Abstract
We present here the case of a 40-year-old woman with a greater than 10 year prior history of bilateral breast silicone injection and saline bag implantation. Bilateral palpable breast nodules were observed, but the ultrasound scan was suboptimal and the magnetic resonance imaging showed no gadolinium-enhanced tumor. The 18F-FDG PET/CT scan showed a hypermetabolic nodule in the left breast with a 30% increase of 18F-FDG uptake on the delayed imaging, and this mimicked breast cancer. She underwent a left partial mastectomy and the pathology demonstrated a siliconoma.
Keywords: Breast, siliconoma; 18F-FDG PET/CT
Although silicone injection for breast augmentation has numerous complications and it makes the exact diagnosis of breast cancer more difficult, this procedure is not uncommon in Asia. 18F-FDG PET is useful for differentiating between benign and malignant lesions in many kinds of tumors, including breast cancer. However, some kinds of inflammation can also show a high 18F-FDG uptake and so false results may occur. We herein present a case of a false positive result on an 18F-FDG PET scan that was caused by a previous silicone injection into the breast.
CASE REPORT
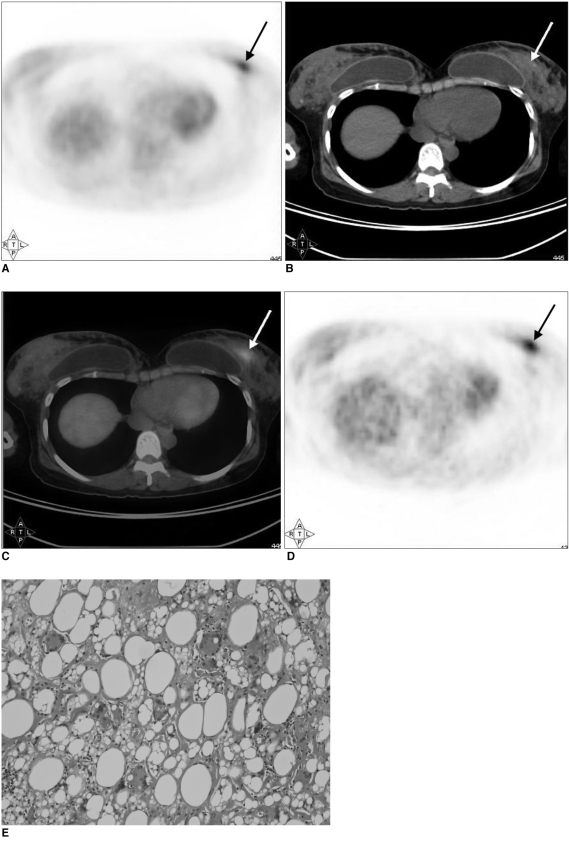
A 40-year-old female with a history of bilateral breast silicone injection and saline bag implantation (10 years previously) came to our hospital because of bilateral palpable breast nodules. The ultrasound showed suboptimal findings due to silicone injection and no abnormality could be found. The magnetic resonance imaging (MRI) with gadolinium enhancement showed multiple non-enhanced silicone cysts, but no gadolinium-enhanced breast tumor was noted. Owing to the clinically palpable breast nodules, she was referred for 18F-FDG PET/CT to determine the nature of the breast nodules. One hour after intravenously injection of 370 MBq (10 mCi) of 18F-FDG, an integrated PET/CT scanner (Biograph; Siemens AG, Berlin, Germany) was used to acquire the images from the head to the upper thighs. The attenuation correction was done by CT. The delayed images were taken two hours post-injection. The images were reconstructed using a standard ordered-subset expectation maximization algorithm (two iterations, 8 subsets). The voxel size was 4.16×4.16×4.16 mm3. 18F-FDG PET/CT showed a hypermetabolic nodule in the left breast with a maximal standardized uptake value (SUV) of 3.7 on the 1-hour post-injection image; the SUV was calculated as tumor activity concentration/(injected dose/body weight) (Fig. 1). The delayed 2-hour image showed a further increase of 18F-FDG uptake in the nodule with a maximal SUV of 4.8 (Fig. 1). Breast cancer was highly suspected owing to the high, persistent rise of the 18F-FDG uptake in the lesion and its nodular shape. Thus, we performed left partial mastectomy. However, the pathology showed a siliconoma (silicone granuloma) and there was no evidence of malignancy.
Fig. 1.
False positive FDG PET/CT caused by breast silicone injection in 40-year-old female.
A-C. Transverse slices of one hour post-injection 18F-FDG PET scan (A), CT (B) and PET/CT fusion image (C) showed focal area of increased 18F-FDG uptake (arrows; maximal SUV = 3.7) in left breast anterolateral to saline bag.
D. Delayed 18F-FDG PET imaging at two hour post-injection showed further increase of 18F-FDG uptake in above lesion (arrow; maximal SUV = 4.8).
E. Foreign body reaction to silicone (siliconoma). Variable-sized silicone spaces were surrounded by multinucleated foreign body-type giant cells, some foamy macrophages and some lymphocytes.
DISCUSSION
Silicone is one of several materials that are used for breast augmentation. Silicone breast injection has numerous adverse effects including skin reaction, pain, infection and the formation of granulomas (i.e. siliconoma). It also precludes the exact diagnosis of breast cancer because injecting silicone makes the breast hard and lumpy and a physical examination cannot differentiate it from breast cancer. Performing mammography of breasts after silicone injection often shows multiple dense nodules and an accurate interpretation is difficult. The findings of sonography are often suboptimal due to the extensive echogenic noise of silicone (1). Although MRI in such cases is considered valuable, it has also been reported that it is difficult to differentiate malignancy from benign angiogenic processes on MRI (2).
18F-FDG PET has been shown to be useful to differentiate benign lesions from malignant lesions in patients with augmentation mammoplasty and it is superior to the more traditional modalities (3, 4). However, false positive results have been reported, such as a curvilinear-shaped increased 18F-FDG uptake around a ruptured breast prosthesis and intense 18F-FDG uptake in the ipsilateral axillary lymph nodes of the ruptured breast implant (5, 6). The 18F-FDG uptake in the above-mentioned case was caused by inflammation. Noh et al. (3) also demonstrated a case of false positive results on 18F-FDG PET from breast silicone injection; however, in that case, there was no pathologic report on the diffuse breast lesions with high 18F-FDG uptake. Our case did have pathologic proof. Besides, in our case, the initial high 18F-FDG uptake in the breast nodule, as well as the further increase of 18F-FDG accumulation in the nodule on the additional delayed images, made malignancy more likely.
Dual-time-point imaging, with increasing and decreasing 18F-FDG uptake over time and this indicates breast malignancy and inflammatory lesions, respectively, has been reported to be highly sensitive and specific (7). Nevertheless, our case demonstrated an inflammatory lesion, which was ultimately proven to be a siliconoma (silicone granuloma) caused by silicone injection, and this led to a false positive result owing to a high and persistent increase in 18F-FDG uptake on the 18F-FDG PET images. In fact, some reports have indicated that some benign lesions, such as a granulomatous pulmonary lesion, can show further increase of 18F-FDG uptake on the delayed images (8). There have been reports of high levels of glucose transporter-1 protein in inflammatory lesions that led to high 18F-FDG uptake (9) and a substantial expression of hexokinase in the granulomatous tissue that contributed to a persistent increase of 18F-FDG uptake (10). These finds can explain the initial high SUV uptake and a further increase of 18F-FDG uptake on the delayed image in our case. Further investigations are needed on the usefulness of dual-time-point 18F-FDG PET in patients with a history of breast silicone injection
In conclusion, we present here the case of a female patient with a history of breast silicone injection that caused a false positive 18F-FDG PET/CT scan owing to the injected silicone's high and persistently increasing SUV.
References
- 1.Leibman AJ, Sybers R. Mammographic and sonographic findings after silicone injection. Ann Plast Surg. 1994;33:412–414. doi: 10.1097/00000637-199410000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Cheung YC, Su MY, Ng SH, Lee KF, Chen SC, Lo YF. Lumpy silicone-injected breasts: enhanced MRI and microscopic correlation. Clin Imaging. 2002;26:397–404. doi: 10.1016/s0899-7071(02)00453-9. [DOI] [PubMed] [Google Scholar]
- 3.Noh DY, Yun IJ, Kang HS, Kim YC, Kim JS, Chung JK, et al. Detection of cancer in augmented breasts by positron emission tomography. Eur J Surg. 1999;165:847–851. doi: 10.1080/11024159950189339. [DOI] [PubMed] [Google Scholar]
- 4.Wahl RL, Helvie MA, Chang AE, Andersson I. Detection of breast cancer in women after augmentation mammoplasty using fluorine-18-fluorodeoxyglucose-PET. J Nucl Med. 1994;35:872–875. [PubMed] [Google Scholar]
- 5.Bhargava P, Glass E, Ghesani M. Inflammatory F-18 FDG uptake secondary to ruptured breast prosthesis. Clin Nucl Med. 2006;31:227–228. doi: 10.1097/01.rlu.0000204490.25782.f8. [DOI] [PubMed] [Google Scholar]
- 6.Hurwitz R. F-18 FDG positron emission tomographic imaging in a case of ruptured breast implant: inflammation or recurrent tumor? Clin Nucl Med. 2003;28:755–756. doi: 10.1097/01.rlu.0000082664.22354.4b. [DOI] [PubMed] [Google Scholar]
- 7.Kumar R, Loving VA, Chauhan A, Zhuang H, Mitchell S, Alavi A. Potential of dual-time-point imaging to improve breast cancer diagnosis with 18F-FDG PET. J Nucl Med. 2005;46:1819–1824. [PubMed] [Google Scholar]
- 8.Ichiya Y, Kuwabara Y, Sasaki M, Yoshida T, Akashi Y, Murayama S, et al. FDG-PET in infectious lesions: the detection and assessment of lesion activity. Ann Nucl Med. 1996;10:185–191. doi: 10.1007/BF03165391. [DOI] [PubMed] [Google Scholar]
- 9.Mochizuki T, Tsukamoto E, Kuge Y, Kanegae K, Zhao S, Hikosaka K, et al. FDG uptake and glucose transporter subtype expressions in experimental tumor and inflammation models. J Nucl Med. 2001;42:1551–1555. [PubMed] [Google Scholar]
- 10.Mamede M, Higashi T, Kitaichi M, Ishizu K, Ishimori T, Nakamoto Y, et al. [18F]FDG uptake and PCNA, Glut-1, and Hexokinase-II expressions in cancers and inflammatory lesions of the lung. Neoplasia. 2005;7:369–379. doi: 10.1593/neo.04577. [DOI] [PMC free article] [PubMed] [Google Scholar]