Abstract
Single-balloon kyphoplasty via an extrapedicular approach has been reported to be effective because it requires less time than conventional two-balloon kyphoplasty and has comparable therapeutic efficacy. However, single-balloon kyphoplasty is not popular because the extrapedicular approach is believed to be complicated and unsuitable for the thoracolumbar and lumbar spine. The authors describe a standardized surgical technique that utilizes a far-lateral extrapedicular approach for single-balloon kyphoplasty, which can be performed in any part of the spine by physicians without substantial difficulty.
Keywords: Osteoporosis, Vertebral compression fractures, Balloon kyphoplasty
INTRODUCTION
Recently, a single-balloon kyphoplasty technique was introduced to overcome the shortcomings of conventional two-balloon kyphoplasty, in particular, the amount of time required for this bilateral procedure. Furthermore, its therapeutic efficacy for osteoporotic vertebral compression fractures has been reported to be comparable to that of two-balloon kyphoplasty12,16). Basically, single-balloon kyphoplasty requires the insertion of a balloon catheter into the center of a vertebral body to achieve a level of biomechanical stability comparable with that of two-balloon kyphoplasty. However, the extrapedicular approach has not been well standardized for single-balloon kyphoplasty, because the required trajectory from skin entry to the center of the vertebral body appears variable according to the level involved and its radiological anatomy. Accordingly, this approach requires an experienced hand and is generally less favored than the transpedicular approach of two-balloon kyphoplasty, which has a comparatively determined trajectory in the pedicle, and can be performed, with less experience.
The authors describe a less-demanding standardized technique of single-balloon kyphoplasty using a far lateral extrapedicular approach.
OPERATIVE TECHNIQUES
The procedure of the far lateral extrapedicular single-balloon kyphoplasty has been described by the authors in the previous report12). In the present study, the procedure required to insert the apparatus that conveys bone cement into the center of a vertebral body is presented in detail, as this is usually considered to be the most difficult aspect of the far lateral extrapedicular approach procedure in single-balloon kyphoplasty.
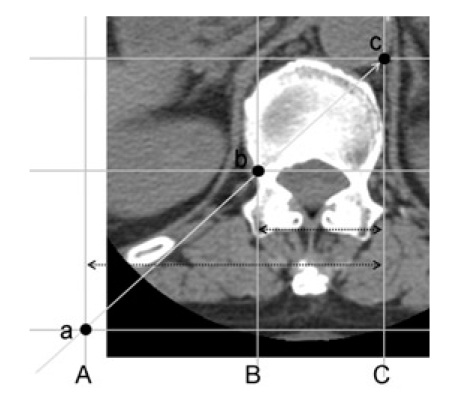
An ideal trajectory required during needle insertion, which places a balloon in the middle of the fractured body, is shown on Fig. 1. This trajectory starts from target 'a' to 'c' through 'b'. The point 'a' is an imaginary point which the diagonal line drawn from 'c' through 'b' intersects the skin of actual human back. To determine the entry point 'a', the authors measured the length of the lines 'α' and 'β' on axial CT scans in 20 adults, who were distributed as 8 male and 12 female in average age of 62.3 years (range; 56-72), and determined (α/β) ratios. In the results, α/β, was about 2.5 irrespective of level observed, as shown on Table 1.
Fig. 1.
Line drawings on axial computed tomography scan showing landmarks for determining skin entry point. Line C is drawn along the lateral border of vertebral body at opposite side. Line B is drawn along the outmost part of pedicluar ring at same side. Line A is apart from line C by 2.5 times of β distance, irrespective of levels. Ideal trajectory of far lateral approach in single balloon kyphoplasty should start from the point a (entry point), through the point b (the outmost border of the ipsilateral pedicle ring), and the point c (the imaginary point where the horizontal line drawn along the anterior cortex meets the vertical line along the contralateral border of the fractured body) is the target. α : a distance between the line A and C, β : a distance between line B and C.
Table 1.
α/β, ratios at different vertebral levels
*Standard deviation
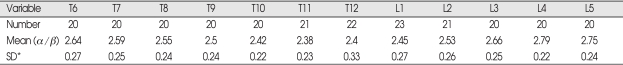
According to these results, the authors drew three lines 'A', 'B' and 'C' on back skin to determine skin entry (Fig. 2). The line 'C' was placed vertically at 'c' on AP views and drawn on skin along the contralateral border of the vertebral body. The line 'B' was oriented vertically to point 'b' and drawn along the outmost border of the ipsilateral pedicle ring, and the line 'A' was drawn longitudinally parallel to the line 'B' and apart from line 'C' by 2.5 times of 'β' distance. These three lines were drawn on AP view under fluoroscopic guidance. In lateral view, a suitable trajectory for needle insertion would be from the skin entry point to the corner made by the anterior cortex and inferior end plate of the fractured body (Fig. 3B). Therefore, the actual skin entry point (a) is defined as the point formed by the intersection of lines line A and the ipsilaterally extending line of the imaginary diagonal line on the fractured vertebral body between the contralateral lower corner (b) and the ipsilateral upper corner (c) in AP view (Fig. 2).
Fig. 2.
A Photograph depicting actual skin entry point (a), defined as the point of that line A meets the extension of the diagonal line (c to b) across the treated vertebral body on anteroposterior view of fluoroscopy. b : the ipsilateral upper corner of the fractured body, c : the contralateral lower corner of fractured body on AP view.
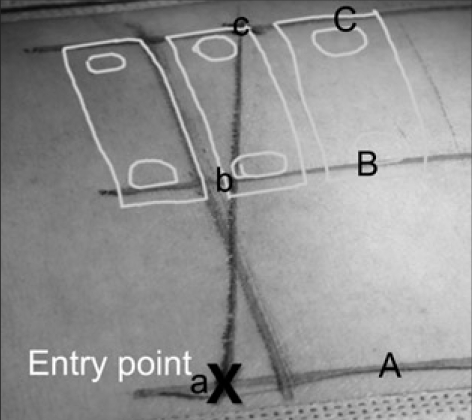
Fig. 3.
A : A disposable 11-gauge Jamshidi needle is inserted with maintaining the angle at 45° to 50° between the horizontal plane and the needle, and is advanced to the outer border of the base of the ipsilateral pedicle, through the ligament complex of the costovertebral joint in the thoracic spine or the transverse process in the lumbar spine, and is advanced to the center of vertebral body. B : The tip of the needle is directed to the point where the anterior cortex of the fractured body meets the inferior end plate on the lateral view.
After making a small stab wound at the determined skin entry point, a disposable 11-gauge Jamshidi needle (Manan Medical, Northbrook, IL) is inserted, while maintaining an angle of 45° to 50° between the horizontal plane and the needle, and advanced to point 'b' (the outer border of the base of the ipsilateral pedicle), through the ligament complex of the costovertebral joint in the thoracic spine or the transverse process in the lumbar spine under fluoroscopic monitoring in AP and lateral views (Fig. 3A). After penetrating the cortex of the vertebral body, the tip of the needle may require minor adjustment as it must be directed to the point where the anterior cortex of the fractured body meets the inferior end plate in lateral view (Fig. 3B), and to the point where the contralateral cortex of the vertebral body meets the inferior endplate in AP view. When the needle is advanced, its tip must be confirmed to be within the pedicle ring on AP view, before passing the posterior wall in lateral view, to avoid compromising the spinal canal. Just after the tip of the needle passes the posterior vertebral wall on lateral view, the stylet is removed and a guide wire is inserted into the vertebral body and advanced until its tip reaches in the body center on AP and lateral views.
The remaining kyphoplasty procedures are almost identical to those in the standard balloon kyphoplasty (Fig. 4).
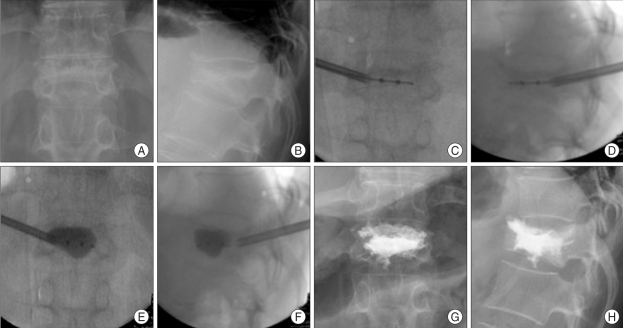
Fig. 4.
Percutaneous kyphopasty using a single-balloon device performed in 12th thoracic vertebra (T12) of a 68-year-old woman with an osteoporotic compression fracture (A and B). Intraoperative anteroposterior (C) and lateral (D) fluoroscopic views show a single balloon tamp in the middle portion of the vertebral body. After inflating a balloon, the height of the body is increased (E and F). Bone cement is filled up the cave created by the single-balloon (G and H).
Clinical assessments
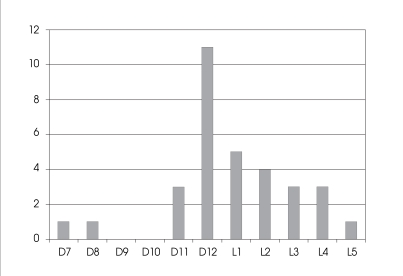
Between September 2007 and May 2008, twenty-nine consecutive patients underwent the kyphoplasty using this technique. The patients included 6 men and 23 women (age range; 50-87 years, mean age; 68.8 years). Three patients underwent two level operations. The level treated were distributed form 7th thoracic to 5th lumbar spine (Fig. 5). Mean amount of PMMA injected to fractured body was 4.90±1.13 cc. There was no case of operation failure.
Fig. 5.
Bar graph showing distribution of the treated vertebrae. Long axis represents the number of fractured levels treated.
Twenty-seven of 29 patients (93.1%) improved the VAS score postoperatively. The mean preoperative VAS score was 9.24±1.22, decreased to 2.33±2.57 at 2 days after operation, and more improved to 1.74±1.85 at 14 days postoperatively (p<0.001).
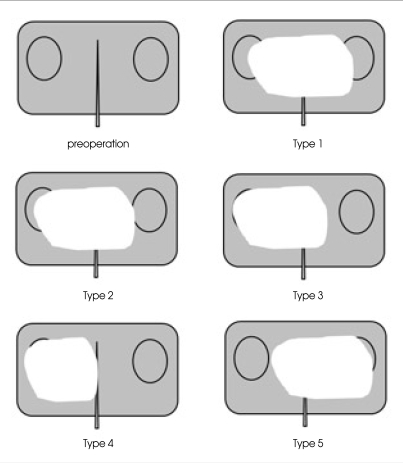
The spread of PMMA in the treated vertebral body was assessed in all patients postoperatively. We classified the pattern of PMMA spread into five types on plain AP projection X-ray postoperatively as follows; Type 1 : evenly spread bone cement in both sides, Type 2 : dominantly spread in the ipsilateral side, but filled up sufficiently in the opposite side also, Type 3 : dominantly spread in the ipsilateral side and insufficiently filled up in the opposite side, Type 4 : only filled up in the ipsilateral side, and Type 5 : dominantly spread in the contralateral side, but filled up sufficiently in the ipsilateral side also (Fig. 6).
Fig. 6.
Diagrams showing a classification system of the bone cement spread injected in the treated vertebral body. Type 1 : Evenly spread bone cement in both sides. Type 2 : Dominantly spread in the ipsilateral side, but filled up sufficiently in the opposite side also. Type 3 : Dominantly spread in the ipsilateral side and insufficiently filled up in the opposite side. Type 4 : only filled up in the ipsilateral side. Type 5 : Dominantly spread in the contralateral side, but filled up sufficiently in the ipsilateral side also.
Height restoration ratio was calculated using the methods introduced by Lieberman et al.9), which was calculated as : (height regained/height loss)×100; height regained=posttreatment height-pretreatment height; height loss=estimated prefracture height-pretreatment fractured height.
Statistical verification was determined using SPSS for Windows (version 11.0.1; SPSS Inc). A result was considered statistically significant if the probability was less than 0.05.
The distribution of the types of PMMA spread in the operated vertebral body is as follows : type 1 in 18 levels (56.3%), type 2 in 6 (18.8%), type 3 in 6 (18.8%), and type 5 in 2 (6.3%) but no case of type 4.
The average percentage of height lost that was restored by this procedure was 30.34±20.98% (range; 0%-78%). The kyphotic deformity was corrected from 15.23±5.12 degree to 8.01±4.82 degree after operation (p<0.001).
Among the 32 treated vertebrae, the extravasation of cement occurred in 5 levels (15.6%) : intradiscal leaks in two levels, leaks into the paravertebral muscles in two, and leaks into the paravertebral venous channel in one. No patient complained of symptoms related with the extravasations. And, there were no complications related with the surgical procedures.
DISCUSSION
The extrapedicular approach was firstly introduced by Brugieres et al.3) in 1990, when it was referred to as the transcostovertebral approach, and was originally designed for conducting biopsies at the center of a vertebral body in the mid or high thoracic spine using a single needle. The extrapedicular approach was later applied to osteoporotic vertebral compression fractures in the mid and high thoracic spine by Boszczyk et al.2) in 2005, and by the authors12). However, surgeons might find it difficult to follow the described procedures based on the descriptions given in the literature, because it is difficult to consistently placing the tip of the needle in the center of a vertebral body. Based on the authors' experiences, the most difficult and important part of the extrapedicular approach in terms of winning the center of a spine is the initial stage, e.g., the determination of the skin entry point, and the maintenance of a trajectory that enables arrival at an ideal position in the posterior vertebral wall. Skin entry point determination is totally dependent on the radioanatomical landmarks of the costovertebral joint and transverse process, which are not clearly demonstrated in advanced osteoporotic patients. Moreover, the procedure is considerably more difficult in the lumbar than in the thoracic spine.
Several reports have been issued on single-balloon kyphoplasty, but the majority have focused on clinical or radiological outcome and not on surgical technique7,13,16,17).
According to the postoperative assessments in the present study, PMMA spread was comparatively even in both sides of the vertebral body in 26/32 levels (81.3%), and even the other 6 levels (18.7%) still showed quite amounts of PMMA in the mid portion and the contralateral side of the vertebral body.
With regard to the other clinical parameters in the present study such as reduction of pain score, restoration rate of decreased vertebral height, improvement in kyphotic deformity and extravasation rate, all the results appeared comparable with the ones of the conventional two-balloon kyphoplasty, which have been reported in the previous literatures1,4-6,8-11,14,15).
The needle advance through the far-lateral route can be put at the potential risks of injuries of the existing nerve roots and the segmental vessels. However, there may be no chance of such complications as long as the approaching route is maintained along the pedicle of the involved vertebra on the anteroposterior and lateral fluoroscopic views. Under local anesthesia, the injury of the nerve root can be avoided by patients' complaining of radicular pain during the procedures.
There would be an individual error in measuring the entry point in this procedure, because this measurement method does not consider the curved surface of human body. However, a gentle sloping curve of human back would allow this possible error to be within an acceptable range.
As long as the procedures described in the present report are strictly followed under fluoroscopic guidance in patients with osteoporotic vertebral compression fractures, bone cement can be delivered into the center of a vertebral body consistently in the mid and high thoracic spines as well as the thoracolumbar and lower lumbar spines, and comparable clinical results can be achieved. Moreover, the principle of this procedure can be applied to both single-balloon kyphoplasty and single-needle vertebroplasty.
CONCLUSION
The described far lateral extrapedicular approach for single-balloon kyphoplasty allows the administration of bone cement into the center of a vertebral body safely and efficiently under fluoroscopic guidance, and can also be applied to osteoporotic vertebral compression fractures in both the thoracic and lumbar spines without significant difficulty.
References
- 1.Berlemann U, Franz T, Orler R, Heini PF. Kyphoplasty for treatment of osteoporotic vertebral fractures : a prospective non-randomized study. Eur Spine J. 2004;13:496–501. doi: 10.1007/s00586-004-0691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boszczyk BM, Bierschneider M, Hauck S, Beisse R, Potulski M, Jaksche H. Transcostovertebral kyphoplasty of the mid and high thoracic spine. Eur Spine J. 2005;14:992–999. doi: 10.1007/s00586-005-0943-1. [DOI] [PubMed] [Google Scholar]
- 3.Brugieres P, Gaston A, Heran F, Voisin MC, Marsault C. Percutaneous biopsies of the thoracic spine under CT guidance : transcostovertebral approach. J Comput Assist Tomogr. 1990;14:446–448. doi: 10.1097/00004728-199005000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Deen HG, Aranda-Michel J, Reimer R, Putzke JD. Preliminary results of balloon kyphoplasty for vertebral compression fractures in organ transplant recipients. Neurosurg Focus. 2005;18:e6. [PubMed] [Google Scholar]
- 5.Feltes C, Fountas KN, Machinis T, Nikolakakos LG, Dimopoulos V, Davydov R, et al. Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus. 2005;18:e5. doi: 10.3171/foc.2005.18.3.6. [DOI] [PubMed] [Google Scholar]
- 6.Grohs JG, Matzner M, Trieb K, Krepler P. Minimal invasive stabilization of osteoporotic vertebral fractures : a prospective nonrandomized comparison of vertebroplasty and balloon kyphoplasty. J Spinal Disord Tech. 2005;18:238–242. [PubMed] [Google Scholar]
- 7.Hadjipavlou A, Tosounidis T, Gaitanis I, Kakavelakis K, Katonis P. Balloon kyphoplasty as a single or as an adjunct procedure for the management of symptomatic vertebral haemangiomas. J Bone Joint Surg Br. 2007;89:495–502. doi: 10.1302/0301-620X.89B4.18121. [DOI] [PubMed] [Google Scholar]
- 8.Ledlie JT, Renfro M. Balloon kyphoplasty : one-year outcomes in vertebral body height restoration, chronic pain, and activity levels. J Neurosurg. 2003;98(1 Suppl):36–42. doi: 10.3171/spi.2003.98.1.0036. [DOI] [PubMed] [Google Scholar]
- 9.Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of "kyphoplasty" in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26:1631–1638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 10.Phillips FM, Ho E, Campbell-Hupp M, McNally T, Todd Wetzel F, Gupta P. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine. 2003;28:2260–2265. doi: 10.1097/01.BRS.0000085092.84097.7B. discussion 2265-2267. [DOI] [PubMed] [Google Scholar]
- 11.Pradhan BB, Bae HW, Kropf MA, Patel VV, Delamarter RB. Kyphoplasty reduction of osteoporotic vertebral compression fractures : correction of local kyphosis versus overall sagittal alignment. Spine. 2006;31:435–441. doi: 10.1097/01.brs.0000200036.08679.1e. [DOI] [PubMed] [Google Scholar]
- 12.Ryu KS, Park CK, Kim MK, Kim DH. Single balloon kyphoplasty using far-lateral extrapedicular approach : technical note and preliminary results. J Spinal Disord Tech. 2007;20:392–398. doi: 10.1097/BSD.0b013e31802da846. [DOI] [PubMed] [Google Scholar]
- 13.Shindle MK, Gardner MJ, Koob J, Bukata S, Cabin JA, Lane JM. Vertebral height restoration in osteoporotic compression fractures : kyphoplasty balloon tamp is superior to postural correction alone. Osteoporos Int. 2006;17:1815–1819. doi: 10.1007/s00198-006-0195-x. [DOI] [PubMed] [Google Scholar]
- 14.Theodorou DJ, Theodorou SJ, Duncan TD, Garfin SR, Wong WH. Percutaneous balloon kyphoplasty for the correction of spinal deformity in painful vertebral body compression fractures. Clin Imaging. 2002;26:1–5. doi: 10.1016/s0899-7071(01)00350-3. [DOI] [PubMed] [Google Scholar]
- 15.Watts NB, Harris ST, Genant HK. Treatment of painful osteoporotic vertebral fractures with percutaneous vertebroplasty or kyphoplasty. Osteoporos Int. 2001;12:429–437. doi: 10.1007/s001980170086. [DOI] [PubMed] [Google Scholar]
- 16.Yang HL, Niu GQ, Liang DC, Wang GL, Meng B, Chen L, et al. [The contrast study between single and double balloon bilateral dilatation of kyphoplasty] Zhonghua Wai Ke Za Zhi. 2004;42:1299–1302. [PubMed] [Google Scholar]
- 17.Zheng ZM, Kuang GM, Dong ZY, Li FB, Lu Y, Chen H, et al. [One-stage single balloon multiple expansions percutaneous kyphoplasty : report of 18 cases] Zhonghua Yi Xue Za Zhi. 2007;87:580–584. [PubMed] [Google Scholar]