMed] [Google Scholar]
- 3.Kasper DL, Braunwald E, Hauser S, Longo D, Jameson JL, Fauci AS. Harrison's Principles of Internal Medicine. 16th ed. New York: McGraw-Hill, Medical Pub. Division; 2003. pp. 2014–2015. [Google Scholar]
- 4.Smith JA, Siddiqui D. Intestinal Behçet's disease presenting as a massive acute lower gastrointestinal bleed. Dig Dis Sci. 2002;47:517–521. doi: 10.1023/a:1017999515606. [DOI] [PubMed] [Google Scholar]
- 5.Morimoto Y, Tanaka Y, Itoh T, Yamamoto S, Kurihara Y, Nishikawa K. Esophagobronchial fistula in a patient with Behçet's disease: report of a case. Surg Today. 2005;35:671–676. doi: 10.1007/s00595-004-2975-2. [DOI] [PubMed] [Google Scholar]
- 6.Powderly WG, Lombard MG, Murray FE, O'Connell D, Counihan TB, Lennon JR. Oesophageal ulceration in Behçet's disease presenting with haemorrhage. Ir J Med Sci. 1987;156:193–194. doi: 10.1007/BF02955204. [DOI] [PubMed] [Google Scholar]
- 7.Bang D, Yoon KH, Chung HG, Choi EH, Lee ES, Lee S. Epidemiological and clinical features of Behçet's disease in Korea. Yonsei Med J. 1997;38:428–436. doi: 10.3349/ymj.1997.38.6.428. [DOI] [PubMed] [Google Scholar]
- 8.Mizushima Y, Inaba G, Mimura Y. Diagnostic criteria for Behçet's disease in 1987, and guideline for treating Behçet's disease. Saishin Igaku. 1988;43:391–393. [Google Scholar]
- 9.International Study Group for Behçet's Disease. Criteria for diagnosis of Behçet's disease. Lancet. 1990;335:1078–1080. [PubMed] [Google Scholar]
- 10.Bayraktar Y, Ozaslan E, Van Thiel DH. Gastrointestinal manifestations of Behçet's disease. J Clin Gastroenterol. 2000;30:144–154. doi: 10.1097/00004836-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Shimizu T, Ehrlich GE, Inaba G, Hayashi K. Behçet disease (Behcet syndrome) Semin Arthritis Rheum. 1979;8:223–260. doi: 10.1016/0049-0172(79)90004-0. [DOI] [PubMed] [Google Scholar]
- 12.Brodie TE, Ochsner JL. Behçet's syndrome with ulcerative oesophagitis: report of the first case. Thorax. 1973;28:637–640. doi: 10.1136/thx.28.5.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Houman MH, Ben Ghorbel I, Lamloum M, Khanfir M, Braham A, Haouet S, Sayem N, Lassoued H, Miled M. Esophageal involvement in Behçet's disease. Yonsei Med J. 2002;43:457–460. doi: 10.3349/ymj.2002.43.4.457. [DOI] [PubMed] [Google Scholar]
- 14.Anti M, Marra G, Rapaccini GL, Barone C, Manna R, Bochicchio GB, Fedeli G. Esophageal involvement in Behçet's syndrome. J Clin Gastroenterol. 1986;8:514–519. doi: 10.1097/00004836-198610000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Oose T, Tokutomi K, Takeuchi A, Hashimoto T. A case of Behçet's disease with severe esophageal stenosis treated with esophageal bujie. Ryumachi. 1995;35:81–84. [PubMed] [Google Scholar]
- 16.Bottomley WW, Dakkak M, Walton S, Bennett JR. Esophageal involvement in Behçet's disease. Is endoscopy necessary? Dig Dis Sci. 1992;37:594–597. doi: 10.1007/BF01307585. [DOI] [PubMed] [Google Scholar]
- 17.Yurdakul S, Mat C, Tüzün Y, Ozyazgan Y, Hamuryudan V, Uysal O, Senocak M, Yazici H. A double-blind trial of colchicine in Behçet's syndrome. Arthritis Rheum. 2001;44:2686–2692. doi: 10.1002/1529-0131(200111)44:11<2686::aid-art448>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 18.Meador R, Ehrlich G, Von Feldt J. Behçet's disease: immunopathologic and therapeutic aspects. Curr Rheumatol Rep. 2002;4:47–54. doi: 10.1007/s11926-002-0023-z. [DOI] [PubMed] [Google Scholar]
- 19.Sonta T, Araki Y, Koubokawa M, Tamura Y, Ochiai T, Harada N, Chijiiwa Y, Nawata H. The beneficial effect of mesalazine on esophageal ulcers in intestinal Behçet's disease. J Clin Gastroenterol. 2000;30:195–199. doi: 10.1097/00004836-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Hamuryudan V, Ozyazgan Y, Hizli N, Mat C, Yurdakul S, Tüzün Y, Senocak M, Yazici H. Azathioprine in Behçet's syndrome: effects on long-term prognosis. Arthritis Rheum. 1997;40:769–774. doi: 10.1002/art.1780400425. [DOI] [PubMed] [Google Scholar]