Abstract
Objective
To evaluate clinical and radiological results of two different fusion techniques in adult low-grade isthmic spondylolisthesis.
Methods
Between November 2003 and December 2004, 46 consecutive patients underwent instrumented mini-transforaminal lumbar interbody fusion (mini-TLIF) (group I) at Wooridul Spine Hospital, Seoul, Korea. Between February 2003 and October 2006, 32 consecutive patients underwent instrumented circumferential fusion (group II) at Leon Wiltse Memorial Hospital, Suwon, Korea. The mean follow-up periods were 29.7 and 26.1 months, respectively.
Results
Mean visual analog scale (VAS) scores for back and leg pain decreased, respectively, from 6.98 and 6.33 to 2.3 and 2.2 in group I and from 7.38 and 6.00 to 1.7 and 1.0 in group II. Mean Oswestry disability index (ODI) improved from 51.85% to 14.4% in group I and from 60% to 9.1% in group II. In both groups, VAS and ODI scores significantly changed from pre- to postoperatively (p<0.001), but postoperative outcome between groups was statistically not significant. Radiologic evidence of fusion was noted in 95.7% and 100% of the patients in group I and II, respectively. In both groups, changes in disc height, segmental lordosis, degree of listhesis, and whole lumbar lordosis between the pre- and postoperative periods were significant except whole lumbar lordosis in both groups.
Conclusion
Clinical and functional outcomes demonstrate no significant differences between groups in treating back and leg pain of adult patients with low-grade isthmic spondylolisthesis. However, in terms of operative data (i.e. operation time and hospital stay), instrumented mini-TLIF demonstrated better results.
Keywords: Low-grade isthmic spondylolisthesis, Instrumented transforaminal lumbar interbody fusion, Instrumented circumferential
INTRODUCTION
Fusion has gained popularity for surgical treatment of adult low-grade isthmic spondylolisthesis in patients with chronic persistent pain24,26). Several fusion methods have been reported for adult low-grade isthmic spondylolisthesis via various approaches including posterolateral fusion (PLF)3,20) and lumbar interbody fusion techniques, such as posterior lumbar interbody fusion (PLIF)5,7,22), transforaminal interbody fusion (TLIF)2,9,15,19), anterior lumbar interbody fusion (ALIF)11,21), and a combined posterior-anterior approach (circumferential fusion, 360 degree fusion)4,12,16,31,33), using different approaches, vertebral fixation modalities35), and fusion materials7). However, the choice of lumbar fusion technique must be individualized based on the clinical needs of each patient, the surgical outcomes for each procedure based on published literature, and the individual skills and the surgeon's preference.
Much has been reported about the advantages of each approach. The present study was undertaken to evaluate retrospectively the results obtained in patients undergoing instrumented mini-TLIF compared with instrumented circumferential fusion for the treatment of low-grade isthmic spondylolisthesis, with a goal of helping in the selection of treatment options. We present the clinical and radiological results obtained during the postoperative period. To the best of our knowledge, this is the first study to analyze the clinical and radiological results of instrumented circumferential fusion in comparison with instrumented mini-TLIF.
MATERIALS AND METHODS
Patient population
This study was conducted at two institutions. Between November 2003 and December 2004, 46 patients underwent mini-TLIF with PPF (group I) performed at Wooridul Spine Hospital, Seoul, Korea. Between February 2003 and October 2006, 32 consecutive patients underwent circumferential fusion with instrumentation (group II) at Leon Wiltse Memorial Hospital, Suwon, Korea.
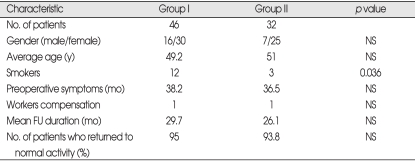
The mean age of the 46 patients in Group I was 49.2 years, and that of the 32 patients in Group II was 51.2 years. Demographic and clinical data are presented in Table 1. We conducted a retrospective review of office charts, hospital charts, and radiological studies to assess preoperative symptomatology, findings on clinical examination, and radiological characteristics.
Table 1.
Patient characteristics
Group I : mini-transforaminal lumbar interbody fusion, Group II : circumferential fusion, FU : follow-up, NS : not significant
The inclusion criteria for the patients were the presence of single-level low-grade (Meyerding grade 1 or 2) isthmic spondylolisthesis, chronic and persistent radiculopathy despite conservative treatment, progressive neurologic deficits, persistent and unremitting lower-back pain for more than 6 months, loss of quality of life because of neurologic claudication, minimum follow-up period of 2 years, and age range of 18-65 years.
The exclusion criteria for the patients were previous spine surgery, concomitant scoliosis of more than 15 degrees, a compression fracture or instability at the adjacent segment, and patients who underwent simultaneous decompression at adjacent segments.
Outcome assessment
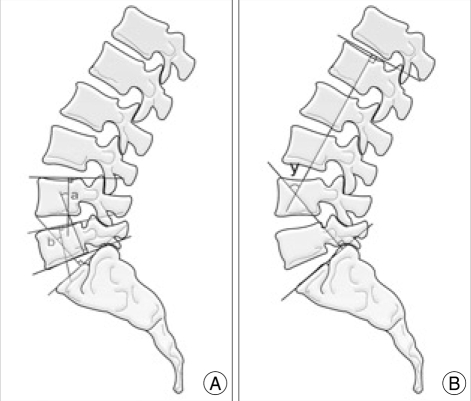
We performed radiological and clinical assessments postoperatively. An independent observer other than the treating surgeons was responsible for the radiographic assessments. The radiological outcome was evaluated on anteroposterior, lateral, and flexion-extension radiographs. The grade or amount of slip according to Meyerding, the percentage of slippage, segmental lordosis (SL), and whole lumbar lordosis (WL) were used as parameters to evaluate sagittal alignment after interbody fusion (Fig. 1).
Fig. 1.
A : The segmental lordosis (SL) at L4-5 (a) is defined as the angle subtended by the superior endplate line of L4 and the inferior endplate line of L5. The SL at L5-S1 (b) is defined as the angle subtended by the superior endplate line of L5 and the superior endplate line of S1. B : The whole lumbar lordosis (WL) (y) is defined as the angle subtended by the superior endplate line of L1 and the superior endplate line of S1.
The criterion for fusion is the presence of bony trabecular continuity between the vertebral bodies23).
Non-union was defined as a visible gap, graft collapse, and motion of greater than 4°. Those parameters were measured on pre- and postoperative standing lateral radiographs by using a measuring program with a built-in picture archiving communication system (PiView™; INFINITT Co. Ltd., Seoul, Korea). Fig. 1 presents the radiological measurements used in this study.
Clinical outcomes were graded using the visual analog scale (VAS; score range 0-10, with 0 representing no pain); functional outcomes were measured using Oswestry disability index (ODI) scores and the patient's return-to-work status.
Surgical Technique
The instrumented mini-TLIF (group I)
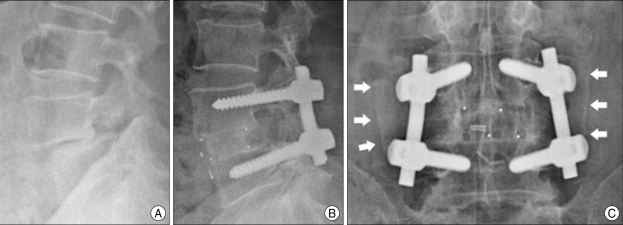
During the surgery, the patients were placed in the prone position; a Wilson Frame and Jackson tables were used for all of the cases. Under fluoroscopic guidance, the proper site for the incision was marked at approximately 2.5 to 3.5 cm off the midline. The surgery was done through a mini-open fashion with expandable working tubes such as the METRx set (Medtronic Sofamor Danek, Memphis, TN); alternatively, the surgery was performed in a minimally invasive fashion using nonexpandable working tubes and the percutaneous Sextant pedicle screws system. Total facetectomy was performed using an osteotome, a high-speed drill, and Kerrison rongeurs through a modified Wiltse transmuscular paraspinal approach.
Next, the ligamentum flavum was removed, which resulted in decompression of the ipsilateral exiting and traversing roots. After performing discectomy and preparing an endplate, a cage (Polyether ether ketone or Fidji cage) filled with graft material (cancellous auto-bone harvested from the lamina mixed with cancellous allograft) was inserted. The same procedure was performed on the contralateral side. After performing insertion of the pedicle screws under the C-arm guidance, compression and pedicle screw fixation were performed. After the interbody construct was placed, the pedicle screws were attached to and mildly compressed on the appropriately sized rods, thereby restoring lumbar lordosis while maintaining the restored disc height (Fig. 2).
Fig. 2.
A : Lateral preoperative radiograph of a patient with isthmic spondylolisthesis L5-S1 grade I. B : Lateral radiographs 55 months after instrumented mini-TLIF.
The instrumented circumferential fusion (group II)
All ALIF procedures were performed using the mini-laparotomic retroperitoneal approach, as previously described. After discectomy, a cage (Polyether ether ketone or Fidji cage) was carefully placed at the affected level as an interbody device containing allograft bone chips in most cases. One neurosurgeon trained extensively in anterior approaches to the spine performed these procedures. After completion of the mini-ALIF, the patient was immediately turned to the prone position; the second stage was performed with an instrumented PLF using an iliac bone graft. The PLF used a midline subperiosteal approach that exposes the transverse processes, pars, and facet joint, which were thoroughly decorticated. Decompression was not performed. The iliac crest autograft was placed in this bed after stabilization with pedicle screws and rods, thereby restoring lumbar lordosis while maintaining the restored disc height (Fig. 3).
Fig. 3.
A : Lateral preoperative radiograph of a patient with isthmic spondylolisthesis L4-5 grade I. B : Lateral radiographs 24 months after instrumented circumferential fusion. C : Anteroposterior radiographs 24 months after instrumented circumferential fusion. White arrows indicate posterolateral fusion mass.
Statistical analysis
For statistical analysis, an analysis of variance was conducted using the two proportions test, independent two-sample t-test, Mann-whitney U test, Chi-square test, Wilcoxon rank-sum test and paired t-test. A probability value of less than 0.05 was considered significant.
RESULTS
Radiological results
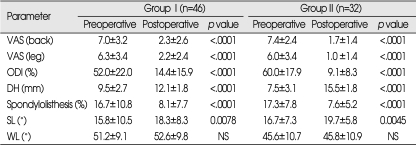
Preoperative, postoperative, and follow-up radiological data are summarized in Tables 2 and 3. Radiological evidence of successful arthrodesis was noted in 44 of 46 patients (95.7%) in the group 1 and in 32 of 32 patients (100%) in the group 2 (p>0.05). There was no significant difference in the preoperative radiological data between groups except disc height (DH) and whole lumbar lordosis (WL). The postoperative radiological data did not show a significant difference in the degree of listhesis and segmental lumbar lordosis (SL) between groups. But, significant difference in DH and WL were noted (Table 2). The mean DH changed from 9.55 to 12.11 mm (p<0.001) after surgery in the group I and from 7.46 to 15.48 mm (p<0.001) after surgery in the group II. The mean preoperative values for SL (°), WL (°), and the degree of listhesis (%) in the group 1 were 15.75°, 51.18° and 16.68% respectively; they were changed to 18.28° (p=0.0078), 52.61° (p=0.28) and 8.13% (p<0.0001) at last follow-up. The mean preoperative values for SL (°), WL (°), and the degree of listhesis (%) in the group II were 16.74°, 45.6° and 17.25% respectively; they were changed to 19.74° (p=0.0045), 45.79° (p=0.95) and 7.62% (p<0.0001) at last follow-up. Radiological data from both groups demonstrated statistically significant differences between the pre- and postoperative periods except WL (Table 3). No measurable subsidence or gliding of the cages was evident at the follow-up evaluation.
Table 2.
Comparison between two groups on pre- and post- operative evaluations
Group I : mini-transforaminal lumbar interbody fusion, Group II : circumferential fusion, Preop : preoperative, Postop : postoperative, NS : not significant, ODI : oswestry disability index
Table 3.
Pre- and post-operative clinical and radiological data
Group I : mini-transforaminal lumbar interbody fusion, Group II : circumferential fusion, DH : disc height, NS : not significant, ODI : oswestry disability index, SL : segmental lordosis, VAS : visual analog scale, WL : whole lumbar lordosis
Clinical and functional outcomes
The clinical and functional outcomes for the 2 treatment groups, as analyzed by VAS and ODI scores, are summarized in Tables 2 and 3. At the postoperative follow-up assessment, both treatment groups showed significant improvement in all categories. Before surgery, both treatment groups had significantly higher disability scores. There were no statistically significant differences between the 2 groups in terms of pre- and postoperative VAS scores for back and leg pain and ODI scores (Table 2). However, clinical and functional data in both groups demonstrated statistically significant improvement from the pre- to postoperative periods (Table 3). The mean VAS scores for back and leg pain significantly decreased from 6.98 to 2.3 and 6.33 to 2.2 in the group I and from 7.38 to 1.7 and 6.0 to 1.0 in the group II, respectively. In the group I, mean ODI scores improved significantly from 51.85% to 14.4% and, in the group II, from 60% to 9.1% (Table 3).
Return to normal activity
There was no significant difference between the 2 groups in regard to the number of patients who returned to normal activity. In the group I, 45 of 46 patients returned to their normal activity, and in the group II, 30 of 32 patients returned to their normal activity.
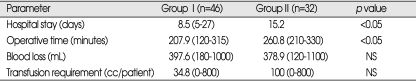
Treatment-related parameters
A summary of the operative results is presented in Table 4. The operative time for the group I (mean 207.9 minutes, range 120-315 minutes) appeared to be shorter than that for the group 2 (mean 260.8 minutes, 210-330), and there was significant difference between the 2 groups. The mean intraoperative blood loss among patients in the group I was 397.6 mL (180-1,000 mL), whereas it was 378.9 mL (120-1100) in the group II. This difference was not significant (p<0.05). Moreover, there appeared to be a shorter convalescence time for patients in the group I compared to those in the group II, the difference was significant (p<0.05).
Table 4.
Operative data
Group I : mini-transforaminal lumbar interbody fusion, Group II : circumferential fusion, NS : not significant
Complications
No serious complications including deep wound infection and revision surgery were experienced by any of the patients in the two treatment groups. One patient in the group I underwent a fracture of the pedicle screw placement. However, dynamic lumbar X-ray and 3D-CT scan later showed fusion mass. Complications related to the ALIF procedure included three cases of sympathetic changes, which were restored to normal state 2 to 4 months following surgery. There was one case of iliac vein injury, which caused more blood loss (1,100 cc) that needed 2 pints transfusion. There was one case of transient retrograde ejaculations following ALIF procedure, which returned to normal state.
DISCUSSION
Since Bagby introduced the early development of the lumbar interbody fusion (LIF) cage, LIF has been increasingly performed on patients with chronic low back pain due to low-grade isthmic spondylolisthesis1). A variety of different surgical techniques can be used to achieve LIF7,14,17). These interbody grafts can be placed either from a separate posterior, including the transforaminal, or from the anterior route.
In 1957, Southwick and Robinson introduced the retroperitoneal approach in ALIF30). After that, ALIF approaches to the spine have experienced many evolutionary changes. Some authors11,21) advocate the effectiveness of ALIF in relation to the following advantages of an anterior approach : direct visualization of the anteriorly displaced vertebral body; release of anterior longitudinal ligament (ALL); avoidance of back muscle trauma and posterior ligament structure; low possibility of a neural injury during the procedure due to indirect decompression; biomechanical widening of the vertebral bodies to their original DH and sagittal balance; weight bearing through the support of anterior column; relatively less need for blood transfusions; a short hospital stay; and a high fusion rate.
Moreover, recent literatures4,16,31) haves suggested that circumferential fusion can theoretically achieve most of the surgical goals in the treatment of isthmic spondylolisthesis. Kwon et al.16) reviewed the radiographic and clinical outcomes of many surgical methods used for the treatment of adult low-grade isthmic spondylolisthesis during recent decades. They concluded that a combined anterior and posterior fusion (circumferential fusion, 360 degree fusion) procedure would achieve the most reliable fusion rate and a successful clinical outcome. Swan et al.31) demonstrated that clinical and radiological outcomes of up to 2 years were superior after a circumferential fusion compared with posterior-alone surgery for unstable spondylolisthesis. Videbaek et al.33), although patient's demographic showed heterogeneous disease group, reported that the circumferentially fused patients had a significantly improved outcome compared with those treated by means of PLF.
However, the circumferential fusion technique requires a longer operative time, is associated with increased perioperative morbidity, higher risk of large vessel injury and may be technically more difficult to perform than posterior approach alone. These disadvantages associated with circumferential fusion, however, can be avoided by posterior approach such as mini-TLIF followed by PPF technique.
Recently, some studies have been reported on the topic of using TLIF to manage isthmic spondylolisthesis2,9,15,19). This approach allows exiting and traversing roots to be decompressed simultaneously, as well as stabilization of the anterior column from a single posterior approach. Some investigators9,15,19) have reported that lumbar lordosis could also be achieved and maintained by TLIF. According to other literature, TLIF has demonstrated its effectiveness in short-term studies with less morbidity and expense to the patient than the combined ALIF10,34). As expected, mini-TLIF approach in the present study can offer some advantages such as a shorter operative time, less paraspinal muscle damage, and less blood loss than circumferential fusion. Moreover, the radiological results in the present study such as DH, degree of listhesis, SL, and WL shows no significant difference between the two treatment groups except DH.
The TLIF approach can be performed in a standard open fashion through a midline lumbar incision, as well as in a mini-open fashion with expandable or nonexpendable working tubes8,13,25,27,29,32) and percutaneous pedicle screws13,25,29). The midline approach is associated with significant trauma to the back muscles and greater blood loss. Recently, authors of some studies8,25,27,29) on mini-TLIF have reported good clinical outcomes; the authors in the present study preferred the mini-open technique for all patients because it minimizes paraspinal muscle trauma and blood loss. The results of the current study also demonstrated that there were significant improvements in pain scores for back pain and leg pain between preoperative and postoperative assessments, although pain scores for back pain and leg pain did not significantly differ between the 2 groups.
In the present study, both treatment groups resulted in a high fusion rate. The fusion rates of 95.7% in the TLIF group and 100% in the circumferential fusion group in this study are comparable or more favorable to those in reports of other fusion techniques combining pedicle screw instrumentation and interbody cages. However, there was no statistically significant difference in the fusion rate between the TLIF and circumferential fusion groups.
Patients in the circumferential fusion group, although there was no significant difference, experienced better clinical outcomes than those in the TLIF group. Moreover, there were no significant differences between the 2 treatment groups in terms of sagittal aligment. These findings are somewhat congruent with those from other study results12,16) Goldstein et al.6) reported that changes in lordotic angles after lumbar fusion with a threaded interbody cage are not predictive of the clinical outcome. However, other investigators31) insisted that, theoretically, the more that the anatomical orientation is maintained, the better the long-term outcome due to the achievement of better spinal balance and decreasing adjacent segment stresses. Another report supports the fact that at the 2-year follow-up the circumferential fusion restored lordosis and provided a higher fusion rate than PLF.33) Therefore, this discordance between the clinical and radiological results may need to have a long enough follow-up study to adequately describe the relationship between the clinical and radiological outcomes and include radiological parameters such as pelvic incidence, pelvic tilt, sacral slope, pelvic lordosis angle, pelvic length and complementary lumbopelvic lordosis18,28). These radiological parameters could not be measured in some patients in our current series because plain radiographs did not show the full contour of the femoral heads and pelvis.
There are some limitations to the current study that should be mentioned; the study was a retrospective, uncontrolled review of the clinical outcomes achieved during a short follow-up period without consideration of psychosocial factors. A larger number of cases with a longer follow-up period than we used, is necessary to prove that examined parameters are effective factors affecting clinical outcomes. However, the present study was a two-center study, which gave the possibility of standardizing both the patient selection and the surgical techniques having similar patient demographics. A prospective trial in which patients are randomized to the TLIF group or the circumferential fusion group and studied during a long-term follow-up period with standard clinical outcome scale assessments would certainly provide more definitive answers and is under consideration.
CONCLUSION
Our results demonstrate that both instrumented mini-TLIF and instrumented circumferential fusion effectively reduce the clinical VAS and ODI scores and restore the radiological findings except whole lumbar lordosis. Clinical and functional outcomes were significantly improved in both groups of patients with adult low-grade isthmic spondylolisthesis.
Acknowledgements
This study was supported by a grant from Wooridul Spine Hospital.
References
- 1.Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. 1988;11:931–934. doi: 10.3928/0147-7447-19880601-13. [DOI] [PubMed] [Google Scholar]
- 2.Chastain CA, Eck JC, Hodges SD, Levi P. Transforaminal lumbar interbody fusion: a retrospective study of long-term pain relief and fusion outcomes. Orthopedics. 2007;30:389–392. doi: 10.3928/01477447-20070501-18. [DOI] [PubMed] [Google Scholar]
- 3.Christensen FB. Lumbar spinal fusion. Outcome in relation to surgical methods, choice of implant and postoperative rehabilitation. Acta Orthop Scand Suppl. 2004;75:2–43. [PubMed] [Google Scholar]
- 4.Christensen FB, Hansen ES, Eiskjaer SP, Høy K, Helmig P, Neumann P, et al. Circumferential lumbar spinal fusion with Brantigan cage versus posterolateral fusion with titanium Cotrel-Dubousset instrumentation : a prospective, randomized clinical study of 146 patients. Spine. 2002;27:2674–2683. doi: 10.1097/00007632-200212010-00006. [DOI] [PubMed] [Google Scholar]
- 5.Dou Y, Hao D, Wen S, He B. Comparison of clinical outcomes between two methods of posterior lumbar interbody fusion in adult spondylolisthesis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2006;20:743–746. [PubMed] [Google Scholar]
- 6.Goldstein JA, Macenski MJ, Griffith SL, McAfee PC. Lumbar sagittal alignment after fusion with a threaded interbody cage. Spine. 2001;26:1137–1142. doi: 10.1097/00007632-200105150-00009. [DOI] [PubMed] [Google Scholar]
- 7.Gödde S, Fritsch E, Dienst M, Kohn D. Influence of cage geometry on sagittal alignment in instrumented posterior lumbar interbody fusion. Spine. 2003;28:1693–1699. doi: 10.1097/01.BRS.0000083167.78853.D5. [DOI] [PubMed] [Google Scholar]
- 8.Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion : indications, technique, and complications. Neurosurg Focus. 2006;20:E6. doi: 10.3171/foc.2006.20.3.7. [DOI] [PubMed] [Google Scholar]
- 9.Houten JK, Post NH, Dryer JW, Errico TJ. Clinical and radiographically/neuroimaging documented outcome in transforaminal lumbar interbody fusion. Neurosurg Focus. 2006;20:E8. doi: 10.3171/foc.2006.20.3.9. [DOI] [PubMed] [Google Scholar]
- 10.Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine. 2001;26:567–571. doi: 10.1097/00007632-200103010-00023. [DOI] [PubMed] [Google Scholar]
- 11.Ishihara H, Osada R, Kanamori M, Kawaguchi Y, Ohmori K, Kimura T, et al. Minimum 10-year follow-up study of anterior lumbar interbody fusion for isthmic spondylolisthesis. J Spinal Disord. 2001;14:91–99. doi: 10.1097/00002517-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs WC, Vreeling A, De Kleuver M. Fusion for low-grade adult isthmic spondylolisthesis : a systematic review of the literature. Eur Spine J. 2006;15:391–402. doi: 10.1007/s00586-005-1021-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jang JS, Lee SH. Minimally invasive transforaminal lumbar interbody fusion with ipsilateral pedicle screw and contralateral facet screw fixation. J Neurosurg Spine. 2005;3:218–223. doi: 10.3171/spi.2005.3.3.0218. [DOI] [PubMed] [Google Scholar]
- 14.Kim NH, Lee JW. Anterior interbody fusion versus posterolateral fusion with transpedicular fixation for isthmic spondylolisthesis in adults. A comparison of clinical results. Spine. 1999;24:812–816. doi: 10.1097/00007632-199904150-00014. discussion 817. [DOI] [PubMed] [Google Scholar]
- 15.Kwon BK, Berta S, Daffner SD, Vaccaro AR, Hilibrand AS, Grauer JN, et al. Radiographic analysis of transforaminal lumbar interbody fusion for the treatment of adult isthmic spondylolisthesis. J Spinal Disord Tech. 2003;16:469–476. doi: 10.1097/00024720-200310000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Kwon BK, Hilibrand AS, Malloy K, Savas PE, Silva MT, Albert TJ, et al. A critical analysis of the literature regarding surgical approach and outcome for adult low-grade isthmic spondylolisthesis. J Spinal Disord Tech. 2005;18(Suppl):S30–S40. doi: 10.1097/01.bsd.0000133064.20466.88. [DOI] [PubMed] [Google Scholar]
- 17.La Rosa G, Conti A, Cacciola F, Cardali S, La Torre D, Gambadauro NM, et al. Pedicle screw fixation for isthmic spondylolisthesis : does posterior lumbar interbody fusion improve outcome over posterolateral fusion? J Neurosurg. 2003;99(2 Suppl):143–150. doi: 10.3171/spi.2003.99.2.0143. [DOI] [PubMed] [Google Scholar]
- 18.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O'Brien M, Chopin D, et al. Spondylolisthesis, pelvic incidence, and spinopelvic balance : a correlation study. Spine. 2004;29:2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 19.Lauber S, Schulte TL, Liljenqvist U, Halm H, Hackenberg L. Clinical and radiologic 2-4-year results of transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Spine. 2006;31:1693–1698. doi: 10.1097/01.brs.0000224530.08481.4e. [DOI] [PubMed] [Google Scholar]
- 20.Laus M, Tigani D, Pignatti G, Alfonso C, Malaguti C, Monti C, et al. Posterolateral spinal fusion : a study of 123 cases with a long-term follow-up. Chir Organi Mov. 1994;79:69–79. [PubMed] [Google Scholar]
- 21.Lee SH, Choi WG, Lim SR, Kang HY, Shin SW. Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis. Spine J. 2004;4:644–649. doi: 10.1016/j.spinee.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Madan S, Boeree NR. Outcome of posterior lumbar interbody fusion versus posterolateral fusion for spondylolytic spondylolisthesis. Spine. 2002;27:1536–1542. doi: 10.1097/00007632-200207150-00011. [DOI] [PubMed] [Google Scholar]
- 23.McAfee PC. Interbody fusion cages in reconstructive operations on the spine. J Bone Joint Surg Am. 1999;81:859–880. doi: 10.2106/00004623-199906000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Moller H, Hedlund R. Surgery versus conservative management in adult isthmic spondylolisthesis--a prospective randomized study : part 1. Spine. 2000;25:1711–1715. doi: 10.1097/00007632-200007010-00016. [DOI] [PubMed] [Google Scholar]
- 25.Mummaneni PV, Rodts GE., Jr The mini-open transforaminal lumbar interbody fusion. Neurosurgery. 2005;57(4 Suppl):256–261. doi: 10.1227/01.neu.0000176408.95304.f3. discussion 256-261. [DOI] [PubMed] [Google Scholar]
- 26.Osterman K, Schlenzka D, Poussa M, Seitsalo S, Virta L. Isthmic spondylolisthesis in symptomatic and asymptomatic subjects, epidemiology, and natural history with special reference to disk abnormality and mode of treatment. Clin Orthop Relat Res. 1993;297:65–70. [PubMed] [Google Scholar]
- 27.Ozgur BM, Yoo K, Rodriguez G, Taylor WR. Minimally-invasive technique for transforaminal lumbar interbody fusion (TLIF) Eur Spine J. 2005;14:887–894. doi: 10.1007/s00586-005-0941-3. [DOI] [PubMed] [Google Scholar]
- 28.Roussouly P, Gollogly S, Berthonnaud E, Labelle H, Weidenbaum M. Sagittal alignment of the spine and pelvis in the presence of L5-s1 isthmic lysis and low-grade spondylolisthesis. Spine. 2006;31:2484–2490. doi: 10.1097/01.brs.0000239155.37261.69. [DOI] [PubMed] [Google Scholar]
- 29.Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF) : technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1–S6. doi: 10.1097/01.bsd.0000132291.50455.d0. [DOI] [PubMed] [Google Scholar]
- 30.Southwick WO, Robinson RA. Surgical approaches to the vertebral bodies in the cervical and lumbar regions. J Bone Joint Surg Am. 1957;39-A:631–644. [PubMed] [Google Scholar]
- 31.Swan J, Hurwitz E, Malek F, van den Haak E, Cheng I, Alamin T, et al. Surgical treatment for unstable low-grade isthmic spondylolisthesis in adults : a prospective controlled study of posterior instrumented fusion compared with combined anterior-posterior fusion. Spine J. 2006;6:606–614. doi: 10.1016/j.spinee.2006.02.032. [DOI] [PubMed] [Google Scholar]
- 32.Tuttle J, Shakir A, Choudhri HF. Paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Technical note and preliminary report on 47 cases. Neurosurg Focus. 2006;20:E5. doi: 10.3171/foc.2006.20.3.6. [DOI] [PubMed] [Google Scholar]
- 33.Videbaek TS, Christensen FB, Soegaard R, Hansen ES, Høy K, Helmig P, et al. Circumferential fusion improves outcome in comparison with instrumented posterolateral fusion : long-term results of a randomized clinical trial. Spine. 2006;31:2875–2880. doi: 10.1097/01.brs.0000247793.99827.b7. [DOI] [PubMed] [Google Scholar]
- 34.Whitecloud TS, 3rd, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anterior-posterior interbody fusion of the lumbar spine : a financial analysis. J Spinal Disord. 2001;14:100–103. doi: 10.1097/00002517-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Yashiro K, Homma T, Hokari Y, Katsumi Y, Okumura H, Hirano A. The Steffee variable screw placement system using different methods of bone grafting. Spine. 1991;16:1329–1334. doi: 10.1097/00007632-199111000-00014. [DOI] [PubMed] [Google Scholar]