Abstract
Introduction
The challenges of knowledge translation in behavioural health care are unique to this field for a variety of reasons including the fact that effective treatment is invariably embedded in a strong relationship between practitioners and the people they serve.
Methods
Practitioners’ knowledge gained from experience and intuition become an even more important consideration in the knowledge translation process since clinicians are, in fact, a component of most treatments. Communication of findings from science must be conceptualized with sensitivity to this reality.
Results
Considering knowledge translation as a communication process suggests the application of contemporary theories of communication which emphasize the creation of shared meaning over the transmission of knowledge from one person to the next.
Conclusion
In this context outcomes management approaches to create a learning environment within clinical practices that facilitate the goals of knowledge transfer while respecting that the scientific enterprise is neither the sole nor primary repository of knowledge.
Keywords: knowledge translation, outcomes management, practice-based evidence
Résumé
Introduction
Les défis présentés par le transfert des connaissances dans le secteur des soins comportementaux sont uniques pour un certain nombre de raisons, notamment parce que la force des liens qui se tissent entre les cliniciens et leurs clients sont un facteur déterminant de l’efficacité du traitement.
Méthodologie
Les connaissances que les cliniciens acquièrent expérimentalement et intuitivement doivent être davantage prises en considération dans le transfert des connaissances parce que les cliniciens sont effectivement, dans la plupart des cas, l’un des éléments du traitement. Les concepts publiés dans les communications scientifiques doivent tenir compte de cette réalité.
Résultats
Considérer le transfert des connaissances comme un processus de communication oblige à appliquer les théories contemporaines qui mettent l’accent sur la création d’un langage commun lors de la transmission des connaissances.
Conclusion
Dans ce contexte, la gestion des résultats crée un environnement d’apprentissage en adoptant des pratiques cliniques qui favorisent le transfert des connaissances tout en sachant que la démarche scientifique n’est ni la seule ni la principale détentrice des connaissances.
Mots clés: création de connaissances, transfert, gestion des résultats, résolution pratique
Introduction
As evidenced by this special issue, interest in how to better communicate the finding of science to the behavioural health care system has never been higher. Many terms have been used to describe this process including knowledge translation, knowledge transfer, implementation, and diffusion of innovation, among others (Bacher, 1991; Caplan, 1979; Landry, Lamari, & Amara, 2001; Lomas, 1993). At the heart of the issue is the observation that findings from research struggle to find traction in the process of evolving the health care system towards more effective practices. There are many reasons for these challenges including time and training of clinicians, ability to read and absorb research findings, business model support from continued learning, and so forth.
There are multiple approaches to managing communication between research and practice communities. Canadian Institutes of Health Research (CIHR) distinguishes two types of knowledge translation (KT)—end of grant KT and integrated KT. The former is the standard dissemination of research findings to practice communities while the later represents a different approach to research in which the ‘researchers and the research users’ work together to shape the research.
Part of the stimulus for increased interest in the ability of the treatment community to infuse scientific findings into practice has been the increased emphasis on using efficacious practices (e.g. treatments with established efficacy through clinical trials) and monitoring the effectiveness of behavioural health interventions in their application (i.e., outcomes management). With growing pressure to demonstrate the effectiveness of treatments and programs, it is natural for the behavioural health field to look to science to provide strategies to maximize results. However, the implementation of evidence-based practices and the use of outcomes management technologies approach the problem of system improvement from two somewhat different perspectives. The implementation of evidence-based practices involves identifying treatments and programs through research, usually clinical trials that can be implemented effectively in systems of care. The approach is consistent with CIHR’s first model of KT, the dissemination of research findings into practice communities.
Monitoring and managing the effectiveness of treatment systems, sometimes called practice-based evidence, seeks to use information collected in practice to inform decisions and create a culture of learning in clinical settings. It is this latter approach to knowledge translation that is the focus of the present paper. This is consistent with the CIHR integrated type of KT, although the CIHR definition, along with others, classifies all parties as either research ‘producers’ or ‘users’ (Mitton, Adair, McKenzie, Patten, & Perry, 2007). This language implies that knowledge comes from the producers and is applied by the users. A practice-based evidence approach makes less of a distinction between ‘production’ and ‘use’.
As implied by the use of the terms ‘producer’ and ‘user,’ knowledge creation is often characterized as a linear process from science to practice. While feedback loops are included in these models, the primary feedback from practice involves the challenges and successes of actually implementing the findings of science. In these models, the burden of establishing knowledge remains with the field of science. Field work fine tunes the applications of this knowledge. This model of knowledge translation can work quite well in the application of bench research to medical care. Scientific breakthroughs in the identification of pathogens that cause diseases facilitate the development of effective treatments or vaccines and allow science to inform medical care.
The situation is somewhat different in behavioural healthcare. First, there are no known pathogens of any psychiatric disorder. While all evidence-based practices have a theory of cause and effect that underlie the treatment approach (e.g. Cognitive Behavioural Therapy assumes that changes in thinking cause changes in emotions and functioning), there is no solid scientific evidence to confirm these theories. Second, the very nature of behavioural health interventions is relational. Regardless of the specific treatment approach, clinicians must establish strong, supportive relationships which serve as the context for any effective practice. While the doctor-patient relationship is important in healthcare, it is not the case that we believe, for example, that the potency of an antibiotic treatment is potentiated by the strength of this doctor-patient relationship. The same limitation applies to the surgeon-patient relationship for most surgical interventions.
On the other hand, it is generally a consensus that a good relationship is a necessary but insufficient condition for an effective behavioural health intervention. The clinician’s involvement in this form of treatment is fundamentally different than his/her physician colleagues’ involvement in medical care. Given these circumstances, the clinician is not so much a tactician who is learning from science and implementing in practice. They are far more directly and personally involved in the process. Third, the person with the behavioural health disorder is also a critical partner in this knowledge process. It is actually their knowledge-base that we seek to impact with knowledge translation activities. So, the effective communication among scientists, clinicians, and people with behavioural health challenges is the central challenge of knowledge translation in behavioural health. Given these circumstances, it may be useful to review concepts of communication theory as they relate to this challenge.
Current Theories of Communication
The field of communication is broad and diverse and often is organized along disciplinary lines which then struggle to share common theories and approaches (Anderson, 1996; Donsbach, 2006). However, over the past several decades communications has evolved as a field of inquiry. One of the early models of communication can be characterized as transmission theories. These models date back to the 18th century British Empiricists. In transmission theories, communication is the process by which information is transferred from one person’s mind to that of another (e.g., Rothenbuhler, 1998). It is the process by which a message may be sent and received. In this way of thinking, the study of communication focuses on how information is created and packaged and sent and then received and processed. Metaphorically, transmission models are much like understanding the postal service. Letters are considered, written, addressed, mailed, delivered, received, opened, read, and processed by a second party.
Among communications theorists, this example of a linear process of information transfer is becoming increasingly quaint. While the example of a letter was a common experience congruent with the communication theories of the time, today most 18 year olds may not have even written, let alone mailed, a letter. New forms of communication such as email, texting and instant messages have reduced our reliance on letters as a form of communication. These new communication options also reveal the limits of transmission theories of communication.
It is worth noting that the transmission model of communication is congruent with the generic model of psychotherapy outcomes proposed by Howard et al. (1986). As shown in Figure 1.1 this general model of understanding mental health services, there components of the process are considered—input, throughout, output.
Figure 1.
The Generic Model of Psychotherapy (Howard, et al., 1986)
Using this generic model, the authors’ discussed how to study components at each of the three stages of the process. Input characteristics include client characteristics and provider characteristics, geographic consideration etc. “Thru put” characteristics include things like the nature of the treatment approach, the development of a therapeutic bond (i.e. the quality and strength of the relationship between the therapist and client), dose (i.e., the number of sessions of therapy received) and so forth. And output characteristics refer to outcomes from the therapeutic process including such things as remoralization, improved subjective well-being, symptom relief and functional improvement and would also include things such as therapist reimbursement, consumer satisfaction and future referrals of friends and acquaintances to the therapist. The linear process described in the generic model is consistent with the linear construction of the transmission models of communication. The limitations are the same. The model has no mechanism to describe any impact thru put or output processes might have on input characteristics. For example, referrals to an outpatient psychotherapist often come from satisfied clients of that therapist who have friends or family seeking help. Referral to a specific therapist from a friend who was helped by that therapist likely potentiates a different therapeutic process than does referral from a stranger.
Although transmission theories of communication remain common, recently some theorists have identified these models as conceptually flawed. Transmission theories tend to be simplistically linear as information (in our case knowledge) is viewed as moving from point A to point B and these theories struggle to include inputs from point B that might actually change the nature of information coming from point A (Carey, 1989). Some theorists (e.g. Deetz, 1994; Pearce, 1989) have proposed a constitutive model which conceptualizes communication as a meaning making activity. In this view communication is a process that produces and reproduces shared meaning. This conceptual model of communication has a great deal of utility for understanding the challenges of knowledge translation applications. The idea that effective communication is making shared meaning among multiple parties reveals the primary goal of knowledge translation but also suggests that linear transmission based strategies may not be optimally effective. Knowledge is not the possession of science that is awarded to practitioners and those they serve; it is created between these perspectives in the process of making meaning. This phenomenon then is better described as knowledge creation rather than translation and it consistent with the iterative CIHR Knowledge to Action process.
The concepts of constitutive communication have been embedded into business world through the work of Tapscott and Williams (2006) on mass collaborative. A core concept within this work is the concept of collective intelligence (c.f. Weiss, 2005). Collective intelligence is the shared intelligence that arises from a network of collaborators or competitors. It is reasonable to propose that knowledge translation is optimally intended to reach a collective intelligence. New media, particularly the Internet, creates opportunities for the evolution of collective intelligence by dramatically enhancing our capacity to communicate more rapidly, broadly, and interactively (Flew, 2008).
If one accepts the premise that enhancing effective practice involves a constitutive communication between scientists and clinicians, then what implications might that have for the field of knowledge translation in behavioural health. The primary implication is that clinicians have a knowledge base that comes from their experiences and that this information is just as much knowledge as the findings of rigorous bench research or the results of a randomized clinical trial. To fail to understand the importance of this experiential form of knowledge, particularly to the individual clinician, would be an error. However, the clinician’s knowledge is far more intuitive and personal than knowledge gleaned from the scientific enterprise. Since these forms of knowledge are quite different, their synthesis is challenging.
One strategy to improve the synthesis of knowledge developed from science and knowledge development from practice is to apply some scientific standards to monitoring practice and provide feedback to clinicians regarding their work in a fashion that is not inconsistent with the form and structure of information that comes from scientific research. This process has been referred to as practice-based evidence. Practice-based evidence involves monitoring the outcomes from clinical interventions as they happen to provide information to those involved in these interventions about the impact of their efforts. Practice-based evidence is one of the outputs of outcomes management approaches. There are many approaches to outcomes management in behavioural health (e.g., Doucette, 2004; Grissom, 2000; Lambert, 2007; Miller & Duncan, 2009), the most comprehensive approach is called Total Clinical Outcomes Management (TCOM, Lyons, 2004). TCOM frames its outcome measurement process within a constitutive communication framework (Lyons, 2009). “Total” refers to the fact that the information should be fully embedded in all aspects of the system from treatment planning to the creation of funding mechanisms and business models. “Clinical”, although risking some potentially unintended connotations, is a term used to indicate that the information is about the people served not the services provided (in counterpoint to quality management strategies). “Outcomes” implies that the information is focused on factors that are relevant to assessing the transformational impact of interventions. “Management” implies that the information is actively used to make decisions at all levels of the system.
Total Clinical Outcomes Management
The TCOM framework is best understood as a philosophy, a strategy, and a set of tactics. From a conceptual perspective, behavioural healthcare is a business enterprise that seeks to do good work by addressing the emotional and behavioural needs of people with psychiatric disorders. Behavioural healthcare often serves as a safety net for those of us who are at a point in their lives where they are struggling. Helping these individuals in their moment of need is the core principle of all behavioural health enterprises. To better serve people with behavioral health needs, it is first important to know what they need. This knowledge is a shared understanding between the person and the behavioral healthcare provider. Next, a decision must be made of what intervention approaches are indicated to address the identified needs. Then, it is important to be able to manage the enterprises with information about the degree to which the individual’s needs have been met. If the needs are not met then a different intervention approach is recommended. In all cases the challenge of the behavioural health enterprise is to keep the work focused on the understood needs of the individual or family in care. Thus the philosophy of TCOM is that the behavioural health system, at all levels, should always make decisions based on the needs and well-being of the people served.
Philosophy
The TCOM approach is grounded in the concept that the various perspectives in a complex service system create tensions. For example, the person providing the treatment often has a different perspective than those responsible for paying for the treatment. Within treatment teams, people from different disciplines often see the treatment process differently. The conflicts that results from these tensions are best managed by keeping a focus on common objectives—a shared vision. In behavioural healthcare, the shared vision is the person (or people served). In health care, the shared vision is the patient; in the child serving system, it is the child and family, and so forth. By creating systems that have the capacity to always return to this shared vision, it is easier to create and manage effective and equitable systems. In other words, the behavioural healthcare system should be about people with behavioural health needs and their families.
A secondary aspect of the philosophy is that all partners in the Behavioural Health system share the same vision of helping those with emotional and behavioural needs. Regardless of whether you are a psychiatrist, psychologist, social worker, case manager, case worker, Ministry representative, or parent, everyone involved in the system wants to see those in need benefit from the treatments and interventions provided. As such, a mass collaboration model is ideal when that model focuses on this shared vision. TCOM is always practiced within the mass collaboration model with strategies and tactics existing in the open domain, free to use by anyone within the system.
Strategy
Creating a system that remains always about the shared vision requires an approach that supports the communication of this shared vision throughout the system of care. Since the shared vision is the person (or people) served, it is necessary to effectively represent these individuals through the behavioural healthcare system. To accomplish this objective, a structured assessment is created that directly informs service/intervention planning. This assessment tool is used to communicate the shared vision throughout the system. Since the individuals working directly with the people that are in the best position to already make their decisions based on the shared vision (the people they are serving), it is critical that the structured assessment is useful to them so that it is completed with reliability and validity. By viewing assessment in these settings as a constitutive, ‘meaning-making’ process between the individual or family in need and the people trying to help, TCOM seeks to provide the strategy to support the ongoing creation of knowledge about how best to serve people with behavioral health challenges.
We have used assessments designed from a communimetric perspective (Lyons, 2009) in which individual items are used to represent different treatment/intervention needs and the levels of each item directly translate into actions. For example, the standard four level communimetric items has the following four action levels:
0 No evidence, no need for action
1 Watchful waiting/prevention
2 Action, need is interfering in a notable way with functioning
3 Immediate or intensive action, dangerous or disabling
By using an action oriented measurement process for the standard assessment, it is possible to create a measurement approach that is immediately and directly relevant to both clinicians and the people they serve. Further, the approach to creating the output from this assessment process is the first opportunity to established shared meaning. The assessment process should be done collaboratively with people served and their families. It is not a diagnosis provided by an expert, it is a consensus on actionable needs and strengths among all parties involved in the care of the person and/or family.
Tactics
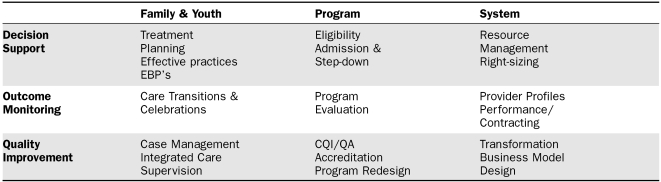
Figure 2 displays example TCOM tactics. This grid is organized by types of applications of information from the structured assessment in the rows to levels of the system in the columns. The idea is that one strategy (i.e. the common assessment) can be used to perform a variety of activities at different levels of the system, from service planning at the individual level to resource management at the system level.
Figure 2.
TCOM Grid of Tactics
Given the action orientation of the common assessment strategy, its link to treatment plan should be clear. At the program level, patterns of actionable needs have a demonstrated relationship to the likely effectiveness of various program types. And at the system level, mapping recognized needs with currently available treatment resources allows for the ‘right sizing’ of a service system. A system level TCOM application involves identifying the physical location of people with a specific need relative to the physical location of providers who are capable of addressing that need. This strategy is referred to as “geomapping.” When geomapping strategies are utilized, this ‘right sizing’ can occur in space as well. For example, Weiner (2008) demonstrated that the location of youth in Chicago who required group home placement was very different than the location of group homes in the city.
In complex systems, most people with multiple needs utilize help from multiple providers. A common assessment strategy allows the assessment at the end of one episode of care to be the starting point of the next. This transition is the outcome monitoring at the individual level. In other words, the discharge assessment from an inpatient hospital stay should be the starting assessment for post-discharge community-based care. In addition, each episode of care can celebrate successes with the involved individuals.
Practitioners often think of structured measurement as only serving a program evaluation function. Viewing the TCOM grid of tactics reveals that program evaluation, while important, is only one application of information in the system of care. Outcomes at the system level can involve performance-based contracting which has been used to reward programs that engage in the most effective practices. And quality improvement and system transformations can be understood within the same framework and informed by the same structured assessment approach. While the focus of this paper has been predominantly on the role of outcomes management in knowledge translation at the individual practitioner level, similar principles apply at each level of the system.
The combination of the philosophy, strategy and tactics of TCOM allows a complex system of care to come together to create a learning environment in which information (i.e. data if you are a scientist) can be used to inform the management of care for an individual person and an entire system simultaneously. This approach creates the type of ongoing learning environment in which the integration of findings from scientific endeavors can be natural and straightforward. TCOM does not remove the important roles of various people in the knowledge translation process (e.g. opinion leaders, facilitators, champions, linking and change agents; Thompson, Estabrooks, & Degner, 2006). Rather the approach supplies these actors with information to facilitate their impact on facilitating behavior change. In this way, TCOM can be thought of as a special case of community-based participatory research (c.f. Park, 1999).
Implications
There is a growing body of evidence that using practice-based evidence in concert with knowledge of evidence-based practice is a powerful strategy for improving the functioning of behavioural healthcare systems. For example, the application of TCOM tactics as displayed in Figure 2 has been used to improve results in a number of different jurisdictions. For example, program eligibility models have been used to improve the match between youth and admission to residential treatment centers resulting in improved performance of these centers over time. The approach also has been used to enhance placement stability in child welfare in other jurisdictions and reduce the number of unnecessary psychiatric hospitalizations. In Illinois, the approach is being used to create a trauma-informed system of care throughout the child welfare system so that all children who come into custody of the state will have access to effective practices to identify and address trauma stress symptoms should they occur. Applications of the approach with geomapping technology allow real time identification of nearby providers who have training in specific evidence-based practice for a specific child. This same system allows the identification of the mismatch between the location of available service providers and children and youth with specific needs (Weiner, 2008). In sum, working to always keep the system focused on its shared vision and mission is an effective strategy for overcoming many of the tensions that impede our progress.
In Canada, the Children’s Hospital of Eastern Ontario has used TCOM to redesign its inpatient program for children and bring in effective practices for the identified needs of the children served (Greenham & Bisnaire, 2008). This process has involved creating a common assessment process that is embraced by both clinical and management staff. This assessment process is used for planning interventions in hospital and supporting effective transitions at discharge. Aggregate data from the assessment has been used to redesign practices on the units. A primary challenge has been to get clinical staff comfortable with constitutive communication approach to assessment whereby multiple professionals and parents are involved in the assessment process. This approach is counterpoint to traditional expert diagnostic strategies that are a standard in healthcare. A secondary challenge has been securing sufficient resources to allow for the timely use of the assessment information in various aggregates.
The advantage of a practice-based evidence approach as a knowledge transfer approach is that it builds on the experiential context of the practitioner. Common assessments provide structure as to what should be attended to in interactions with people served. The constitutive nature of the assessment process reinforces the learning culture philosophy of the approach. Information taken directly from their experiences is fed-back in an organized fashion. If they are providing effective interventions, there is little need to adopt a different practice. If they are not effective, in general or with particular types of people, then a credible context for a change in practice is clearly established within their experiential set.
Conclusion
Most agree with Caplan’s (1979) observation of that the two communities—one of researchers and the other of practitioners remain apart (Schryer-Roy, 2005). If we are truly to achieve one community, it will be important for the field of science to embrace the reality that science is one strategy for the creation of knowledge but that other strategies exist and have value. It is equally important for practitioners to recognize the value of findings from scientific research to their clinical practice and that intuition is sometime overly influenced by more vivid experiences that do not represent the norms of practice. In the final analysis both parties work in service to people with behavioural health needs. Always returning to this core value of the system is fundamental to creating a learning environment in which all partners work together, respecting the contribution of others, to achieve the goals of accessible and effective behavioural healthcare for those in need. This is collective intelligence and that is the essence of knowledge translation.
Acknowledgements/Conflict of Interest
The authors have no financial relationships or conflicts to disclose.
References
- Anderson JA. Communication theory: Epsitemological foundations. New York: Guildford Press; 1996. [Google Scholar]
- Bacher T. Knowledge utilization: The third wave. Knowledge. 1991:225–240. [Google Scholar]
- Brown P, Lauder H. Collective Intelligence. In: Brown, Lauder, editors. Capitalism and social progress: the future of society in a global economy. Hamshire; United Kingdom, Palgrave: 2001. [Google Scholar]
- Caplan N. The two communities theory and knowledge utilization. American Behavioural Scientist. 1979;23:4. [Google Scholar]
- Carey JW. Communication as culture: Essays on media and society. Winchester MA: Unwin Hyman; 1989. [Google Scholar]
- Deetz SA. Future of the discipline: The challenges, the research, and the social contribution. In: Deetz SA, editor. Communication Yearbook. Vol. 17. Thousand Oaks, CA: Sage; 1994. pp. 565–600. [Google Scholar]
- Donsbach W. The identify of communications research. Journal of Communication. 2006;56:437–448. [Google Scholar]
- Doucette A. Child/adolescent measurement system. CAMS: user manual; Nashville, TN: 2004. [Google Scholar]
- Flew T. New Media: An introduction Melbourne. Oxford University Press; 2008. [Google Scholar]
- Greenham S, Bisnaire L. An outcome evaluation of an inpatient crisis stabilization and assessment program for adolescents. Residential Treatment for Children and Youth. 2008;25:123–144. [Google Scholar]
- Grissom G. Behavioral Outcomes and Guidelines Sourcesbook. New York: Faulkner & Gray; 2000. The advent of outcomes management and the culture of measurement. [Google Scholar]
- Howard KI, Kopta M, Krause MS, Orlinsky DE. The dose-effect relationship in psychotherapy. American Psychologist. 1986;41:159–163. [PubMed] [Google Scholar]
- Lambert M. Presidential address: What we have learned from a decade of research aimed at improving psychotherapy outcomes in routine care. Psychotherapy Research. 2007;17:1–14. [Google Scholar]
- Landry R, Lamari M, Amara N. Extent and determinants of utilization of University research in Government agencies. Public Administration Review. 2001;63:193–205. [Google Scholar]
- Lumas J. Diffusion, dissemination, and implementation: who should do what? Annals of the New York Academy of Sciences. 1993;703:226–235. doi: 10.1111/j.1749-6632.1993.tb26351.x. [DOI] [PubMed] [Google Scholar]
- Lyons JS. Redressing the emperor: Improving our children’s public mental health service system. New York: Praeger; 2004. [Google Scholar]
- Lyons JS. Communimetrics: A theory of measurement for human service enterprises. New York: Springer; 2009. (forthcoming) [Google Scholar]
- Miller SD, Duncan BL. The Institute for the Study of Therapeutic Change. 2009 www.talkingcure.com.
- Mitton C, Adair CE, McKenzie E, Patten SB, Perry BW. Knowledge transfer and exchange: Review and synthesis of the literature. The Milbank Quarterly. 2007;85:729–768. doi: 10.1111/j.1468-0009.2007.00506.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park P. People, knowledge, and change in participatory research. Management Learning. 1999;30:141–157. [Google Scholar]
- Pearce WB. Communication and the human condition. Carbondale: Southern Illinois University Press; 1989. [Google Scholar]
- Rothenbuhler EW. Ritual communication: From everyday conversation to medical ceremony. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Tapscott D, Williams AD. Wikinomics: How mass collaboration changes everything. New York, Penguin; Group: 2006. [Google Scholar]
- Thompson GN, Estabrooks CA, Degner LF. Clarifyin the concepts of knowledge transfer: a literature review. The Authors. 2006:691–701. doi: 10.1111/j.1365-2648.2006.03775.x. [DOI] [PubMed] [Google Scholar]
- Weiner DA. Developing a trauma informed child welfare system. Presented to the 5th annual CANS Conference; Nashville, TN. September 29th.2008. [Google Scholar]