Abstract
BACKGROUND:
Mitral insufficiency is known to occur in a substantial proportion of patients with heart failure. Its relationship with morbidity and mortality is poorly described.
METHODS:
The mortality and hospitalization for heart failure were retrospectively examined in patients who underwent baseline echocardiography in the Studies Of Left Ventricular Dysfunction (SOLVD) treatment and prevention trials. The presence and grade of mitral insufficiency was assessed, and patients with and without mitral insufficiency were compared.
RESULTS:
Patients with left ventricular dysfunction and mitral insufficiency had greater than twofold increased risk of death or admission for heart failure over two years (RR 2.38, 95% CI 1.43 to 3.97). This excess risk persisted after adjustment for the severity of heart failure, etiology and differences in treatment (RR 1.82, 95% CI 1.04 to 3.17; P=0.04). The presence of moderate mitral insufficiency versus no insufficiency was associated with even greater independent risk (RR 2.20, 95% CI 1.01 to 4.80; P=0.05). Results were consistent with binary and ordinal analysis of mitral insufficiency.
CONCLUSION:
The presence of mitral insufficiency in patients with left ventricular dysfunction is independently associated with adverse outcomes, including death and hospitalization for heart failure. This has potentially important clinical implications for the assessment and management of patients with heart failure.
Keywords: Congestive heart failure, Left ventricular dysfunction, Mitral insufficiency
Abstract
HISTORIQUE :
On sait que l’insuffisance mitrale se produit dans une proportion substantielle de patients atteints d’insuffisance cardiaque. Son lien avec la morbidité et la mortalité est peu décrit.
MÉTHODOLOGIE :
On a procédé à l’examen rétrospectif du taux de mortalité et des hospitalisations imputables à l’insuffisance cardiaque chez des patients qui avaient subi une échocardiographie de départ dans le cadre de l’essai de prévention et de traitement SOLVD des études du dysfonctionnement ventriculaire gauche. On a évalué la présence et le stade d’insuffisance mitrale et comparé les patients atteints et non atteints d’insuffisance mitrale.
RÉSULTATS :
Les patients atteints d’un dysfonctionnement ventriculaire gauche et d’insuffisance mitrale ont vu leur risque de décès ou d’hospitalisation en raison d’une insuffisance cardiaque plus que doubler sur une période de deux ans (RR 2,38, 95 % IC 1,43 à 3,97). Ce risque excédentaire persistait après rajustement, compte tenu de la gravité de l’insuffisance cardiaque, de l’étiologie et des différences de traitement (RR 1,82, 95 % IC 1,04 à 3,17; p = 0,04). La présence d’insuffisance mitrale modérée par rapport à l’absence d’insuffisance s’associait à un risque interdépendant encore plus élevé (RR 2,20, 95 % IC 1,01 à 4,80; p = 0,05). Les résultats étaient compatibles avec l’analyse binaire et ordinale d’insuffisance mitrale
CONCLUSION :
La présence d’insuffisance mitrale chez les patients atteints d’un dysfonctionnement ventriculaire gauche s’associe de manière indépendante à des issues négatives, y compris des décès et des hospitalisations attribuables à l’insuffisance cardiaque. Ce phénomène a des répercussions cliniques potentielles d’importance pour évaluer et prendre en charge les patients atteints d’insuffisance cardiaque.
Heart failure is a growing cause of morbidity and mortality around the world, and it is the final common pathway of a variety of cardiovascular disorders (1,2). There have been a large number of clinical trials of medical therapy for heart failure, and survival continues to improve (3,4). Despite these improvements, survival and quality of life in patients with advanced heart failure (New York Heart Association [NYHA] class III and IV) remains poor (5,6).
Mitral insufficiency is estimated to occur in up to one-half of patients with heart failure (7,8). The presence of mitral insufficiency in heart failure is known to be associated with poorer quality of life (6). A recent study from the Mayo Clinic (8) followed patients with and without ischemic mitral regurgitation after myocardial infarction. Mortality at two and five years was 15% versus 40% and 39% versus 62%, respectively (P<0.001 for both). Other recent studies have demonstrated adverse outcomes associated with mitral insufficiency in patients with left ventricular dysfunction (9–12).
In light of these recent findings and promising developments in the surgical treatment of heart failure (13), we decided to examine the prognostic significance of mitral insufficiency in heart failure patients using data from the Studies Of Left Ventricular Dysfunction (SOLVD) treatment and prevention trials (14).
METHODS
Patients
The present study was an analysis of 301 patients from the SOLVD trials who underwent echocardiographic evaluation as part of the echocardiography substudy. Results of the SOLVD trials have been published (14,15). Patients between 21 and 80 years of age with an ejection fraction greater than 35% (on angiography, echocardiography or radionuclide scan) were eligible for enrolment. Exclusion criteria included current use of an angiotensin-converting enzyme (ACE) inhibitor, contraindication to ACE inhibitor use, unstable angina thought to require revascularization, valvular disease requiring surgery, myocardial infarction within 30 days, serum creatinine levels higher than 177 μmol/L, severe pulmonary disease or another disease likely to limit survival. A total of 6797 patients were enrolled – 4228 in the prevention trial (mostly asymptomatic) and 2569 in the treatment trial (symptoms of overt heart failure).
After a run-in period, patients were randomly assigned to placebo or enalapril starting at 2.5 mg to 5 mg twice daily and increasing to a maximum of 10 mg twice daily as tolerated. Patients were followed for a mean of 41±7 months (15,16).
Echocardiography substudy
All echocardiographic studies were performed according to a standard protocol. A baseline study was done within 24 h of the eligibility visit (before treatment). Measurements taken included chamber size, left ventricular mass, and septal and posterior wall thickness ejection fraction; mitral insufficiency was also quantified. Follow-up echocardiograms were performed at four and 12 months. For the present study, all baseline echocardiograms were interpreted at the individual sites. Two hundred fifty-nine patients had echocardiographic studies considered to be adequate for interpretation (17). The present analysis is of these 259 patients.
Variables
Continuous variables recorded at baseline included age and ejection fraction. Other variables recorded included sex, medication use (ACE inhibitor, acetylsalicylic acid and beta-blocker), diabetes, atrial fibrillation, smoking status and hypertension (all at baseline) (Table 1). Mitral insufficiency (absent, grade 1, grade 2, grade 3 and grade 4) and NYHA functional class were recorded as categorical variables, also at the time of enrolment.
TABLE 1.
Patient baseline characteristics according to the presence of mitral insufficiency
| Characteristic | No mitral insufficiency (n=220) | Mitral insufficiency (n=39) | P |
|---|---|---|---|
| Age, years (mean ± SD) | 58±11 | 60±10 | 0.3 |
| Female sex, % | 13 | 26 | 0.04 |
| NYHA functional class, % | 0.03 | ||
| I | 40 | 18 | |
| II | 47 | 62 | |
| III/IV | 13 | 20 | |
| Ejection fraction (mean ± SD) | 0.27±0.07 | 0.27±0.06 | 0.5 |
| Ischemic etiology, % | 66 | 46 | 0.02 |
| Medical history, % | |||
| Hypertension | 32 | 44 | 0.2 |
| Diabetes | 12 | 21 | 0.2 |
| Atrial fibrillation | 11 | 8 | 0.6 |
| Current smoker | 21 | 13 | 0.2 |
| Medication use, % | |||
| Randomly assigned to enalapril | 48 | 49 | 0.9 |
| Beta-blocker | 12 | 13 | 0.9 |
| Digoxin | 41 | 47 | 0.5 |
| Acetylsalicylic acid | 47 | 26 | 0.01 |
| Diuretic | 57 | 45 | 0.02 |
NYHA New York Heart Association
Outcomes
The primary outcome of the SOLVD trials was all-cause mortality. In the current study, a composite end point of all-cause mortality or hospitalization for heart failure was used.
Statistical analysis
Statistical analyses were performed using Stata 6.0 (StataCorp LP, USA). Baseline characteristics of the patients with and without mitral insufficiency were compared using χ2 tests or t tests, as appropriate. Kaplan-Meier methods and log-rank tests were used to compare occurrence of events over time for patients with and without mitral insufficiency (18). Cox proportional hazard modelling (19) was used to estimate the univariate and multivariate associations between the presence and severity of mitral insufficiency with the outcome of death or hospitalization for heart failure. The primary outcome of interest was to compare clinical events (death or rehospitalization for heart failure) in those patients with any mitral insufficiency and those with no insufficiency. Results are presented as estimates of RR, as well as 95% CI surrounding these estimates.
RESULTS
The patients in the echocardiography substudy were similar to those in the entire SOLVD cohort. A greater proportion of the echocardiography patients were in the prevention arm of the study (69.8% versus 61.9%). Slightly more echocardiography study patients were receiving beta-blockers (22% versus 18%; P=0.06), vasodilators (38% versus 33%; P=0.08) or calcium channel blockers (38% versus 33%; P=0.1) at entry into the study. For the other variables examined, there was no significant difference between those in the echocardiography study and the remainder of the SOLVD patients (17).
Two hundred fifty-nine of 301 patients (86%) undergoing echocardiographic follow-up had adequate studies to assess mitral insufficiency. Thirty-nine patients (15%) had mitral insufficiency; none had grade 4 mitral insufficiency. Baseline characteristics of patients with and without mitral insufficiency were similar (Table 1). A greater proportion of the patients with mitral insufficiency were female and in NYHA functional class III or IV. Those without mitral insufficiency were more likely to have an ischemic etiology and to be using acetylsalicylic acid and diuretics at study entry.
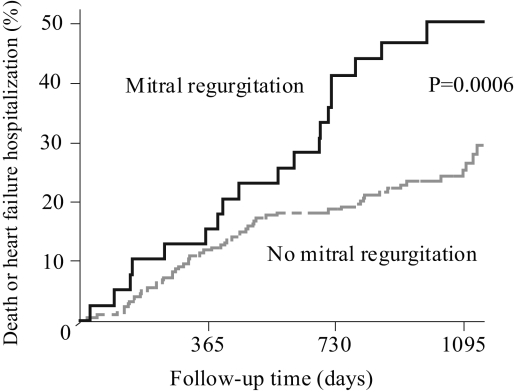
The incidence of all-cause mortality was 10 per 100 person-years for patients with mitral insufficiency and six per 100 person-years for patients without mitral insufficiency (P=0.17). The incidence of admission for heart failure was 15 per 100 person-years for patients with mitral insufficiency and 7.6 per 100 person-years for those without mitral insufficiency (P=0.03). Patients with mitral insufficiency were more likely to die or be admitted for heart failure. By two years, fewer than 20% of patients without mitral insufficiency had died or been hospitalized for heart failure, while more than 40% of those with mitral insufficiency had reached this composite end point (log-rank test, P=0.0006) (Figure 1).
Figure 1).
Kaplan-Meier analysis of cumulative events according to the presence of mitral insufficiency. The end point was a composite of death or hospitalization for heart failure. The 39 patients with mitral insufficiency were significantly more likely than the 220 patients without mitral insufficiency to reach the composite end point (P=0.0006, logrank test)
In univariate Cox proportional hazard analysis, the presence of mitral insufficiency of any grade compared with no mitral insufficiency was associated with a 70% increase in the composite outcome of death or hospitalization for heart failure (Table 2). After adjustment for age, sex, ejection fraction, etiology of heart failure, presence of atrial fibrillation at baseline, history of hypertension or diabetes, medication use and NYHA class, the presence of mitral insufficiency remained independently associated with an increased risk of death or hospitalization for heart failure (RR 1.49, 95% CI 1.05 to 2.11) (Table 2). Results were similar for mitral insufficiency as a binary variable (no mitral insufficiency versus any mitral insufficiency), with an 82% increase in the risk of death or hospitalization for heart failure (RR 1.82, 95% CI 1.04 to 3.17). The risk is more pronounced for patients with grade 2 or 3 mitral insufficiency at baseline compared with those with no mitral insufficiency, with a 120% increased risk after adjustment for baseline differences (RR 2.20, 95% CI 1.01 to 4.80) (Table 2). Patients with only grade 1 mitral insufficiency compared with those without insufficiency were more likely to reach the composite end point, although this was not statistically significant. The association between mitral insufficiency and death or hospitalization for heart failure was consistent across different categories of the mitral insufficiency variable and appeared to increase with increasing severity of mitral insufficiency.
TABLE 2.
Results of the multivariate analysis for the composite end point of death from all causes or hospitalization for heart failure*
| RR (95% CI) | P | |
|---|---|---|
| Mitral insufficiency (0, 1, 2, 3) – ordinal | ||
| Univariate | 1.70 (1.27–2.30) | <0.001 |
| Multivariate | 1.49 (1.05–2.11) | 0.03 |
| Mitral insufficiency (≥1 versus 0) – binary | ||
| Univariate | 2.38 (1.43–3.97) | 0.001 |
| Multivariate | 1.82 (1.04–3.17) | 0.04 |
| Mitral insufficiency (1 versus 0) | ||
| Univariate | 1.80 (0.92–3.54) | 0.09 |
| Multivariate | 1.55 (0.76–3.14) | 0.2 |
| Mitral insufficiency (2 or 3 versus 0) | ||
| Univariate | 3.47 (1.77–6.83) | 0.001 |
| Multivariate | 2.20 (1.01–4.80) | 0.05 |
Mitral insufficiency was graded as 0 (absent), 1 (trivial), 2 (mild), 3 (moderate) or 4 (severe).
Each multivariate model includes age, sex, left ventricular ejection fraction, New York Heart Association class, etiology of left ventricular dysfunction (ischemic or nonischemic), treatment assignment (placebo or enalapril), baseline medication use (beta-blocker, digoxin, acetylsalicylic acid, diuretic), presence of atrial fibrillation, hypertension, diabetes mellitus and smoking
DISCUSSION
The present study demonstrated that patients with left ventricular dysfunction and mitral insufficiency are more likely to die or be admitted to hospital for heart failure. The presence of any mitral insufficiency was associated with an 82% increased risk of death or hospitalization. The association between mitral insufficiency and death or hospitalization for heart failure is consistent across different categories of the mitral insufficiency variable and appears to increase with increasing severity of mitral insufficiency.
Several recent studies have found similar results, with mitral insufficiency being associated with poorer long-term outcomes, including more symptoms (8,12) and death (8,9–11). The incidence of mitral insufficiency in these studies was higher (43% to 70%) than in the current study of SOLVD trial patients (15%). This may be due to the much greater proportion of patients in NYHA class III or IV in these studies (43% [8], 75% [10] and 100% [11]) than in our study – 14%. In addition, the studies by Koelling et al (9) and Trichon et al (10) found similar hazard ratios and gradients of association between increasing severity of mitral insufficiency, as well as poorer outcomes (9,10). Interestingly, Grigioni et al (8), whose study included only patients with ischemic mitral insufficiency, also found very similar results. Consistent among all these studies is that patients with left ventricular dysfunction and mitral insufficiency have a particularly poor prognosis, which appears to persist regardless of the etiology and severity of symptoms. Importantly, our results extend the association between mitral insufficiency and poor prognosis to patients with less advanced heart failure.
A potential limitation of the present study is that the SOLVD study was not designed to evaluate the effect of mitral insufficiency in left ventricular dysfunction. However, the SOLVD echocardiography substudy was designed to examine the longitudinal effects of ACE inhibitor therapy on left ventricular remodelling. There were very few differences between the echocardiography substudy patients and the entire SOLVD study cohort (17). Thus, the findings of the current study are likely to be representative of all the SOLVD study patients. A second limitation is that all echocardiograms were performed and interpreted at various study sites rather than in a centralized echocardiography laboratory. Thus, there may be some differences of interpretation between different echocardiographers. However, this is more reflective of real practice. Furthermore, any differences in interpretation that may exist across sites are likely only to be among grades of mitral insufficiency rather than for its presence or absence. In addition, the management of heart failure has changed dramatically since the SOLVD study. However, more recent studies show remarkably similar results in more symptomatic patients (8,11).
Despite improved survival with medical therapy, an important finding from most heart failure studies, particularly in patients with advanced heart failure symptoms, is that the majority of patients remain in a poor functional class (3,20). More than 60% of patients surviving in the treatment arm of the Randomized ALdactone Evaluation Study (RALES) (3) remained in NYHA class III or IV. In the COoperative North Scandinavian ENalapril SUrvival Study (CONSENSUS) (20) of class IV heart failure patients, 59 of 77 survivors in the treatment group were in NYHA class III or IV. Quality of life studies in heart failure patients have shown that treatment demonstrated to improve survival did not improve quality of life, and that quality of life was not different than in patients receiving standard treatment (21).
Other options for these patients include optimization of current medical therapy and newer classes of drugs. It is not clear whether the mitral insufficiency is the result of particularly adverse ventricular remodelling and, as such, is merely a marker of advanced disease, or whether the mitral insufficiency itself results in the poorer outcomes. However, given the mechanical nature of mitral insufficiency in left ventricular dysfunction, surgical possibilities also need to be explored. Recently, several surgical series have reported encouraging results with mitral annuloplasty in patients with NYHA class III or IV symptoms, low ejection fraction and severe functional mitral insufficiency (13,22–24). Survival at one and two years is comparable with that of recent medical trials, while the functional class appears to be much better (3,13). To date, however, there is no direct comparison between medical and surgical therapy for patients with heart failure and mitral insufficiency. More effort is needed to improve the outcomes of this large subgroup of heart failure patients, perhaps with different modalities of treatment.
CONCLUSIONS
We have demonstrated that mitral insufficiency in patients with left ventricular dysfunction is independently associated with death or rehospitalization for heart failure in patients with less severe heart failure. These findings have important implications for both clinicians and researchers in heart failure. The presence of mitral insufficiency and left ventricular dysfunction identifies a particularly high-risk patient who may require special attention and perhaps consideration for novel management strategies.
REFERENCES
- 1.McMurray J, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart. 2000;83:596–602. doi: 10.1136/heart.83.5.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ho KK, Pinsky JL, Kannel WB, Levy D. The epidemiology of heart failure: The Framingham Study. J Am Coll Cardiol. 1993;22:6A–13A. doi: 10.1016/0735-1097(93)90455-a. [DOI] [PubMed] [Google Scholar]
- 3.Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–17. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 4.The effect of digoxin on mortality and morbidity in patients with heart failure The Digitalis Investigation Group. N Engl J Med. 1997;336:525–33. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]
- 5.MacIntyre K, Capewell S, Stewart S, et al. Evidence of improving prognosis in heart failure: Trends in case fatality in 66 547 patients hospitalized between 1986 and 1995. Circulation. 2000;102:1126–31. doi: 10.1161/01.cir.102.10.1126. [DOI] [PubMed] [Google Scholar]
- 6.Steptoe A, Mohabir A, Mahon N, McKenna WJ. Health related quality of life and psychological wellbeing in patients with dilated cardiomyopathy. Heart. 2000;83:645–50. doi: 10.1136/heart.83.6.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Junker A, Thayssen P, Nielsen B, Andersen P. The hemodynamic and prognostic significance of echo-Doppler-proven mitral regurgitation in patients with dilated cardiomyopathy. Cardiology. 1993;83:14–20. doi: 10.1159/000175942. [DOI] [PubMed] [Google Scholar]
- 8.Grigioni F, Enriquez-Sarano M, Zehr KJ, Bailey KR, Tajik AJ. Ischemic mitral regurgitation: Long-term outcome and prognostic implications with quantitative Doppler assessment. Circulation. 2001;103:1759–64. doi: 10.1161/01.cir.103.13.1759. [DOI] [PubMed] [Google Scholar]
- 9.Koelling TM, Aaronson KD, Cody RJ, Bach DS, Armstrong WF. Prognostic significance of mitral regurgitation and tricuspid regurgitation in patients with left ventricular systolic dysfunction. Am Heart J. 2002;144:524–9. doi: 10.1067/mhj.2002.123575. [DOI] [PubMed] [Google Scholar]
- 10.Trichon BH, Felker GM, Shaw LK, Cabell CH, O’Connor CM. Relation of frequency and severity of mitral regurgitation to survival among patients with left ventricular systolic dysfunction and heart failure. Am J Cardiol. 2003;91:538–43. doi: 10.1016/s0002-9149(02)03301-5. [DOI] [PubMed] [Google Scholar]
- 11.Cabell CH, Trichon BH, Velazquez EJ, et al. Importance of echocardiography in patients with severe nonischemic heart failure: The second Prospective Randomized Amlodipine Survival Evaluation (PRAISE-2) echocardiographic study. Am Heart J. 2004;147:151–7. doi: 10.1016/j.ahj.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Robbins JD, Maniar PB, Cotts W, Parker MA, Bonow RO, Gheorghiade M. Prevalence and severity of mitral regurgitation in chronic systolic heart failure. Am J Cardiol. 2003;91:360–2. doi: 10.1016/s0002-9149(02)03172-7. [DOI] [PubMed] [Google Scholar]
- 13.Smolens I, Pagani F, Bolling S. Mitral valve repair in heart failure. Eur J Heart Fail. 2000;2:365–71. doi: 10.1016/s1388-9842(00)00125-2. [DOI] [PubMed] [Google Scholar]
- 14.Studies of left ventricular dysfunction (SOLVD) – rationale, design and methods: Two trials that evaluate the effect of enalapril in patients with reduced ejection fraction Am J Cardiol 199066315–22.(Erratum in 1990;66:1026). [DOI] [PubMed] [Google Scholar]
- 15.Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 16.Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions N Engl J Med 1992327685–91.(Erratum in 1992;327:1768). [DOI] [PubMed] [Google Scholar]
- 17.Greenberg B, Quinones M, Koilpillai C, et al. Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation. 1995;91:2573–81. doi: 10.1161/01.cir.91.10.2573. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81. [Google Scholar]
- 19.Cox DR. Regression models and life-tables. J R Stat Soc B. 1972;34:187–220. [Google Scholar]
- 20.Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group. N Engl J Med. 1987;316:1429–35. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 21.Rector TS, Johnson G, Dunkman WB, et al. Evaluation by patients with heart failure of the effects of enalapril compared with hydralazine plus isosorbide dinitrate on quality of life. V-HeFT II. The V-HeFT VA Cooperative Studies Group. Circulation. 1993;87(6 Suppl):VI71–7. [PubMed] [Google Scholar]
- 22.Bishay E, McCarthy P, Cosgrove D, et al. Mitral valve surgery in patients with severe left ventricular dysfunction. Eur J Cardiothorac Surg. 2000;17:213–21. doi: 10.1016/s1010-7940(00)00345-6. [DOI] [PubMed] [Google Scholar]
- 23.Chen F, Adams D, Aranki S, et al. Mitral valve repair in cardiomyopathy. Circulation. 1998;98(19 Suppl):II124–7. [PubMed] [Google Scholar]
- 24.Calafiore A, Gallina S, DiMauro M, et al. Mitral valve procedure in dilated cardiomyopathy: Repair or replacement? Ann Thorac Surg. 2001;71:1146–52. doi: 10.1016/s0003-4975(00)02650-3. [DOI] [PubMed] [Google Scholar]