“We have in hand most of the information we need to facilitate a new golden age of medicine. And what we don’t have in hand we can get fairly readily by wise investment in targeted research and intervention.” This “dangerous idea” (Ewald, 2007) was put forward by Paul Ewald, an evolutionary biologist. His idea has merit and is consistent with the way we, at the Canadian Institutes of Health Research, think about knowledge translation, which is our term for closing the gap between what we know from research and what we do.
From our perspective, knowledge translation (KT) is about making users aware of knowledge or innovations and facilitating their use of it to improve health and health care systems. It is about closing the gap between what we know and what we do (reducing the know-do gap) and about moving knowledge into action. There are other terms in use to describe this concept, many of which are not operationally defined (Tetroe et al., 2008; Graham I.D. et al., 2006) but, at the CIHR, we have developed the following working definition: “Knowledge translation is a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically sound application of knowledge to improve the health of Canadians, provide more effective health services and products and strengthen the health care system. This process takes place within a complex system of interactions between researchers and knowledge users which may vary in intensity, complexity and level of engagement depending on the nature of the research and the findings as well as the needs of the particular knowledge user.” An examination of the meaning of the specific concepts in this definition allows a more in-depth understanding of what we mean by KT.
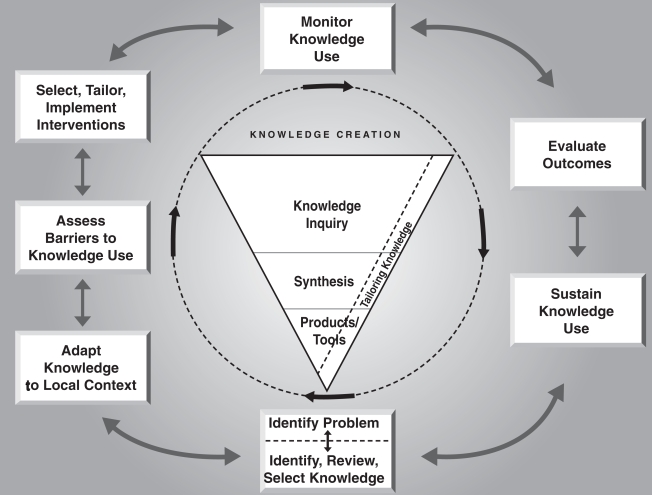
Synthesis in this context means the contextualization and integration of research findings of individual research studies within the larger body of knowledge on the topic. A synthesis must be reproducible and transparent in its methods, using quantitative and/or qualitative methods. It could take the form of a systematic review; follow the methods developed by the Cochrane or Campbell Collaborations, or other methods; and may synthesize qualitative or quantitative findings. Meta-analyses, realist reviews, narrative syntheses, meta-syntheses and practice guidelines are all forms of synthesis. Dissemination involves identifying the appropriate audience, and tailoring the message and medium to the audience. Dissemination activities can include such things as summary/briefings to stakeholders, educational sessions with patients, practitioners and/or policy makers, engaging knowledge users in developing and executing dissemination/implementation plan, tools creation, and media engagement. The exchange of knowledge refers to the interaction between the knowledge user and the researcher resulting in mutual learning through the process of planning, producing, disseminating, and applying existing or new knowledge. Ethically sound knowledge translation activities are those that are consistent with ethical principles and norms, social values as well as legal and other regulatory frameworks- while keeping in mind that principles, values and laws can compete among and between each other at any given point in time. The term application is used to refer to the iterative process by which knowledge is put into practice or policy and has been illustrated in the action cycle of the knowledge to action process (see Figure 1) Implicit in the CIHR definition is the notion that evaluation and monitoring of KT initiatives, processes, and activities are key components of KT.
Figure 1.
The Knowledge to Action Process
Figure 1, page 19, Graham, I.D., Logan, J., Harrison M.B., Straus, S, Tetroe, J.M., Caswell, W., et al. (2006). Lost in knowledge translation: time for a map? Journal of Continuing Education in the Health Professions, 26, 13–24. Reprinted with permission.
Given the complexity of behavior change and the multiple factors that can influence it in positive and negative ways, there is growing recognition that application efforts could and should be guided by conceptual models or frameworks (McDonald et al., 2004; The Improved Clinical Effectiveness through Behavioural Research Group (ICEBeRG), 2006). The usefulness of conceptual models comes from the organization they provide for thinking, for observation, and for interpreting what is seen. They provide a systematic structure and a rationale for activities and have the basic purpose of focusing, ruling some things in as relevant and ruling others out due to their lesser importance. The Knowledge to Action Process, which guides our understanding of KT, was derived from a concept analysis of 31 planned action theories and models (Graham & Tetroe, 2009; Graham & Tetroe, 2007).
In CIHR’s view, knowledge translation can be divided into three broad categories; KT Science -studying the determinants of knowledge use and effective methods of promoting the uptake of knowledge, end of grant KT – initiatives undertaken once the grant/research has been completed and integrated KT (iKT) - initiatives woven into the research process. End of grant KT refers to the standard KT activities of most researchers: KT to their peers such as conference presentations and publications in peer-reviewed journals. But CIHR also encourages end of grant dissemination activities that tailor the message and medium to a specific audience, such as summary briefings to stakeholders; educational sessions with patients, practitioners and/or policy makers; media engagement and the use of knowledge brokers to get the findings to relevant audiences. Integrated KT at CIHR represents a different approach and involves collaboration between researchers and research users in the research process including the shaping of the research questions, deciding the methodology, involvement in the data collection and tools development, interpreting the findings and helping disseminating the research results. Research users could be other investigators from difference disciplines, teams or countries but more often are policy makers, decision makers, research funders, industry, clinicians or the public. This category of KT is similar to participatory research (Macaulay et al., 1999), or Gibbons’ Mode 2 knowledge production (Gibbons et al., 1994) in that it includes “a wider, more heterogeneous set of practitioners, collaborating on a problem defined in a specific and localized context”(Gibbons et al 1994, page 3). It is not our view that every researcher should be involved in integrated KT. For many researchers, disseminating research findings to the appropriate audience (this includes other researchers) is usually sufficient. In cases where more intense knowledge translation is warranted to roll out research findings proven to be effective, this can take place at the end of the grant or in a more integrated fashion – depending on the circumstances. The intensity of knowledge translation would depend on factors such as the potential importance/impact of using the findings; the strength of the evidence supporting the findings (synthesis); the target audience(s); what is known about effective strategies to reach the audience(s); what is practical and feasible to do under the circumstances and considerations of who else should be involved in KT efforts.
What does all this have to do with Paul Ewald’s quote? “We have in hand most of the information we need to facilitate a new golden age of medicine.” In line with the views of Paul Ewald, we need syntheses to determine what we already know (or should know). Tens of thousands of medical research articles are published every year. Through synthesis and systematic reviews, we can sift the wheat from the chaff to determine areas requiring clear action based on strong evidence. For example, Choripta et al. (Chorpita et al., 2007) pointed out the need for the widespread promotion and implementation of treatments with a strong evidence base, in both scientific and applied research in psychology and psychiatry. To facilitate this, they developed a distillation and matching model to provide a means for clinicians to identify evidence-based treatments. Similarly, Thomas (Thomas, 2006), demonstrated the value of searching the Cochrane Library’s Database of Systematic Reviews as a source of synthesized evidence on treating conduct disorder. Finally, Fergusson et al (Fergusson et al., 2005) conducted a systematic review, which documented an association between suicide attempts and the use of SSRIs, which would have not been known without combining the results of many studies. Their cumulative meta analysis further reinforced concern with the potential trend towards harm with this class of drugs.
“….And what we don’t have in hand we can get fairly readily by wise investment in targeted research and intervention.” When research gaps are identified through synthesis, the appropriate people need to be involved from the beginning in order to conduct applied, collaborative, interdisciplinary research – in other words – iKT. Today’s health problems are complex and interdisciplinary and require mixed methods to solve them. Furthermore, research users need to be involved in setting the research agenda and defining the research questions to ensure relevance and greater likelihood of uptake of the findings when they become available. With their input, relevant research can be fostered and encouraged through appropriate targeted funding.
But even if relevant research is being funded and conducted, once the results are in, they are not “one size fits all.” This is equally true of clinical practice guidelines, systematic reviews and quality improvement initiatives. Users need to adapt and take ownership of knowledge for local use. In health care, use of research is not only influenced by the evidence itself, but by existing resources, patient preferences, and clinical expertise (DiCensco & Cullum, 1998; Cullum et al., 2007). The knowledge to action cycle (Graham I.D. et al., 2006) demonstrates how adaptation can be incorporated into the implementation process.
Getting evidence into policy and practice: Perspective of a health research funder
Knowledge translation is a means of moving evidence to policy and practice. But our examination of what precisely is meant by this term has revealed some of the intricacies and complexities involved in making this leap. First, we need to be sure we have a strong evidence base and that we have considered the opportunity costs of implementing it. Next, having identified gaps for targeted research, we need to ensure that the appropriate people are involved in conducting that research and that those involved in implementation research, in particular, should collect robust performance measurement data. This could contribute to much-needed research on intervention design, implementation and evaluation of knowledge use, as well as to improved health and health services and products. Finally, evidence needs to be tailored and adapted for use in the local policy and practice environment. As research funders, we at CIHR are committed to funding syntheses as well as end of grant and integrated knowledge translation research as part of fulfilling our KT mandate (see Table 1). We encourage our researchers to disseminate their research results to the appropriate audiences and to consider the impact of their work within the context of existing knowledge.
Table 1.
Funding Opportunities for KT at CIHR
| KT Focus | Funding mechanisms |
|---|---|
| Synthesis |
|
| Integrated KT |
|
| End of Grant KT |
|
| Science of KT |
|
The knowledge to action process derived from our theory analysis can be used to form a theoretical underpinning to these knowledge translation efforts and at the very least can be used as talking points with the research end-users in order to facilitate the implementation process and ultimately, to facilitate the uptake of evidence-based practice and improved health outcomes. Implementation research will be enabled to take huge strides forward when KT scientists develop standardized and valid outcome measures of knowledge/research use as well as validated measures of potential predictor variables related to KT best practice. We need to be able to simultaneously consider the individual and group level when measuring and predicting knowledge/research-use.
Knowledge translation is an important part of the CIHR mandate and through our funding opportunities and messaging, we are determined to increase the capacity in Canada to close the gap between what we know and what we do.
Acknowledgements/Conflict of Interest
The ideas in this paper were based on an invited plenary at the Joanna Briggs Institute 2007 International Convention, Adelaide, Australia November 26th – 28th).
References
- Chorpita BF, Becker KD, Daleiden EL. Understanding the common elements of evidence-based practice: misconceptions and clinical examples. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:647–652. doi: 10.1097/chi.0b013e318033ff71. [DOI] [PubMed] [Google Scholar]
- Cullum N, Ciliska D, Haynes BH, Marks S. Evidence-Based Nursing: An Introduction Wiley- Blackwell; 2007. [Google Scholar]
- DiCensco A, Cullum N. Implementing Evidence-based nursing: some misconceptions. Evidence-Based Nursing. 1998;1:38–40. [Google Scholar]
- Ewald P. A New Golden Age of Medicine. In: Brockman John., editor. What is your dangerous idea? Toronto: Harper Perennial; 2007. pp. 84–89. [Google Scholar]
- Fergusson D, Doucette S, Glass KC, Shapiro S, Healy D, Hebert P, et al. Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials. BMJ. 2005;330:396. doi: 10.1136/bmj.330.7488.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons M, Limoges C, Nowotny H, Schwartzmann S, Scott P, Trow M. The new production of knowledge: The dynamics of science and research in contemporary societies. London: Sage; 1994. [Google Scholar]
- Graham ID, Logan J, Harrison MB, Straus S, Tetroe JM, Caswell W, et al. Lost in knowledge translation: Time for a map? Journal of Continuing Education in Health Professions. 2006;26:13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
- Graham ID, Tetroe J. Some theoretical underpinnings of knowledge translation. Academic Emergency Medicine. 2007;14:936–941. doi: 10.1197/j.aem.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Graham ID, Tetroe JM. Theories of Knowledge to Action: Planned Action Theories. In: Straus S, Tetroe JM, Graham ID, editors. Knowledge Translation in Health Care Moving from Evidence to Practice. London: Wiley-Blackwell; 2009. [Google Scholar]
- Macaulay AC, Commanda LE, Freeman WL, Gibson N, McCabe ML, Robbins CM, et al. Participatory research maximises community and lay involvement. North American Primary Care Research Group. BMJ. 1999;319:774–778. doi: 10.1136/bmj.319.7212.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald K, Graham I, Grimshaw J. Toward a Theoretic Basis for Quality Improvement Interventions. In: Shojania KG, McDonald K, Wachter R, Owens D, editors. Closing the quality gap: a critical analysis of quality improvement practices (Vol 1: diabetes mellitus and hypertension) Technical review #9 ed. Washington, DC: AHRQ; 2004. [Google Scholar]
- Tetroe JM, Graham ID, Foy R, Robinson N, Eccles MP, Wensing M, et al. Health research funding agencies’ support and promotion of knowledge translation: an international study. Milbank Q. 2008;86:125–155. doi: 10.1111/j.1468-0009.2007.00515.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Improved Clinical Effectiveness through Behavioural Research Group (ICEBeRG) Designing theoretically-informed implementation interventions. Implementation Science. 2006;1 doi: 10.1186/1748-5908-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas C. Evidence-based practice for conduct disorder symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:109–114. doi: 10.1097/01.chi.0000184928.33799.60. [DOI] [PubMed] [Google Scholar]