Abstract
Torsade de pointes occuring due to a long QT interval is a rare but potentially fatal arrhythmia. Acquired long QT develops most commonly because of drugs that prolong ventricular repolarization. It has been reported that fluoroquinolone antimicrobials prolong the corrected QT interval but rarely cause torsade de pointes. A patient with torsade de pointes risk factors (female sex, advanced age, extreme bradycardia and renal failure) who developed the condition on the fourth day of 400 mg/day of oral moxifloxacin treatment is presented. After the moxifloxacin was stopped, the corrected QT interval normalized and a permanent cardiac pacemaker was implanted. During 11 months of follow-up, arrhythmia did not recur.
Keywords: Moxifloxacin, Torsade de pointes
Abstract
Les torsades de pointe attribuables à un intervalle QT long sont des arythmies rares, mais au potentiel fatal. D’ordinaire, les intervalles QT longs se manifestent en raison de médicaments qui prolongent la repolarisation ventriculaire. Il a été signalé que les fluoroquinolones, un antimicrobien, prolongent l’intervalle QT corrigé mais sont rarement responsables de torsades de pointe. On présente le cas d’une patiente ayant des facteurs de risque de torsades de pointe (sexe féminin, âge avancé, bradycardie extrême et insuffisance rénale) qui a souffert de ce trouble après avoir suivi un traitement de 400 mg/jour de moxiflocacine par voie orale pendant quatre jours. Après l’abandon de la moxifloxacine, l’intervalle QT corrigé s’est normalisé, et on a implanté à la patiente un stimulateur cardiaque permanent. L’arythmie ne s’est pas manifestée de nouveau au cours des 11 mois de suivi.
Along QT interval, which is the surface electrocardiogram (ECG) manifestation of a prolonged repolarization phase, is associated with an increased risk of torsade de pointes (TdP). If transient, it may present with syncope, and if is not transient, it may cause sudden death. A long QT interval may be congenital or acquired. The most common cause of an acquired long QT interval is drug administration (1). The drugs that interfere with potassium influx, commonly by blocking the human ether-a-go-go-related gene channel-dependent potassium current (as with fluoroquinolones) in myocyte membranes produce a prolongation of the corrected QT (QTc) interval and increase the risk of spontaneous arrhythmia generation (2). Fluoroquinolones have been reported to prolong the QTc interval and precipitate TdP in patients at high risk (1,3). We present a patient with bradycardia who developed TdP during oral moxifloxacin therapy for pneumonia.
CASE PRESENTATION
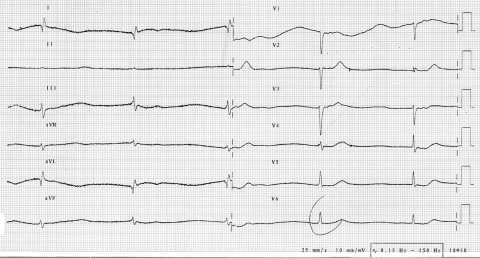
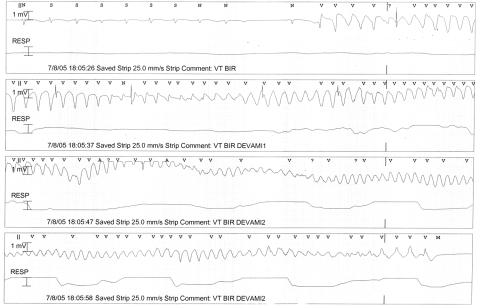
An 87-year-old woman with hypertension, chronic renal failure and dementia was admitted to the emergency department with presyncope. Junctional rhythm with a rate of 30/min was present on ECG, and the QT interval was 0.66 s; the QTc interval, according to Bazett’s formula, was 0.47 s (Figure 1). There were no previous ECGs performed. Medications she was using at the time of admission included ginkgo glycosides (19.2 mg/day), valsartan 80 mg plus hydrochlorothiazide (12.5 mg/day), acetylsalicylic acid (100 mg/day) and citalopram (20 mg/day). Her serum creatinine level was 283 μmol/L and potassium level was 4.2 mmol/L at admission. Other biochemical tests were normal. A temporary transvenous cardiac pacemaker was implanted and set to a rate of 60 beats/min. The pacemaker was turned off 24 h after the implantation because sinus rhythm resumed, but it was left in place in case of bradycardia. On that day, 400 mg/day oral moxifloxacin was prescribed to the patient for aspiration pneumonia. At the beginning of moxifloxacin treatment, the rhythm was normal, with normal QT (0.40 s) and QTc (0.43 s) intervals at a heart rate of 68 beats/min. The patient was transferred to the intensive care unit for telemetric follow-up due to the possible recurrence of symptomatic bradycardia. Intermittant junctional rhythms were observed on the monitor, but sinus rhythm was dominant. On the fourth day of moxifloxacin therapy, TdP developed following a short-long-short sequence of junctional rhythm (Figure 2) and recovered spontaneously after 36 s. The QT interval on the ECG taken on the same day was prolonged (QT 0.65 s, QTc 0.58 s) at a heart rate of 48 beats/min. Moxifloxacin was stopped, and the temporary pacemaker was turned on and set to a high rate. There were no electrolyte abnormalities when TdP developed. In the following days, a permanent dual-chamber pacemaker was implanted with an indication of symptomatic bradycardia and programmed to DDD mode at a rate of 75 beats/min with a long atrioventricular interval. The QT and QTc intervals returned to normal (0.39 s and 0.44 s, respectively) with a heart rate of 75 beats/min (atrial pacing) seven days after the cessation of moxifloxacin treatment. During 11 months of follow-up, QT prolongation and TdP did not recur.
Figure 1).
The electrocardiogram of the patient at admission. A junctional rhythm with a rate of 30 beats/min is seen. The QT interval was 0.66 s and the corrected QT interval was 0.47 s (the paper speed was 25 mm/s)
Figure 2).
Telemetry record showing torsade de pointes that terminated spontaneously after 36 s. A short-long-short sequence preceded the arrhythmia (the paper speed was 25 mm/s)
DISCUSSION
As a class, fluoroquinolones are generally well tolerated and safe. The adverse effects associated with fluoroquinolones most commonly include gastrointestinal disturbances, central nervous system reactions and dermatological effects, and these are reversible on cessation of treatment. Serious adverse events include photo-toxicity and QTc prolongation (4). Moxifloxacin, one of the third-generation fluoroquinolones, is a preferable antibiotic for its longer half-life, as well as its excellent activity against anaerobes and atypical pneumonia agents in recent years (4,5). Like all fluoroquinolones, moxifloxacin has the potential to prolong the QTc interval, but TdP is very rare (1,3,5). Although moxifloxacin prolongs the QTc interval more than the other fluoroquinolones levofloxacin and ofloxocin (6), TdP probability with moxifloxacin is lower than with these drugs (7). In a registry of more than one million patients receiving treatment with moxifloxacin, there has been only a single case of possibly associated TdP (1). The patient who experienced the arrhythmia was an 83-year-old woman with pre-existing hypokalemia, sick sinus syndrome with a cardiac pacemaker and coronary artery disease. It is recommended that drugs with the possibility to prolong QTc interval must be used cautiously in patients with risk factors (female sex, advanced age, underlying heart disease, electrolyte imbalance, concomitant drug use that prolongs the QTc interval, severe bradycardias and presence of other diseases) for TdP (1,3,5). Our patient can be classified as a high-risk patient for TdP due to her sex, advanced age and presence of extreme bradycardia at the time of hospital admission. The QT interval was prolonged (0.66 s), although the QTc interval was slightly longer (0.47 s) than the upper normal limit during bradycardia at admission. Here, the absolute QT interval is more accurate, because Bazett’s formula undercorrects at very slow heart rates (8). Prolonged bradycardia may cause QT prolongation and increase susceptibility to TdP development via inducing cardiac electrical remodelling (9). There were no previous ECGs performed on our patient to make a judgement about how long the bradycardia had persisted. If the bradycardia was presumed to have persisted for a long time, electrical remodelling might have decreased the threshold for the development of TdP. The QT interval that had normalized on the next day of emergency department admission was again prolonged by the fourth day of moxifloxacin therapy, and a short-long-short sequence initiated the TdP, and not at an extremely slow heart rate (Figure 2). Therefore, moxifloxacin was assumed to be the predisposing factor for the development of TdP, with its QT interval-prolonging effect, in addition to the above-mentioned risk factors. The use of the Naranjo adverse drug reaction probability scale (10) indicated a probable relationship (score of 5) between the TdP observed and moxifloxacin therapy in this patient. Citalopram has also been reported to prolong the QTc interval, but this occurs only at toxic doses (11). Our patient used citalopram at a low dose for a long time before the event, and it did not cause any QTc prolongation itself; therefore; we think that citalopram was not responsible for the TdP, but it might have assisted in its development.
CONCLUSION
In conclusion, the drugs that have the potential to prolong the QTc interval must be used cautiously in patients with multiple risk factors for TdP (female sex, advanced age, concomitant drug use that prolongs the QTc interval, severe bradycardias, presence of other diseases such as chronic renal failure, etc). If possible, an alternative drug that does not interfere with the QTc interval should be chosen.
REFERENCES
- 1.Ball P. Quinolone-induced QT interval prolongation: A not-so-unexpected class effect. J Antimicrob Chemother. 2000;45:557–9. doi: 10.1093/jac/45.5.557. [DOI] [PubMed] [Google Scholar]
- 2.Chiba K, Sugiyama A, Hagiwara T, Takahashi S, Takasuna K, Hashimoto K. In vivo experimental approach for the risk assessment of fluoroquinolone antibacterial agents-induced long QT syndrome. Eur J Pharmacol. 2004;486:189–200. doi: 10.1016/j.ejphar.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Owens RC, Ambrose PG. Torsades de pointes associated with fluoroquinolones. Pharmacotherapy. 2002;22:663–8. doi: 10.1592/phco.22.8.663.33201. [DOI] [PubMed] [Google Scholar]
- 4.Bertino J, Fish D. The safety profile of the fluoroquinolones. Clin Ther. 2000;22:798–817. doi: 10.1016/S0149-2918(00)80053-3. [DOI] [PubMed] [Google Scholar]
- 5.Démolis JL, Kubitza D, Tennezé L, Funck-Brentano C. Effect of a single oral dose of moxifloxacin (400 mg and 800 mg) on ventricular repolarization in healthy subjects. Clin Pharmacol Ther. 2000;68:658–66. doi: 10.1067/mcp.2000.111482. [DOI] [PubMed] [Google Scholar]
- 6.Noel GJ, Natarajan J, Chien S, Hunt TL, Goodman DB, Abels R. Effects of three fluoroquinolones on QT interval in healthy adults after single doses. Clin Pharmacol Ther. 2003;73:292–303. doi: 10.1016/s0009-9236(03)00009-2. [DOI] [PubMed] [Google Scholar]
- 7.Frothingham R. Rates of torsades de pointes associated with ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin. Pharmacotherapy. 2001;21:1468–72. doi: 10.1592/phco.21.20.1468.34482. [DOI] [PubMed] [Google Scholar]
- 8.Sagie A, Larson MG, Goldberg RJ, Bengtson JR, Levy D. An improved method for adjusting the QT interval for heart rate (the Framingham Heart Study) Am J Cardiol. 1992;70:797–801. doi: 10.1016/0002-9149(92)90562-d. [DOI] [PubMed] [Google Scholar]
- 9.Tsuji Y, Zicha S, Qi XY, Kodama I, Nattel S. Potassium channel subunit remodeling in rabbits exposed to long-term bradycardia or tachycardia: Discrete arrhythmogenic consequences related to differential delayed-rectifier changes. Circulation. 2006;113:345–55. doi: 10.1161/CIRCULATIONAHA.105.552968. [DOI] [PubMed] [Google Scholar]
- 10.Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 11.Catalano G, Catalano MC, Epstein MA, Tsambiras PE. QTc interval prolongation associated with citalopram overdose: A case report and literature review. Clin Neuropharmacol. 2001;24:158–62. doi: 10.1097/00002826-200105000-00007. [DOI] [PubMed] [Google Scholar]