Abstract
BACKGROUND:
In the past two decades, cases involving patients requiring cardiac surgery have become more complex, presenting with more comorbidities. Outcome analysis has become very important in assessing the quality of cardiac surgical care in these patients. The latest version of the Parsonnet scoring system was developed in 2000 and is the most recent system available.
OBJECTIVE:
To evaluate the accuracy of the Parsonnet scoring system in a major Canadian university-based cardiac surgery centre with a population of high-risk patients.
METHODS:
Data on 4883 consecutive patients operated on between 2000 and 2005 were prospectively collected, and a standardized mortality rate was calculated using the Parsonnet score as the ratio of observed deaths to expected deaths. Analyses were conducted on the whole group and on subgroups, based on Parsonnet score distribution quantiles, age and surgery status.
RESULTS:
The mean Parsonnet score was 18.8±13.7 (range 0 to 83). The overall mortality rate was 6.4%. The overall standardized mortality ratio was 0.52 (95% CI 0.420 to 0.568), which was statistically significant (P=0.01). The observed mortality rate was significantly lower than expected in all categories.
CONCLUSIONS:
Despite more complex cases with multiple comorbidities, the results of cardiac surgery in a Canadian university hospital show better results than expected when using the Parsonnet score.
Keywords: Cardiac surgery, Mortality, Parsonnet score
Abstract
HISTORIQUE :
Depuis vingt ans, les cas de patients devant subir une chirurgie cardiaque sont devenus plus complexes et s’accompagnent d’un plus grand nombre de comorbidités. L’analyse des issues est devenue essentielle pour évaluer la qualité des soins de chirurgie cardiaque chez ces patients. La dernière version du score de Parsonnet a été mise au point en 2000 et est le système le plus récent disponible.
OBJECTIF :
Évaluer la précision du score de Parsonnet dans un grand centre universitaire canadien de chirurgie cardiaque peuplé de patients à haut risque.
MÉTHODOLOGIE :
Les auteurs ont colligé prospectivement les données sur 4 883 patients consécutifs opérés entre 2000 et 2005 et ont calculé le taux normalisé de mortalité en utilisant le score de Parsonnet comme ratio entre les décès observés et les décès prévus. Ils ont procédé à des analyses sur l’ensemble du groupe et sur des sous-groupes, d’après les quantiles de répartition du score de Parsonnet, l’âge et le statut de l’opération.
RÉSULTATS :
Le score de Parsonnet moyen était de 18,8±13,7 (fourchette de 0 à 83). Le taux de mortalité global était de 6,4 %. Le ratio normalisé global de mortalité était de 0,52 (95 % IC 0,420 à 0,568), ce qui était statistiquement significatif (p = 0,01). Le taux de mortalité observé était considérablement plus faible que prévu dans toutes les catégories.
CONCLUSIONS :
Malgré des cas plus complexes aux comorbidités multiples, les résultats de la chirurgie cardiaque dans un hôpital universitaire canadien sont meilleurs que prévu à l’aide du score de Parsonnet.
The past two decades have seen a significant change in the profile of patients who undergo cardiac surgery. The number of patients undergoing coronary artery bypass grafting (CABG) surgery is decreasing, but the proportion of patients requiring valve surgery is increasing. Moreover, cardiac surgery is now offered to high-risk patients who have several comorbidities. For these patients, surgical treatment was not an option in the previous decade. In this context, it is important that the evaluation of patient outcomes takes into account the overall patient risk profile. Quality management should not be based on crude assessments of mortality or complications, but rather on estimates of these outcomes that are adjusted for the baseline state and overall risk profile of the patient population. Failure to take baseline risk into consideration results in biased estimates of outcomes and poor quality assessments for institutions that are providing high-level, state-of-the-art care to high-risk patients. Patient registries are a valuable tool in conducting such independent reviews. In Canada, there is limited implementation of provincial databases in cardiac surgery with risk-adjustment algorithms, such as the one proposed by the Cardiac Care Network of Ontario (1). The province of Quebec, to date, does not have a provincial database for cardiac surgery.
Many scoring systems have been designed to predict mortality rate among cardiac surgery patients (1–6). Most of these scoring systems have been designed to assess CABG patients, but they have been widely applied to patients undergoing valvular heart operations. The EuroScore (3), The Society of Thoracic Surgeons database score (5,6) and the Parsonnet score (2) have been used to predict the risk of short-term mortality on the basis of preoperative patient characteristics. Evaluation of these risk models has shown that they are valid, especially in the low- or intermediate-risk patients. The predictive power of these models, however, becomes weaker for the higher-risk categories because of the smaller sample sizes.
The Division of Cardiac Surgery at the McGill University Health Centre (Montreal, Quebec) adopted the latest version of the Parsonnet scoring system after it was published in 2000 (2). This version was based on 37 parameters that are used to predict the perioperative mortality ratio of cardiac surgery patients. The purpose of the present study was to assess quality of care as measured by standardized mortality ratios (SMRs) based on quantifiable risk estimated by the Parsonnet scoring system, in a university-based cardiac surgery centre. This assessment is particularly important given the increasing prevalence of high risk cardiac surgery patients in our institution.
METHODS
Data were collected prospectively over a five-year period (2000 to 2005) and entered into the McGill University cardiac surgery registry. All patients undergoing cardiac surgery at the McGill University Health Centre are entered into the registry. Data were abstracted from patient charts and were entered into the registry by cardiac surgery nurses who were trained to abstract and enter data. All data were reviewed by the treating surgeon for quality assessment and final record closure. A Parsonnet score was calculated for all patients undergoing elective, urgent or emergency cardiac surgery at the two McGill University Health Centre sites, the Royal Victoria Hospital and the Montreal General Hospital (both in Montreal, Quebec). Individual patient Parsonnet scores were rounded to the nearest half-integer. Thus, the total score range was 0 to 100. Excluded were patients undergoing heart or heart-lung transplantation, as well as ascending, arch or thoracic aortic surgery, ventricular assist device implantation and adult congenital cardiac surgery. This is because the complexity of the procedures currently does not allow precise measurement of the risks associated with the operations. A total of 4883 patients were included in the present study.
Perioperative mortality in the present study was defined as proposed by The Society of Thoracic Surgeons, and included “death from any cause during or after operation within 30 days if the patient is discharged or within any interval if the patient is not discharged” (7). Moreover, for the purpose of the present study, inter-hospital transfers were not considered to be patient discharge.
Descriptive statistics were produced for all relevant variables. SMRs were calculated by indirect standardization using the Parsonnet score. For each patient, risk of mortality was estimated using the logistic regression parameters reported for the Parsonnet score (2). Therefore, for each patient the odds of death (Odeath) = ec+γ, where c is the constant and γ = β1X1+β2X2+…βnXn. β is the logistic regression coefficient for each variable and X is the value of the variable for the patient. The probability of death for each patient was estimated using the estimated Odeath as Odeath/(1+Odeath). The sum of the individual patient probabilities of death was used as the estimate of the number of expected deaths. SMRs were calculated as the ratio of observed deaths to expected deaths. The 95% CI for the SMR estimates were calculated according to the methods developed by Breslow and Day (8). An SMR of 1.0 indicates no difference between the observed and expected mortality rates. This suggests quality of care that is equivalent to the established standards. An SMR of less than 1.0 indicates quality of care that is superior to the established standard of care, and an SMR of greater than 1.0 indicates quality of care that is inferior to the standards of care. SMR analyses were conducted for the study sample as a whole, and for patient subgroups defined according to Parsonnet score distribution quantiles, age (younger than 70 years, 70 to 75 years, 76 to 79 years, and 80 years or older) and surgery status (elective, emergency and urgent). For these subgroups, mortality risk was estimated from the Parsonnet score without consideration of the variance in the risk associated with each subgroup. These stratified analyses were conducted to observe variation in the quality of care between clinically important patient groups. In the article published by Bernstein and Parsonnet (2), the maximum Parsonnet score was 50.0. However, the actual possible range of the Parsonnet score is between 0 and 100. In the current study, patients with Parsonnet scores greater than 50.0 were included in the analysis. This is acceptable, because the estimation of mortality risk is not limited by the observed score range of the original article, but rather by the actual possible range of the score. The predictive accuracy of the score is based on the validity of the parameter estimates for each variable included in the model. It follows that a score of any value can be achieved through various combinations of different variables, not only a limited set of variables. Therefore, scores beyond the reported range are possible and should have the same predictive validity as lower scores. Therefore, the estimates of the mortality risk for patients with scores greater than 50.0 remain valid, and these patients were included in the analysis. As a reference, however, patients with Parsonnet scores greater than 50.0 were analyzed as a separate subgroup.
RESULTS
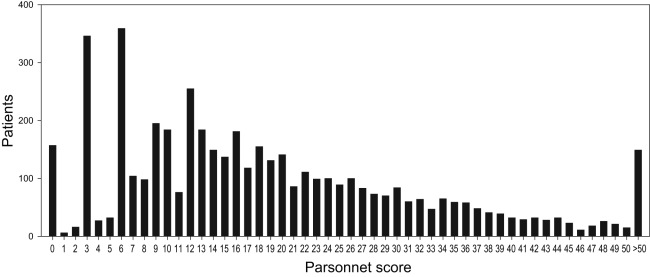
There were 4883 patients included in the present study, 56.3% of whom were male. The mean patient age was 65.6±11.0 years, with a range of 18 to 94 years and a median of 67 years. Approximately 20% of the patients were older than 75 years of age, and 7% were older than 80 years of age. A total of 3271 patients (67%) underwent isolated CABG surgery, while the others underwent valvular surgery or combined procedures. Seventy-seven per cent of patients with a score of less than 30 underwent isolated CABG surgery, while only 33% of patients with scores of 30 or higher underwent CABG surgery alone. The prevalence of comorbid conditions in the study cohort is summarized in Table 1. These results show that the majority of patients had a history of hypertension (74.9%), followed by congestive heart failure (37.3%), diabetes (30.9%), ejection fraction between 30% and 49% (30.9%), left main coronary artery disease (21.6%) and pulmonary hypertension (15.1%). Figure 1 demonstrates the distribution of Parsonnet scores for the study population. The mean Parsonnet score for the study cohort was 18.8±13.7, with a range of 0 to 83 and a median of 16. Operative status was urgent for 2672 patients (54.7%), elective for 1785 patients (36.6%) and emergent for 426 patients (8.7%). The overall mortality rate was 6.37% (n=311).
TABLE 1.
Prevalence of comorbid conditions (n=4883)
| Condition | n (%) |
|---|---|
| Hypertension | 3657 (74.9) |
| Congestive heart failure | 1821 (37.3) |
| Diabetes | 1509 (30.9) |
| Ejection fraction 30% to 49% | 1509 (30.9) |
| Left main coronary artery disease | 1055 (21.6) |
| Pulmonary hypertension | 737 (15.1) |
| Renal failure | 615 (12.6) |
| Mitral valve | 620 (12.7) |
| Valve and aortocoronary bypass | 591 (12.1) |
| Chronic obstructive pulmonary disease | 542 (11.1) |
| Morbid obesity | 493 (10.1) |
| Ejection fraction <30% | 483 (9.9) |
| Severe peripheral vascular disease | 474 (9.7) |
| Aortic valve | 469 (9.6) |
| Severe neurological disorder | 293 (6.0) |
| Preoperative intra-aortic balloon pump | 269 (5.5) |
| Cardiogenic shock | 249 (5.1) |
| Carotid disease | 171 (3.5) |
| Asthma | 146 (3.0) |
| Dialysis dependency | 146 (3.0) |
| Active endocarditits | 88 (1.8) |
| Tricuspid valve | 78 (1.6) |
| Cirrhosis | 44 (0.9) |
| Idiopathic thrombocytopenia | 19 (0.3) |
| Pacemaker | 24 (0.5) |
| Treated endocarditits | 24 (0.5) |
Figure 1).
Patient distribution in each Parsonnet score (n=4883)
Table 2 summarizes the SMR analyses for the study sample and relevant patient subgroups. These results show that there were a total of 311 deaths (6.37%), while 594 deaths (12.16%) were expected according to indirect standardization. The overall SMR was 0.52 (95% CI 0.420 to 0.568). This indicates that the observed mortality rate was 48% less than that expected. The overall SMR was statistically significant (P=0.001).
TABLE 2.
Standardized mortality ratio analyses
| Stratum | Patients, n | Mortality
|
Standardized mortality ratio
|
P | |||
|---|---|---|---|---|---|---|---|
| Observed, n (%) | Expected, n (%)* | Estimate | 95% CI | ||||
| Total | All | 4883 | 311 (6.37) | 594 (12.16) | 0.52 | 0.424–0.568 | 0.001 |
| Parsonnet score (categories) | 0–6.9 | 951 | 4 (0.4) | 20 (2.2) | 0.20 | 0.069–0.583 | 0.001 |
| 7.0–12.9 | 744 | 7 (0.9) | 25 (3.4) | 0.28 | 0.122–0.643 | 0.001 | |
| 13.0–16.9 | 831 | 17 (2.0) | 39 (4.7) | 0.44 | 0.249–0.764 | 0.001 | |
| 17.0–22.9 | 749 | 27 (3.6) | 56 (7.5) | 0.48 | 0.308–0.755 | 0.001 | |
| 23.0–32.9 | 829 | 53 (6.4) | 117 (14.1) | 0.45 | 0.332–0.618 | 0.001 | |
| 33.0–50.9 | 630 | 128 (20.3) | 226 (35.9) | 0.57 | 0.476–0.692 | 0.001 | |
| ≥51 | 149 | 75 (50.3) | 110 (73.7) | 0.68 | 0.566–0.821 | 0.001 | |
| Age (years) | <70 | 3032 | 111 (3.66) | 273 (9.02) | 0.41 | 0.304–0.485 | 0.001 |
| 70–75 | 881 | 77 (8.74) | 116 (13.2) | 0.66 | 0.460–0.866 | 0.001 | |
| 76–79 | 535 | 55 (10.28) | 99 (18.53) | 0.55 | 0.349–0.730 | 0.001 | |
| ≥80 | 435 | 68 (15.63) | 105 (24.13) | 0.65 | 0.409–0.829 | 0.001 | |
| Surgical status | Elective | 1785 | 54 (3.03) | 169 (9.47) | 0.32 | 0.215–0.413 | 0.001 |
| Emergent | 426 | 92 (21.6) | 115 (27.08) | 0.80 | 0.537–1.033 | 0.080 | |
| Urgent | 2672 | 165 (6.18) | 309 (11.58) | 0.53 | 0.424–0.568 | 0.001 | |
*Calculated as the average individual predicted mortality risk, as estimated by the Parsonnet score for each patient in the corresponding stratum
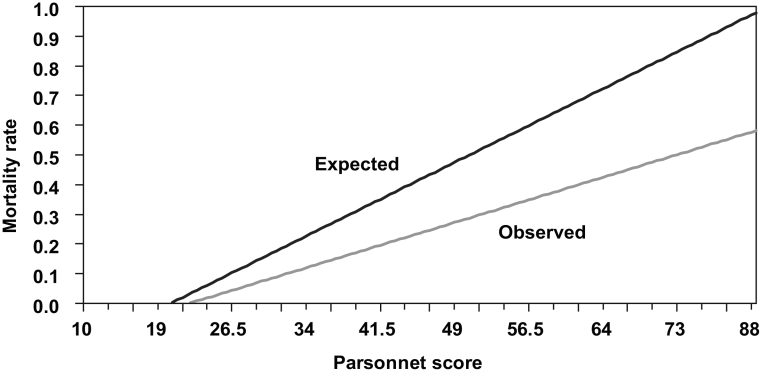
Figure 2 shows the linear regression modelling for the observed and expected mortality rates as a function of the Parsonnet score. These results show that the observed mortality rate was significantly lower than the expected rate according to indirect standardization to the Parsonnet model. Linear regression analyses produced a parameter estimate of 0.0082% per Parsonnet score unit for the expected mortality rate compared with 0.0052% per unit for the observed mortality rate. These two parameter estimates are significantly different (P<0.001) and indicate an overall adjusted SMR of 0.63 (P<0.001).
Figure 2).
Linear regression model comparing the observed mortality with expected mortality in study patients
Stratification by Parsonnet score showed that the observed mortality rate was significantly lower than expected for all categories, as indicated by SMR estimates that were statistically significantly lower than unity (P=0.001).
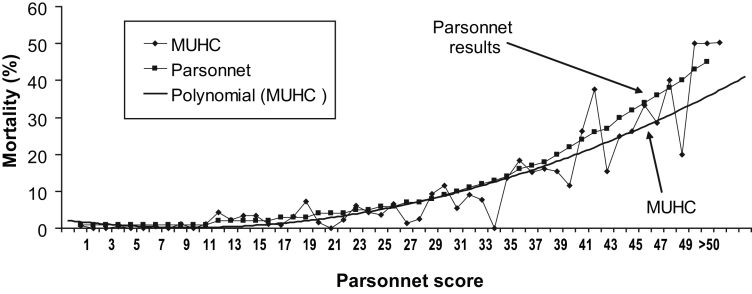
Figure 3 shows the actual Parsonnet-predicted mortality risk rate compared with the observed McGill University Health Centre patient mortality rate for all score categories. The solid line is based on a multivariate model for the observed mortality rate as a function of the Parsonnet score. The McGill University Health Centre mortality rate was lower for all categories of scores.
Figure 3).
Comparison of Parsonnet curve to observed mortality curve at the McGill University Health Centre ([MUHC] Montreal, Quebec). The multivariate curve was derived from the observed mortality curve in 4883 patients through the curve-fit model of Excel software (Microsoft Windows Office 2003; Microsoft Inc, USA)
Stratification by age also showed significantly lower observed versus expected mortality rates, as shown by the significant SMR estimates (P=0.001). The lowest SMR estimate was observed for those patients who were younger than 70 years of age, followed by the estimate for patients between 76 and 79 years of age. Higher SMR estimates were observed for patients in the 70 to 75 years old and 80 years or older age groups.
Patients undergoing elective surgery had significantly lower SMR rates than patients undergoing emergent or urgent surgery. The SMR estimate for elective and urgent cases was statistically significantly lower than unity (P=0.001); however, the estimate for emergent patients was lower than unity, but only approached statistical significance (P=0.080). The latter observation may be due to the smaller number of patients in the emergent surgery group.
DISCUSSION
In the current study, the Parsonnet score was used to produce estimates of expected pericardiac surgery mortality as a function of baseline patient comorbidity. The Parsonnet score model was recently developed using data from a large cohort of patients undergoing cardiac surgery procedures in 10 New Jersey centres during 1994 and 1995 (2). Other methods have been developed primarily for CABG surgery patients, while the Parsonnet score has been based on 10,703 patients undergoing CABG, valve replacement or repair, or a combination of procedures. The advantage of the Parsonnet score is that the parameters representing risk factors are easily and objectively measurable, and have high content validity that is recognized and accepted by the majority of clinicians. As opposed to other scoring methods, variables that are based completely or even partly on subjective assessment, such as unstable angina, operative priority or diffuseness of disease, are not included in this model. Outcomes after CABG surgery have been extensively studied (9–14), and many scoring systems have been developed for these patients; their use has been extended to other types of cardiac operations. As the number of CABG procedures rapidly declines and the number of valvular or combined operations rises, it is important to use a scoring system that is applicable to all patients.
One of the inherent problems with most predictive scoring systems is the very broad CI for higher-score categories. This is due to the smaller numbers of patients and the higher variability in these higher categories. Most scoring systems in use today were developed using cohorts of patients in which isolated CABG was the predominant procedure. The paper by Parsonnet and Bernstein (2) does not mention the proportion of CABG surgery compared with other procedures. Our study clearly documented that higher-risk patient cohorts consist mostly of patients undergoing procedures other than isolated CABG surgery (67% of patients with scores of 30 or greater underwent other procedures). The higher variability of procedures may partially explain the lower predictive power of the model for scores of 30 or greater.
Risk stratification models have been developed for valve surgery (4,15,16). Nowicki et al (16) suggested two models for risk stratification of patients undergoing either aortic or mitral valve surgery. These mathematical models were highly accurate in predicting in-hospital mortality. The area under the receiver operating characteristic curve was 0.75 (95% CI 0.72 to 0.77) for aortic valve patients and 0.79 (95% CI 0.76 to 0.81) for mitral valve patients.
However, the Parsonnet scoring system includes only patient characteristics and comorbid conditions that can be easily ascertained before surgery, and may appear better suited to an increasingly diversified population of patients in terms of procedures and comorbidities.
The model has also been used to preoperatively identify patients who are likely to spend longer than 24 h in the intensive care unit (17). In another study (18), a Parsonnet score of greater than 20 strongly predicted readmission to the intensive care unit in fast-tracked patients (OR 3.08, 95% CI 1.43 to 6.69). Such a model can therefore serve multiple purposes in the administration of a busy cardiac surgery service in an era of scant resources.
This was a retrospective study of registry data obtained during a five-year period from a large, Canadian, university-based cardiac surgery centre. A review of patient profiles revealed that the study cohort had a relatively high-risk baseline profile. This is evident by increased age and the high proportion of patients older than 75 years of age. Thirty-three per cent of patients in this cohort underwent procedures other than isolated CABG surgery. This declining proportion of CABG operations over other procedures has been observed around the world in recent years and should be taken into consideration when assessing outcomes of cardiac surgery as a whole. In addition, our cohort had a high prevalence of clinically important comorbid conditions, including congestive heart failure and diabetes, as one would expect from general, multispecialty tertiary centres performing cardiac surgery. Moreover, a high-volume heart failure and transplantation program attracts a large number of patients who are now offered conventional surgical options.
The results of our study have shown that despite the increased baseline risk, the observed mortality rate in our cohort was consistently significantly lower than that expected by standardization with the Parsonnet score cohort. This was observed for moderate-risk and high-risk patients. The higher patient risk profile in our institution during the study period has contributed, through volume-performance association, to the improved outcomes of our high-risk patients. It is safe to presume that the Parsonnet scoring system can be applied to our cohort of patients undergoing cardiac surgery in the current era, as well as in the Canadian health care system. It can be used to measure quality of care and plan for resource use.
Acknowledgments
The authors express their gratitude to Ms Christine Pagé RN and Ms Catherine Robineau RN for the prospective collection of data on this cohort of patients. Ms Jocelyne Prince played a very important role in data entry.
REFERENCES
- 1.Tu JV, Jaglal SB, Naylor CD. Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Steering Committee of the Provincial Adult Cardiac Care Network of Ontario. Circulation. 1995;91:677–84. doi: 10.1161/01.cir.91.3.677. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein AD, Parsonnet V. Bedside estimation of risk as an aid for decision-making in cardiac surgery. Ann Thorac Surg. 2000;69:823–8. doi: 10.1016/s0003-4975(99)01424-1. [DOI] [PubMed] [Google Scholar]
- 3.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surgery. 1999;16:9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 4.Ambler G, Omar RZ, Royston P, Kinsman R, Keogh BE, Taylor KM. Generic, simple risk stratification model for heart valve surgery. Circulation. 2005;112:224–31. doi: 10.1161/CIRCULATIONAHA.104.515049. [DOI] [PubMed] [Google Scholar]
- 5.Clark RE. The development of The Society of Thoracic Surgeons voluntary national database system: Genesis, issues, growth, and status. Best Pract Benchmarking Healthc. 1996;1:62–9. [PubMed] [Google Scholar]
- 6.Edwards FH, Clark RE, Schwartz M. Practical considerations in the management of large multiinstitutional databases. Ann Thorac Surg. 1994;58:1841–4. doi: 10.1016/0003-4975(94)91724-8. [DOI] [PubMed] [Google Scholar]
- 7.Guidelines for reporting morbidity and mortality after cardiac valvular operations. Ann Thorac Surg. 1988;46:257–9. doi: 10.1016/s0003-4975(10)65920-6. [DOI] [PubMed] [Google Scholar]
- 8.Breslow NE, Day NE. Statistical methods in cancer research Volume II – The Design and Analysis of Cohort Studies. International Agency for Research on Cancer; Lyon: 1987. [PubMed] [Google Scholar]
- 9.Ghali WA, Quan H, Shrive FM, Hirsch GM, Canadian Cardiovascular Outcomes Research Team Outcomes after coronary artery bypass graft surgery in Canada: 1992/93 to 2000/01. Can J Cardiol. 2003;19:774–81. [PubMed] [Google Scholar]
- 10.Hannan EL, Kilburn H, Jr, O’Donnell JF, Lukacik G, Shields EP. Adult open heart surgery in New York State. An analysis of risk factors and hospital mortality rates. JAMA. 1990;264:2768–74. [PubMed] [Google Scholar]
- 11.O’Connor GT, Plume SK, Olmstead EM, et al. A regional prospective study of in-hospital mortality associated with coronary artery bypass grafting. The Northern New England Cardiovascular Disease Study Group. JAMA. 1991;266:803–9. [PubMed] [Google Scholar]
- 12.Tu JV, Naylor CD. Coronary artery bypass mortality rates in Ontario. A Canadian approach to quality assurance in cardiac surgery. Steering Committee of the Provincial Adult Cardiac Care Network of Ontario. Circulation. 1996;94:2429–33. doi: 10.1161/01.cir.94.10.2429. [DOI] [PubMed] [Google Scholar]
- 13.Ghali WA, Quan H, Brant R. Coronary artery bypass grafting in Canada: National and provincial mortality trends, 1992–1995. CMAJ. 1998;159:25–31. [PMC free article] [PubMed] [Google Scholar]
- 14.Ghali WA, Quan H, Brant R. Coronary artery bypass grafting in Canada: Hospital mortality rates, 1992–1995. CMAJ. 1998;159:926–30. [PMC free article] [PubMed] [Google Scholar]
- 15.Jamieson WR, Edwards FH, Schwartz M, Bero JW, Clark RE, Grover FL. Risk stratification for cardiac valve replacement. National Cardiac Surgery Database. Database Committee of The Society of Thoracic Surgeons. Ann Thorac Surg. 1999;67:943–51. doi: 10.1016/s0003-4975(99)00175-7. [DOI] [PubMed] [Google Scholar]
- 16.Nowicki ER, Birkmeyer NJ, Weintraub RW, et al. Northern New England Cardiovascular Disease Study Group and the Center for Evaluative Clinical Sciences, Dartmouth Medical School Multivariable prediction of in-hospital mortality associated with aortic and mitral valve surgery in Northern New England. Ann Thorac Surg. 2004;77:1966–77. doi: 10.1016/j.athoracsur.2003.12.035. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence DR, Valencia O, Smith EE, Murday A, Treasure T. Parsonnet score is a good predictor of the duration of intensive care unit stay following cardiac surgery. Heart. 2000;83:429–32. doi: 10.1136/heart.83.4.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kogan A, Cohen J, Raanani E, et al. Readmission to the intensive care unit after “fast-track” cardiac surgery: Risk factors and outcomes. Ann Thorac Surg. 2003;76:503–7. doi: 10.1016/s0003-4975(03)00510-1. [DOI] [PubMed] [Google Scholar]